Abstract
Australia, New Zealand and the Pacific Region define a large area in the southern hemisphere comprising multiple countries with disparate characteristics. Defining the Pacific Region is challenging as there is no consensus on which countries are included. Thus, the World Bank includes The Federated States of Micronesia, Fiji, Kiribati, Palau, the Republic of the Marshall Islands, Samoa, the Solomon Islands, Tonga and Vanuatu (The World Bank 2009).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Australia, New Zealand and the Pacific Region define a large area in the southern hemisphere comprising multiple countries with disparate characteristics. Defining the Pacific Region is challenging as there is no consensus on which countries are included. Thus, the World Bank includes The Federated States of Micronesia, Fiji, Kiribati, Palau, the Republic of the Marshall Islands, Samoa, the Solomon Islands, Tonga and Vanuatu (The World Bank 2009). According to the World Health Organization (World Health Organisation 2009), the Western Pacific Region in addition to the aforementioned countries also includes Cook Islands, Nauru, Niue, Palau Papua and Papua New Guinea, and additional countries which fit into the Asia Pacific Region, not included in this chapter. While Australia and New Zealand are relatively wealthy, developed countries, the countries encompassing the Pacific Region are more socio-economically diverse. In contrast cultural and ethnic diversity is high in Australia and New Zealand while countries in the Pacific Region, with the exception of Fiji, tend to be relatively ethnically homogeneous. A further distinguishing feature of the areas covered in this chapter is political stability, which is high in Australia and New Zealand but less so in many of the countries encompassing the Pacific Region.
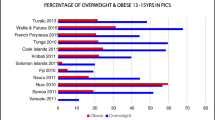
The epidemiology of overweight and obesity is well described in Australia and New Zealand. This is not the case in the Pacific Region, with no nationally representative data available for many of the smaller Pacific Region countries. Similar patterns of obesity prevalence have been documented in Australia and New Zealand over recent decades, indicating that more than half the adult population and approximately one quarter of the child and adolescent populations are currently overweight or obese. Secular trend data suggest these rates of overweight and obesity have increased over recent decades. Obesity prevalence amongst Pacific Region populations tends to be higher than in Australia and New Zealand, but coexists with issues of undernutrition, particularly amongst children.
While many studies conducted in Australia and New Zealand describe the prevalence of overweight and obesity and associations with potential risk factors, studies involving nationally representative samples in these countries are sparse with no systematic regular national data collection in Australia or New Zealand. The available nationally representative studies investigating the prevalence of overweight and obesity provide limited information on associations with potential risk factors.
This chapter describes evidence from nationally representative studies on the prevalence of overweight and obesity in children and youth in Australia and New Zealand and, where available, provides information on associations with potential risk factors. With no nationally representative data available for countries within the Pacific Region, estimates from large scale prevalence studies are reported.
Geographic Area
The geographic area encompassing Australia, New Zealand and the Pacific Region consists of more than 85 million square kilometers of land mass. Each country within this region is an island, or series of islands. Australia makes up the vast majority of the total land mass, although much of the land area is sparsely populated, with most of the population inhabiting the coastal areas. The combined population of Australia, New Zealand and the Pacific Region exceeds 33 million people. Approximately two thirds of this total population inhabits Australia (>20 million), with the next most populous country being Papua New Guinea (>6 million) followed by New Zealand (> 4 million) (see Table 7.1).
This is a culturally diverse region. Within Australia 2.5% of the population are indigenous (Aboriginal or Torres Strait Islander) and 25% of the population have recently immigrated, mainly from Europe or Asia. The remaining majority of inhabitants are Australian born but represent the cultural diversity of a predominantly immigrant nation, with a high proportion of second-, third- and subsequent-generation Australians of predominantly European background (Australian Bureau of Statistics 2006). This cultural diversity has implications for the prevalence of overweight and obesity, with the rates of these conditions known to be higher amongst certain cultural and ethnic groups, for example, higher amongst Mediterranean peoples who are populous in Australia. New Zealand has a much larger indigenous population than Australia. More than one quarter of the New Zealand population identify as either Maori or Pacific, with the remainder predominantly of European or Asian descent. While information is available for only a few Pacific Region countries, the majority of these are primarily inhabited by indigenous peoples: Tonga 98% indigenous (Tonga Department of Statistics 2006); Cook Islands 90% indigenous (Secretariat of the Pacific Community Noumea New Caledonia 1999); Vanuatu 99% indigenous (Vanuatu National Statistics Office 1999). The exception is Fiji where 57% of the population are indigenous, 38% Indian and the remainder born in other countries (Fiji Islands Bureau of Statistics 2007).
Disparities in wealth and health across the countries comprising these regions are highlighted by rankings on the Human Development Index (HDI), which provides a composite measure of the achievements of a country on three broad dimensions of human development. These dimensions are: (1) living a long and healthy life, as measured by life expectancy at birth; (2) knowledge or education, as measured by adult literacy rates and gross primary, secondary and tertiary level education enrolment; and (3) standard of living, as measured by gross domestic product per capita in purchasing power parity. Australia ranks highest in the region and second internationally, with New Zealand also ranked amongst the high human development countries (20th internationally). Only six Pacific Region Countries have a ranking on the HDI (ranging from 94th to 148th internationally), all classified as having medium human development. Thus while Australia and New Zealand are clearly classified as developed nations, many of the countries comprised within the Pacific Region fall within the classification of developing nations.
The per capita gross domestic product of Australia ($38,100) and New Zealand ($27,900) far exceeds that of any of the Pacific Region countries ($1,900 to $9,100). This is reflected in general health statistics, with infant mortality of less than 5 per 1,000 live births in Australia and New Zealand, compared with much higher rates in most of the Pacific Region countries. The highest infant mortality rates are recorded in Papua New Guinea, with in excess of 45 per 1,000 live births. These trends in infant mortality are also reflected in life expectancies across countries. In both Australia and New Zealand the average life expectancy of the population exceeds 80 years. This is notably higher than in the Pacific Region countries where average life expectancy ranges between 63 and 74 years. Crude birth rates for Australia and New Zealand (12.6 and 14.1 per 1,000 population, respectively) are lower than for the Pacific Region countries (range: 16.7 to 31.5 per 1,000 population). As would be expected with higher life expectancy and lower birth rates, the number of youth (aged under 15 years) as a proportion of the total population is lower in Australia (19.6%) and New Zealand (20.7%) than in Pacific Region countries (22.9 to 39.5%).
Prevalence of Overweight and Obesity
For all studies reported here, overweight and obesity are defined based on the age- and sex-specific body mass index cut-off points recommended by the International Obesity Task Force (Cole et al. 2000). Table 7.2 provides an overview and comparison of the prevalence of overweight and obesity by different countries in the region.
Australia
The most recent nationally representative data on the prevalence of overweight and obesity in Australian children and adolescents come from three recent population-based studies: the 2007–2008 National Health Survey (Australian Bureau of Statistics 2009) which included children aged 5–17 years of age; the 2007 Australian National Children’s Nutrition and Physical Activity Survey (Commonwealth of Australia 2008) which involved children 2–16 years of age; and the Longitudinal Study of Australian Children (LSAC) (Soloff et al. 2005) which involved children 4–5 years of age.
The 2007–2008 National Health Survey was conducted between August 2007 and June 2008. It is the seventh in a series of national surveys assessing the health of Australians which have been conducted by the Australian Bureau of Statistics since 1977, but the first to collect anthropometric data on children. This survey collected information on a broad range of health-related issues from residents in more than 15,800 randomly selected private homes across Australia. Within each of these homes, one adult (aged 18 years and over) and one child were randomly selected for inclusion in the survey. This sample closely approximated the socio-demographic characteristics of the wider population, however, population weights were applied to the data.
The 2007 Australian National Children’s Nutrition and Physical Activity Survey was conducted between February and August 2007 and involved a total of 4,487 children aged 2–16 years from across Australia. Households containing children 2–16 years of age were randomly sampled using random digit dialing. One child from each eligible household participated. Approximately 500 girls and 500 boys were sampled from each of the age groups: 2–3, 4–8, 9–13, 14–16 years. In addition, one state (South Australia) funded the collection of data from an additional 400 children in that state. This survey was limited by the fact that the sample was not representative of the Australian population in terms of cultural diversity or socio-economic diversity. The resultant sample contained a lower proportion of non-Australian born caregivers (parents or guardians), families speaking a language other than English at home, and children of indigenous background, than were reported in 2006 national Census data (Australian Bureau of Statistics 2006). In addition, the sample appeared to underrepresent socio-economically disadvantaged families by having a substantially higher proportion of tertiary educated caregivers and households in the higher income brackets than would be expected based on national Census data. Population weights were applied to data from the 2007 Australian National Children’s Nutrition and Physical Activity Survey to minimize the impact of these sampling biases.
The first wave of the Longitudinal Study of Australian Children (LSAC) was conducted between March and November 2004. It collected data from two cohorts of children: 5,107 infants aged 3–19 months (not discussed here as overweight and obesity prevalence was not investigated in this cohort) and 4,983 children aged 4–5 years (59% of those selected for the sample participated). Children were sampled from 311 postal areas across Australia that were randomly selected with probability proportional to size, stratified by state or territory and by a capital city vs. rest of state dichotomy. An average of 40 children were selected from each postal area in larger states and an average of 20 children selected from postal areas in smaller states and territories. The resultant sample was broadly representative of the Australian population although children whose parents had completed secondary school were slightly overrepresented and children living in single parent families were underrepresented. Population weights were applied to the data.
Findings from the 2007 to 2008 National Health Survey
Height, weight and waist circumference data were collected from children in the 2007–2008 National Health Survey by trained assessors during face-to-face interviews in the home. National prevalence estimates of overweight and obesity, stratified by age groupings, are presented in Table 7.3. Proportions of children overweight and obese in this cohort were not presented stratified by sex and age concurrently, although child and adolescent datas were presented by sex. Overall, 17% of 5–17 year old children were classified as overweight and 8% as obese. Proportions of children classified above the healthy weight range (i.e. overweight or obese) were similar for boys (26%) and girls (24%), however, the proportion of boys who were obese (10%) was higher than the proportion of girls (6%) (Australian Bureau of Statistics, 2009). The prevalence of overweight and obesity increased across the age groupings included in the study. While waist circumference was measured in this survey, crude average waist circumference measurements were reported which do not allow classification of overweight and obesity.
Findings from the 2007 Australian National Children’s Nutrition and Physical Activity Survey
Height, weight and waist circumference data were collected from children in the 2007 Australian National Children’s Nutrition and Physical Activity Survey by trained assessors during face-to-face interviews in the home. Additional information on food intake and activity levels was collected during a subsequent telephone interview. National prevalence estimates of overweight and obesity, for boys and girls in each of the age groups sampled are presented in Table 7.4. Overall, approximately 5% of Australian children were found to be underweight, 17% overweight and 6% obese. With an additional 5% classified as thin (underweight), almost three quarters (72%) of these children were of a healthy weight (Commonwealth of Australia 2008).
While there is less agreement on appropriate cut-off points to define overweight and obesity using waist circumference measurements, a commonly applied definition of excess weight assessed by waist circumference for those aged 5 years and above is a waist-to-height ratio greater than 50% (Ashwell and Hsieh 2005). This is the definition applied in the 2007 Australian National Children’s Nutrition and Physical Activity Survey. Proportion of children exceeding 50% waist-to-height ratio are presented for boys and girls in each of the sampled age groups in Table 7.4. Note that the proportion exceeding the ratio is not presented for the 2–4 years age groups as there is no agreed cut-off point for young children. For Australian children aged 5–16 years, approximately one sixth had waist circumferences which exceeded the 50% waist-to-height ratio.
Significant inverse associations between physical activity level (measured by a 4-day computer assisted activity recall) and weight category were found for children aged 9–16 years. Physical activity level was not assessed for younger children. Children aged 9–16 years who were thin (underweight) or obese tended to report lower physical activity levels than children who were classified as being of healthy weight. Physical activity levels for children who were overweight were similar to levels for children who were classified as being of healthy weight. Reporting biases may have influenced this subjective physical activity data.
Associations between total energy intake (measured by food recall using a three pass 24 h recall interview methodology) and weight category were found for 2–16 year old children. Obese children tended to report lower energy intakes than healthy weight children. This may reflect reporting biases or methodological issues inherent in the use of a single day’s food recall. No differences were noted in energy intake between healthy weight children and either thin (underweight) or overweight children.
Findings from the Longitudinal Study of Australian Children (2004)
Height, weight and waist circumference were collected from children in the Longitudinal Study of Australian Children by trained assessors during face-to-face interviews in the home. Prevalence estimates for overweight and obesity in these 4–5 year old children were 15% and 6% respectively (Wake et al. 2007). Prevalence was higher for girls (17% overweight and 6% obese) than boys (14% overweight and 5% obese). The prevalence of overweight and obesity was higher amongst the 181 children of Aboriginal or Torres Strait Islander (indigenous) descent included in the sample (17% overweight and 11% obese) and also amongst the 613 children who spoke a language other than English at home (17% overweight and 8% obese). There was evidence of a socio-economic gradient in overweight and obesity prevalence. Prevalence of overweight and obesity by maternal education level (one measure of socio-economic position) is presented in Table 7.5. Similar results were seen for other measures of socio-economic position. Children of lower socio-economic position, as indicated independently by each of maternal education, family income, postal area level socio-economic disadvantage (Socio-Economic Indices For Areas (SEIFA)), and highest family occupation class, had higher odds of being classified as overweight or obese. With no agreed definition of excess weight by waist circumference, average crude waist circumference measurement for 4–5 year old children was reported in the Longitudinal Study of Australian Children. The average waist circumference measurement was 54.6 cm, with average measurements being almost identical for boys and girls.
Secular Trends
Australia does not have a regular national monitoring or surveillance system for childhood overweight and obesity and does not regularly collect national data on body mass index, diet or activity levels in children and adolescents. Prior to the 2007 Australian National Children’s Nutrition and Physical Activity Survey and the 2007–2008 National Health Survey, a national survey including assessment of children’s adiposity had not been conducted for over a decade, since the 1995 National Nutrition Survey, and prior to that in the 1985 Australian Health and Fitness Survey. While the sampling frames of these surveys were quite different, all had trained assessors measure height and weight from which body mass index was derived and provide some evidence of secular trends in weight status in the Australian child and adolescent population (see Table 7.6).
Sampling methodologies of the 2007 Australian National Children’s Nutrition and Physical Activity Survey and the 2009–2008 National Health Survey are reported above. Sampling for the 1995 National Nutrition Survey involved a systematically selected subsample of private homes involved in the 1995 National Health Survey. Data collection from 2,962 2–18 year old children occurred between February 1995 and March 1996. Sampling for the 1985 Australian Health and Fitness Survey involved a random sample of 109 schools selected proportional to total number of children enrolled, followed by a systematic selection of 15 students within each age and sex category. Data collection from 8,492 7–15 year old children occurred between May and October 1985.
For boys, secular increases in the prevalence of overweight and obesity were observed across the 1995 and 2007 national surveys for 2–3 and 4–6 year old children (4–8 years in 2007 survey). For girls, there was no clear secular trend amongst these age groups. Data were not available for younger children in the 1985 dataset.
Substantial increases in the prevalence of overweight and obesity were observed in 7–11 year old children (9–13 years in 2007 survey) across 1985, 1995, and 2007 in boys and girls. Increases were also seen across this 12 year period in 12–15 year old girls (14–16 year olds in 2007), although for boys substantial increases in overweight and obesity prevalence observed between 1985 and 1995 did not appear to continue, with suggestion of a plateau between 1995 and 2007.
While differences in study methodologies and sample representativeness between the four national surveys makes conclusions on secular trends in national overweight and obesity prevalence difficult, it is clear that the prevalence of overweight and obesity in Australian children and adolescents has increased over recent decades.
New Zealand
Data on the prevalence of overweight and obesity in New Zealand children are available from two recent nationally representative samples; the 2002 national Children’s Nutrition Survey (Ministry of Health 2003) and the 2006/2007 New Zealand Health Survey (Ministry of Health 2008). Although only 22% of New Zealand children identify as Maori and 10% as Pacific Islanders (Statistics New Zealand 2002), these groups were over-sampled in both surveys to ensure that robust national estimates could be obtained for key outcomes (Ministry of Health 2008). The Children’s Nutrition Survey used a two-stage sampling frame to recruit approximately equal numbers of children aged 5–14 years into each of three main ethnic groups: Maori, Pacific, and New Zealand European & Others, and trained interviewers completed all anthropometric measurements at school. The New Zealand Health Survey used a multi-stage, stratified, probability proportionate to size design to recruit children aged 2–14 years, through home visits. In this latter survey, Asian peoples were included as a separate fourth ethnic group, due to recent rapid increases in this sector of the New Zealand population. Ethnicity was self-reported in both samples, using national Census questions.
Table 7.7 reports the prevalence of overweight and obesity according to age and sex from the more recent New Zealand Health Survey (Ministry of Health 2008). Overall, one in five children were overweight (21%) and a further one in twelve (8%) were obese. Sexual dimorphism in the prevalence of overweight or obesity was not apparent, with no sex differences in prevalence, adjusted for age.
Marked differences in the prevalence of overweight and obesity were apparent by ethnic group (Table 7.8). Approximately one in twenty Asian or European/other children were obese, whereas obesity was considerably more common in Maori (12%) and especially Pacific (23%) children. Comparable patterns were observed in the prevalence of overweight. One in six Asian and one in five European/other children had BMI (body mass index) values indicating that they were overweight, compared with one in four Maori and as many as one in three Pacific children. Standardized rate ratios indicate that Pacific children were greater than 2.5 times more likely to be obese than the total population, and Maori children approximately 1.5 times more likely (Ministry of Health 2008). By contrast, Asian (0.71) and European/other (0.67) children were less likely to be obese than the total population of children aged 2–14 years.
These ethnic disparities are even more marked when investigating the prevalence of extreme obesity, defined as a BMI greater than the 99th age and sex-specific percentile of US reference data (Kuczmarski et al. 2000). Based on the Children’s Nutrition Survey data of children aged 5–14 years (Ministry of Health 2003), 10% of Pacific females and 11% of Pacific males had extreme obesity (Goulding et al. 2007). While the level of extreme obesity was still of concern in Maori children (4% in girls, 6% in boys), equating to another 6,000 children nationwide, the prevalence was considerably reduced compared with Pacific youth. Finally, extreme obesity was rare in New Zealand European & Other children, being less than 1% in both sexes (Goulding et al. 2007).
Social class is related to obesity in New Zealand children (Ministry of Health 2008), as measured using the New Zealand Deprivation Index (NZDep2006) (Salmond et al. 2007). NZDep2006 shows a graduated scale of deprivation based on variables that reflect eight types of deprivation (including income, home ownership, family support, employment, qualifications and transport). A score of one represents the least deprived 10% of areas (rather than individuals) while ten is given to the most deprived 10% of areas (Salmond et al. 2007). Data from the 2006/2007 New Zealand Health Survey show that children living in areas of high neighborhood deprivation (NZDep2006 quintile 5) were significantly more likely (P < 0.05) to be obese than children living in all other areas (quintiles 1–4), in both sexes. Fourteen percent of boys and 16% of girls in the most deprived quintile were obese compared with 5–6% of children in the least deprived areas (adjusted for age). It is difficult to tease out the relative influence of ethnicity and deprivation in these statistics, given that children from the ethnic minorities are over represented in the more deprived areas (Table 7.9).
Little data are available examining the links between behavioral indicators of energy balance and overweight in nationally representative samples of New Zealand children. Analyses utilizing the Children’s Nutrition Survey data (Ministry of Health 2003) have investigated several potential dietary and lifestyle determinants of body weight in children aged 5–14 years (Utter et al. 2007). After controlling for demographics, mean BMI was significantly higher in children who had higher sweet beverage intakes (P = 0.03), those who bought school food from the dairy/takeaway shops more often (P = 0.02), and in children who skipped breakfast (P < 0.01). Similarly, increased television viewing (P = 0.02) or decreased participation in physical activity (P = 0.04) were associated with higher BMI values. After controlling for all other behaviors in the model, only buying school food from the dairy/takeaway shops and skipping breakfast remained significantly associated with BMI.
Secular Trends
It is widely acknowledged that the prevalence of obesity has increased dramatically in children throughout the world over the past 10 to 20 years (Lobstein et al. 2004). Suitable data are not available within New Zealand to inform discussions regarding secular trends prior to the first national survey in children in 2002 (Ministry of Health 2003). By this time much of the increase in prevalence in overweight and obesity had already been observed internationally (see remaining chapters in Part I of this book). Examination of our two national prevalence surveys (Ministry of Health 2003, 2008) demonstrates that the prevalence of obesity in children did not change between 2002 and 2006/2007 in either sex; 8% of boys aged 5–14 years were classified as obese at both time points, whereas in girls, 10% were obese in 2002 compared with 9% in the latest survey (Table 7.10).
Pacific Region
The capacity to report the prevalence of overweight and obesity in children and adolescents in the Pacific countries is very limited, with data only available for Fiji and Tonga. These data were collected as part of the Obesity Prevention In Communities project (OPIC) commenced in 2005 (Utter et al. 2008). The primary aim of the OPIC study is to evaluate the effectiveness of community-based obesity prevention strategies at sites in Fiji, Tonga, New Zealand and Australia. It uses a quasi-experimental study design to compare secondary school students attending schools in intervention areas with students at comparison schools in control areas and thus these data are not necessarily representative of the entire adolescent population.
Height, weight and waist circumference data were collected from children and adolescents in 2005/2006 for the OPIC study. Measurements were taken by trained assessors during face-to-face interviews at the children’s schools.
Findings from the 2005/2006 Obesity Prevention in Communities Study for Fiji
Fiji, in contrast to Tonga, is an ethnically heterogeneous community with two distinct ethnic groups, indigenous Fijians and Indo-Fijians, comprising the bulk of the population. Reflecting this, 43% of students identified their ethnicity as indigenous and 52% as Indo-Fijian. Five percent of students identified their ethnicity as “other”.
As shown in Table 7.11, ethnic differences in the prevalence of overweight and obesity were observed in Fiji with the indigenous students being most likely to be overweight and obese (22% of boys and 39% of girls), while the Indo-Fijian students were least likely to classified as overweight or obese (13% of boys and 13% of girls). Few differences in obesity by sex were observed.
While more than three-quarters of students in Fiji (89% boys; 76% girls) had a waist-to-height ratio within the healthy range (<0.5), this did differ by ethnicity with 67% of indigenous Fijian females and 93% of indigenous Fijian males having waist-to-height ratios less than 0.5 compared to 83% of Indo-Fijian females and 87% of Indo-Fijian males.
Findings from the 2005/2006 Obesity Prevention in Communities Study for Tonga
Approximately 10% of students in Tonga were classified as obese (Table 7.11). However, the prevalence of obesity was significantly higher among girls (15%) than boys (7%). This increased prevalence in girls was also pronounced in the figures for overweight with 38% of girls and 24% of boys classified as overweight.
Assessments of waist-to-height ratios for Tongan students showed that around half of all girls had ratios greater than 0.5 (unhealthy). In contrast, the prevalence in boys was substantially lower with 15% of boys falling into the unhealthy category.
Secular Trends
No secular data on overweight and obesity prevalence are available for any of the Pacific countries.
Conclusions
Overweight and obesity is commonly observed in children and adolescents in Australia, New Zealand and the Pacific region, with the prevalence being higher amongst children and adolescents in the Pacific region and of Pacific descent living in New Zealand. There is evidence of secular increases in overweight and obesity in children and adolescents in Australia, however, the available data are sparse. National surveys for New Zealand do not suggest secular increases in the prevalence of overweight and obesity in children in that country. While New Zealand regularly collects data on overweight and obesity prevalence through their national health survey, Australia does not have regular, frequent, national data collections to monitor rates of overweight and obesity. Further while both Australia and New Zealand collect national data on potential risk factors for the development of overweight and obesity including diet and physical activity, such data are generally not collected in conjunction with weight status data in Australia. In New Zealand, while potential risk factor data are collected they have not been analyzed in conjunction with weight status data, precluding conclusions about associations. What can be elicited from the available data is that overweight and obesity are likely to be socio-economically patterned, with children and adolescents from lower socio-economic families more likely to be overweight or obese. Further, there are distinct ethnic disparities in the prevalence of overweight and obesity in New Zealand children and adolescents. Those of Maori and Pacific descent are not only substantially more likely to be overweight or obese, but also tend to represent the more severe cases of excess weight, with extreme obesity experienced almost exclusively by Maori and Pacific youth.
Data for the Pacific region is almost non-existent. No nationally representative data are available and no data were identified for the majority of countries making up the Pacific region. Given the countries grouped within the Pacific region are heterogeneous in terms of geographic, social and economic circumstances, data from one country within this region may not accurately reflect the picture of childhood overweight and obesity in the entire region. Children and adolescents of Pacific descent living in New Zealand have been identified as being of particularly high risk for overweight and obesity. Thus data on indigenous Pacific children and adolescents is important as it may assist in explaining the reasons for this increased risk.
In conclusion, the data summarized in this chapter highlight the need for regular and frequent collections of nationally representative data on the prevalence and associated risk factors of overweight and obesity in children and adolescents in this region. This information is vital for understanding the epidemiology of overweight and obesity in this region. It is also imperative to inform national planning for prevention and treatment strategies.
References
Ashwell, M., & Hsieh, S.D. (2005). Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health risks of obesity and how its use could simplify the international public health message on obesity. International Journal of Food Science & Nutrition, 56(5), 303–307.
Australian Bureau of Statistics (2005). Population by age and sex, Australia (September 5, 2008); http://www.abs.gov.au/ausstats/abs@.nsf/productsbytitle/1F51406DCEEBAC14CA256EC7007B5B4E?OpenDocument.
Australian Bureau of Statistics (2006). A picture of the nation: the statistician’s report on the 2006 census. Catalogue No. 2070.0.
Australian Bureau of Statistics (2009). National Health Survey 2007-2008. Catalogue No. 4364.0.
Central Intelligence Agency (2009). The world factbook. (August, 2009); https://www.cia.gov/library/publications/the-world-factbook/index.html.
Cole, T.J., Bellizzi, M.C., Flegal, K.M., & Dietz, W.H. (2000). Establishing a standard definition for child overweight and obesity worldwide: international survey. British Medical Journal, 320(7244), 1240–1243.
Commonwealth of Australia (2008). 2007 Australian National Children’s Nutrition and Physical Activity Survey: Main findings, Commonwealth of Australia.
Fiji Islands Bureau of Statistics (2007). 2007 census of population and housing. (August 2009); http://www.statsfiji.gov.fj/Census2007.
Goulding, A., Grant, A.M., Taylor, R.W., Williams, S.M., Parnell, W.R., Wilson, N., & Mann, J.I. (2007). Ethnic differences in extreme obesity. Journal of Pediatrics, 151, 542–544.
Kuczmarski, R.J., Ogden, C.L., Grummer-Strawn, L.M., Flegal, K.M., Guo, S.S., Wei, R., Mei, Z., Curtin, L.R., Roche, A.F., & Johnson, C.L. (2000). CDC growth charts: United States. Advance data from Vital and Health Statistics: n. 314. Hyattsville, Maryland: National Center for Health Statistics.
Lobstein, T., Baur, L., & Uauy, R. for the IASO International Obesity Taskforce (2004). Obesity in children and young people: a crisis in public health. Obesity Reviews, 5(Suppl 1), 4–85.
Ministry of Health (2003). NZ Food NZ Children: Key results of the 2002 National Children’s Nutrition Survey. Wellington, New Zealand.
Ministry of Health (2008). A Portrait of Health: Key results of the 2006/07 New Zealand Health Survey. Wellington, New Zealand.
Salmond, C., Crampton, P., & Atkinson, H. (2007). NZDep2006 Index of Deprivation. Wellington, New Zealand: Department of Public Health, University of Otago.
Secretariat of the Pacific Community Noumea New Caledonia (1999). Cook Islands Population Profile Based on 1996 Census: a guide for planners and policy-makers.
Soloff, C., Lawrence, D., & Johnstone, R. (2005). The Longitudinal Study of Australian Children (LSAC). Sample design. LSAC Technical Paper No. 1, Australian Institute of Family Studies.
Statistics New Zealand (2002). 2001 census of population and dwellings; population and dwelling statistics. Wellington, New Zealand.
Statistics New Zealand (2006). QuickStats about New Zealand’s population and dewllings-population counts. (May 18, 2007); http://www.stats.govt.nz/Census/2006CensusHomePage/QuickStats/quickstats-about-a-subject/nzs-population-and-dwellings/population-counts.aspx.
The World Bank (2009). Pacific Islands brief. (August, 2009); http://web.worldbank.org/WBSITE/EXTERNAL/COUNTRIES/EASTASIAPACIFICEXT/PACIFICISLANDSEXTN/0,,contentMDK:20212765∼menuPK:441895∼pagePK:1497618∼piPK:217854∼theSitePK:441883∼isCURL:Y,00.html.
Tonga Department of Statistics (2006). Tonga statistics population census 2006. Analytical Report Volume 2.
United Nations Development Programme (2009). Human development report 2009-HDI rankings. (December, 2009); http://hdr.undp.org/en/statistics/.
Utter, J., Scragg, R., Schaaf, D., Fitzgerald, E., & Wilson, N. (2007). Correlates of body mass index among a nationally representative sample of New Zealand children. International Journal of Pediatric Obesity, 2, 104–113.
Utter, J., Faeamani, G., Malakellis, M., Vanualailai, N., Kremer, P., Scragg, R., & Swinburn, B. (2008). Lifestyle and obesity in South Pacific youth: Baseline results from the Pacific Obesity Prevention in Communities (OPIC) project in New Zealand, Fiji, Tonga and Australia. Auckland, University of Auckland.
Vanuatu National Statistics Office (1999). Population statistics: population by ethnicity 1999. (June 26, 2009). http://www.spc.int/prism/country/vu/stats/social/population/ethnicity.htm.
Wake, M., Hardy, P., Canterford, L., Sawyer, M., & Carlin, J.B. (2007). Overweight, obesity and girth of Australian preschoolers: prevalence and socio-economic correlates. International Journal of Obesity, 31(7), 1044–1051.
World Health Organisation (2009). Regional office for the Western Pacific: Countries and areas. (August, 2009); http://www.wpro.who.int/countries/countries.htm.
Acknowledgments
Kylie Hesketh is supported by a National Heart Foundation of Australia Career Development Award. Karen Campbell is supported by a Victorian Health Promotion Foundation Fellowship. Rachael Taylor is supported by the Karitane Products Society Fellowship.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Hesketh, K., Campbell, K., Taylor, R. (2011). Epidemiology of Obesity in Children and Adolescents in Australia, New Zealand and the Pacific Region. In: Moreno, L., Pigeot, I., Ahrens, W. (eds) Epidemiology of Obesity in Children and Adolescents. Springer Series on Epidemiology and Public Health, vol 2. Springer, New York, NY. https://doi.org/10.1007/978-1-4419-6039-9_7
Download citation
DOI: https://doi.org/10.1007/978-1-4419-6039-9_7
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4419-6038-2
Online ISBN: 978-1-4419-6039-9
eBook Packages: MedicineMedicine (R0)