Abstract
Biomolecule-responsive hydrogels that exhibit volume changes in response to target biomolecules have become increasingly important because of their potential applications as smart biomaterials. Researchers are developing novel biomedical systems using glucose, proteins and other biomolecule-responsive hydrogels as biosensing systems for applications such as drug delivery and cell culture systems. In the synthesis of biomolecule-responsive hydrogels, both biomolecular recognition and responsive functions that perceive a target biomolecule and induce structural changes must be introduced into the hydrogels network. Many biomolecule-responsive hydrogels are prepared by combining structural designs of hydrogels networks with molecular recognition events of biomolecules, such as enzymes, lectins and antibodies. Most important is the need to synthesize and develop more biomolecule-responsive hydrogels in tandem with their biomedical applications so that the field continues to evolve.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Atom Transfer Radical Polymerization
- Atom Transfer Radical Polymerization
- Lower Critical Solution Temperature
- Gluconic Acid
- Phenylboronic Acid
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Hydrogels are attractive soft materials consisting of physically or chemically crosslinked polymer networks and large amounts of aqueous solutions. Since hydrogels have a variety of fascinating properties; swelling properties, mechanical properties, permeation properties, surface properties, and optical properties. They have been already utilized as adsorbents, chromatography columns, contact lenses, foods, and industrial materials [1–3]. In addition, some hydrogels have a unique property in that they undergo abrupt changes in their volume in response to environmental changes, such as pH and temperature [4–7]. Such unique hydrogels are named stimuli-responsive hydrogels, intelligent hydrogels or smart hydrogels. Stimuli-responsive hydrogels are fascinating materials for mimicking natural feedback systems because they can sense a stimulus as a signal and induce volume changes. Therefore, stimuli-responsive hydrogels are very suitable materials for designing smart systems in the biochemical and biomedical fields; they can be utilized as switches, sensors, actuators, bio-reactors, separation systems, drug delivery systems, and cell culture systems.
Many researchers have prepared various types of stimuli-responsive hydrogels that undergo volume changes in response to environmental changes such as pH [8, 9], temperature [10–14], electric field [15, 16], and light [17, 18]. The pH-responsive hydrogels are usually formed from polymers with carboxyl or amino groups that can carry charge in response to pH changes [19–24]. Some polymers have lower critical solution temperature (LCST), such as poly(N-alkylacrylamide), poly(vinyl methyl ether), poly(ethylene oxide)-poly(propylene oxide)-poly(ethylene oxide); they are unique polymers whose solubility in water changes drastically at their LCST. Hydrogels with these polymers as main chains exhibit abrupt volume changes in response to temperature [25–29]. These pH- and temperature-responsive hydrogels are effective biomaterials for constructing self-regulating drug delivery systems, cell culture systems, and diagnosic signals for monitoring physiological changes.
Most biosystems are closely associated with a natural feedback system, such as homeostasis. These natural feedback systems perceive specific ions or biological molecules like enzymes and hormones, and induce conformational changes that rearrange their constitutional biomolecules to elicit biological responses. For example, they respond to the presence of specific molecules as well as physicochemical and environmental changes like pH and temperature. Therefore, stimuli-responsive hydrogels that respond to specific biomolecules (biomolecule-responsive hydrogels) are required to develop self-regulating systems by mimicking natural feedback signals. Specific biomolecules, such as a tumor marker, give important signals for monitoring living biological systems and stimuli-responsive hydrogels that can recognize these target biomolecules are very useful for fabricating molecular diagnostics systems and self-regulating drug delivery systems. For example, the stimuli-responsive hydrogels that undergo volume changes in response to blood glucose concentrations can self-regulate insulin delivery in the amount of insulin necessary. There are several biomolecule-responsive hydrogels that exhibit swelling/shrinking changes in response to target biomolecules and so provide the potential for many bioapplications, such as smart devices in sensing systems and molecular diagnostics [30, 31].
Glucose-Responsive Hydrogels
Insulin, which is secreted from the Islets of Langerhans of the pancreas, controls glucose metabolism. The inability of the pancreas to control blood glucose concentrations is the cause of diabetes. To treat diabetes, specific amounts of insulin are administered along with close monitoring of the blood glucose concentration. Consequently, glucose-responsive hydrogels are attractive candidates as an artificial pancreas to control the administration of insulin in response to the blood glucose levels. A typical glucose-responsive insulin release system is illustrated in Fig. 1. Currently, there are three different types of strategies used for glucose-responsive hydrogels to self-regulate insulin release.
Glucose-Responsive Hydrogels Using Glucose Oxidase
The combination of an enzymatic reaction of glucose oxidase with the pH-responsive swelling/shrinking behavior of polyelectrolyte hydrogels is the most common approach. The glucose-responsive hydrogels regulate insulin release by changing the pH environment in response to the glucose levels in the blood; the pH-responsive hydrogels respond to the environmental changes, followed by swelling or shrinking accordingly to control the rate of insulin release.
Basically, the glucose oxidase-loaded hydrogels convert glucose to gluconic acid which lowers the pH within the hydrogel. The lower pH causes the pH-responsive hydrogels networks to be expanded and allow insulin to permeate into the blood through the networks; thus enabling self-regulated insulin release in response to the glucose concentration.
A glucose-responsive insulin release system using a copolymer of N,N-diethylaminoethyl methacrylate (DEA) and 2-hydroxypropyl methacrylate (HPMA) as the pH-responsive polymer was reported, in which glucose oxidase was loaded in a DEA–HPMA composite membrane to sense glucose [32]. The presence of glucose enhanced the insulin permeability through the glucose oxidase-loaded DEA–HPMA copolymer membranes (Fig. 2). As the glucose diffuses into the copolymer membranes, it is converted to gluconic acid by the glucose oxidase; the gluconic acid decreases the pH and induces the copolymer membranes to swell and to release insulin. In addition, glucose-responsive polymer capsules containing insulin were prepared by a conventional interfacial precipitation [33]. The steady-state behavior of the glucose-responsive hydrogels membrane prepared by entrapping the glucose oxidase within the DEA-hydroxyethyl methacrylate copolymer matrix was investigated from both theoretical and experimental view points [34–36].
Permeation profile of insulin through a glucose-responsive polymer membrane consisting of a poly(amine) and glucose oxidase-immobilized hydrogels. Glucose concentration: (filled triangle) 0 M; (filled circle) 0.1 M; (open circle) 0.2 M; (open triangle) 0.2M without glucose oxidase [32].
The complex formed between methacrylic acid (MAAc) and ethylene glycol (EG) was utilized to form a pH-responsive hydrogels network to prepare glucose-responsive hydrogels [37, 38]. The poly(MAAc-EG) hydrogel’s pH-responsive swelling/shrinking behavior responded to the pH changes elicited by the gluconic acid generated based on the amount of glucose converted by the glucose oxidase. The swelling of the glucose oxidase-loaded hydrogels at high glucose (hyperglycemic conditions) was greater than at low glucose concentrations.
Glucose-Responsive Hydrogels Using Phenylboronic Acid
Phenylboronic acid and its derivatives recognize glucose as they form complexes with polyol compounds. These complexes are dissociated in the presence of competing polyol compounds that have a stronger affinity for phenylboronic acid. Totally synthetic hydrogels with glucose-responsivity were prepared based on the complex that forms between phenylboronic acid and a polyol compound. For example, a complex readily forms between poly(vinyl alcohol) (PVA) and a copolymer of N-vinyl-2-pyrrolidone (NVP) and 3-(acrylamide)phenylboronic acid (PBA). A glucose-responsive insulin delivery system was derived by using the complex formation between PVA and poly(NVP-co-PBA), which dissociates in the presence of free glucose [39, 40].
The strategy involved combining the glucose recognition function of phenylboronic acid with temperature-responsive PNIPAAm to form glucose-responsive hydrogels. The dissociation of phenylboronic acid moiety is in equilibrium between the uncharged (nonionic) and the charged (ionic) form (Fig. 3); since glucose forms a complex with the charged phenylboronic acid more readily than with the uncharged form, the presence of glucose leads to an increase in charged form and a decrease in uncharged form due to a shift in the dissociation equilibrium of the phenylboronic acid. Therefore, the solubility of PNIPAAm copolymers with phenylboronic acid groups is greatly enhanced by the presence of glucose due to a shift in the LCST by increasing number of charges. For example, LCST of the copolymer of NIPAAm and 3-(acrylamido)phenylboronic acid (APBA) is shifted to a higher temperature in the presence of free glucose, based on the shift in the dissociation equilibrium of phenylboronic acid due to complex formations with glucose [41].
Temperature dependence of swelling curves for PNIPAAm copolymer hydrogels with phenylboronic acid moieties at different glucose concentrations [42].
Some glucose-responsive insulin release systems focus on glucose-responsive LCST changes of PNIPAAm copolymer with phenylboronic acid. Totally synthetic hydrogels showing glucose-responsive volume changes were prepared by copolymerization of NIPAAm and monomeric phenylboronic acid [42, 43]. The LCST of these NIPAAm–APBA hydrogels in the presence of free glucose was higher than that in its absence (Fig. 3). Therefore, the NIPAAm–APBA hydrogels swell in response to free glucose at a constant temperature between LCSTs in the presence and absence of glucose. Insulin was not released from the hydrogels in a buffer solution without glucose but a remarkable insulin release took place for the hydrogels immersed in a solution with glucose. Repeated on–off release of insulin on changing the concentration of external glucose was achieved by using the NIPAAm–APBA hydrogels (Fig. 4). In addition, the hydrogels that exhibit glucose-responsive swelling/shrinking changes under physiological conditions (pH and temperature) were prepared by copolymerizing an APBA derivative with a low pKa and a monomer with a higher LCST than that of PNIPAAm [44]. These results indicate that glucose-responsive hydrogels can be developed by combining the glucose recognition features of phenylboronic acid with the temperature-responsive behavior of PNIPAAm derivatives without any biological components, such as glucose oxidase.
Repeated on–off release of FITC-insulin from the glucose-responsive hydrogels at 28°C, pH 9.0, in response to external glucose concentration [42].
Glucose-Responsive Hydrogels Using Lectin
Lectins are carbohydrate-binding proteins that form complexes with carbohydrate chains of glycoproteins and glycolipids on the cell surface. Lectins are used to fabricate sensing systems based on this unique property of carbohydrate recognition. For example, glucose-responsive insulin systems control the release of glycosylated insulin by lectin-binding in response to free glucose using the competitive and complementary binding properties of glycosylated insulin and glucose to lectins [45–48].
Saccharide-responsive hydrogels are prepared by combining the carbohydrate-binding ability of concanavalin A (Con.A), which is a lectin that recognizes glucose and mannose, with temperature-responsive PNIPAAm [49]. The LCST of the Con.A-loaded PNIPAAm hydrogels is shifted by complex formation between Con.A and the ionic saccharide, dextran sulfate. The Con.A-loaded PNIPAAm hydrogels swells dramatically in the presence of the ionic saccharide dextran sulfate because the LCST is increased by incorporating ionized saccharide in the hydrogels. The hydrogels collapses to its native volume by replacing the ionic saccharide dextran sulfate with the nonionic saccharide. Thus, the Con.A-loaded PNIPAAm hydrogels can undergo abrupt volume changes in response to ionized saccharide based on the combination of carbohydrate-binding property of Con.A with the temperature-responsive property of PNIPAAm.
Some polymers modified with pendant saccharides have been synthesized as potential biomaterials for biochemical and biomedical applications [50]. These pendant-saccharide polymers form complexes with lectins but the complexes are inhibited by the presence of saccharide which has a stronger affinity for lectin. For example, the competitive and complementary binding properties of poly(2-glucosyloxyethyl methacrylate) (PGEMA) as a pendant glucose polymer was investigated using Con.A as a lectin [51]. PGEMA formed a complex with Con.A but the resulting PGEMA–Con.A complex dissociated in the presence of free glucose and mannose. Since Con.A forms a complex with glucose and mannose but not with galactose, the PGEMA–Con.A complex does not dissociate in the presence of free galactose. This monosaccharide-responsive behavior of the PGEMA–Con.A complex is useful in fabricating glucose-responsive hydrogels.
Researchers have developed glucose-responsive hydrogels that undergo volume changes in response to glucose concentration by using complexes between lectins and polymer with pendant glucose as reversible crosslinks in their networks. For example, glucose-responsive hydrogels were prepared by copolymerization of a monomer with a pendant glucose (GEMA) and N,N′-methylenebisacrylamide (MBAA) after the formation of GEMA–Con.A complex that acted as reversible crosslinks in the networks [52]. The Con.A-entrapped PGEMA hydrogels swelled immediately in a buffer solution containing free glucose and mannose, but did not change volume in a solution containing galactose (Fig. 5). The compressive modulus measurements demonstrated that crosslinking density of the Con.A-entrapped PGEMA hydrogels decreased with increasing glucose concentration in a buffer solution. Therefore, the glucose-responsive swelling behavior of the Con.A-entrapped PGEMA hydrogels is attributed to the dissociation of the complex between Con.A and pendant glucose on GEMA that played an important role as reversible crosslinks (Fig. 6). Con.A has a stronger affinity for mannose than glucose and does not have any for galactose. Therefore, the presence of free mannose and glucose induced the dissociation of PGEMA–Con.A complex by competitive complex exchange, while free galactose does not. As a result, the Con.A-entrapped PGEMA hydrogels swell remarkably more in the presence of mannose and glucose as they decrease the crosslinking density, but do not change in the presence of galactose.
Swelling ratio changes of PGEMA–Con.A hydrogels as a function of time, when the hydrogels was immersed in a buffer solution containing 1 wt% of monosaccharide: (open circle), glucose; (filled square), mannose; (filled circle) galactose [52].
Schematic representation of glucose-responsive swelling changes of the PGEMA–Con.A hydrogels [52].
To obtain reversible glucose-responsive hydrogels that swell in the presence of free glucose and shrink in its absence, Con.A-copolymerized PGEMA hydrogels were prepared by copolymerizing GEMA with chemically vinyl-modified Con.A [53]. The Con.A-copolymerized PGEMA hydrogels exhibited reversible volume changes in response to stepwise changes in glucose concentration but the Con.A-entrapment hydrogels did not change. The Con.A-entrapment hydrogels did not shrink in the absence of free glucose because the Con.A had leaked out of the hydrogels during the swelling in the presence of free glucose. However, since Con.A in the Con.A-copolymerized PGEMA hydrogels was covalently immobilized in the hydrogels networks, the hydrogels shrank in the absence of glucose due to repeated complex formation between Con.A and pendant glucose on PGEMA.
Sol–gel phase transitions responding to changes in the environmental glucose concentrations were also achieved based on the complex formation between a polymer with pendant glucose and Con.A [54, 55]. The addition of Con.A induced the gelation of aqueous solutions containing a polymer with pendant glucose, such as vinylpyrrolidinone-allylglucose or acrylamide-allylglucose copolymers, and the sol–gel phase transition obtained was strongly dependent upon glucose concentration in the solution. The releases of lysozyme and insulin as model protein drugs were controlled by sol–gel phase transition based on the complex formation between the polymer with pendant glucose and Con.A [56]. The glucose-responsive hydrogels regulated the release of model drugs in response to the glucose concentration. Thus, smart systems, such as self-regulated drug release systems that regulate insulin release in response to environmental glucose concentration, can be fabricated by using the complex formation and dissociation between Con.A and polymers with pendant glucose groups.
Protein-Responsive Hydrogels
Enzyme-Responsive Hydrogels
Some enzymes give important diagnostic signals for several physiological changes. Enzymes located in specific areas of the body can also provide signals for site-specific drug delivery. Therefore, enzyme-responsive hydrogels that undergo changes triggered by selective enzyme catalysis can be utilized as smart materials to monitor physiological changes or direct drugs to a specific site. In order to develop enzyme-responsive hydrogels, some researchers have focused on enzymatic activity followed by structural changes of hydrogels networks [57]. Biodegradable polymers are promising candidates for preparing enzyme-responsive hydrogels since they are degraded by specific enzymes.
The microbial enzymes localized predominantly in the colon have been used as promising markers for drug delivery to the colon. Colon-specific drug is conjugated via azoaromatic bonds to construct the delivery systems since these bonds are degraded by azoreductase, an enzyme produced by the microbial flora of the colon, to release the drug [58–63]. The copolymer hydrogels, prepared with acrylamide derivatives, acrylic acid and crosslinker with azoaromatic bonds, swell at high pH and shrink at low pH; protein drugs loaded in this hydrogels are protected against digestion by proteolytic enzymes in the stomach (low pH). In the colon, azoreductase is accessible to the azoaromatic crosslinks due to swelling of the hydrogels and to degrade the hydrogels networks to release drug release.
Dextranases are microbial enzymes that exist in the colon; as smart biomaterials for achieving colon-specific drug delivery, dextranase-responsive hydrogels were prepared by crosslinking of dextran with diisocyanate [64]. These dextran hydrogels were degraded in vitro (in a human colonic fermentation model) and in vivo (in rats).
Tetrapeptide sequence, Cys-Tyr-Lys-Cys, as a crosslinker was used to create poly(acrylamide) hydrogels that degrade when subjected to α-chymotrypsin [65]. The chemoselective conjugations of methacrylamide containing peptides were made for more advanced protease-responsive hydrogels applications. A new type of disulfide-based thermo-responsive triblock copolymer was also synthesized by atom transfer radical polymerization (ATRP) of 2-(methacryloyloxy)ethyl phosphorylcholine (MPC) and NIPAAm using the disulfide-based initiator [66]. The cleavage of the central disulfide bond induced irreversible dissolution of the micellar gels.
Monitoring two or more enzymes simultaneously to sense physiological changes would allow clinical screening for several diseases at the same time. Dual-stimuli-responsive hydrogels, which degrade in the presence of two enzymes, papain and dextranase, were prepared as an interpenetrating polymer network (IPN) hydrogels of oligopeptide-terminated poly(ethylene glycol) (PEG) and dextran that can be degraded by papain and dextranase, respectively [67, 68]. The presence of both papain and dextranase induced the degradation of the PEG/dextran IPN hydrogels, but the presence of one of the two enzymes did not result in degradation (Fig. 7). Furthermore, the gelatin/dextran IPN hydrogels released lipid microspheres in the presence of both α-chymotrypsin and dextranase but did not in the presence of either enzyme alone (Fig. 8). Dual-stimuli-responsive hydrogels that degrade in the presence of a specific enzyme within a certain temperature range were also prepared by combining PNIPAAm temperature responsiveness with enzymatic biodegradation [69, 70]. The temperature-responsive biodegradation of the hydrogels was based on the effect of network structural changes, caused by PNIPAAm temperature responsiveness, on the formation of the enzyme-substrate complex.
Concept of dual-stimuli-responsive drug release by IPN-structured hydrogels [68].
Lipid microsphere release from gelatin/dextran IPN hydrogels in phosphate buffer at 37°C. Open circle, 5 U/ml α-chymotrypsin + 0.5 U/ml dextranase; open triangle, 5 U/ml α-chymotrypsin; open square, 0.5 U/ml dextranase [68].
A enzyme-responsive hydrogels formation was achieved by crosslinking functionalized PEG and a lysine-containing polypeptide through the action of transglutaminase (TGase) that catalyzes an acyl-transfer reaction between the γ-carboxamide of protein-bound glutaminyl residues and the ε-amino group of Lys residues [71, 72]. Short peptide substrates of TGase provide enzyme-responsive gelation of polymer-peptide conjugates within the few minutes, which is for many medical applications.
Chemically crosslinked polyethylene glycol acrylamide hydrogels that are enzyme-responsive and swell/collapse in response to specific proteases are very interesting [73]. These enzyme-responsive hydrogels are programmable to respond uniquely to target enzymes by selection of appropriate enzyme cleavable linkers. Enzyme-responsive hydrogels that exhibited selective, enzyme-triggered, charge-induced polymer swelling were prepared to release dextran and protein from the hydrogels [74] (Fig. 9). The enzyme-responsive hydrogels, with the zwitterionic peptide linkers that are hydrolyzed by specific enzyme, swelled due to doubly charged peptide fragments produced by the enzymatic hydrolysis. These enzyme-responsive hydrogels have applications in selective therapeutic release at specifically targeted enzyme locations.
Schematic representation of selective enzyme-triggered charge-induced swelling of the enzyme-responsive hydrogels with the zwitterionic peptide linkers that are hydrolyzed by specific enzyme [74].
Antigen-Responsive Hydrogels
An antibody recognizes a specific antigen and forms an antigen–antibody binding through multiple noncovalent bonds, such as electrostatic, hydrogen, hydrophobic, and van der Waals interactions. The specificity and versatility of antibodies provide the basis for immunological assays to detect and signal physiological changes to specific biomolecules [75]. Antigen-responsive hydrogels were prepared to recognize a target antigen and induce the volume changes of the hydrogels.
The first antigen-responsive hydrogels were designed to swell in response to a target antigen. Using rabbit IgG as the antigen and goat anti-rabbit IgG (GAR IgG) as the antibody, an antigen–antibody binding hydrogels network was constructed with reversible crosslinks. The antigen–antibody entrapped hydrogels were prepared by copolymerizing rabbit IgG with polymerizable groups, acrylamide (AAm) and N,N′-methylenebisacrylamide (MBAA) in the presence of GAR IgG, whose antigen–antibody binding form crosslinks [76]. The antigen–antibody entrapped hydrogels swell in a buffer solution containing rabbit IgG as a target antigen and the swelling ratio is directly dependent upon the antigen concentration of the buffer solution.
The application of stimuli-responsive hydrogels requires reversible behavior in response to environmental stimuli changes. Therefore, reversibly antigen-responsive hydrogels that undergo reversible swelling/shrinking changes in response to a target antigen were developed by forming a semi-interpenetrating polymer network (semi-IPN) composed of linear PAAm grafted with antibodies (GAR IgG) and PAAm networks grafted with antigen (rabbit IgG). The complexes that form between the grafted antibodies and grafted antigens act as reversible crosslinks (Fig. 10) [77]. The antigen–antibody semi-IPN hydrogels, in the presence of rabbit IgG as a target antigen in a buffer solution, drastically increase their swelling ratio but do not change their swelling ratio in the presence of goat IgG. Furthermore, the antigen–antibody semi-IPN hydrogels swell immediately in the presence of rabbit IgG and shrank in its absence, when their hydrogels were immersed in a buffer solution with and without rabbit IgG (Fig. 11). These reversible antigen-responsive volume changes are due to reversible changes in the crosslinking density caused by the formation and dissociation of the binding between grafted antigen and grafted antibody in the absence and presence of a free antigen, respectively (Fig. 10b). These results suggest that the antigen–antibody semi-IPN hydrogels can recognize only rabbit IgG and induce reversibly responsive volume change.
Schematic representation of the preparation (a) and responsive behavior (b) of an antigen-responsive hydrogels with a semi-IPN structure [77].
Reversible swelling changes and antigen-responsive permeation profiles of hemoglobin, through the PAAm semi-IPN hydrogels (open circle) and the antigen–antibody semi-IPN hydrogels (filled circle) in response to stepwise changes in the antigen concentration between 0 and 4 mg/ml [77].
Biomolecule-responsive hydrogels are used for self-regulated drug delivery systems in which drugs are administered in response to specific physiological changes. Antigen-responsive drug release systems were constructed using antigen–antibody semi-IPN hydrogels as smart devices for self-regulated drug delivery [77]. The drug permeates through the antigen–antibody semi-IPN hydrogels in the presence of a target antigen but not in its absence (Fig. 11). The antigen–antibody semi-IPN hydrogels controls drug permeation in response to changes in the target antigen concentration. Thus, reversibly antigen-responsive hydrogels are effective as smart devices to modulate drug release in response to a specific antigen and physiological changes.
Antigen-responsive hydrogels were prepared by the copolymerization of functionalized antibody Fab’ fragments with NIPAAm and MBAA [78]. The PNIPAAm hydrogels with Fab’ fragments undergo reversible volume changes in alternative incubations with hydrophobic fluorescein and hydrophilic dendrimer-modified fluorescein as target antigens in a buffer solution. The antigen-responsive swelling/shrinking behavior of the PNIPAAm hydrogels with Fab’ fragments was attributed to drastic changes in hydrophilicity of PNIPAAm-based networks by the exchange of Fab’ fragment binding between hydrophobic and hydrophilic antigen.
Stimuli-responsive hydrogels microparticles were fabricated as dynamically tunable microlens array using antigen-responsive microlenses, prepared from antigen–antibody bonded microparticles [79–82]. A coulombic assembly of the NIPAAm-AAc hydrogels microparticles was fabricated on a glass substrate after being conjugated with biotin to bind antigen and aminobenzophenone. The antigen-responsive hydrogels microlenses, constructed by using a simple bright field optical microscopic technique, exhibit a difference in appearance in the differential interference contrast (DIC) images in response to a target antigen. These antigen-responsive hydrogels microlens constructs may have applications as a label-free biosensing/bioassay of protein and small molecules.
Other Biomolecule-Responsive Hydrogels
Molecularly Imprinted Hydrogels
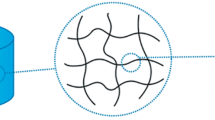
Enzymes and antibodies can recognize specific substrate based on fitting guest molecules into molecular cavity. Molecular imprinting is a technique to make biomimetic polymers with molecular cavity as recognition sites [83–89]. After monomers are prearranged around a print molecule by noncovalent interactions and then polymerized, the print molecule is removed from the resulting polymer for leaving a molecular cavity as a recognition site (Fig. 12). The molecularly imprinted polymer can recognize the guest molecule (print molecule) on the basis of a combination of reversible binding and shape complementarity of the cavity. Molecular imprinting is also used to create molecular recognition sites in stimuli-responsive hydrogels.
Temperature-responsive hydrogels consisting of NIPAAm and AAc were prepared in the presence of norephedrine as the print molecule by molecular imprinting [90]. These norephedrine-imprinted hydrogels do not change in the presence of norephedrine when the hydrogels are in the swollen state at a low temperature. However, in the collapsed state at a high temperature, the hydrogels swell gradually with increasing norephedrine concentration but do not with increasing adrenaline concentration (Fig. 13). The norephedrine-responsive swelling behavior of the norephedrine-imprinted hydrogels is due to a shift of LCST by the binding of norephedrine with its recognition site created by molecular imprinting. Other studies revealed that temperature-responsive hydrogels prepared by molecular imprinting can memorize the print molecule in their collapsed states and that undergo their specific volume change in response to the guest molecule [91, 92].
Equilibrium swelling ratios at 50°C as a function of concentration of either norephedrine (filled circle) or adrenaline (open circle) in water for molecular recognition hydrogels prepared in the presence of norephedrine (a) and adrenaline (b) [90].
In molecular imprinting, low-molecular-weight monomers with a functional group, such as acrylic acid, are used as ligand monomers for the print molecule. Most molecular imprinting requires a large amount of crosslinkers to fix the structure of the molecular cavity for the print molecule. However, biomolecules such as lectin and antibody can be utilized as ligands for a print biomolecule with minute amounts of crosslinkers that enable structural changes in response to a target biomolecule.
α-Fetoprotein (AFP) is a tumor-specific marker glycoprotein widely used for the serum diagnosis of primary hepatoma. To prepare tumor marker-responsive hydrogels in biomolecular imprinting, lectins and antibodies were used as ligands for saccharide and peptide chains of AFP as a print biomolecule, respectively (Fig. 14) [93]. After synthesis of poly(acrylamide) (PAAm)-grafted lectins and acryloyl-antibody, AAm as a main monomer was copolymerized with MBAA as a chemical crosslinker and acryloyl-antibody in the presence of print AFP and PAAm-grafted lectins to form lectin–AFP–antibody complexes. The AFP-imprinted hydrogels were then prepared by removing the print AFP from the resultant networks having lectin–AFP–antibody complexes. The AFP-imprinted hydrogels began to shrink as soon as they were immersed in a phosphate buffer solution containing AFP, but nonimprinted hydrogels prepared without using molecular imprinting experienced slight swelling and PAAm hydrogels exhibited no volume change. The fact that the swelling ratio of AFP-imprinted hydrogels depended on the AFP concentration in a buffer solution means that the hydrogels were tumor marker-responsive hydrogels. The compressive modulus measurements demonstrated that crosslinking density of the AFP-imprinted hydrogels increased gradually with increasing AFP concentration in a buffer solution, but those of the nonimprinted and PAAm hydrogels did not change at all. Biomolecular imprinting enabled the lectins and antibodies as ligands to be organized at optimal positions for the simultaneous recognition of AFP saccharide and peptide chains. Therefore, AFP-responsive shrinking of the AFP-imprinted hydrogels is due to the formation of the sandwich-like lectin–AFP–antibody complexes that played an important role as crosslinks.
Synthesis of tumor marker-responsive hydrogels using lectins and antibodies as ligands for print glycoprotein molecules (tumor-specific marker AFP) in biomolecular imprinting [93].
Glycoprotein recognition behavior by AFP-imprinted and nonimprinted hydrogels were investigated by measuring their swelling ratios in the presence of AFP or ovalbumin (Fig. 15). Ovalbumin has a saccharide chain similar to AFP, but has a peptide chain different from AFP. The swelling ratio of the nonimprinted hydrogels increased slightly in the presence of AFP and ovalbumin, but immediately shrank in the presence of AFP while swelling slightly in the presence of ovalbumin. These demonstrate that AFP-imprinted hydrogels only shrink when both lectins and antibodies in the hydrogels simultaneously recognize the saccharide and peptide chains of the target glycoprotein. Therefore, swelling or shrinking behaviors of AFP-imprinted hydrogels in the presence of glycoproteins enable the accurate detection and recognition of glycoproteins with a double-lock function. This fascinating behavior of biomolecule-imprinted hydrogels with the accurate detection and recognition of a tumor-specific marker glycoprotein indicates many future opportunities as smart biomaterials for fabricating novel sensor systems and molecular diagnostics.
Swelling ratio changes of nonimprinted hydrogels (a) and AFP-imprinted hydrogels (b) following the addition of AFP (open circle) and ovalbumin (filled circle) after their swelling had attained equilibrium in a phosphate buffer solution at 25°C [93].
Other Biomolecule-Responsive Hydrogels
In addition to glucose-responsive hydrogels and protein-responsive hydrogels, biomolecule-responsive hydrogels undergo structural changes in response to biomolecules such as cell surface receptors and antibiotic drugs as well as DNA. Assembly and erosion profiles of noncovalently associated hydrogels were produced by the interaction of a low-molecular-weight heparin-modified polyethylene glycol star polymer (PEG-LMWH) and a dimeric heparin-binding growth factor (VEGF) (Fig. 16) [94]. The addition of VEGF, which played a key role as a crosslinker, into a phosphate-buffered saline (PBS) of PEG-LMWH immediately formed hydrogels by the complex formation of PEG-LMWH and VEGF. However, selective removal of VEGF crosslinks in the presence of VEGF receptors induced receptor-mediated erosion of the PEG-LMWH/VEGF hydrogels. The VEGF release in response to cell surface receptors was achieved by the receptor-mediated erosion of the PEG-LMWH/VEGF hydrogels. Selective release of such growth factors from cell receptor-responsive hydrogels showed potential for use in vascular therapy.
Schematic representation of hydrogels formation by the crosslinking of heparin-modified star polymer by dimeric, heparin-binding growth factors, followed by receptor-mediated erosion [94].
Cell-responsive sol–gel transition systems, made by gelation of multiarmed PEG with an adhesion receptor-binding motif (an adhesion ligand based on the RGD peptide) by the addition of the bis-cysteine peptide crosslinker, are sequence sensitive to matrix metalloproteinases (MMPs), a protease family extensively involved in tissue development and remodeling (Fig. 17) [95, 96]. A Michael-type addition reaction between vinyl sulfone-functionalized multiarmed PEGs and mono-cysteine adhesion peptides or bis-cysteine MMP substrate peptides was used to form the cell-responsive hydrogels that were designed to locally respond to local protease activity such as MMP at the cell surface. The MMP-responsive hydrogels were proteolytically invaded by primary human fibroblasts and the invasion process depended on MMP substrate activity, adhesion ligand concentration, and network crosslinking density. When the MMP-responsive hydrogels were used to deliver recombinant human bone morphogenetic protein-2 to the site of critical defects in rat cranium, bone regeneration was dependent on the proteolytic responsive behavior of the hydrogels. These results indicate potential applications of the cell-responsive hydrogels in tissue engineering and regenerative medicine.
Cell-responsive sol–gel transition systems by gelation of multiarmed PEG with an adhesion receptor-binding motif by the addition of the bis-cysteine peptide crosslinker [95].
Some proteins undergo a substantial conformational change in response to a given stimulus. This conformational change of proteins has provided useful tools in engineering smart hydrogels with specified responses to particular stimuli. For example, smart hydrogels that undergo volume changes or sol–gel transition in response to pH and temperature were prepared by bioconjugation of well-defined folding motifs of proteins and synthetic polymers [97, 98]. Similarly, hybrid hydrogels are capable of producing a stimuli-responsive action mechanism caused by an induced conformational change and binding affinities of genetically engineered proteins in response to a stimulus [99]. As a biological recognition element to prepare the stimuli-responsive hydrogels, calmodulin (CaM), which is a calcium-binding protein exhibiting two conformational changes; one in the presence of Ca2+ and the other in the presence of phenothiazines, was used. The hybrid hydrogels demonstrated three-stage active swelling characteristics achieved by coupling ligand sensing with the conformational change of the site-specifically immobilized CaM. The hybrid hydrogels controlled transport of small molecules in response to Ca2+ by their reversible swelling/shrinking cycles. They act as a gate controlling the flow from a reservoir in microfluidics.
Drug-responsive hydrogels can be designed for trigger-inducible release of human vascular endothelial growth factor [100]. Polyacrylamide conjugated with genetically engineered bacterial gyrase subunit B (GyrB) forms a hydrogels by the addition of the aminocoumarin antibiotic coumermycin because of the dimerization of GyrB through coumermycin. The addition of increasing concentrations of clinically validated novobiocin (albamycin) resulted in dissociation of the hydrogels by the dissociation of the GyrB subunits, followed by the release of the human vascular endothelial growth factors 121 (VEGF121) entrapped within the hydrogels networks. Such antibiotic-inducible release using drug-responsive hydrogels enables optimal administration of the rapidly growing number of protein-based biopharmaceuticals.
Most of the biomolecule-responsive hydrogels made to exploit molecular recognition events of proteins, such as enzyme, lectin, and antibody. Since DNAs form duplexes with complementary DNAs or DNA aptamers, the mutated sequence and the folded structure bind to specific targets, their molecular recognition functions can provide the useful tools for creating biomolecule-responsive hydrogels with a wide variety of uses. The concept of reversibly DNA-responsive sol–gel transition systems using DNA-strand displacement by base pairing provided the possibility of cyclically manipulating sol–gel transitions by the addition of DNA strands that acted as crosslinkers at constant temperature and under unchanged buffer conditions [101]. Controllable macroscopic rheological properties of DNA-responsive sol–gel transition, trapping, and DNA-triggered release from DNA-responsive hydrogels were visualized using fluorescent semi-conductor quantum dots (QDs) [102]. The DNA-responsive sol–gel transition system was combined with a specific thrombin-binding aptamer, which was able to form a double-stacked G quadruplex with a high affinity to α-thrombin, in order to capture and release the thrombin [103]. These results point to the potential of the DNA-responsive sol–gel transition as a controlled release system.
DNA-responsive hydrogels that are capable of shrinking or swelling in response to DNA were prepared with a stem-loop structured DNA on the basis of the binding with its complementary target DNA [104, 105]. Highly selective target-responsive hydrogels were engineered with DNA aptamers as the crosslinks that selectively recognize a variety of target molecules (Fig. 18) [106]. The hydrogels formed by hybridization of the DNA aptamer and two kinds of single-stranded DNAs conjugated with polyacrylamide was dissolved by the addition of adenosine, which was the target molecule to competitively bind the DNA aptamer. Thus, biomolecule-responsive hydrogels conjugated with DNA have many advantages in sensing systems and the selective release of therapeutic agents in response to the target molecule demonstrating physiological changes.
Schematic representation of target molecule-responsive sol–gel transition by hybridization of the DNA aptamer and DNA-polyacrylamide conjugates [106].
Summary
Biomolecule-responsive hydrogels that undergo volume changes in response to a variety of target biomolecules are useful in many bioapplications. The properties of the biomolecule-responsive hydrogels can provide the useful tools for creating intelligent biomaterials with a wide variety of uses. The design of the biomolecule-responsive hydrogels requires detailed understanding of the structural factors that control their molecular recognition and responsive behavior. The knowledge gained from successful designs provides the basis for the development of smart biomaterials as well as more insight into the biological functions of biomolecules, cells and other biosystems. Bioconjugation of polymers with biomolecular recognition is directing research to better strategies for developing biomolecule-responsive biomaterials that have the high potential as smart biomaterials for spatiotemporally controlled drug delivery, cell culture, and tissue engineering.
References
Peppas NA (1987) Hydrogels in medicine and pharmacy. CRC, Boca Raton
DeRossi D, Kajiwara K, Osada Y, Yamauchi A (1991) Polymer gels, fundamentals and biomedical applications. Plenum, New York
Miyata T (2002) Gels and interpenetrating polymer networks. In: Yui N (ed) Supramolecular design for biological applications. CRC, Boca Raton, FL, pp 95–136, Chapter 6
Dusek K (1993) Responsive gels: volume transitions I, Adv Polym Sci, vol 109. Springer, Berlin
Dusek K (1993) Responsive gels: volume transitions II, Adv Polym Sci, vol 110. Springer, Berlin
Okano T (1998) Biorelated polymers and gels. Academic, Boston
Miyata T (2002) Stimuli-responsive polymers and gels. In: Yui N (ed) Supramolecular design for biological applications. CRC, Boca Raton, FL, pp 191–225, Chapter 9
Tanaka T, Fillmore D, Sun S-T, Nishio I, Swislow G, Shah A (1980) Phys Rev Lett 45:1636–1639
Annaka M, Tanaka T (1992) Nature 355:430–432
Tanaka T (1978) Phys Rev Lett 40:820823
Hirokawa Y, Tanaka T (1984) J Chem Phys 81:6379–6380
Amiya T, Hirokawa Y, Hirose Y, Li Y, Tanaka T (1987) J Chem Phys 86:2375–2379
Chen G, Hoffman AS (1995) Nature 373:49–52
Yoshida R, Uchida K, Kaneko T, Sakai K, Kikuchi A, Sakurai Y, Okano T (1995) Nature 374:240–242
Tanaka T, Nishio I, Sun S-T, Ueno-Nishio S (1982) Science 218:467–469
Osada Y, Okuzaki H, Hori H (1992) Nature 355:242–244
Irie M (1993) Adv Polym Sci 110:49–65
Suzuki A, Tanaka T (1990) Nature 346:345–347
Siegel RA (1993) Adv Polym Sci 109:233–267
Peppas LB, Peppas NA (1989) J Control Release 8:267–274
Brazel CS, Peppas NA (1995) Macromolecules 28:8016–8020
Dong L-C, Hoffman AS (1991) J Control Release 15:141–152
Miyata T, Nakamae K, Hoffman AS, Kanzaki Y (1994) Macromol Chem Phys 195:1111–1120
Nakamae K, Nizuka T, Miyata T, Furukawa M, Nishino T, Kato K, Inoue T, Hoffman AS, Kanzaki Y (1997) J Biomater Sci Polym Ed 9:43–53
Hoffman AS (1987) J Control Release 6:297–305
Okano T (1993) Adv Polym Sci 110:179–197
Dong L-C, Hoffman AS (1990) J Control Release 13:21–31
Okano T, Bae YH, Jacobs H, Kim SW (1990) J Control Release 11:255–265
Katono H, Maruyama A, Sanui K, Ogata N, Okano T, Sakurai Y (1991) J Control Release 16:215–227
Miyata T, Uragami T, Nakamae K (2002) Adv Drug Deliv Rev 54:79–98
Miyata T, Uragami T (2002) Biological stimuli-responsive hydrogels. In: Dumitriu S (ed) Polymeric biomaterials. Marcel Dekker, New York, pp 959–974, Chapter 36
Ishihara K, Kobayashi M, Ishimaru N, Shinohara I (1984) Polym J 16:625–631
Ishihara K, Matsui K (1986) J Polym Sci Polym Lett Ed 24:413–417
Albin G, Horbett TA, Ratner BD (1985) J Control Release 2:153–164
Albin GW, Horbett TA, Miller SR, Ricker NL (1987) J Control Release 6:267–291
Cartier S, Horbett TA, Ratner BD (1995) J Membr Sci 106:17–24
Hassan CM, Doyle FJ III, Peppas NA (1997) Macrmolecules 30:6166–6173
Parker RS, Doyle FJ III, Peppas NA (1999) IEEE Trans Biomed Eng 46:148–157
Kataoka K, Miyazaki H, Okano T, Sakurai Y (1994) Macromolecules 27:1061–1062
Shiino D, Murata Y, Kubo A, Kim YJ, Kataoka K, Koyama Y, Kikuchi A, Yokoyama M, Sakurai Y, Okano T (1995) J Control Release 37:269–276
Aoki T, Nagao Y, Sanui K, Ogata N, Kikuchi A, Sakurai Y, Kataoka K, Okano T (1996) Polym J 28:371–374
Kataoka K, Miyazaki H, Bunya M, Okano T, Sakurai Y (1998) J Am Chem Soc 120:12694–12695
Matsumoto A, Kurata T, Shiino D, Kataoka K (2004) Macromolecules 37:1502–1510
Matsumoto A, Yoshida R, Kataoka K (2004) Biomacromolecules 5:1038–1045
Brownlee M, Cerami A (1979) Science 206:1190–1191
Seminoff LA, Olsen GB, Kim SW (1989) Int J Pharm 54:241–249
Kim SW, Pai CM, Makino K, Seminoff LA, Holmberg DL, Gleeson JM, Wilson DE, Mack EJ (1990) J Control Release 11:193–201
Makino K, Mack EJ, Okano T, Kim SW (1990) J Control Release 12:235–239
Kokufuta E, Zhang Y-Q, Tanaka T (1991) Nature 351:302–304
Miyata T, Nakamae K (1997) Trend Polym Sci 5:198–206
Nakamae K, Miyata T, Jikihara A, Hoffman AS (1994) J Biomater Sci Polym Ed 6:79–90
Miyata T, Jikihara A, Nakamae K, Hoffman AS (1996) Macromol Chem Phys 197:1135–1146
Miyata T, Jikihara A, Nakamae K, Hoffman AS (2004) J Biomater Sci Polym Ed 15:1085–1098
Lee SJ, Park K (1996) J Mol Recognit 9:549–557
Obaidat AA, Park K (1996) Pharm Res 13:989–995
Obaidat AA, Park K (1997) Biomaterials 18:801–806
Ulijn RV (2006) J Mater Chem 16:2217–2225
Saffran M, Kumar GS, Savariar C, Burnham JC, Williams F, Neckers DC (1986) Science 233:1081–1086
Yeh P-Y, Kopeckova P, Kopecek J (1994) J Polm Sci A Polym Chem 32:1627–1637
Yeh P-Y, Kopeckova P, Kopecek J (1995) Macromol Chem Phys 196:2183–2202
Ghandehari H, Kopeckova P, Yeh P-Y, Kopecek J (1996) Macromol Chem Phys 197:965–980
Ghandehari H, Kopeckova P, Kopecek J (1997) Biomaterials 18:861–872
Akala EO, Kopeckova P, Kopecek J (1998) Biomaterials 19:1037–1047
Hovgaard L, Brøndsted H (1995) J Control Release 36:159–166
Plunkett KN, Berkowski KL, Moore JS (2005) Biomacromolecules 6:632–637
Li C, Madsen J, Armes SP, Lewis AL (2006) Angew Chem Int Ed 45:3510–3513
Yamamoto N, Kurisawa M, Yui N (1996) Macromol Rapid Commun 17:313–318
Kurisawa M, Yui N (1998) J Control Release 54:191–200
Kurisawa M, Matsuo Y, Yui N (1998) Macromol Chem Phys 199:705–709
Huh KM, Hashi J, Ooya T, Yui N (2000) Macromol Chem Phys 201:613–619
Sperinde JJ, Griffith LG (1997) Macromolecules 30:5255–5264
Hu B-H, Messersmith PB (2003) J Am Chem Soc 125:14298–14299
Thornton PD, McConnell G, Ulijn RV (2005) Chem Commun 47:5913–5915
Thornton PD, Mart RJ, Ulijn RV (2007) Adv Mater 19:1252–1256
Diamandis EP, Christopoulos TK (1996) Immunoassay. Academic, New York
Miyata T, Asami N, Uragami T (1999) Macromolecules 32:2082–2084
Miyata T, Asami N, Uragami T (1999) Nature 399:766–769
Lu Z-R, Kopeckova P, Kopecek J (2003) Macromol Biosci 3:296–300
Nayak S, Lyon LA (2005) Angew Chem Int Ed 44:7686–7708
Kim J, Nayak S, Lyon LA (2005) J Am Chem Soc 127:9588–9592
Kim J, Singh N, Lyon LA (2006) Angew Chem Int Ed 45:1446–1449
Kim J, Singh N, Lyon LA (2007) Chem Mater 19:2527–2532
Wulff G, Sarhan A, Zabrocki K (1973) Tetrahedron Lett 44:4329–4332
Sellergren B, Lepisto M, Mosbach K, Am J (1988) Chem Soc 110:5853–5860
Mosbach K (1994) Trends Biochem Sci 19:9–14
Shea K (1994) Trends Polym Sci 2:166–173
Wulff G (1995) Angew Chem Int Ed Engl 34:1812–1832
Byrne M, Park K, Peppas NA (2002) Adv Drug Deliv Rev 54:149–161
Bergmann NM, Peppas NA (2008) Prog Polym Sci 33:271–288
Watanabe M, Akahoshi T, Tabata Y, Nakayama D (1998) J Am Chem Soc 120:5577–5578
Wang GQ, Kuroda K, Enoki T, Grosberg A, Masamune S, Oya T, Takeoka Y, Tanaka T (2000) Proc Natl Acad Sci USA 97:9861–9864
Oya T, Enoki T, Grosberg AY, Masamune S, Sakiyama T, Takeoka Y, Tanaka K, Wang GQ, Yilmaz Y, Feld MS, Dasari R, Tanaka T (1999) Science 286:1543–1545
Miyata T, Jige M, Nakaminami T, Uragami T (2006) Proc Natl Acad Sci USA 103:1190–1193
Yamaguchi N, Zhang L, Chae B-S, Palla CS, Furst EM, Kiick KL (2007) J Am Chem Soc 129:3040–3041
Lutolf MP, Raeber GP, Zisch AH, Tirelli N, Hubbell JA (2003) Adv Mater 15:888–892
Lutolf MP, Lauer-Fields JL, Schmoekel HG, Metters AT, Weber FE, Fields GB, Hubbell JA (2003) Proc Natl Acad Sci USA 100:5413–5418
Petka WA, Harden JL, McGrath KP, Wirtz D, Tirrell DA (1998) Science 281:389–392
Wang C, Stewart RJ, Kopecek J (1999) Nature 397:417–420
Ehrick JD, Deo SK, Browning TW, Bachas LG, Madou MJ, Daunert S (2005) Nat Mater 4:298–302
Ehrbar M, Schoenmakers R, Christen EH, Fussenegger M, Weber W (2008) Nat Mater 7:800–804
Lin DC, Yurke B, Langrana NA (2004) J Biomech Eng 126:104–110
Liedl T, Dietz H, Yurke B, Simmel F (2007) Small 3:1688–1693
Wei B, Cheng I, Luo KQ, Mi Y (2008) Angew Chem Int Ed 47:331–333
Murakami Y, Maeda M (2005) Macromolecules 38:1535–1537
Murakami Y, Maeda M (2005) Biomacromolecules 6:2927–2929
Yang H, Liu H, Kang H, Tan W (2008) J Am Chem Soc 130:6320–6321
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Miyata, T. (2010). Biomolecule-Responsive Hydrogels. In: Ottenbrite, R., Park, K., Okano, T. (eds) Biomedical Applications of Hydrogels Handbook. Springer, New York, NY. https://doi.org/10.1007/978-1-4419-5919-5_4
Download citation
DOI: https://doi.org/10.1007/978-1-4419-5919-5_4
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4419-5918-8
Online ISBN: 978-1-4419-5919-5
eBook Packages: Chemistry and Materials ScienceChemistry and Material Science (R0)