Abstract
The role of positron emission tomography (PET) in clinical practice is increasing. Clinical decisions based on PET studies are changing patient management by adding functional information to that obtained from conventional morphologic modalities. Focal areas of abnormally increased fluorodeoxyglucose (FDG) uptake are considered suspicious for malignant disease, as metabolic changes often precede the anatomic changes associated with disease. Disease management depends on the tumor type, extent and aggressiveness of the lesion, and on local and distant metastases. Whole-body FDG PET is becoming a standard procedure for the imaging of cancer, and FDG PET can play a significant role in establishing therapeutic response.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Positron Emission Tomography
- Positron Emission Tomography Scanner
- Positron Emission Tomography Scan
- Oxygen Extraction Fraction
- Change Patient Management
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
The role of positron emission tomography (PET) in clinical practice is increasing. Clinical decisions based on PET studies are changing patient management by adding functional information to that obtained from conventional morphologic modalities. Focal areas of abnormally increased fluorodeoxyglucose (FDG) uptake are considered suspicious for malignant disease, as metabolic changes often precede the anatomic changes associated with disease. Disease management depends on the tumor type, extent and aggressiveness of the lesion, and on local and distant metastases. Whole-body FDG PET is becoming a standard procedure for the imaging of cancer, and FDG PET can play a significant role in establishing therapeutic response.
There is difficulty in interpreting FDG PET scans, particularly of the neck and abdomen, because of the absence of identifiable anatomic structures. The low contrast and resolution in the PET scan is insufficient for precise anatomic structures and anatomic localization of abnormal uptake. A combined PET/CT scanner successfully acquires co-registered anatomic and functional images in a single scanning session. Technical factors must be considered when evaluating organ function because they may introduce artifacts and findings that are, in reality, normal variants. These include the time between injection and scanning, the dose administered, filtering and processing steps, test-retest variability, and the type of scanner. Patient preparation, with good instructions and a questionnaire, is vitally important for proper PET scanning.
Radiopharmaceutical, Dosimetry, and Instrument
2-F-18-fluoro-2-deoxy-d-glucose (18F-FDG), 5–20 mCi, is administered intravenously (IV) through an intracatheter (23–25 gauge) or butterfly needle and flushed with 10–20 cc of normal saline. The IV system should then be removed and a residual activity should be checked. If whole-body imaging will be performed in addition to the brain study, then 15–20 mCi of 18F-FDG should be given. If three-dimensional (3D) imaging is necessary, a lower dose of 18F-FDG should be given so that the ratio between true and random activity remains in an ideal range.
The bladder wall is the critical organ and receives 3.15 rad per 5 mCi 18F-FDG. Radiation dose estimates for the bladder, heart, and brain are 1.10, 2.20, and 1.20 rad per 5 mCi 18F-FDG, respectively.
The Siemens Medical System CTI ECAT HR+ dedicated full-ring PET scanner and the GE Medical Systems Discovery LS PET/CT system are commonly utilized equipment.
General Procedure
-
1.
Patient checks in at the reception area.
-
2.
Nurse confirms the chart and required paperwork.
-
3.
Nurse reviews and answers any of the patient’s questions regarding the procedure, and ensures that all of the required preparation before the examination has been performed.
-
4.
Patient can change into a hospital gown or simply remove all metal objects, prostheses, etc.
-
5.
Nurse should alert the technologist or physician if there is reason to believe that the patient cannot tolerate the procedure.
-
6.
Patient’s height and weight should be measured.
-
7.
Patient’s blood sugar levels should be measured and recorded with a glucometer. If the patient’s blood sugar level exceeds 200 mg/dL, the nurse should notify the technologist or physician.
-
8.
Patients should answer questionnaire, and female patients should sign the consent form.
-
9.
Nurses should then begin a 20- to 23-gauge intracatheter or butterfly.
-
10.
The prepared dose of radiopharmaceutical should be checked out from the radiopharmacy.
-
11.
The dose of 5–20 mCi of 18F-FDG and flush with 10–20 cc of normal saline should be given to the patient. The syringe should be checked to determine the residual, which should be documented.
-
12.
Patient waits comfortably in the holding area for 30–45 min postinjection.
-
13.
The patient should be positioned in the scanner supine with the head toward the gantry. The head should be secured to limit patient movement.
-
14.
Set up the protocol (energy window centered at 511 keV) with lower level discriminator of 350 and upper level discriminator of 650, and assure that the correct time of injection, dose administered, and patient height and weight are entered for the procedure.
-
15.
Perform scanning of the patient, taking care to ensure correct positioning.
-
16.
If no transmission scan is needed because emission and normative data will be used to calculate attenuation, the study may be stopped after completion of the emission scan.
-
17.
Upon completion of scanning, the patient may change back into their clothes and wait for the images to be reviewed before leaving. The gown or scrubs used should be placed in the linen bag to ensure there is no radiation contamination from urine.
Protocol for Whole-Body PET Using 18F-FDG
Procedure
-
1.
Set up the protocol. Ensure that the patient’s height is represented in the database of the patient. Also, ensure that the correct time of injection, dose administered minus residual, and patient weight are entered for the procedure.
-
Use 2D, seven planes of overlap, or 3D, 15 planes of overlap whole-body imaging.
-
Check the number of bed positions based on the height of the patient.
-
-
2.
Position the patient from the orbits to 2 cm below the pubic symphysis. The first bed position should be over the pelvis to avoid artifacts in the retrovesical region from later accumulation of radioactive urine in the bladder.
-
3.
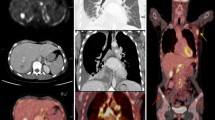
Data acquisition of PET/CT. A combined PET/CT system (Discovery LS, GE Medical Systems, Waukesha, WI) is able to obtain CT images and PET data of the same patient in one session (Fig. 7.1). A GE Advance Nxi PET scanner and a multidetector-row helical CT (LightSpeed Plus) are integrated into this dedicated system. The table excursion permits scanning of six continuous PET sections covering 867 mm, which gives adequate coverage from head to pelvic floor in all patients. The PET and CT datasets are acquired on two independent computer consoles that are connected by an interface to transfer CT data to the PET scanner. For viewing of the images, the PET and CT datasets are transferred to an independent, personal computer-based workstation by DICOM transfer. All viewing of co-registered images is performed with dedicated software (eNTEGRA, ELGEMS, Haifa, Israel). While PET images are acquired during free breathing and each image is acquired over multiple respiratory cycles, CT scans are acquired during shallow breathing.
Fig. 7.1 Selected coronal PET/CT image (top) of the axial body with 18F FDG shows a large focal area of markedly increased activity in the upper mediastinum (arrow) extending into left supraclavicular lymphatic chain. Selected axial PET image of the upper chest (left lower) shows a large focal area of markedly increased activity in the anterior mediastinum (arrow) as well as preaortic and right paraesophageal lymphatic chains. Axial noncontrast CT image (right lower) of upper chest at the same level shows ill-defined masses corresponding to increased activities. Diagnosis was Hodgkins’ disease
The patients are fasted for at least 4 h prior to the intravenous administration of 10 mCi (370 MBq) of FDG. Forty-five minutes postinjection, the combined examination begins. CT data are acquired first. The patient is positioned on the table in a head-first, supine position. The arms of the patient are placed in an elevated position above the head to reduce beam-hardening artifacts. However, in patients unable to maintain this position, arms are positioned in front of the abdomen. For the CT data acquisition, the following parameters are used: tube rotation time 0.5 s/evolution; 140 kV; 80 mA; 22.5 mm/rotation; slice pitch 6 (high-speed mode); reconstructed slice thickness 5 mm; scan length 867 mm; acquisition time 22.5 s per CT scan. No intravenous or oral contrast agents are used.
After the CT data acquisition is completed, the tabletop is automatically advanced into the PET gantry, and acquisition of PET emission data is started at the level of the pelvic floor. Six incremental table positions are obtained with minimal overlap, thereby covering 867 mm of table travel. For each position, 35 2D non-attenuations−corrected scans are obtained simultaneously over a 5-min period. No transmission scans are obtained because CT data are used for transmission correction. Transaxial, attenuation-corrected slices are reconstructed using iterative reconstruction. Image reconstruction matrix is 128 × 128 with a transaxial field of view (FOV) of 49.7 × 49.7 cm.
-
4.
Image analysis of PET/CT: Clinical preimaging data are available for reviewers. This information includes location of primary tumor, suspicion of local recurrence, and/or metastases. Image interpretation is performed without any objective measurements regarding FDG uptake. However, the images are consistently windowed so that brain FDG activity is in the over range and the lower window level is close to zero. On a grading scale from 0 to 4, activity comparable with brain was 4; between brain and liver, 3; liver, 2; and below liver, 1. Lesions are called positive only if they had FDG uptake of at least level 3 in PET, while in PET/CT small lesions noted on CT such as multiple intrapulmonary lesions are called positive even in the face of negative PET.
For lesion-based image analysis, the following three categories are evaluated if applicable: recurrence of primary, metastases, and second primary tumor. Because localization of the lesion is crucial for staging, all lesions are assigned to an anatomic region. Therefore, the full evaluation of a dataset includes status as well as location of recurrence, number and location of regional and distant metastases, and possible number and location of second primary tumors.
Protocol for PET Using 15O Water or Gases and 11C Methionine
-
1.
15O water is used to measure blood flow. PET data can be acquired in 3D mode with a model-based correction applying to account for 35% of 3D scatter fraction. Images are reconstructed with a Harming filter (cutoff Nyquist). For each 15O water study, 15–20 mCi are injected in 5 mL saline as a rapid bolus using an automated injector with simultaneous sampling of arterial blood and 4-min gynamic PET scan (23 frames; 10 × 3 s, 3 × 10 s, 4 × 15 s, and 6 × 20 s). The arterial blood data (input function) are collected over 4 min. Blood is drawn at a 6-mL/min rate and radioactive events are detected. Eight sequential PET scans are obtained at 20-min intervals. The data are analyzed using the tissue compartment model.
-
2.
15O gases are used to measure blood flow and volume as well as oxygen extraction and metabolism. 15O gases, O2, CO2, and CO, are administered sequentially in one session to provide three separate datasets.
The 15O O2 and 15O CO2 gases are delivered continuously at flows of 10 mCi/min at 80 mL/min, and 5 mCi/min at 60 mL/min, respectively during the study period. Labeled gases are mixed with 200 mL/min of medical air, and are supplied to the patient through a plastic face mask. Once inhalation of the labeled gas is initiated, equilibrium will be established over a 12-min period, followed by scans with 1.5–2.5 million for each 15O O2 image and 2–4 million 15O for each CO2 image. 15O CO is administered at 80 mCi at 100 mL/min for 4 min. The 15O CO supply is then discontinued, and following a 1-min equilibrium period, images can be obtained with 300,000–500,000 true coincidences. Blood samples are obtained from an arterial line for the measurement of blood gases throughout the studies.
The oxygen analysis program generates maps for the functional parameters for each anatomic plane as a composite dataset. The oxygen extraction fraction and metabolic rate are corrected for blood volume.
-
3.
11C-Methionine PET. 11C-methionine is another tracer for PET that can be used to assess metabolic demand for amino acids in cancer cells. Methionine PET has been useful in the differential diagnosis of benign and malignant lesions in the brain and lungs. Patients fast for at least 6 h before the PET scan. A transmission scan is acquired for 20 min using a rotating 68Ge source, and the total counts per slice are more than seven million. Emission scans are obtained over a 15-min scanning period, 20–30 min after intravenous injection of 10 mCi 11C-methionine, with more than three million counts per slice. Image reconstruction in a 128 × 128 matrix using measured attenuation correction is performed using a Shepp and Logan filter.
Common Questions Asked by Patients and Answers
What Is PET?
PET is a technology that combines the fields of medicine, computer science, chemistry, physics, and physiology to study the function of organs such as the heart, brain, and bone. It is different from conventional imaging equipment such as radiography, CT, sonography, and MRI, in that PET images contain information about how tissues function. The other imaging modalities show what the tissues look like.
What Does a PET Scanner Look Like?
The PET scanner is similar in shape to a CT or MRI scanner; however, a PET scanner makes no noise. The bed on the scanner moves during the examination so that each area of the body can be imaged.
What Can I Expect?
-
You will be asked questions about your illness.
-
Your blood glucose (sugar) levels will be checked.
-
A small IV tube will be placed into your arm to administer a very small quantity of a radioactive material. This allows for the PET scanner to “see” where sugar metabolizes in your body.
-
Because the injection you will receive is radioactive and because it is important that you are relaxed and quiet after the injection, family members are not allowed in the area while you are in the PET suite.
-
Depending on the type of PET scan that you are receiving, you may be given a medicine called Lasix through the same IV line that the radioactive sugar was injected. Lasix is a diuretic that will stimulate you to urinate.
-
Again, depending on the type of PET scan, you might need to have a tube, also known as a Foley catheter, placed in your bladder. This is done so that the scanner can “see” the area surrounding your bladder.
-
After the injection, you will need to rest quietly until it is time for your scan. Again, the amount of quiet time depends on the study, but be prepared to wait for between 45 and 90 min.
-
During the scan, you will lie on your back on a table.
-
The amount of time the scan takes depends on how tall you are and why you are having the test.
-
When the examination is over, the data will be processed and the results will be reported to your physician the following day.
Can I Eat?
No. We cannot emphasize this enough. If you eat within 6 h of your test, there is an exceptionally high chance that your examination will be canceled. The reason for this is that the scan relies on how your body absorbs sugar, and if you have eaten, your body is saturated with sugar and the medication we give will not distribute properly.
If your PET scan is scheduled in the morning, you must only drink water. No caffeine or sugar products may be consumed. If your scan is later in the afternoon, do not eat for at least 6 h before your test. You may take all of your medications. If the medication needs to be taken with food, we will contact your physician and give you further instructions.
How Long Does the Test Take?
Overall, you should allow approximately 3 h for your test. The preparation for the scan takes about 45 min. The procedure typically takes a little over an hour. However, the physician may want to obtain additional images.
Is PET Safe?
PET is a noninvasive technique that provides maximum information to your physicians with minimal radiation exposure. The radiotracers remain in the body for only short periods of time and have no known side effects.
Questionnaire for Patients
Table 7.1 is an example of a questionnaire given to patients.
Worksheet for PET
Table 7.2 is an example of a worksheet for staff.
Checklist for Female Patients
Table 7.3 is an example of a checklist for female patients.
Radiation Safety
Gamma quanta and radiographs are ionizing radiations that produce various biological effects in tissues. The energy doses delivered to patients in PET/CT are far below the 0.5 Gy threshold dose. Radiation exposure in CT may occur to organs located directly in the path of the X-ray beam or may result from the scattering of radiation inside or outside the body. The energy dose in CT depends on the current−time product (mAs), the kilovoltage (kv), and scanner-specific features. The dose is also indirectly affected by parameters such as slice thickness, object thickness, pitch factor, scan time, rotational speed, and FOV. The effective dose is the sum of the energy doses accumulated in an organ exposed to x-rays and gamma rays multiplied by tissue-weighting factors specific to that organ.
The properties of both gamma rays and x-rays must be accounted for in the radiation protection of technical staffs involved in PET/CT examinations. The half-value layer for lead shielding (the thickness of lead needed to reduce radiation intensity by one half) is 0.1 mm for x-rays (150 kv) and 4.5 mm for gamma rays (511 kev). The lead aprons used for the protection of diagnostic x-rays are of no practical value because of the penetrating power of gamma rays.
Interpretation of PET/CT
PET/CT is a combination of two highly specialized examinations, and thus each procedure must be evaluated individually to interpret all the findings correctly. PET, with its sensitive detection of metabolically active foci, can draw attention to even very subtle morphologic changes. However, this must not lead to a failure to evaluate the CT results with diagnostic intent based on classic analytical criteria. In general, FDG PET is a very sensitive but less specific modality. Therefore, an approach to optimal interpretation is to maximize specificity by correlations with clinical data and morphologic imaging. For typical PET scans, three sets of data are provided. The nonattenuation and attenuation-corrected images are typically reconstructed in axial, sagittal, and coronal planes. Findings on all datasets should be closely correlated. Errors caused by attenuation correction may lead to an apparent decrease in metabolic activity. Lowering the arms during the acquisition will usually cause artifacts of attenuation correction, especially about the shoulder girdle but also in the chest. PET has decreased sensitivity but increased specificity in small lesions while PET has increased sensitivity but possibly decreased specificity in larger lesions. A low level of metabolic activity does not always exclude a tumor. Because PET is performed during free breathing whereas CT may be acquired during a breath-hold, inaccurate localization of lesions may result. The head and breast may be changed in position between CT and PET examinations.
A hypermetabolic lesion does not always signify malignancy. It is associated with reconstruction artifacts, metallic implants, barium-based contrast media, certain benign tumors, inflammations, and brown fat. For oncologic patients, it is important to report standard uptake values of index lesions. The impression should state clearly any potential limitations of PET for the specific disease process, and the relevance of PET findings should be stated explicitly. A uniform color scale should be used for evaluating maximum intensity projection and sectional images. Inverted gray and yellow-red scales have proved effective in practice.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Kim, E.E., Wong, F.C.L. (2013). Technical Principles, Radiation Safety, and Image Interpretation. In: Kim, E., Lee, MC., Inoue, T., Wong, WH. (eds) Clinical PET and PET/CT. Springer, New York, NY. https://doi.org/10.1007/978-1-4419-0802-5_7
Download citation
DOI: https://doi.org/10.1007/978-1-4419-0802-5_7
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4419-0801-8
Online ISBN: 978-1-4419-0802-5
eBook Packages: MedicineMedicine (R0)