Abstract
A paraneoplastic visual syndrome is a syndrome of cancer-related ocular dysfunction that is not due to either direct effects of primary or metastatic tumor or treatment or treatment-related complications. Paraneoplastic visual syndromes are thought to be principally autoimmune conditions in which the tumor expresses a neuronal antigen that triggers an immune response against cross-reacting ocular antigens. Carcinoma-associated retinopathy (CAR), the most common paraneoplastic visual disorder, results in visual loss that is usually bilateral, rapid, and painless, with both cone and rod dysfunction. The carcinoma-associated cone dysfunction syndrome, part of the CAR spectrum, is very rare; patients with this syndrome have antibodies primarily directed against cones. Melanoma-associated retinopathy is distinguished by symptoms such as sudden shimmering and night blindness; usually, there is near normal color vision, visual acuity, and central vision. Paraneoplastic optic neuropathy is a syndrome of visual loss that is usually characterized by bilateral optic disc swelling, nerve fiber layer hemorrhages, and vitritis; sometimes there are abnormal findings on electroretinography. Treatments that have been tried in patients with paraneoplastic visual syndromes include immunotherapies and monoclonal antibodies. Though temporary improvement in vision has been reported, a progressive decline to severe visual loss is the usual course, even with treatment.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Uveal Melanoma
- Night Blindness
- Serous Macular Detachment
- Acute Zonal Occult Outer Retinopathy
- Vitelliform Macular Dystrophy
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Paraneoplastic visual syndrome is the term used to refer to cancer-related ocular dysfunction that is not due to either direct effects of primary or metastatic tumor or treatment or treatment-related complications. Paraneoplastic visual syndromes include paraneoplastic retinopathies and paraneoplastic optic neuropathy.
Paraneoplastic retinopathies are retinal disorders that present with a constellation of symptoms, few if any ocular signs, abnormal findings on electroretinography (ERG), and usually circulating antiretinal antibodies. The diagnosis is often missed initially, particularly in the absence of an established history of malignancy. Carcinoma-associated retinopathy is the term used for an autoimmune retinopathy associated with a cancer other than melanoma. Melanoma-associated retinopathy is the term used for an autoimmune retinopathy associated specifically with melanoma. Paraneoplastic optic neuropathy is a rare disorder characterized by painless visual loss, most commonly associated with optic disc edema. Occasionally there is also retinal dysfunction.
Evidence supports an autoimmune basis for the ocular dysfunction associated with paraneoplastic visual syndromes, which are characterized by the presence of circulating autoantibodies and a lack of obvious cancer metastasis causing the structural and functional damage to the retina or nerve [1, 2].
Paraneoplastic neurologic and ophthalmologic syndromes affect the eye as well as other parts of the nervous system, including the cerebellum, limbic system, and peripheral nerves. These syndromes may become apparent before the oncologic diagnosis. Many of these syndromes have antibodies associated with a specific malignancy, which allows targeting the workup to specific organs and/or tissue types. Paraneoplastic neurologic and ophthalmologic syndromes often cause severe and permanent neurologic and ocular morbidity. In general, it is not uncommon for more than one paraneoplastic neurologic syndrome and antibody to coexist in the same patient. However, paraneoplastic retinopathies usually occur without other neurologic autoimmune syndromes and, therefore, the presentation is usually that of vision loss alone. In contrast, paraneoplastic optic neuropathy is commonly associated with cerebellar, cognitive, and other neurological deficits.
2 Pathogenesis
Paraneoplastic visual syndromes are thought to be principally autoimmune conditions in which the tumor expresses a neuronal antigen that triggers an immune response against cross-reacting ocular antigens. Antibodies implicated in causing central nervous system paraneoplastic phenomena have been well described and include antineuronal nuclear antibody (ANNA-1 (anti-Hu) and ANNA-2 (anti-Ri)), to name just a couple.
However, in paraneoplastic retinopathy, although a large number of antiretinal antibodies have been reported, only two antibodies have been well characterized [3–5]: antibodies against recoverin (a 23-kDa protein found in rod and cone photoreceptors) and alpha-enolase (a 46-kDa protein). In addition to these, several other antibodies have been suggested as pathogenic in carcinoma-associated retinopathy (CAR)—including tubby-like protein, heat shock cognate protein (hsc70), and 22-, 35-, 40-, and 70-kDa proteins—but their exact location and function in the retina are still being investigated [6–9]. While a few protein antigens, such as mitofilin and titin, have been implicated in melanoma-associated retinopathy (MAR), the immune response characteristically involves antigens within the bipolar cell layer [10].
In paraneoplastic optic neuropathy, CRMP-5 (anti-CV2) has frequently been isolated from the optic nerve [11]. A 22-kDa antigen has also been implicated in paraneoplastic optic neuropathy [6].
3 Carcinoma-Associated Retinopathy
CAR is the most common paraneoplastic visual disorder and is most often associated with small cell lung carcinoma and less often associated with carcinoma of the endometrium, ovary, cervix, or breast; hepatocellular carcinoma; gastric cancer; thymoma; colon cancer; and prostate cancer [12–22].
CAR results in visual loss that is usually bilateral, rapid, and painless, with both cone and rod dysfunction. CAR must be suspected in patients who complain of positive visual phenomena like flashing lights, flickering, smoky or swirling vision, transient visual dimming, loss of color vision, and nyctalopia. CAR usually presents after the diagnosis of a malignancy, but in some cases, CAR precedes the cancer diagnosis. On examination, in the early stages of CAR, visual acuity may be preserved, or there may be central vision loss or scotoma, dyschromatopsia, and mild anterior or posterior uveitis; there are few if any fundus changes in the early stages of the disease. Later examinations may reveal retinal vascular attenuation, retinal pigment epithelium loss, and, rarely, optic disc pallor. These findings are usually bilateral, though they may be asymmetric. CAR is associated with abnormalities of a- and b-waves on ERG, signifying photoreceptor dysfunction.
In CAR, there is usually an autoantibody against a specific retinal antigen. Antibodies against recoverin and α-enolase are commonly detected. Anti-recoverin antibodies are almost always associated with a malignancy, whereas anti-enolase antibodies are associated with a malignancy in only about 40% of cases. This means that anti-enolase antibodies can be seen in a syndrome that looks like CAR but no cancer is detectable. In this situation we call the syndrome an autoimmune retinopathy (see Section 33.6) [23].
Recoverin is believed to be a product of a gene localized to the short arm of chromosome 17 at p13.1, close to the gene for the p53 tumor suppressor protein [24]. Recoverin is a 23-kDa calcium-binding protein with 202 amino acid residues. Recoverin can be found not only in rod and cone cells but also in pineal body, optic nerve, and optic tectum [5, 26]. It is known to play an important role in light and dark adaptation by regulating rhodopsin phosphorylation and dephosphorylation in a calcium-dependent manner. Recoverin has been found to be aberrantly expressed in cancer cells or cancer cell lines obtained from CAR patients, and this aberrant expression may trigger the autoimmune reaction, causing progressive retinal degeneration through apoptosis of retinal cells [21, 25]. Expression of recoverin was also found in 50% of cancer tissues from patients without visual symptoms of CAR. To elucidate the functional roles of aberrant recoverin expression, investigators transfected recoverin into a lung adenocarcinoma cell line (A549) not originally expressing recoverin and found that this caused a slowdown in cell proliferation [21]. Further, the investigators found that recoverin-specific cytotoxic T lymphocytes exist in the peripheral circulation of CAR patients and that these cytotoxic T lymphocytes can recognize tumor that expresses recoverin.
These observations along with the identification of serum antiretinal antibodies point to the autoimmune nature of CAR, which may involve either cell-mediated or humoral immunity, and form the basis for utilizing autoimmune modulating therapies for this condition [26, 27].
4 Carcinoma-Associated Cone Dysfunction Syndrome
The carcinoma-associated cone dysfunction syndrome, part of the CAR spectrum, is a rare manifestation of a systemic malignancy, with only a few cases reported in the literature [28–30]. Patients with carcinoma-associated cone dysfunction syndrome have antibodies primarily directed against cones (the antibodies reported are against 23-, 40-, and 50-kDa retinal antigens [28–30]) and consequently have decreased central vision, achromatopsia, central scotomas, glare after light exposure, photosensitivity, positive photostress test, and ERG findings showing marked reduction in cone responses compared to rod responses. Multifocal ERG would be extremely helpful in diagnosing this entity. Histopathology shows loss of cones in the macula and infiltration by macrophages.
5 Melanoma-Associated Retinopathy
The other well-known paraneoplastic retinopathy is MAR. This syndrome usually occurs months to years after diagnosis of melanoma when there is advanced metastatic disease, including brain metastasis [31]. The earliest reports of MAR were associated with cutaneous melanoma and, in these cases, MAR was detected at the same time as metastases [32, 33]. While one study found an average time of 3.6 years from the diagnosis of melanoma to the onset of MAR [31], reports in the literature indicate that latency can range from 2 months to 23 years [31, 34].
MAR is distinguished by symptoms such as sudden shimmering and night blindness; usually, there is near normal color vision, visual acuity, and central vision. ERG typically shows markedly reduced or absent dark-adapted b-wave with sparing of a-wave. The fundus findings are initially unremarkable, but subtle abnormalities may be seen by the time a diagnosis is made. In a study of 51 patients with MAR by Keltner et al. [31], fundus findings were normal in 44% of patients; optic disc pallor was observed in 23%, retinal vessel attenuation in 30%, and vitreous cells in 30%. In addition, atypical findings such as serous macular detachment and nummular vitelliform lesions resembling Best vitelliform macular dystrophy have been described [34, 35].
The immune response involves antigens characteristically within the bipolar cell layer detected by immunohistochemistry. The bipolar cell antigens involved are very small quantities of proteins, proteoglycans, lipids, or carbohydrates [31]. Other antigens such as neuronal antigen (22 kDa), transducin β, Muller cell protein (35 kDa), mitofilin, and titin have also been implicated in MAR and can be detected by Western blotting [6, 10, 36, 37]. MAR has also been reported with uveal melanomas [34, 35, 38]. In two cases of MAR associated with uveal melanoma, a 120-kDa antiretinal antibody, anti-enolase (46 kDa), and bestrophin-1 (68 kDa) were isolated from the serum without any signs of bipolar reactivity.
Unfortunately, melanoma has usually metastasized to the central nervous system by the time of diagnosis of MAR, and therefore, patients with this condition usually have a poor prognosis for life.
6 Autoimmune Retinopathy
Autoimmune retinopathy is a diagnosis of exclusion established in patients who present with paraneoplastic retinal symptoms but have no malignancy detected after an extensive search. Autoimmune retinopathy has been reported in case reports in the literature [25, 39–42]. In a patient diagnosed with autoimmune retinopathy and a negative initial cancer workup, it is important to repeat the cancer evaluation again after a sufficient duration of follow-up since many patients present with visual symptoms months to years before a malignancy is diagnosed.
The symptoms are generally more subclinical and gradually progressive compared with CAR. However, some patients may have rapid deterioration of vision [27]. Autoimmune retinopathy appears to be self-limiting [42] and has rarely been reported to progress to total blindness as is often the case with CAR due to anti-recoverin [26]. Patients initially complain of central visual loss and photopsia; the periphery may gradually be involved as the condition progresses. Dyschromatopsia, relative afferent pupillary defect disproportionate to the loss of vision, visual field defects, and significant attenuation of amplitude on ERG together with isolation of one or more antiretinal antibodies support the diagnosis of autoimmune retinopathy.
Treatments with immunosuppressive agents are rarely effective in this condition. One reason may be that diagnosis is often delayed until there has been irreversible damage to the neurosensory layers of the retina.
7 Paraneoplastic Optic Neuropathy
Paraneoplastic optic neuropathy is a syndrome of visual loss that is usually characterized by bilateral optic disc swelling, nerve fiber layer hemorrhages, and vitritis; sometimes there are abnormal findings on ERG indicating there is also an associated retinopathy. CRMP-5 and anti-CV2 (62 kDa) immunoglobulin, anti-60-kDa, and antiretinal ganglion cell antibodies have been reported in association with this syndrome [11, 43, 44]. Neurological problems are often seen, such as mental status abnormalities, seizures, neuropathies, muscle weaknesses, chorea, hemiballismus, and cerebellar and autonomic abnormalities. Tumors associated with paraneoplastic optic neuropathy include small cell carcinoma of the lung and, less commonly, Hodgkin’s disease, non-Hodgkin’s lymphoma, neuroblastoma, and thymoma.
8 Diagnostic Testing
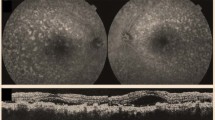
Given the usual paucity of findings on retinal examination, additional investigations are useful in establishing a diagnosis of paraneoplastic visual syndrome. Electrophysiologic investigations in the form of ERG, visual evoked potential, and sometimes electrooculography have been found to be useful [33]. Photopic and scotopic full-field ERG show extreme attenuation of the electrical response, or even nonrecordable response, but multifocal ERG is useful in demonstrating localized involvement, which is often central. In the conventional full-field ERG the response represents the summed response from different parts of the field; hence, localized defects can be missed. Particularly in cases in which the macula is involved almost exclusively, e.g., carcinoma-associated cone dysfunction, the full-field ERG may not show the extent of the abnormality whereas the multifocal ERG can isolate focal abnormalities in the latency and amplitude of the response. It also provides an alternative for patients who cannot reliably perform visual field tests. A decrease of visual evoked potential that is disproportionate to the decline in visual acuity suggests impairment of the macula or the optic nerve as seen in paraneoplastic syndromes [45]. Amsler’s grid testing, computerized visual field testing, and ocular coherence tomography (showing thinning of the retina) are other noninvasive techniques that may aid diagnosis [46].
Computerized tomography, magnetic resonance imaging, and positron emission tomography are systemic investigations that are done to rule out the presence of a malignancy when the above investigations point to a diagnosis of paraneoplastic syndrome but no malignancy has previously been identified (Fig. 33.1) [47].
Humphrey visual fields (30-2) showing severe scotoma in a 72-year-old woman. She was diagnosed with autoimmune retinopathy and was diagnosed 1 year later with neuroendocrine carcinoma of the right fallopian tube. From Raghunath A, Adamus G, Bodurka DC, et al. Cancer-associated retinopathy in neuroendocrine carcinoma of the fallopian tube. J Neuroophthalmol 2010;30:252–254. Reprinted with permission
9 Differential Diagnosis
A paraneoplastic syndrome is rarely initially considered when a patient presents with symptoms of photopsia or visual loss. Bilateral retinal, bilateral optic nerve, as well as bilateral postchiasmal cortical visual loss should be considered in the differential diagnosis. The more common diagnoses to be considered are infectious diseases, collagen vascular disorders, sarcoid, vasculitis, uveitic syndromes, chemotherapy- or radiation-induced retinopathy, and retinal disorders such as acute zonal occult outer retinopathy (AZOOR) [48, 49]. AZOOR is seen most commonly in females with myopia [50]. It presents with photopsias and almost always involves the blind spot; therefore, AZOOR almost always manifests with enlargement of the blind spot as well as marked areas of visual loss adjacent to the blind spot. The etiology of AZOOR is unknown but may relate to an infectious agent that propagates from the optic disc to the peripapillary choroid.
10 Treatment and Prognosis
Visual deterioration in patients with paraneoplastic visual syndromes is believed to occur mainly because of photoreceptor and neuronal cell death by apoptosis, which is permanent once it occurs. This would explain why total recovery of vision has not been reported either spontaneously or with treatment. This also implies that early treatment is necessary for salvaging vision. Though temporary improvement in vision has been reported, a progressive decline to severe visual loss is the usual course, even with treatment.
Various immunotherapies have been tried in patients with paraneoplastic visual syndromes to help prevent deterioration of vision. Agents that have been administered in conjunction with antineoplastic therapy include oral and intravenous steroids, plasmapheresis, intravenous immunoglobulin, and cyclosporine; these have resulted in partial or no success in visual stabilization as reviewed by Chan et al. [51–54].
Other treatments that have been tried include monoclonal antibodies, such as alemtuzumab, which stabilized vision in a patient with chronic lymphocytic leukemia for 8 years [55]. We have used rituximab with mixed results in various syndromes. We had a patient with potential lymphoma-associated retinopathy who responded to rituximab and not steroids.
Anti-recoverin antibody, which is the antibody most commonly associated with CAR, is believed to localize to the photoreceptors and enhance rhodopsin phosphorylation in a calcium-dependent manner, which finally leads to apoptosis of the cell [56]. This prompted some investigators to experimentally use calcium channel blockers such as nilvadipine to reduce intracellular calcium levels and suppress retinal cellular apoptosis [57]. This approach has not yet been proven to be clinically effective [46].
11 Conclusion
In conclusion, not only are the paraneoplastic visual syndromes difficult to diagnose, they are also difficult to treat. There is no particular recommended treatment that would work for every patient. Patient tolerance, response to therapy, and titers of circulating antiretinal or anti-optic nerve antibodies could be used as guidelines to choose the best therapy for trying to limit the devastating visual loss seen with paraneoplastic visual syndromes.
References
Grunwald GB, Klein R, Simmonds MA, Kornguth SE. Autoimmune basis for visual paraneoplastic syndrome in patients with small-cell lung carcinoma. Lancet 1985;1(8430):658–661.
Thirkill CE. Cancer-induced, immune-mediated ocular degenerations. Ocul Immunol Inflamm 2005;13(2–3):119–31.
Adamus G, Amundson D, Seigel GM, Machnicki M. Anti-enolase-alpha autoantibodies in cancer-associated retinopathy: epitope mapping and cytotoxicity on retinal cells. J Autoimmun 1998;11(6):671–7.
Adamus G, Guy J, Schmied JL, Arendt A, Hargrave PA. Role of anti-recoverin autoantibodies in cancer-associated retinopathy. Invest Ophthalmol Vis Sci 1993;34(9):2626–33.
Adamus G, Machnicki M, Elerding H, Sugden B, Blocker YS, Fox DA. Antibodies to recoverin induce apoptosis of photoreceptor and bipolar cells in vivo. J Autoimmun 1998;11(5):523–33.
Keltner JL, Thirkill CE. The 22-kDa antigen in optic nerve and retinal diseases. J Neuroophthalmol 1999;19(2):71–83.
Ohguro H, Ogawa K, Nakagawa T. Recoverin and Hsc 70 are found as autoantigens in patients with cancer-associated retinopathy. Invest Ophthalmol Vis Sci 1999;40(1):82–9.
Takahashi K, Suzuki J, Ohguro H, Ohyachi H, Yoshida K, Takahashi H, Nakagawa T. [A case of paraneoplastic retinopathy with serum antibody against retinal soluble 70 kDa protein]. Nippon Ganka Gakkai Zasshi 1997;101(1):92–6.
Kikuchi T, Arai J, Shibuki H, Kawashima H, Yoshimura N. Tubby-like protein 1 as an autoantigen in cancer-associated retinopathy. J Neuroimmunol 2000;103(1):26–33.
Pfohler C, Preuss KD, Tilgen W, Stark A, Regitz E, Fadle N, Pfreundschuh M. Mitofilin and titin as target antigens in melanoma-associated retinopathy. Int J Cancer 2007;120(4):788–95.
Cross SA, Salomao DR, Parisi JE, Kryzer TJ, Bradley EA, Mines JA, Lam BL, Lennon VA. Paraneoplastic autoimmune optic neuritis with retinitis defined by CRMP-5-IgG. Ann Neurol 2003;54(1):38–50.
Adamus G, Amundson D, MacKay C, Gouras P. Long-term persistence of antirecoverin antibodies in endometrial cancer-associated retinopathy. Arch Ophthalmol 1998;116(2):251–3.
Khan N, Huang JJ, Foster CS. Cancer associated retinopathy (CAR): an autoimmune-mediated paraneoplastic syndrome. Semin Ophthalmol 2006;21(3):135–41.
Chang PY, Yang CH, Yang CM. Cancer-associated retinopathy in a patient with hepatocellular carcinoma: case report and literature review. Retina 2005;25(8):1093–6.
Eltabbakh GH, Hoogerland DL, Kay MC. Paraneoplastic retinopathy associated with uterine sarcoma. Gynecol Oncol 1995;58(1):120–3.
Harmon JP, Purvin VA, Guy J, Aptsiauri N, Sutton GP. Cancer-associated retinopathy in a patient with advanced epithelial ovarian carcinoma. Gynecol Oncol 1999;73(3):430–2.
Harper DG, Arsura EL, Bobba RK, Reddy CM, Sawh AK. Acquired color blindness in an elderly male patient from recurrent metastatic prostate cancer. J Am Geriatr Soc 2005;53(7):1265–7.
Seles S, Lang GE. [CAR syndrome (carcinoma-associated retinopathy syndrome) associated with an adenocarcinoma of the cervix]. Klin Monbl Augenheilkd 2005;222(9):736–9.
Yamada G, Ohguro H, Aketa K, Itoh T, Shijubo N, Takahashi H, Fujiwara O, Satoh M, Ohtsuka K, Abe S. Invasive thymoma with paraneoplastic retinopathy. Hum Pathol 2003;34(7):717–9.
Yoon YH, Cho EH, Sohn J, Thirkill CE. An unusual type of cancer-associated retinopathy in a patient with ovarian cancer. Korean J Ophthalmol 1999;13(1):43–8.
Ohguro H, Odagiri H, Miyagawa Y, Ohguro I, Sasaki M, Nakazawa M. Clinicopathological features of gastric cancer cases and aberrantly expressed recoverin. Tohoku J Exp Med 2004;202(3):213–9.
Jacobson DM, Adamus G. Retinal anti-bipolar cell antibodies in a patient with paraneoplastic retinopathy and colon carcinoma. Am J Ophthalmol 2001;131(6):806–8.
Weleber RG, Watzke RC, Shults WT, Trzupek KM, Heckenlively JR, Egan RA, Adamus G. Clinical and electrophysiologic characterization of paraneoplastic and autoimmune retinopathies associated with antienolase antibodies. Am J Ophthalmol 2005;139(5):780–94.
McGinnis JF, Austin B, Klisak I, Heinzmann C, Kojis T, Sparkes RS, Bateman JB, Lerious V. Chromosomal assignment of the human gene for the cancer-associated retinopathy protein (recoverin) to chromosome 17p13.1. J Neurosci Res 1995;40(2):165–8.
Adamus G. Autoantibody-induced apoptosis as a possible mechanism of autoimmune retinopathy. Autoimmun Rev 2003;2(2):63–8.
Whitcup SM, Vistica BP, Milam AH, Nussenblatt RB, Gery I. Recoverin-associated retinopathy: a clinically and immunologically distinctive disease. Am J Ophthalmol 1998;126(2):230–7.
Heckenlively JR, Fawzi AA, Oversier J, Jordan BL, Aptsiauri N. Autoimmune retinopathy: patients with antirecoverin immunoreactivity and panretinal degeneration. Arch Ophthalmol 2000;118(11):1525–33.
Jacobson DM, Thirkill CE. Paraneoplastic cone dysfunction: an unusual visual remote effect of cancer. Arch Ophthalmol 1995;113(12):1580–2.
Parc CE, Azan E, Bonnel S, Sahel JA, Kaplan J, Thirkill CE. Cone dysfunction as a paraneoplastic syndrome associated with retinal antigens approximating 40 kiloDalton. Ophthalmic Genet 2006;27(2):57–61.
Cogan DG, Kuwabara T, Currie J, Kattah J. [Paraneoplastic retinopathy simulating cone dystrophy with achromatopsia]. Klin Monbl Augenheilkd 1990;197(2):156–8.
Keltner JL, Thirkill CE, Yip PT. Clinical and immunologic characteristics of melanoma-associated retinopathy syndrome: eleven new cases and a review of 51 previously published cases. J Neuroophthalmol 2001;21(3):173–87.
Rougier MB, Hostyn P, Bret-Dibat C, Delaunay MM, Riss I, Le Rebeller MJ. [Paraneoplastic retinopathy associated with cutaneous melanoma. An update apropos of a case]. J Fr Ophthalmol 1995;18(5):396–403.
Weinstein JM, Kelman SE, Bresnick GH, Kornguth SE. Paraneoplastic retinopathy associated with antiretinal bipolar cell antibodies in cutaneous malignant melanoma. Ophthalmology 1994;101(7):1236–43.
Zacks DN, Pinnolis MK, Berson EL, Gragoudas ES. Melanoma-associated retinopathy and recurrent exudative retinal detachments in a patient with choroidal melanoma. Am J Ophthalmol 2001;132(4):578–81.
Eksandh L, Adamus G, Mosgrove L, Andreasson S. Autoantibodies against bestrophin in a patient with vitelliform paraneoplastic retinopathy and a metastatic choroidal malignant melanoma. Arch Ophthalmol 2008;126(3):432–5.
Flynn M, Fishman G, Adamus G. Antiretinal Muller cell antibodies in patients with melanoma associated and autoimmune retinopathy. Invest Ophthalmol Vis Sci 2000;41:S567.
Potter MJ, Adamus G, Szabo SM, Lee R, Mohaseb K, Behn D. Autoantibodies to transducin in a patient with melanoma-associated retinopathy. Am J Ophthalmol 2002;134(1):128–30.
Sotodeh M, Paridaens D, Keunen J, van Schooneveld M, Adamus G, Baarsma S. Paraneoplastic vitelliform retinopathy associated with cutaneous or uveal melanoma and metastases. Klin Monbl Augenheilkd 2005;222(11):910–4.
Peek R, Verbraak F, Coevoet HM, Kijlstra A. Muller cell-specific autoantibodies in a patient with progressive loss of vision. Invest Ophthalmol Vis Sci 1998;39(10):1976–9.
Hargitai J, MacKay C, Behrens M, Odel JG, Hood DC, Gouras P. Auto-immune-like cone dystrophy. Doc Ophthalmol 2004;109(3):215–21.
Mizener JB, Kimura AE, Adamus G, Thirkill CE, Goeken JA, Kardon RH. Autoimmune retinopathy in the absence of cancer. Am J Ophthalmol 1997;123(5):607–18.
Mantel I, Ramchand KV, Holder GE, Ohbayashi M, Morohoshi K, Patel N, Toda M, Fitzke FW, Bird AC, Ono SJ. Macular and retinal dysfunction of unknown origin in adults with normal fundi: evidence for an autoimmune pathophysiology. Exp Mol Pathol 2008;84(2):90–101.
Lieberman FS, Odel J, Hirsh J, Heinemann M, Michaeli J, Posner J. Bilateral optic neuropathy with IgGkappa multiple myeloma improved after myeloablative chemotherapy. Neurology 1999;52(2):414–6.
Luiz JE, Lee AG, Keltner JL, Thirkill CE, Lai EC. Paraneoplastic optic neuropathy and autoantibody production in small-cell carcinoma of the lung. J Neuroophthalmol 1998;18(3):178–81.
Matsui Y, Mehta MC, Katsumi O, Brodie SE, Hirose T. Electrophysiological findings in paraneoplastic retinopathy. Graefes Arch Clin Exp Ophthalmol 1992;230(4):324–8.
Mohamed Q, Harper CA. Acute optical coherence tomographic findings in cancer-associated retinopathy. Arch Ophthalmol 2007;125(8):1132–3.
Linke R, Schroeder M, Helmberger T, Voltz R. Antibody-positive paraneoplastic neurologic syndromes: value of CT and PET for tumor diagnosis. Neurology 2004;63(2):282–6.
Sadowski B, Kriegbaum C, Apfelstedt-Sylla E. Tamoxifen side effects, age-related macular degeneration (AMD) or cancer associated retinopathy (CAR)? Eur J Ophthalmol 2001;11(3):309–12.
Koestinger A, Guex-Crosier Y, Borruat FX. Autoimmune retinal dysfunction in sarcoid chorioretinopathy. Klin Monbl Augenheilkd 2006;223(5):428–30.
Gass JD. Acute zonal occult outer retinopathy. Donders Lecture: The Netherlands Ophthalmological Society, Maastricht, Holland, June 19, 1992. J Clin Neuroophthalmol 1993;13(2):79–97.
Guy J, Aptsiauri N. Treatment of paraneoplastic visual loss with intravenous immunoglobulin: report of 3 cases. Arch Ophthalmol 1999;117(4):471–7.
Klingele TG, Burde RM, Rappazzo JA, Isserman MJ, Burgess D, Kantor O. Paraneoplastic retinopathy. J Clin Neuroophthalmol 1984;4(4):239–45.
Chan JW. Paraneoplastic retinopathies and optic neuropathies. Surv Ophthalmol 2003;48(1):12–38.
Subhadra C, Dudek AZ, Rath PP, Lee MS. Improvement in visual fields in a patient with melanoma-associated retinopathy treated with intravenous immunoglobulin. J Neuroophthalmol 2008;28(1):23–6.
Espandar L, O’Brien S, Thirkill C, Lubecki LA, Esmaeli B. Successful treatment of cancer-associated retinopathy with alemtuzumab. J Neurooncol 2007;83(3):295–302.
Maeda T, Maeda A, Maruyama I, Ogawa KI, Kuroki Y, Sahara H, Sato N, Ohguro H. Mechanisms of photoreceptor cell death in cancer-associated retinopathy. Invest Ophthalmol Vis Sci 2001;42(3):705–12.
Ohguro H, Ogawa K, Maeda T, Maruyama I, Maeda A, Takano Y, Nakazawa M. Retinal dysfunction in cancer-associated retinopathy is improved by Ca(2+) antagonist administration and dark adaptation. Invest Ophthalmol Vis Sci 2001;42(11):2589–95.
Raghunath A, Adamus G, Bodurka DC, Liu J, Schiffman J. Cancer-associated retinopathy in neuroendocrine carcinoma of the fallopian tube. J Neuroopthalmol 2010;30(3):252–4.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Raghunath, A., Schiffman, J.S. (2010). Paraneoplastic Visual Syndromes. In: Esmaeli, B. (eds) Ophthalmic Oncology. M.D. Anderson Solid Tumor Oncology Series, vol 6. Springer, Boston, MA. https://doi.org/10.1007/978-1-4419-0374-7_33
Download citation
DOI: https://doi.org/10.1007/978-1-4419-0374-7_33
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4419-0373-0
Online ISBN: 978-1-4419-0374-7
eBook Packages: MedicineMedicine (R0)