Abstract
We herein report a patient with cancer-associated retinopathy who experienced multiple bouts of paraneoplastic retinopathy and optic neuropathy but responded to treatments with alemtuzumab and was able to maintain useful vision over the course of 8 years of follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Paraneoplastic syndromes with ocular manifestations are characterized by visual or neurologic dysfunction that occurs in a patients with a known or suspected malignancy and cannot be attributed to direct involvement of the eye or nervous system by tumor; toxic effects of antineoplastic agents, opportunistic infection, or another known cause. Such syndromes are thought to originate from an autoimmune process; circulating antibodies to specific neuronal antigens have been identified in some cases [1]. Paraneoplastic syndromes with ocular manifestations may involve the retina (“paraneoplastic retinopathy”), optic nerve, brainstem, and cerebellum [2–5]. One of the most common forms of paraneoplastic retinopathy is cancer-associated retinopathy (CAR), a subacute, progressive autoimmune retinopathy that affects both cones and rods and usually leads to severe bilateral visual loss [6–8]. Paraneoplastic optic neuropathy is a subacute, progressive, usually bilateral visual loss and usually not associated with pain. The optic disk in patients with paraneoplastic optic neuropathy can be normal in appearance early on but eventually develops pallor. Direct compression or infiltration of the optic nerve due to cancer and/or acute ischemic optic neuropathy should be ruled out before the diagnosis of paraneoplastic optic neuropathy is entertained.
There are few effective vision-saving treatments for CAR or paraneoplastic optic neuropathy. Corticosteroids have been used with variable modest success, but severe visual loss is the usual ultimate outcome in patients with CAR.
We herein report a patient with serologically proven CAR and paraneoplastic optic neuropathy who was successfully treated with alemtuzumab (Campath, Cambridge, MA) over an 8-year follow-up period after the initial diagnosis of CAR. Although the patient experienced some permanent decline in her visual fields and visual acuity after each episode of CAR, alemtuzumab therapy resulted in maintenance of fairly good visual function during the entire follow-up period.
Clinical history
A 66-year-old woman presented to our Ophthalmology Clinic in October 1998 with a complaint of onset of retrobulbar headache with positive visual phenomenon (flashes of light) in both eyes. She had been diagnosed with breast cancer in 1978 and was treated in that same year with lumpectomy, axillary lymph node dissection (all nodes examined were free of disease), and adjuvant chemotherapy without radiation therapy. In 1991, the patient developed an elevated white blood cell count (23,000/μl, 73% lymphocytes), and she was diagnosed with chronic lymphocytic leukemia (CLL) on the basis of a bone marrow biopsy. The patient was subsequently referred to our institution for treatment of her leukemia. She was treated in 1991with three cycles of fludarabine and experienced a complete remission. She did well until October 1998, when she presented to our Ophthalmology Clinic.
At presentation, the patient’s best corrected visual acuity was 20/20 in the right eye and 20/30 in the left eye. Findings on the rest of the ophthalmologic exam were normal except for a mild left optic nerve pallor and a mild left relative afferent pupillary defect. The patient had bilateral visual field deficits as shown in Fig. 1. She underwent magnetic resonance imaging and magnetic resonance angiography with diffusion-weighted imaging, fluid-attenuated inversion recovery sequences, and gadolinium enhancement; findings on all studies were normal. She also had a lumbar puncture with normal findings (normal opening pressure, cytology, cultures, and other chemistry values). Findings on carotid ultrasonography and electroencephalography were also normal. A temporal artery biopsy was negative for temporal arteritis. Immunologic tests, including tests for antinuclear antibodies, antibodies against SS-A and SS-B antigen, and rheumatoid factor were negative; her erythrocyte sedimentation rate was three.
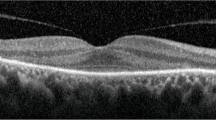
The patient was treated with high-dose steroids (prednisone 80 mg/day) for the presumed diagnosis of optic neuritis. Her visual function initially improved, but as soon as the steroid dose was tapered to 50 mg/day, her symptoms recurred. She also became intolerant of the side effects of high-dose steroids. Plasmapheresis and intravenous cyclosporin were tried but did not yield any significant improvement in the patient’s visual acuity or function and she continued to have further deterioration of her visual fields. In July 1999, her best corrected visual acuity was 20/60 in both eyes, and her visual field deficits had progressed (Fig. 2). A flash electroretinogram was obtained following dilation of the pupils and dark adaptation for 30 min. Briefly, corneal electrodes were placed on both eyes and a flash electrical stimulus was conducted and the response of the photoreceptors was recorded. The patient had an abnormal electroretinogram (Fig. 3a, b). CAR was suspected, and serologic testing for CAR antibodies was done at the University of California, Davis. The patient had a titer of 1/800 in the retina, the focus of antibody activity was the outer plexiform layer. These findings were consistent with a diagnosis of autoimmune-mediated paraneoplastic retinopathy (CAR). Her serum reacted with the 40 kDa CAR antigen as described in some previous reports [9], but not with the 23 kDa CAR antigen, also referred to as “recoverin” [10].
Beginning in June 1999, the patient was treated with alemtuzumab (Campath), 30 mg intravenously three times a week for 4 weeks on an outpatient basis. She experienced no side effects from the drug except for mild infusion-related chills and nausea. She had almost immediate improvement of visual function after the start of alemtuzumab therapy; her symptoms of flashes of light and her visual acuity and visual fields improved dramatically. In October 1999, 4 months after the start of alemtuzumab treatment, her best corrected visual acuity was 20/25 in the right eye and 20/30 in the left; her visual fields were also improved (Fig. 4).
The patient’s visual acuity and visual fields remained stable for almost 2.5 years, until May 2001, when she had a recurrent bout of paraneoplastic syndrome associated with flashes of light and severe throbbing pain behind both eyes, bilateral visual loss, visual field deterioration in the left eye (Fig. 5a), and a severe tingling sensation in her fingertips. She was once again treated with alemtuzumab 30 mg intravenously three times a week for 4 weeks. She experienced some mild tremor for a few minutes at the time of each infusion of alemtuzumab and had fatigue for a few days after each infusion as temporary side effects of the drug, but she once again had almost immediate improvement of visual symptoms and regained most of her visual acuity, although the visual-field deficit in the left eye did not completely resolve (Fig. 5b). In November 2001, 3 months after the start of the second round of alemtuzumab therapy, her best corrected visual acuity was 20/25 in the right eye and 20/40 in the left eye.
The patient experienced one more bout of paraneoplastic retinopathy and optic neuropathy in October 2005. This latest recurrence was once again heralded by subjective visual symptoms described by the patient as flashes of light and constricted visual fields in both eyes, more pronounced on the left than on the right, and was documented with a complete ophthalmologic exam and a repeat visual field test. After each of these two recurrences, the patient was treated with alemtuzumab 30 mg intravenously three times a week for 4 months. During her most recent examination, in April 2006, the best corrected visual acuity was 20/25 in the right eye and 20/70 in the left eye. She had a definite left afferent papillary defect. The left optic disc had significant pallor, and the right optic nerve had mild pallor. Results of the visual field test in April 2006 are shown in Fig. 6.
Discussion
We have described a patient with serologically proven CAR who responded well to alemtuzumab during several bouts of paraneoplastic retinopathy and optic neuropathy over an 8 year follow-up period after the diagnosis of CAR. Because steroids, plasmapheresis, and cyclosporine were not successful, alemtuzumab was used as a new form of treatment for her paraneoplastic autoimmune retinopathy. Alemtuzumab was chosen because of preliminary data suggesting its positive effects in treatment of other forms of paraneoplastic syndrome such as paraneoplastic pemphigus in B-cell CLL [11]. The patient’s visual symptoms resolved and her visual acuity and visual fields improved dramatically in response to alemtuzumab, although with each attack she experienced some permanent visual-acuity and visual-field loss. The patient’s final visual outcome 8 years after the diagnosis of CAR was very good compared with previously reported outcomes in the literature, and she may be one of the longest-surviving patients with CAR ever reported.
Alemtuzumab is a recombinant DNA-derived humanized monoclonal antibody that is directed against the 21–28-kDa cell surface glycoprotein CD52. CD52 is expressed on the surface of normal and malignant B and T lymphocytes, natural killer cells, monocytes, macrophages, and tissues of the male reproductive system.
Alemtuzumab is indicated and Food and Drug Administration-approved for the treatment of B-cell CLL in patients who have been treated with alkylating agents and in whom fludarabine therapy failed to control disease [12]. There are many published studies and case reports of the use of alemtuzumab for treatment of acute lymphocytic leukemia [13], T-cell Leukemia [14], graft-versus-host disease (GVHD) [15], severe paraneoplastic pemphigus in B-cell CLL [11], severe peripheral ulcerative keratitis associated with Wegener’s granulomatosis [16], and multiple sclerosis [17], and for prevention of GVHD [18]. The mechanism of action of alemtuzumab is thought to be mostly immune mediated, through both complement-dependent lysis and antibody-dependent cellular cytotoxicity. The most common side effect of alemtuzumab is infusion-related adverse events, which occur in about 5% of patients and may include rigors, drug-related fever, nausea, vomiting, and hypotension. Other reported side effects include rash, fatigue, urticaria, dyspnea, pruritis, headache, and diarrhea. Acute infusion-related events are most common during the first week of therapy.
A variety of drugs have previously been used to treat CAR, with limited success. Several previously published case reports have described mild to moderate transient improvement in visual acuity and visual fields in patients with CAR in response to treatment with high-dose intravenous methylprednisolone [19–22]. Keltner et al. described a patient whose antibody levels diminished and visual function improved and stabilized during 7 months of corticosteroid therapy; this patient died 7 months after the diagnosis of CAR [23]. However, other reports have failed to show any beneficial effect of steroids [24–26]. Murphy et al. described a patient in whom oral corticosteroid therapy combined with plasmapheresis resulted in recovery of vision, but the recovery lasted only 4 months [25]. In another study, plasmapheresis failed to prevent progression of visual loss in a patient with CAR [27]. Guy and Aptsiauri reported response to intravenous immunoglobulin in two of three patients with paraneoplastic retinopathy [28]. In all of the aforementioned cases, the very limited lifespan of the patients and short reported follow-up data (a few weeks) precluded observation of any long-term effects of treatment on visual function.
Other studies have demonstrated that surgery, chemotherapy, and radiation therapy to treat the primary tumor did not alter the visual prognosis in patients with CAR [28, 29]. Progressive worsening of vision despite removal of tumor cells suggests that the circulating antibodies persist and cause ongoing retinal inflammation and apoptosis.
Any adult with unexplained visual loss, with rod or cone dysfunction, or with known or suspected malignancy in the absence of other neurologic symptoms should undergo a thorough investigation for CAR. The role of alemtuzumab in the treatment of paraneoplastic retinopathy and optic neuropathy should be studied in future larger-scale studies.
References
Jacobson DM (1998) Paraneoplastic diseases of neuro-ophthalmologic interest. In: Miller NR, Newman N (eds) Walsh & Hoyts clinical neuro-ophthalmology, 5th edn. Williams and Wilkins, Baltimore, pp 2497–2551
Adamus G, Guy J, Schmied JL et al (1993) Role of anti-recoverin autoantibodies in cancer-associated retinopathy. Invest Ophthalmol Vis Sci 34:2626–2633
Thirkill CE, Tait RC, Tyler NK et al (1992) The cancer-associated retinopathy antigen is a recoverin-like protein. Invest Ophthalmol Vis Sci 33:2768–2772
Malik S, Furlan AJ, Sweeney PJ, Kosmorsky GS, Wong M (1992) Optic neuropathy: a rare paraneoplastic syndrome. J Clin Neuroophthalmol 12:137–141
Keltner JL, Thirkill CE (1998) Cancer-associated retinopathy vs recoverin-associated retinopathy. Am J Ophthalmol 126:296–302
Luiz JE, Lee AG, Keltner JL, Thirkill CE, Lai EC (1998) Paraneoplastic optic neuropathy and autoantibody production in small-cell carcinoma of the lung. J Neuroophthalmol 18:178–181
de la Sayette V, Bertran F, Honnorat J, Schaeffer S, Iglesias S, Defer G (1998) Paraneoplastic cerebellar syndrome and optic neuritis with anti-CV2 antibodies: clinical response to excision of the primary tumor. Arch Neurol 55:405–408
Thambisetty MR, Scherzer CR, Yu Z, Lennon VA, Newman NJ (2001) Paraneoplastic optic neuropathy and cerebellar ataxia with small cell carcinoma of the lung. J Neuroophthalmol 21:164–167
Browning AC, Amoaku WM, Vernon SA et al (2004) Cachexia and poor night vision. Lancet 363:1305
Cancer-associated retinopathy (CAR syndrome) with antibodies reacting with retinal, optic nerve, and cancer cells. (1989) N Engl J Med 321:1589–1594
Hohwy T, Bang K, Steiniche T, Peterslund NA, d_Amore F (2004) Alemtuzumab-induced remission of both severe paraneoplastic pemphigus and leukaemic bone marrow infiltration in a case of treatment-resistant B-cell chronic lymphocytic leukaemia. Eur J Haematol 73:206–209
Full prescribing information (PI) for Campath®. www.campath.com
Golay J, Cortiana C, Manganini M et al (2006) The sensitivity of acute lymphoblastic leukemia cells carrying the t(12;21) translocation to campath-1H-mediated cell lysis. Haematologica 91:322–330
Ravandi F, Kantarjian H, Jones D, Dearden C, Keating M, O’Brien S (2005) Mature T-cell leukemias. Cancer 104:1808–1818
Busca A, Locatelli F, Lovisone E et al (2005) Treatment of severe refractory acute graft-versus-host disease of the gastrointestinal tract with campath-1H. Biol Blood Marrow Transplant 11:734–736
Wertheim MS, Ross AH, Tole DM. The use of Campath in severe peripheral ulcerative keratitis associated with Wegener’s granulomatosis. Eye Advance. Online publication, 7 April 2006; doi:10.1038/sj.eye.6702330
Coles AJ, Cox A, Le Page E et al (2006) The window of therapeutic opportunity in multiple sclerosis: Evidence from monoclonal antibody therapy. J Neurol 253:98–108
Chalandon Y, Roosnek E, Mermillod B, Waelchli L, Helg C, Chapuis B (2006) Can only partial T-cell depletion of the graft before hematopoietic stem cell transplantation mitigate graft-versus-host disease while preserving a graft-versus-leukemia reaction? A prospective phase II study. Biol Blood Marrow Transplant 12:102–110
Keltner JL, Thirkill CE, Tyler NK et al (1992) Management and monitoring of cancer-associated retinopathy. Arch Ophthalmol 110:48–53
Jacobson DM, Thirkill CE, Tipping SJ (1990) A clinical triad to diagnose paraneoplastic retinopathy. Ann Neurol 28:162–167
Kashiwabara K, Nakamura H, Kishi K et al (1999) Cancer-associated retinopathy during treatment for small-cell lung carcinoma. Intern Med 38:597–601
Thirkill CE, Roth AM, Keltner JL (1987) Cancer-associated retinopathy. Arch Ophthalmol 105:372–375
Keltner JL, Thirkill CE, Tyler NK et al (1992) Management and monitoring of cancer-associated retinopathy. Arch Ophthalmol 110:48–53
Yoon YH, Cho EH, Sohn J, Thirkill CE (1999) An unusual type of cancer-associated retinopathy in a patient with ovarian cancer. Korean J Ophthalmol 13:43–48
Murphy MA, Thirkill CE, Hart WM (1996) Paraneoplastic retinopathy: a novel autoantibody reaction associated with small cell lung carcinoma. J Neuroophthalmol 17:77–83
Salgia R, Hedges TR, Rizk M et al (1998) Cancer-associated retinopathy in a patient with non-small-cell lung carcinoma. Lung Cancer 22:149–152
Thirkill CE, FitzGerald P, Sergott RC et al (1989) Cancer-associated retinopathy (CAR syndrome) with antibodies reacting with retinal, optic-nerve, and cancer cells. N Engl J Med 321:1589–1594
Guy J, Aptsiauri N (1999) Treatment of paraneoplastic visual loss with intravenous immunoglobulin: report of 3 cases. Arch Ophthalmol 117:471–477
Brink H, Deutman A, Beex L (1997) Unusual retinal pigment epitheliopathy and choroidopathy in carcinomatosis: a rare case of cancer-associated retinopathy. Graefes Arch Clin Exp Ophthalmol 236:75
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Espandar, L., O’Brien, S., Thirkill, C. et al. Successful treatment of cancer-associated retinopathy with alemtuzumab. J Neurooncol 83, 295–302 (2007). https://doi.org/10.1007/s11060-006-9326-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-006-9326-7