Abstract
Data suggest that low levels of dopamine D2 receptors and attenuated responsivity of dopamine-target regions to food intake is associated with increased eating and elevated weight. There is also growing (although mixed) evidence that genotypes that appear to lead to reduced dopamine signaling (e.g., DRD2, DRD4, and DAT) and certain appetite-related hormones and peptides (e.g., ghrelin, orexin A, leptin) moderate the relation between dopamine signaling, overeating, and obesity. This chapter reviews findings from studies that have investigated the relation between dopamine functioning and food intake and how certain genotypes and appetite-related hormones and peptides affect this relation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction: Dopamine Reward and Overeating
Considerable research has implicated dopamine-based meso-limbic and meso-cortical circuitries in eating behavior. Microdialysis studies with animals reveal that consumption of high-sugar or high-fat food results in dopamine release in the nucleus accumbens (Avena et al. 2008). Consumption of a pleasant meal in humans results in dopamine release in the dorsal striatum and the magnitude of release correlates with ratings of meal pleasantness (Small et al. 2003). Furthermore, brain dopamine release increases during the anticipation of food intake (Volkow et al. 2002).
Incentive salience theory posits that consummatory and anticipatory reward operates in tandem in the development of reinforcing value of food, but that with repeated intake of a food, hedonics decrease, while anticipatory reward increases (Robinson and Berridge 2000). By conditioning, food images and cues come to activate reward circuitry, leading to food cravings, and possibly to overeating and weight gain (Ritchie and Noble 2003). This motivational state, mediated by increased dopamine in reward circuitry, draws attention to food and results in attentional bias for food stimuli (Berridge and Robinson 1998; Bowirrat and Oscar-Berman 2005). After conditioning, the reward value of food shifts from food intake to anticipated food intake. For example, naive monkeys that had not experienced rewards in a setting showed increased firing of dopamine neurons in midbrain only in response to food taste; however, after conditioning, increased firing began to precede reward delivery and eventually maximal firing was elicited by the conditioned stimuli that predicted food reward versus actual food receipt (Schultz et al. 1993). Kiyatkin and Gratton (1994) found that the greatest dopamine neuronal activity occurred in an anticipatory fashion as rats approached and pressed a bar that produced food reward, with activity decreasing as the rat received and ate the food. Indeed, although DA release occurs in response to unexpected palatable food, Blackburn et al. (1989) found that dopamine release was greater in the nucleus accumbens of rats after presentation of a conditioned stimulus that usually signaled food receipt than after delivery of an unexpected meal.
2 Relation of Dopamine Functioning to Overeating and Obesity
Increasing data suggests that variations in dopamine receptors and dopamine release play a role in overeating and obesity. Animal research implicates that when exposed to the same high-fat diet, mice with lower dopamine D2 receptor density in the putamen show more weight gain than mice with higher D2 receptor density in this region (Huang et al. 2006). A transgenic mouse with persistently elevated striatal dopamine displayed increased food intake and increased incentive motivation to consume food (Orosco et al. 1996). Compared to lean Zucker rats, obese Zucker rats, which have defective leptin receptor function, have fewer D2 receptors and reduced hypothalamic dopamine activity when fasting, but release more phasic dopamine when eating and do not stop eating in response to insulin and glucose administration (Orosco et al. 1996). In addition, D2 receptor blockade causes obese, but not lean, Zucker rats to overeat (Fetissov et al. 2002), implying that blockade of already low D2 receptor availability may increase the incentive value of food in obese rats. Obesity-prone (DIO) Sprague-Dawley rats, compared to the obesity-resistant strain, also have reduced dopamine turnover in the hypothalamus compared to the obesity-resistant strain before they become obese, and develop obesity only when given a palatable high-energy diet (Levin and Meynell 2002). When exposed to the same high-fat diet, mice with lower D2 receptor density in the putamen show more weight gain than mice with higher D2 receptor density in this region (Huang et al. 2006).
Positron emission tomography (PET) studies suggest that obese versus lean adults show less striatal D2 receptor binding (Volkow et al. 2008), and that D2 receptors are reduced in the striatum in morbidly obese individuals in proportion to their body mass (Wang et al. 2001). Lower D2 striatal receptor density is also correlated with lower resting metabolism in the prefrontal cortex, which may contribute to overeating because of reduced inhibitory control (Volkow et al. 2008). These results echo evidence that substance abuse is associated with low D2 receptor density and less sensitivity of corticolimbic reward circuitry in response to general reinforcers, such as money (Goldstein et al. 2007), and also evidence that experimentally increased expression of D2 receptors reduces alcohol self-administration in rats (Thanos et al. 2001).
Using functional magnetic resonance imaging (fMRI), we found that obese relative to lean adolescents show weaker activation in dopamine-target regions (caudate and putamen) in response to food intake, and that those showing reduced striatal response to food intake who had an A1 allele of the TaqIA (DRD2/ANKK1) gene, which is associated with lower striatal D2 receptor density and attenuated striatal dopamine signaling, were at elevated risk for weight gain over a 1-year follow-up (Stice et al. 2008a,b). Because BOLD responses were measured, we can only speculate that the effects reflect lower D2 receptor density. This interpretation seems reasonable because the presence of the Taq1A A1 allele, which has been associated with reduced dopaminergic signaling in several postmortem and PET studies (Ritchie and Noble 2003; Tupala et al. 2003), significantly moderated the observed BOLD effects. Yet, the blunted striatal activation may also implicate altered dopamine release from food intake rather than a lower D2 receptor density (Knutson and Gibbs 2007). Research has also found that obese rats (due to a cafeteria diet) had lower extracellular dopamine and lower amphetamine-induced dopamine release (Geiger et al. 2009). Furthermore, obese individuals show greater activation in the insula and anterior cingulate cortex in response to food receipt relative to healthy controls (Stice et al. 2008b). Although the above-mentioned data suggest that obese versus lean individuals have fewer striatal D2 receptors available and process food reward differently, there are key gaps in the literature. First, existing studies in humans have used either fMRI measures of responses to food or PET measures of dopamine binding, but have never measured both in the same participants. Thus, it is unclear to what extent the fMRI results are dependent on dopamine mechanisms. It is possible that the blunted striatal activation may also implicate altered dopamine release from food intake rather than a lower D2 receptor density. It is theorized that consumption of high-fat, high-sugar diet leads to downregulation of D2 receptors (Small et al. 2003) and reduced dopamine turnover (Davis et al. 2008). In support, animal studies suggest that repeated intake of sweet and fatty foods results in downregulation of postsynaptic D2 receptors, increased D1 receptor binding, and decreased D2 sensitivity (Bello et al. 2002; Kelley et al. 2003), changes that also occur in response to chronic substance abuse. As well, experimental exposure to a high-fat diet results in reduced response to psychostimulants and meso-limbic dopamine turnover (Davis et al. 2008; Wellman et al. 2007). Paradoxically, regular exposure to high-sugar food results in subsequent increases in sugar intake (Avena et al. 2008), despite the changes to dopamine circuitry observed by others from repeated sugar intake (Bello et al. 2002; Kelley et al. 2003). To date, no PET imaging study has tested whether obese humans show greater dopamine release in response to food intake relative to lean humans. Accordingly, it will be important to investigate dopamine release in response to food intake in obese versus lean individuals. A second gap in the literature is that research has not tested whether abnormal responsivity of reward circuitry increases risk for future weight gain. Therefore, it is important for future studies to characterize dopaminergic synaptic function in humans and to examine its effects on future weight gain. Finally, striatal dopamine is thought to encode a reward prediction error signal (the difference between actual and expected reward), as demonstrated by numerous animal and human studies (Bayer and Glimcher 2005). Therefore, reduced BOLD signal upon food receipt may result from increased reward anticipation and hence a reduced reward prediction error signal (Hare et al. 2008).
3 Genetic Variation in Dopaminergic Reward in Humans
Given that dopamine plays a key role in reward circuitry and is involved in feeding behavior (Small et al. 2003; Yamamoto 2006), it follows that genetic polymorphisms that affect the availability and release of dopamine and the expression or functioning of dopamine receptors could influence the risk for weight gain. Research has identified several genes that influence dopamine functioning, including those that affect dopamine receptors, transport, and breakdown.
3.1 The Taq1A Polymorphism of the DRD2 Gene
To date, the most empirical support has emerged for the Taq1A polymorphism of the DRD2 gene. The Taq1A polymorphism has three allelic variants: A1/A1, A1/A2, and A2/A2. Taq1A was originally thought to be located in the 3′-untranslated region of DRD2, but it actually resides in the neighboring ANKK1 gene (Fossella et al. 2006). Postmortem and PET studies suggest that individuals with one or two copies of the A1 allele have 30–40% fewer D2 receptors when compared to those without an A1 allele (Ritchie and Noble 2003; Tupala et al. 2003). There is emerging evidence that the relation between abnormalities in food reinforcement and amount eaten is moderated by the A1 allele. Epstein and colleagues (Epstein et al. 2004, 2007) found an interaction between A1 allele and individual differences in food reward in adults, such that the greatest ad lib food intake occurred in those who reported more reinforcement from food and who had the A1 allele. Individuals with the A1 allele report greater food craving and work harder for food than those without this allele (Epstein et al. 2007; Comings et al. 1993). Those with the A1 allele versus those without it are also more likely to abuse drugs and to experience greater cue-induced cravings for cigarettes and heroin (Li et al. 2006; Erblich et al. 2005).
Some (Spitz et al. 2000; Thomas et al. 2001), but not all (Southon et al. 2003), studies have found positive correlations between the A1 TaqIA allele and body mass index (BMI; weight in kg/height in m2). Stice et al. (2008a) found that the relation between fMRI activation in response to anticipated and actual eating (e.g., weaker caudate activation in response to milkshake receipt) was significantly more strongly related to current BMI and future weight gain over a 1-year follow-up in those with the A1 allele versus those without it. Using another fMRI experimental paradigm, Stice et al. (2010) found that weaker activation of the frontal operculum, lateral orbitofrontal cortex, and striatum in response to imagined eating of appetizing foods, versus imagined eating of less palatable foods or drinking water, predicted elevated weight gain for those with the A1 allele. Kirsch et al. (2006) found an increase of reward circuitry activation in response to the dopamine D2 receptor agonist bromocriptine in individuals with an A1 allele, but not A2/A2 carriers, and furthermore that the former showed improved behavioral performance in response to bromocriptine, implying that individuals with an A1 allele are more sensitive to dopamine agonists. Collectively, these data suggest that low D2 receptor density associated with the A1 TaqIA DRD2 allele is related to increased ad lib food intake, weight gain, and risk for obesity overeating and risk for obesity.
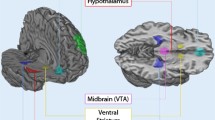
3.2 Variants in the DRD4 Gene
DRD4 is a postsynaptic dopamine receptor whose principal action is to inhibit the second messenger adenylate cyclase. D4 receptors are predominantly localized in areas that are innervated by meso-cortical projections from the ventral tegmental area (VTA), including the prefrontal cortex, cingulate gyrus, and insula (Noain et al. 2006). The 7-repeat or longer allele of this gene (DRD4-L) has been linked to reduced dopamine functioning in an in vitro study (Asghari et al. 1995), to weaker response to dopamine-stimulating drugs (Hamarman et al. 2004), and to less dopamine release in the ventral caudate and nucleus accumbens after nicotine use (Brody et al. 2006), suggesting it may affect reward sensitivity. Adults with the DRD4-L allele versus without it have shown stronger food cravings in response to food cues (Sobik et al. 2005), stronger smoking cravings and fMRI activation of the superior frontal gyrus and insula in response to smoking cues (McClernon et al. 2007), stronger alcohol cravings and fMRI activation in the OFC, anterior cingulate gyrus, and striatum in response to alcohol (Hutchison et al. 2002; Filbey et al. 2008), and greater heroin craving in response to heroin cues (Shao et al. 2006). Weaker activation of the frontal operculum in response to imagined eating of appetizing foods, versus imagined eating of less palatable foods or drinking water, predicted elevated weight gain for those with the DRD4-L allele (Stice et al. 2010). Presence of the DRD4-L allele has also been associated with higher maximum BMI in humans at risk for obesity, including individuals with seasonal affective disorder who report overeating, individuals with bulimia nervosa (Kaplan et al. 2008; Levitan et al. 2004), and African-American adolescents (Guo et al. 2007).
3.3 Variants in the Dopamine Transporter
Phasically released dopamine is normally eliminated by rapid reuptake into presynaptic terminals through the dopamine transporter (DAT), which is abundant in the striatum (Floresco et al. 2003). Lower DAT expression, which is associated with a 10 repeat allele (DAT-L), may reduce synaptic clearance and produce higher basal, or tonic, dopamine levels and blunted phasic dopamine release (Brody et al. 2006). Pecina et al. (2003) found that a DAT knockdown mouse with increased extracellular dopamine displayed increased energy intake and preference for palatable foods. In a study of normal mice, a high-fat diet significantly decreased DAT density in the dorsal and ventral parts of the caudate and putamen compared to a low-fat diet (South and Huang 2008). Lower striatal DAT levels also have been associated with elevated BMI in humans (Chen et al. 2008). DAT-L has been associated with obesity in African-American smokers, versus smokers of other ethnic groups (Epstein et al. 2002).
3.4 Variants in the Catechol-O-Methyltransferase Gene
Catechol-O-methyltransferase (COMT) also has been implicated in the regulation of dopamine signaling. COMT regulates extra-synaptic dopamine breakdown, which occurs predominantly in the prefrontal cortex but also plays a factor in the striatum (Matsumoto et al. 2003). A single nucleotide exchange in the COMT gene, a valine to methionine substitution (Val/Met-158), is associated with a fourfold reduction in COMT activity in humans. There is some evidence that individuals with the Met-allele (low enzyme activity) had relatively higher tonic dopamine levels in prefrontal and striatal regions, but reduced phasic dopamine release in the striatum (Bilder et al. 2004). However, both pharmacological and genetic manipulations of COMT (Gogos et al. 1998) have clarified its role in dopamine metabolism in rodents. Under basal physiological circumstances, both COMT inhibition and genetic deficiencies of COMT have little effect on DA concentrations in the striatum (Bilder et al. 2004). Indeed, individuals with the Met-allele versus without it showed less phasic release of dopamine in response to cigarette smoking (Brody et al. 2006). Although one study involving patients with eating disorders found that individuals with the Met-allele reported elevated bulimic symptoms than those without this allele (Sobik et al. 2005), another study found that individuals with bulimia nervosa were marginally less likely to have a Met-allele than healthy controls (Mikolajczyk et al. 2006). Interestingly, individuals with the Val/Val genotype also showed a preference for an immediate reward versus a larger, delayed reward as well as greater activity levels in the dorsal prefrontal cortex and posterior parietal cortex (Boettiger et al. 2007), suggesting an important interplay between reward sensitivity and impulsivity.
3.5 AKT
AKT (also known as protein kinase B) is a protein kinase effector that acts downstream of the phosphatidylinositol 3-kinase (PI3K)-dependent intracellular signaling pathway. Over-expression of AKT decreases DAT expression (Garcia et al. 2005). Furthermore, the functioning of AKT is regulated by insulin; indeed, AKT appears to represent the primary pathway through which insulin affects dopamine transmission, including the amount of dopamine released during exposure to amphetamine (Williams et al. 2007). This effect is mediated through changes in both the membrane-surface expression and the functionality of DAT. The importance of the AKT for amphetamine responsivity is demonstrated by the ability of the AKT1 inhibitor LY294002 to block amphetamine-induced dopamine release and reuptake (Williams et al. 2007). There is also evidence that phosphorylation of the AKT substrate PRAS40 is markedly reduced in rats fed a high-fat diet (Nascimento et al. 2007), suggesting a mechanism through which diet may influence DAT expression and dopamine release. Given this combination of clinical and preclinical data, AKT1 may be an important candidate for understanding genetic relations between dopamine functioning and overeating.
4 Appetite-Regulating Hormones and Peptides
Beyond the genetic polymorphisms affecting dopamine functioning, there are several hormones and peptides that may exert a direct influence on dopamine functioning and therefore moderate the relation between dopamine and overeating. For instance, the phasically released orexigenic agents ghrelin and orexin A (hypocretin A), both of which enhance appetite, have direct influences on dopamine functioning. Ghrelin binds to neurons in the VTA, increases dopamine neuronal activity, and increases dopamine turnover in the nucleus accumbens (Abizaid et al. 2006). Orexin A increases dopamine firing (Korotkova et al. 2006) and causes increased release of dopamine both in prefrontal regions (Vittoz and Berridge 2006) and in the nucleus accumbens shell (Narita et al. 2006). In addition to increasing dopamine firing and release, injection of orexin into the VTA leads to behavioral changes associated with dopamine stimulation (Narita et al. 2006). In contrast, neuropeptide Y has been found to inhibit dopamine neurons in the VTA (Korotkova et al. 2006). Leptin and insulin, which produce more tonic influences on appetite, also show relations with dopamine functioning in animal studies. Critically, leptin robustly modulates brain reward circuitry, as it has been found to alter operant response rates for rewarding brain stimulation (Fulton et al. 2000; Fulton et al. 2004), reverse the effect of food deprivation on the reinstatement of drug-seeking behavior (Shalev et al. 2001), and block conditioned place-preference for high-fat diets (Figlewicz et al. 2003). It may also provide direct or indirect effects on dopamine responsiveness to psychostimulants, although its immediate effects in normal ad lib-fed rodents are limited (Cota et al. 2006; Hao et al. 2004). Insulin exerts a direct effect on the DAT, by increasing DAT function (and dopamine uptake) (Patterson et al. 1998; Carvelli et al. 2002). Indeed, there may be a direct effect of insulin in the activation of reward circuitry by amphetamine, as insulin appears to prevent amphetamine-induced cell surface redistribution of DAT (Garcia et al. 2005; Carvelli et al. 2002). As noted, insulin’s action on DAT is mediated by AKT1 (Garcia et al. 2005). Taken together, these data highlight the potential links between appetite-regulating hormones, dopamine functioning, and striatal responsivity. Yet, few studies have examined these relations in humans.
5 Conclusion
Overall data suggest that low levels of dopamine D2 receptors and attenuated responsivity of dopamine-target regions (e.g., striatum) to food intake are associated with increased eating and elevated weight. There is also growing (although partially) mixed evidence that genotypes that appear to lead to reduced dopamine signaling (e.g., DRD2, DRD4, and DAT) and certain appetite-related hormones and peptides (e.g., ghrelin, orexin A, leptin) moderate the relation between dopamine signaling, overeating, and obesity. However, there are several gaps in the literature for future studies to address. First, because existing studies in humans have used either fMRI measures of responses to food or PET measures of dopamine binding, but have never measured both in the same participants, it is unclear to what extent the fMRI findings are dependent on dopamine mechanisms and whether this explains the differential responsivity in obese versus lean individuals. It will be important for future studies to integrate measurement of dopamine functioning with fMRI measures of striatal and cortical responses to food. Second, although there is emerging evidence that reduced responsivity of brain regions implicated in food reward increases risk for future weight gain in individuals who appear to be at genetic risk for attenuated dopamine signaling by virtue of DRD2 and DRD4 genotypes, it will be important to replicate these relations in independent studies with larger sample sizes. Third, it is also important to characterize the relations between specific parameters of dopaminergic synaptic function, such as dopamine receptor density, basal extracellular dopamine levels, and phasic dopamine release, and genotypes, hormones, and peptides that influence dopamine functioning to eating and unhealthy weight gain. Finally, future research should continue exploring factors that moderate the risk conveyed by abnormalities in reward circuitry in response to food reward, as such abnormalities have been implicated in obesity as well as substance abuse and pathological gambling. Interestingly, there is some evidence that obese individuals show a decreased risk of substance use and abuse (Simon et al. 2006; Warren et al. 2005), suggesting that routinely engaging in one reinforcing behavior may reduce the probability of turning to another reinforcing behavior. It is hoped that an improved understanding of the role of dopamine-based reward circuitry as well as factors that influence the functioning of this circuitry will inform the design of more effective preventive and treatment interventions for obesity.
References
Abizaid A, Liu ZW, Andrews ZB, Shanabrough M, Borok E, Elsworth JD, Roth RH, Sleeman MW, Picciotto MR, Tschop MH, Gao XB, Horvath TL (2006) Ghrelin modulates the activity and synaptic input organization of midbrain dopamine neurons while promoting appetite. J Clin Investig 116:3229–3239
Asghari V, Sanyal S, Buchwaldt S, Paterson A, Jovanovic V, Van Tol HH (1995) Modulation of intracellular cyclic AMP levels by different human dopamine D4 receptor variants. J Neurochem 65:1157–1165
Avena NM, Rada P, Hoebel BG (2008) Underweight rats have enhanced dopamine release and blunted acetylcholine response in the nucleus accumbens while bingeing on sucrose. Neuroscience 16:865–871
Bayer HM, Glimcher PW (2005) Midbrain dopamine neurons encode a quantitative reward prediction error signal. Neuron 47(1):129–141
Bello NT, Lucas LR, Hajnal A (2002) Repeated sucrose access influences dopamine D2 receptor density in the striatum. Neuroreport 13(12):1575–1578
Berridge KC, Robinson TE (1998) What is the role of dopamine in reward: hedonic impact, reward learning, or incentive salience? Brain Res Brain Res Rev 28(3):309–369
Bilder R, Volavka J, Lachman H, Grace A (2004) Relations to the tonic-phasic dopamine hypothesis and neuropsychiatric phenotypes. Neuropsychopharmacology 29(11):1943–1961
Blackburn JR, Phillips AG, Jakubovic A, Fibiger HC (1989) Dopamine and preparatory behavior: a neurochemical analysis. Behav Neurosci 103:15–23
Boettiger CA, Mitchell JM, Tavares VC, Robertson M, Joslyn G, D'Esposito M, Fields HL (2007) Immediate reward bias in humans: fronto-parietal networks and a role for the catechol-O methyltransferase 158(Val/Val) genotype. J Neurosci 27(52):14383–14391
Bowirrat A, Oscar-Berman M (2005) Relationship between dopaminergic neurotransmission, alcoholism, and reward deficiency syndrome. Am J Med Genet B Neuropsychiatr Genet 132(1):29–37
Brody AL, Mandelkern MA, Olmstead RE, Scheibal D, Hahn E, Shiraga S, Zamora-Paja E, Farahi J, Saxena S, London ED, McCracken JT (2006) Gene variants of brain dopamine pathways and smoking-induced dopamine release in the ventral caudate/nucleus accumbens. Arch Gen Psychiatry 63:808–816
Carvelli L, Moron JA, Kahlig KM, Ferrer V (2002) PI 3-kinase regulation of dopamine uptake. J Neurochem 81:859–869
Chen PS, Yang YK, Yeh TL, Lee IH, Yao WJ, Chiu NT, Lu RB (2008) Correlation between body mass index and striatal dopamine transporter availability in healthy volunteers: a SPECT study. Neuroimage 40:275–279
Comings DE, Flanagan SD, Dietz G, Muhleman D, Knell E, Gysin R (1993) The dopamine D2 receptor (DRD2) as a major gene in obesity and height. Biochem Med Metab Biol 50(2):176–185
Cota D, Barrera JG, Seeley RJ (2006) Leptin in energy balance and reward: two faces of the same coin? Neuron 51:678–680
Davis JF, Tracy AL, Schurdak JD, Tschöp MH, Lipton JW, Clegg DJ, Benoit SC (2008) Exposure to elevated levels of dietary fat attenuates psychostimulant reward and mesolimbic dopamine turnover in the rat. Behav Neurosci 122(6):1257–1263
Epstein LH, Jaroni JL, Paluch RA, Leddy JJ, Vahue HE, Hawk L, Pl W, Shields PG, Lerman C (2002) Dopamine transport genotype as a risk factor for obesity in smokers. Obesity 10:1232–1240
Epstein LH, Wright SM, Paluch RA, Leddy JJ, Hawk LW, Jaroni JL, Saad FG, Crystal-Mansour S, Shields PG, Lerman C (2004) Relation between food reinforcement and dopamine genotypes and its effect on food intake in smokers. Am J Clin Nutr 80:82–88
Epstein LJ, Leddy JJ, Temple JL, Faith MS (2007) Food reinforcment and eating: a multilevel analysis. Psychol Bull 133:884–906
Erblich J, Lerman C, Self DW, Diaz GA, Bovbjerg DH (2005) Effects of dopamine D2 receptor (DRD2) and transporter (SLC6A3) polymorphisms on smoking cue-induced cigarette craving among African American smokers. Mol Psychiatry 10:407–414
Fetissov SO, Meguid MM, Sato T, Zhang LH (2002) Expression of dopaminergic receptors in the hypothalamus of lean and obese Zucker rates and food intake. Am J Physiol Regul Integr Comp Physiol 283:905–910
Figlewicz DP, Evans SB, Murphy J, Hoen M, Baskin DG (2003) Expression of receptors for insulin and leptin in the ventral tegmental area/substantia nigra (VTA/SN) of the rat. Brain Res 964(1):107–115
Filbey FM, Ray L, Smolen A, Claus ED, Audette A, Hutchison K (2008) Differential neural response to alcohol priming and alcohol taste cues is associated with DRD4 VNTR and OPRM1 genotypes. Alcohol Clin Exp Res 32:1–11
Floresco SB, West AR, Ash B, Moore H, Grace AA (2003) Afferent modulation of dopamine neuron firing differentially regulates tonic and phasic dopamine transmission. Nat Neurosci 6:968–973
Fossella J, Green AE, Fan J (2006) Evaluation of a structural polymorphism in the ankyrin repeat and kinase domain containing 1 (ANKK1) gene and the activation of executive attention networks. Cogn Affect Behav Neurosci 6:71–78
Fulton S, Woodside B, Shizgal P (2000) Modulation of brain reward circuitry by leptin. Science 287:125–128
Fulton S, Richard D, Woodside B, Shizgal P (2004) Food restriction and leptin impact brain reward circuitry in lean and obese Zucker rats. Behav Brain Res 155:319–329
Garcia BG, Wei Y, Moron JA, Lin RZ, Javitch JA, Galli A (2005) Akt is essential for insulin modulation of amphetamine-induced human dopamine transporter cell-surface redistribution. Mol Pharmacol 68:102–109
Geiger BM, Haburcak M, Avena NM, Moeyer MC, Hoebel BG, Photos EN (2009) Deficits of mesolimbic dopamine neurotransmission in rat dietary obesity. Neuroscience 159(4):1193–1199
Gogos JA, Morgan M, Luine V, Santha M, Ogawa S, Pfaff D et al (1998) Catechol-O-methyltransferase-deficient mice exhibit sexually dimorphic changes in catecholamine levels and behavior. Proc Natl Acad Sci U S A 95:9991–9996
Goldstein R, Klein A, Tomasi D, Zhang L, Cottone L, Maloney T et al (2007) Is decreased prefrontal cortical sensitivity to monetary reward associated with impaired motivation and self-control in cocaine addiction? Am J Psychiatry 164:43–51
Guo G, North KE, Gorden-Larsen P, Bulik CM, Choi S (2007) Body mass, DRD4, physical activity, sedentary behavior, and family socioeconomic status. Obesity 15:1199–1206
Hamarman S, Fossella J, Ulger C, Brimacombe M, Dermody J (2004) Dopamine receptor 4 (DRD4) 7-repeat allele predicts methylphenidate dose response in children with attention deficit hyperactivity disorders: a pharmacogenetic study. J Child Adolesc Psychopharmacol 14:564–574
Hao J, Cabeza DV, Carr KD (2004) Effects of chronic ICV leptin infusion on motor-activating effects of D-amphetamine in food-restricted and ad libitum fed rats. Physiol Behav 83:377–381
Hare TA, O'Doherty J, Camerer CF, Schultz W, Rangel A (2008) Dissociating the role of the orbitofrontal cortex and the striatum in the computation of goal values and prediction errors. J Neurosci 28(22):5623–5630
Huang XF, Zavitsanou K, Huang X, Yu Y, Wang H, Chen F, Lawrence AJ, Deng C (2006) Dopamine transporter and D2 receptor binding densities in mice prone or resistant to chronic high fat diet-incuded obesity. Behav Brain Res 175:415–419
Hutchison KE, McGeary J, Smolen A, Bryan A, Swift RM (2002) The DRD4 VNTR polymorphism moderates craving after alcohol consumption. Health Psychol 21:139–146
Kaplan AS, Levitan RD, Yilmaz Z, Davis C, Tharmalingam S, Kennedy JL (2008) A DRD4/BDNF gene-gene interaction associated with maximum BMI in women with bulimia nervosa. Int J Eat Disord 41:22–28
Kelley AE, Will MJ, Steininger TL, Zhang M, Haber SN (2003) Restricted daily consumption of a highly palatable food (chocolate Ensure(R)) alters striatal enkephalin gene expression. Eur J Neurosci 18(9):2592–2598
Kirsch P, Reuter M, Mier D, Lonsdorf T, Stark R, Gallhofer B et al (2006) Imaging gene-substance interactions: the effect of the DRD2 TaqIA polymorphism and the dopamine agonists bromocriptine on the brain activation during the anticipation of reward. Neurosci Lett 405:196–201
Kiyatkin EA, Gratton A (1994) Electrochemical monitoring of extracellular dopamine in nucleus accumbens of rats lever-pressing for food. Brain Res 652:225–234
Knutson B, Gibbs SE (2007) Linking nucleus accumbens dopamine and blood oxygenation. Psychopharmacology (Berl) 191(3):813–822
Korotkova TM, Brown RE, Sergeeva OA, Ponomarenko AA, Haas HL (2006) Effects of arousal and feeding-related neuropeptides on dopaminergic and GABAergic neurons in the ventral tegmental area of the rat. Eur J Neurosci 23:2677–2685
Levin BE, Meynell AA (2002) Defense of body weight depends on dietary composition and palatability in rats with diet-induced obesity. Am J Physiol Regul Integr Comp Physiol 282:R46–54
Levitan RD, Masellis M, Lam RW, Muglia P, Basile VS, Jain U, Kaplan AS, Tharmakingam S, Kennedy SH, Kennedy JL (2004) Childhood in-attention and dysphoria and adult obesity associated with the dopamine D4 receptor gene in overeating women with seasonal affective disorder. Neuropsychopharmacology 29:179–186
Li Y, Shao C, Zhang D, Zhao M, Lin L, Yan P, Xie Y, Jiang K, Jin L (2006) The effect of dopamine D2, D5 receptor and transporter (SLC6A3) polymorphisms on the cue-elicited heroin craving in Chinese. Am J Med Genet B Neuropsychiatr Genet 141B:269–273
Matsumoto M, Weickert C, Beltaifa S, Kolachana B, Chen J, Hyde TM, Herman MM, Weinberger DR, Kleinman JE (2003) Catechol 0-methyltransferase (COMT) mRNA expression in the dorsolateral prefrontal cortex of patients with schizophrenia. Neuropsychopharmacology 28(8):1521–30
McClernon FJ, Hutchison KE, Rose JE, Kozink RV (2007) DRD4 VNTR polymorphism is associated with transient fMRI-BOLD responses to smoking cues. Psychopharmacology (Berl) 194:433–441
Mikolajczyk E, Smiarowska M, Grzywacz A, Samochowiec J (2006) Association of eating disorders with catechol-O-methyltransferase gene functional polymorphism. Neuropsychobiology 54(1):82–86
Narita M, Nagumo Y, Hashimoto S, Narita M, Khotib J, Miyatake M et al (2006) Direct involvement of orexinergic systems in the activation of the mesolimbic dopamine pathway and related behaviors induced by morphine. J Neurosci 26:398–405
Nascimento EBM, Fodor M, van der Zon GCM, Jazet IM, Meinders AE, Voshol PJ, Vlasblom R, Baan B, Eckel J, Maassen JA, Diamant M, Ouwens DM (2007) Insulin-mediated phosphorylation of the proline-rich AKT substrate PRAS40 is impaired in insulin target tissues of high-fat diet-fed rats. Diabetes Nutr Metab 55(12):3221–3228
Noain D, Avale ME, Wedemeyer C, Calvo D, Peper M, Rubinstein M (2006) Identification of brain neurons expressin the dopamine D4 receptor gene using BAC transgenic mice. Eur J Neurosci 24:2429–2438
Orosco M, Rouch C, Nicolaidis S (1996) Rostromedial hypothalamic monoamine changes in response to intravenous infusions of insulin and glucose in freely feeding obese Zucker rats: a microdialysis study. Appetite 26:1–20
Patterson TA, Brot MD, Zavosh A, Schenk JO, Szot P, Figlewicz DP (1998) Food deprivation decreases mRNA and activity of the rat dopamine transporter. Neuroendocrinology 68:11–20
Pecina S, Cagniard B, Berridge KC, Aldrigde JW, Zhuang X (2003) Hyperdopaminergic mutant mice have higher “wanting” but not “liking” for sweet rewards. J Neurosci 23:9395–9402
Ritchie T, Noble EP (2003) Association of seven polymorphisms of the D2 dopamine receptor gene with brain receptor-binding characteristics. Neurochem Res 28:73–82
Robinson TE, Berridge KC (2000) Intra-accumbens amphetamine increases the conditioned incentive salience of sucrose reward: enhancement of reward “wanting” without enhanced “liking” or response reinforcement. J Neurosci 20:s91–s117
Schultz W, Apicella P, Ljungberg T (1993) Responses of monkey dopamine neurons to reward and conditioned stimuli during successive steps of learning a delayed response task. J Neurosci 13(3):900–913
Shalev U, Yap J, Shaham Y (2001) Leptin attenuates acute food deprivation-induced relapse to heroin seeking. J Neurosci 21:RC129
Shao C, Li Y, Jiang K, Zhang D, Xu Y, Lin L, Wang Q, Zhao M, Jin L (2006) Dopamine D4 receptor polymorphism modulates cue-elicited heroin craving in Chinese. Psychopharmacology (Berl) 186:185–190
Simon G, von Korff M, Saunders K, Miglioretti D, Crane P et al (2006) Association between obesity and psychiatric disorders in the US population. Arch Gen Psychiatry 63:824–830
Small DM, Jones-Gotman M, Dagher A (2003) Feeding-induced dopamine release in dorsal striatum correlates with meal pleasantness ratings in healthy human volunteers. Neuroimage 19:1709–15
Sobik L, Hutchison K, Craighead L (2005) Cue-elicited craving for food: a fresh approach to the study of binge eating. Appetite 44:253–61
South T, Huang XF (2008) High-fat diet exposure increases dopamine D2 receptor and decreases dopamine transporter receptor binding density in the nucleus accumbens and caudate putamen of mice. Neurochem Res 33:598–605
Southon AWK, Sanigorski AM, Zimmet P, Nicholson GC, Kotowicz MA, Collier G (2003) The Taq IA and Ser311 Cys polymorphisms in the dopamine D2 receptor gene and obesity. Diabetes Nutr Metab 16:72–76
Spitz MR, Detry MA, Pillow P, Hu YH, Amos CI, Hong WK, Wu X (2000) Variant alleles of the D2 dopamine receptor gene and obesity. Nutr Res 20:371–380
Stice E, Spoor S, Bohon C, Small DM (2008a) Relation between obesity and blunted striatal response to food is moderated by TaqIA A1 allele. Science 322:449–452
Stice E, Spoor S, Bohon C, Veldhuizen M, Small DM (2008b) Relation of reward from food intake and anticipated intake to obesity: a functional magnretic resonance imaging study. J Abnorm Psychol 117:924–935
Stice E, Yokum S, Bohon C, Marti N, Smolen A (2010) Reward circuitry responsivity to food predicts future increases in body mass: moderating effects of DRD2 and DRD4. Neuroimage 50(4):1618–1625
Thanos PK, Volkow ND, Freimuth P, Umegaki H, Ikari H, Roth G, Ingram DK, Hitzemann R (2001) Overexpression of dopamine receptors reduces alcohol self-administration. J Neurochem 78(5):1094–1103
Thomas GN, Critchley JA, Tomlinson B, Cockram CS, Chan JC (2001) Relationships between the TaqI polymorphism of the dopamine D2 receptor and blood pressure in hyperglycemic and normoglycemic Chinese subjects. Clin Endocrinol 55:605–611
Tupala E, Hall H, Bergström K, Mantere T, Räsänen P, Särkioja T, Tiihonen J (2003) Dopamine D2 receptors and transporters in type 1 and 2 alcoholics measured with human whole hemisphere autoradiography. Hum Brain Mapp 20(2):91–102
Vittoz NM, Berridge CW (2006) Hypocretin/orexin selectively increases dopamine efflux within the prefrontal cortex: involvement of the ventral tegmental area. Neuropsychopharmacology 31:384–395
Volkow ND, Fowler JS, Wang GJ (2002) Role of dopamine in drug reinforcement and addiction in humans: results from imaging studies. Behav Pharmacol 13:355–366
Volkow ND, Wang GJ, Telang F, Fowler JS, Thanos PK, Logan J, Alexoff D, Ding YS, Wong C, Ma Y, Pradhan K (2008) Low dopamine striatal D2 receptors are associated with prefrontal metabolism in obese subjects: possible contributing factors. Neuroimage 42(4):1537–1543
Wang GJ, Volkow ND, Logan J, Pappas NR, Wong CT, Zhu W, Netusil N, Fowler JS (2001) Brain dopamine and obesity. Lancet 357(9253):354–357
Warren M, Frost-Pineda K, Gold M (2005) Body mass index and marijuana use. J Addict Dis 24:95–100
Wellman PJ, Nation JR, Davis KW (2007) Impairment of cocaine self-administration in rats maintained on a high fat diet. Pharmacol Biochem Behav 88:89–93
Williams JM, Owens WA, Turner GH, Saunders C, Dipace C, Blakely RD, France CP, Gore JC, Daws LC, Avison MJ, Galli A (2007) Hypoinsulinemia regulates amphetamine-induced reverse transport of dopamine. PLoS Biol 5(10):e274
Yamamoto T (2006) Neural substrates for the processing of cognitive and affective aspects of taste in the brain. Arch Histol Cytol 69:243–255
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Stice, E., Yokum, S., Zald, D., Dagher, A. (2010). Dopamine-Based Reward Circuitry Responsivity, Genetics, and Overeating. In: Adan, R., Kaye, W. (eds) Behavioral Neurobiology of Eating Disorders. Current Topics in Behavioral Neurosciences, vol 6. Springer, Berlin, Heidelberg. https://doi.org/10.1007/7854_2010_89
Download citation
DOI: https://doi.org/10.1007/7854_2010_89
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-15130-9
Online ISBN: 978-3-642-15131-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)