Abstract
In this chapter, we review human health effects associated with the brominated flame retardants (BFRs) that have constituted the overwhelming majority of BFR production and subsequent exposure in humans. These include tetrabromobisphenol A (TBBPA), hexabromocyclododecane (HBCD), and three commercial mixtures of polybrominated diphenyl ethers (PBDEs), or biphenyl oxides, which are known as decabromodiphenyl ether (DecaBDE), octabromodiphenyl ether (OctaBDE), and pentabromodiphenyl ether (PentaBDE). The primary endpoint of concern appears to be endocrine disruption. Other potential effects include hepatotoxicity and neurotoxicity, the later particularly during development. While the toxicological database for these chemicals is growing, further research is needed to understand potential health effects associated with less-studied PBDE congeners, examine the potential carcinogenicity of HBCD and TBBPA, and investigate the overall toxicity of a number of developing alternative BFRs. The increasing contamination of the environment and people by BFRs coupled with clear evidence of adverse health effects resulting from their exposure highlights the importance of identifying emerging issues and data gaps to fully understand the human health risks.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Endocrine disruption
- Hexabromocyclododecane
- Polybrominated diphenyl ether
- Tetrabromobisphenol A
- Thyroid hormones
1 Introduction
In this chapter, we review the human health effects associated with five BFRs that have constituted the overwhelming majority of BFR production and subsequent exposure in humans. These include tetrabromobisphenol A (TBBPA), hexabromocyclododecane (HBCD), and three commercial mixtures of polybrominated diphenyl ethers (PBDEs), or biphenyl oxides, which are known as decabromodiphenyl ether (DecaBDE), octabromodiphenyl ether (OctaBDE), and pentabromodiphenyl ether (PentaBDE). The majority of data characterizing toxicity in humans are associated with exposures to PBDEs, though limited data are available for both TBBPA and HBCD. For the later compounds, a more comprehensive overview of the data reported in animal studies is provided. For PBDEs, the primary focus is on information reported in humans, though a discussion on the relationship of human to animal data is also included.
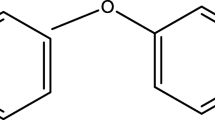
2 Polybrominated Diphenyl Ethers
The majority of laboratory studies on PBDEs published to date have focused on the commercial mixture, PentaBDE, or the individual congeners contained in PentaBDE (primarily BDEs 47 and 99); however, a number of studies are available reporting on exposures to other commercial mixtures, OctaBDE and DecaBDE, or their primary congeners. Similarly, epidemiological studies have also focused on effects associated with exposure to BDEs 47 and 99, as they are the most commonly measured PBDE congeners in humans and tend to be associated with greater toxicity in animal studies relative to other congeners. However, an increasing number of studies have reported on BDEs 100, 153, 154, and 183; very little is still known about the human toxicity of the fully brominated congener, BDE 209. In this section, an overview of the published data in animal studies is provided, followed by a detailed discussion of the health effects observed in humans.
2.1 Health Effects in Laboratory Studies
Although most of the studies on PentaBDE are based on the oral route of exposure, a limited number of studies have demonstrated toxicity following high-dose inhalation exposures and a general lack of toxicity following dermal exposures [1, 2]. Studies in rats and mice consistently indicate that the liver is a target organ following exposure to PentaBDE or OctaBDE congeners. Effects include increased enzymatic activity, increased liver weight, histopathological changes, and disruptions to normal function [3]. Changes in thyroid hormone levels (also a common finding) have been linked to changes in metabolic function of the liver. Although there is a great deal of controversy, a series of studies have demonstrated neurobehavioral effects in mice following exposure to several PentaBDE congeners [4]. Studies in bacteria indicate that PentaBDE is not mutagenic; these data are supported by studies in mammalian cells. A number of in vitro and in vivo studies have also suggested reproductive toxicity and developmental neurotoxicity following exposure to a number of lower brominated BDE congeners.
The most comprehensive study on any PBDE compound was recently completed by the National Toxicology Program [5]. DE-71 was tested using a 2-year bioassay that included carcinogenicity, acute and chronic toxicity, genetic toxicity, and toxicogenomics. Presently, only the subchronic data are available for 13-week exposures. Results indicate adverse toxicity in the liver (the primary target) in both rats and mice as demonstrated by increases in a number of phase I and II enzymes, pathological changes, and increases in liver weight.
The toxicity of OctaBDE compounds has been evaluated in laboratory animals primarily via oral exposure, though toxicity following inhalation has also been assessed. These compounds are generally of low acute toxicity [4]. Toxicities following repeated exposures tend to be in the liver and include induction of hepatic enzymes, increased liver weight, hyperplastic nodules, and enlargement of the liver. Other effects include increases in thyroid weight and altered levels of thyroid hormones. OctaBDE (the commercial mixture itself) does not cause skin or eye irritation, or sensitization in animal studies, nor is it classified as a mutagenic compound based on Salmonella tests. Developmental studies have demonstrated mixed findings, although they suggest the potential for effects related to changes in thyroid hormones. Data have also been published providing suggestive evidence for developmental neurotoxicity [6, 7] associated with a hexa-substituted congener found in OctaBDE (BDE 153). Research studies are not available to characterize chronic exposures, carcinogenicity, or reproductive effects.
DecaBDE, or BDE 209, has been evaluated less often than the other compounds, even though it is the most widespread BDE congener in use. Bacterial tests indicate that BDE 209 is not mutagenic. Additionally, studies in mice suggest evidence for thyroid hormone disruption and delayed developmental neurotoxicity [8]. Neonatal exposure to DecaBDE in mice resulted in a dose-related reduction of serum thyroxine levels in males and delayed development of the palpebral reflex in infants [9], and disruption of normal sex- and age- specific characteristics of spontaneous locomotion in adults. Additionally, impairment in performing behavioral tasks was observed in aging mice following neonatal exposure to DecaBDE, while minimal impairment was observed during young adulthood [10]. Disruption of normal spontaneous behavior has also been reported in other studies on mice and rats following neonatal exposure [7, 11]. In a recent study, Xing et al. [12] showed that exposure to BDE 209 during five different developmental periods could lead to impaired synaptic plasticity in adults, and exposure during lactation was the most sensitive scenario. Chronic, oral exposure studies have demonstrated that very high doses of BDE 209 result in hepatic carcinogenicity in rodents [8, 13]. Additionally, follicular cell hyperplasia incidence increased significantly in male mice, and the incidence of thyroid gland follicular adenomas/carcinomas was slightly increased in treated mice of both sexes.
2.2 Effects in Humans
Studies characterizing potential effects in humans have been relatively limited until recently. As public health interest increases, additional epidemiological investigations are being conducted and published. These studies generally focus on three main outcomes: endocrine disruption, neurotoxicity, and reproductive toxicity (and are discussed as such in this section). The latter two outcomes could both be related to endocrine disrupting effects, lending mechanistic support to the overall findings. The available epidemiological studies tend to be based on key toxicological findings in laboratory studies as well as knowledge about compounds with similar structure, such as the polychlorinated biphenyls (PCBs). It is important to note that none of the available studies evaluated BDE 209, the most highly substituted congener, and thus this congener is excluded from the generalizations and trends discussed in this section.
2.2.1 Thyroid Hormone Disruption
The majority of studies in human populations have evaluated disruption of the endocrine system, and most of the focus has been on disruption of thyroid hormones. This is due mainly to the similarity in structure between PBDEs and thyroid hormones triidothyronine (T3) and thyroxin (T4), and thus the potential for PBDEs to mimic and disrupt homeostatic conditions. Furthermore, data in laboratory studies demonstrate altered levels of thyroid hormones following exposures to PBDEs in rodents. Some studies have also reported hyperplastic changes in the thyroid [14]. Studies in animals have indicated the potential for hydroxylated PBDEs to also interfere with thyroid hormones.
One of the first studies evaluating the potential association between PBDEs and levels of hormones was published by Hagmar et al. in 2001 [15]. These authors assessed associations (after correcting for age) between levels of several persistent organohalogens and a variety of hormones in men who consumed fatty fish from the Baltic Sea. Only two associations were found, one with pentachlorophenol, and a negative association between thyroid-stimulating hormone (TSH) and BDE 47. It is important to note that although the authors noted a relationship, they also stated that given the number of evaluations conducted, there could be some significant correlations that resulted from pure chance. Furthermore, the TSH levels measured in the population were all within normal reference ranges. The author’s ultimate conclusion was that the results suggest that it was very unlikely that even a high consumption of such fish polluted with organohalogens would cause disturbances of circulating hormone levels.
Shortly after this investigation, Mazdai et al. [16] published findings of a small (n = 12), but important study. In a dataset consisting of paired maternal and cord blood samples, the authors reported that fetal concentrations of PBDEs were very similar to that measured in the mother. Thus, the findings demonstrated that for BDEs 47, 99, 100, 153, 154, and 183, maternal serum concentrations are good predictors of fetal exposures. These data are particularly important, given the role of thyroid hormones during development (including in utero). These authors also evaluated thyroid hormones (T3 and T4; total and free) in the paired maternal and fetal samples, though no correlations were found between concentrations of PBDEs and hormone levels. Furthermore, there were no associations between PBDE concentrations or clinical parameters, including infant birth weight.
Another small-scale study in Sweden evaluated thyroid hormones with few significant findings [17]. This group of investigators assessed the concentration of PBDEs in serum and thyroid status in a small group of workers from an electronic recycling facility. Samples were collected from 11 workers before beginning work at the facility, and thereafter at defined intervals, including measurements following vacation periods. Only seven BDE congeners were measured; levels of BDE 47 were highest, followed by 153 and 99. The authors did not find a consistent increase in concentration with increasing length of exposure (employment). Despite a number of approaches for evaluating thyroid hormones, no significant findings were noted when all data were considered; specifically, no correlations were found between PBDE concentrations and T3, T4, or TSH. Limited correlations were observed on an individual level for three workers. However, the authors noted that all of the levels were within the laboratory reference range and also within the normal physiological range. These findings led to the conclusion that no relevant changes were present in relation to PBDE exposures in the study.
Since 2008, there have been an increasing number of well-conducted studies focused on the association between PBDEs and thyroid homeostasis, all of which examined much larger populations. In an interesting study of Chinese workers from an e-waste dismantling site, Yuan et al. [18] evaluated serum concentrations of PBDEs, TSH levels, the frequency of micronucleated binucleated cells, and biomarkers of oxidative stress in blood and urine. The objective was to explore factors that may influence selected biomarkers for exposure to e-wastes. Although the PBDE congeners measured were not stated (results only provided as sums), the authors reported that the median serum concentration was 382 ng/g lipid in the e-waste workers and 158 ng/g lipid in the control group (a group located ~50 km from the e-waste facility). The median serum TSH level was significantly higher in the workers as compared to the control group. The frequency of micronucleated cells was 5% in the exposed group and 0% in the control group, thus suggesting an association between exposures to e-waste and DNA damage. However, no differences were observed for other markers of DNA damage (8-hydroxy-2′-deoxyguanosine levels in urine, or SOD, MDA, and GSH levels). Using logistical regression, the authors reported that working with e-wastes was the only significant predictor of the increased micronucleated cell frequency, and no factors were associated with increased serum TSH levels. The authors concluded that exposures to other compounds (such as PAHs or metals) may have been responsible for the observed genotoxic effects; however, PBDEs were associated with altered levels of TSH, suggesting potential adverse effects to the thyroid hormone system in these workers. More recently, Wang et al. [19] reported that people working in e-waste recycling had significantly lower TSH compared with control groups. Additionally, these authors noted a positive association between BDEs 205 and 126 with levels of T4.
Turyk et al. [20] reported on hormone disruption in adult male sport fish consumers. This group of researchers invited participants from a previously studied cohort of frequent and infrequent consumers of Great Lakes fish to participate in a follow-up study on PBDE exposures. Approximately 300 men provided information on fish consumption, medical diseases, use of medications and supplements, as well as blood and urine samples for the study. All samples were analyzed for thyroid and steroid hormone levels as well as concentrations of PBDEs in an effort to determine whether PBDE body burdens were related to hormone levels. Associations between hormones and ∑PBDE levels (∑PBDE = BDE congeners 28, 47, 49, 85, 99, 100, 138, and 153), as well as BDE 47 alone, were modeled using linear regression with consideration for a number of confounding variables (e.g., body mass index, age, serum lipids, smoking, fish meals, etc.). Dose–response relationships were evaluated for ∑PBDE levels by quartile and for individual BDE congeners 47, 99, 100, and 153 by tertile.
The median ∑PBDE concentration was 38 ng/g lipid (range of 16–1,360 ng/g lipid). ∑PBDE concentrations were positively related to measures of T4 (total T4, free T4, and urinary T4), rT3, and the percentage of T4 bound to albumin. In contrast, ∑PBDE concentrations were inversely related to total T3, TSH, and the percentage of T4 bound to thyroid-binding globulin (TBG). Associations were less apparent and generally inconsistent when evaluated with BDE 47 alone. For both sets of evaluations, statistical significance was often dependent on adjustment for other hormone levels and/or other DDE; thus the associations were difficult to interpret. Dose–response evaluations with ∑PBDE concentrations were also difficult to interpret given the large variability between quartiles; however, the authors reported positive relationships for urinary T4. Only the highest quartile was elevated for free T4, rT3, and T4 binding to serum proteins. Total T3 was negatively associated by quartile. No dose–response relationship was observed for total T4 and TSH. When evaluated by individual congener, urinary T4 was the only parameter that exhibited a positive dose–response relationship with all congeners evaluated. Trends were not apparent or inconsistent for other congeners or parameters.
Importantly, these findings suggest independent pathways for the various BDE congeners evaluated with respect to several effects on thyroid hormones. The authors speculated that some of the observed associations suggested a role of thyroid hormone deiodinases, given their key role in maintaining thyroid homeostasis, and specifically an effect between PBDE exposure and deiodinase activity. The overall conclusion by the authors was that PBDE exposure at levels consistent with those observed in the general US population was associated with increased thyroglobulin antibodies and increased T4 in adult males. However, the authors did not compare the reported hormone or steroid levels to those measured in the general population, and thus the clinical significance of the findings is unclear, particularly considering that none of the cohort participants had diabetes, thyroid disease, or other conditions that could correlate PBDE levels to disease. Their results were initially a surprise, given the lack of consistency with the effects observed in animal studies.
In another study published the same year, Herbstman et al. [21] reported on the relationship(s) between cord serum concentrations of PBDEs and thyroid hormones from cord blood serum and neonatal blood spots in an effort to understand if PBDEs alter umbilical cord levels of thyroid hormones. Furthermore, the authors wanted to understand if the birth delivery mode modified any such associations, given that intrapartum stress could substantially change thyroid hormone levels (and thus potentially mask effects of xenobiotic exposures). Using linear regression, crude and adjusted relationships between log PBDE concentrations (based on individual BDE congeners) and total T4 (TT4), free T4 (FT4), thyrotropin, and TSH were evaluated. Although BDE 100 and 153 were weakly associated with average lower TT4 in cord blood, no significant relationships were observed. When considerations for delivery type (i.e., spontaneous unassisted vaginal delivery [SUVD] vs. all other types) were included in the model, higher levels of three congeners (BDEs 47, 100 and 153) were associated with lower TSH, though the associations were not statistically significant. However, higher concentrations of BDE 100 were significantly associated with lower TT4 in babies born via SUVD. The authors concluded that umbilical cord levels of PBDEs were not associated with higher TSH or FT4. It is of interest to note that this study also evaluated a number of PCB congeners; associations between effects on thyroid hormones and PCBs were much stronger than with PBDEs.
A separate group of researchers also evaluated both PCBs and PBDE exposures with respect to adverse effects on thyroid hormones. Chevrier et al. [22] first evaluated associations between PCB exposures and thyroid hormones in population of pregnant low-income Latina women in California; in a separate study, they evaluated relationships between PBDE concentrations and thyroid function. Based on the data collected in 1999/2000, multiple linear regression models were used to evaluate the relationship between maternal PBDE concentrations and thyroid hormones (and also included analyses based on clinical definitions of maternal hyperthyroidism). Concentrations of PBDEs were lower than those observed in the general US population and were dominated by BDEs 47, 99, 100, and 153 (BDEs 17, 66, 85, 154, and 183 were detected in fewer than 50% of the samples and thus were not considered in the health-based analyses). Associations between PBDEs and free and total T4 were not statistically significant, though both individual congeners and sum PBDEs were inversely associated with TSH levels. Associations were not linear, though when evaluated by quartile, data demonstrated suggestive evidence of a non-monotonic exposure–response relationship (based on increased odds of subclinical hyperthyroidism in the fourth quartile relative to the first). The authors concluded that the data suggest PBDE exposures are associated with lower TSH during pregnancy, and altered thyroid homeostasis has been shown to be particularly harmful to the developing fetus.
A group of researchers in the USA evaluated associations between the concentrations of PBDEs in house dust and hormone levels in a small group of men (n = 24) recruited from an infertility clinic [23]. BDE 47 and 99 were detected in all house dust samples; BDE 100 was detected in 67% of samples. The authors showed that PBDE concentrations in house dust were positively associated with free T4. Because the authors did not evaluate levels of PBDEs in serum, it is very difficult to interpret these findings without direct correlations between dust exposure and serum concentrations in this population, although such a correlation has been seen in other populations. The authors also point out that their results are preliminary and could be due to chance.
When the thyroid hormone disruption data are considered collectively, it is difficult to generate a conclusion given the lack of consistency between studies. Many different populations have been studied worldwide, including both occupationally exposed cohorts and sensitive cohorts (e.g., pregnant women and infants). The difficulties in finding consistencies may be due to the fact that many of the studies did not evaluate the same congeners, nor did they conduct congener-specific analyses, but rather depended on analyses based on the sum of PBDEs measured (which was also not consistent among studies). Furthermore, measurement of thyroid hormones is often subject to a large amount of analytical sensitivity and variability. Importantly, though several of the studies available looked at key parameters, very few evaluated enough parameters (or accessory information) to fully interpret changes in thyroid hormone status. Despite these limitations, the evidence suggests that serum concentrations of PBDEs, and some congeners in particular, are associated with altered levels of thyroid hormones. The data supporting an inverse association with TSH were the strongest, though not all studies consistently reported such. Most studies reported a lack of correlation with T4. Most authors did not evaluate the clinical relevance of changes in thyroid hormone levels – this type of information is a key to determining the impact on human health. Thus, in summary, additional studies are needed to clarify the findings published to date and to further characterize the relationship between PBDE exposure and changes to the endocrine system in humans.
2.2.2 Diabetes
Lim et al. [24] conducted a cross-sectional evaluation of the National Health and Nutrition Examination Survey (NHANES) data in an effort to identify potential associations between BFRs and diabetes and/or metabolic syndrome in the US population. The NHANES dataset is a part of a large-scale biomonitoring effort led by the Centers for Disease Control and Prevention, designed to characterize the health and nutritional status of the general US population. It is often used as the primary source for establishing “reference ranges” of exposure to various environmental compounds; however, the usefulness for evaluating health status is highly dependent on the outcome of interest. In this study, the authors relied on self-reported data regarding medications for treatment of diabetes or measurements of plasma glucose (not all of which were fasting). Similarly, diagnosis of metabolic syndrome was based on meeting various criteria (e.g., fasting glucose, waist circumference). These outcomes were evaluated relative to serum concentrations of BDE congeners that were above the analytical limit of detection in at least 60% of the study population; thus analyses were limited to BDEs 28, 47, 99, 100, and 153. Participants with serum concentrations less than the limit of detection were used as the reference group; the remaining participants were evaluated by quartiles using logistic regression models.
After adjusting for several confounding variables, there was a nonlinear association with diabetes for BDE 153. Statistically significant associations were not observed for the other congeners. A similar finding was noted by the authors for metabolic syndrome: only BDE 153 showed a weak association, though it was a U-shaped curve when evaluated by quartile. The authors state that the findings should be interpreted with caution due to the cross-sectional nature of the study and because of multiple comparison intrinsic to the dataset (e.g., complex weighting, many compounds evaluated, etc).
2.2.3 Neurotoxicity
A handful of studies have been published recently addressing neurotoxicity outcomes in human populations and potential associations with PBDE exposures. These types of studies are a result of laboratory studies in rodents indicating the potential for neurotoxicity following developmental exposure to several BDE congeners (reviewed by [25]), and also because of structural similarity to known neurotoxic substances, particularly PCBs. The first study was published in 2009 by Roze et al. [26] and was based on findings from a prospective cohort study evaluating neuropsychological function in 62 children in the Netherlands. Blood levels of ten organohalogen compounds including BDEs 47, 99, 100, 153, and 154, as well as HBCD were measured in mothers during the 35th week of pregnancy. Thyroid hormones were also measured in umbilical cord blood samples. At ages 5–6, children were then evaluated for motor performance (coordination, fine motor skills), cognition (intelligence, visual perception, visuomotor integration, inhibitory control, verbal memory, and attention), and behavior. Correlations were evaluated between the concentrations of the organohalogen compounds in the mothers before birth and the functional analyses in children, both with and without correction for socioeconomic status, sex, and home observation for measurement (HOME, which the authors indicated may exert an influence on the cognition and behavior of the children).
The authors reported that brominated flame retardants (BFRs) were correlated with worse fine manipulative abilities, worse attention, better coordination, better visual perception, and better behavior. The congener-specific data without corrections showed that BDE 47 was negatively associated (described as a worse outcome) with sustained attention, but positively associated (described as a better outcome) with internalizing behavior, total behavior outcome, and coordination. BDE 99 was positively correlated with internalizing behavior and total behavioral outcome. BDE 100 was positively associated with coordination, internalizing behavior, externalizing behavior, and total behavioral outcome. BDE 153 was positively correlated with visual perception. BDE 154 was negatively correlated with fine manipulative abilities, and HBCD was positively associated with coordination. Thus, the majority of outcomes with significant correlations were positive (11 of 13); only BDE 47 and BDE 154 exhibited negative correlations. When the data were corrected for SES, sex, and HOME, 16 correlations were noted for the BFRs in this study. All significant correlations with HBCD were positive (coordination, total intelligence, and verbal intelligence). BDE 153 was negatively associated with verbal memory. BDEs 47, 99, and 100 were negatively associated with sustained attention. BDE 47 was positively associated with selective attention and internalizing behavior. BDEs 99 and 100 were positively associated with total behavior outcome and internalizing behavior.
Regarding the conflicting (positive and negative) correlations between BFRs and outcome, the authors stated “it is difficult to determine implications of these results for functioning later in life.” The authors also noted that it was difficult to determine which effects could reliably be assigned to the specific contaminants, particularly considering colinearity issues. Furthermore, many other contaminants, such as methyl mercury (a known developmental toxicant), may also have played a role (but were not measured in the current study). Thus, given the conflicting nature of the results and limitations in the study design, the findings are difficult to interpret with respect to evaluating human health risk.
In an effort to follow-up on animal studies suggesting neurodevelopmental effects following exposures to PBDEs, Herbstman et al. [27] conducted a prospective cohort study to evaluate the potential associations between prenatal exposure to PBDEs and neurodevelopment. The authors relied on a cohort initiated after 11 September 2001, of women and their children from New York (USA). In total, 210 cord blood samples were collected and analyzed for PBDEs. Approximately half this number participated in subsequent neurodevelopmental testing in children between 12–48 and 72 months of age (note: a different number of children were tested at each age). Median cord plasma concentrations of BDE 47, 99, and 100 were 12.1, 3.5, and approximately 1.5 ng/g lipid, respectively. PBDE concentrations were evaluated in a cross-sectional analysis using multivariate linear regression to determine associations with Psychomotor Development Index (PDI), Mental Development Index (MDI), full IQ scores, verbal IQ scores, and performance IQ scores. MDI and PDI were evaluated at 12, 24, and 36 months of age, whereas IQ tests were performed at 48 and 72 months of age.
A number of negative associations were found for BDEs 47, 99, 100, and 153; however, only a few were statistically significant. For BDE 47, these included the 12-month PDI (not a strong association), 24-month MDI, and 48-month full and verbal IQ scores. For BDE 99, the 24-month MDI was the only neurodevelopmental endpoint significantly impacted. BDE 100 concentrations were negatively associated with 24-month MDI, 48-month full, verbal and performance IQ scores, as well as 72-month performance IQ scores. And for BDE 153, negative associations were detected for the 48-month and 72-month full and performance IQ scores. The authors reported that for every ln-unit change in BDE 47, 100, or 153, IQs were several points lower. The authors also compared the mean scores from children in the upper 20% of the prenatal exposure distribution to those in the lower 80% and found that generally children with higher PBDE concentrations scored lower than the rest of the population in the neurodevelopmental tests.
The findings reported by Herbstman et al. [27] are consistent with toxicological data published in animal studies, thus lending confidence to these findings with the support of biological plausibility. However, not all trends observed in animal studies were observed by Herbstman et al. [27], suggesting differential mechanisms and/or effects between species. These data are important and demonstrate that additional research is required to understand potential associations, particularly considering a number of the confounders that limit the interpretation of the current dataset (e.g., the authors noted that the associations were impacted by maternal education, breastfeeding, etc). However, when considered collectively, these two studies suggest the potential for neurodevelopmental effects associated with exposures to PBDEs, though the type and severity of effects warrant further assessment.
Using these data, along with data from animal studies, Messer [28] proposed that PBDEs could play a role as risk factors for autism or other disorders of brain development and briefly overviews some of the data to support this hypothesis. The premise of the mini-review leans on data demonstrating endocrine disruption in both animals and humans as a possible mechanistic link between observed neurobehavioral effects observed in rodents. The author also describes further testing paradigms that would be useful for better understanding the potential adverse effects of PBDE exposure, particularly as they relate to characterizing health risk in humans. Such studies would include more thorough pharmacokinetic investigations, evaluations of genetic alterations, and chronic toxicity studies in animal models. The author also suggested additional in vitro assays to characterize binding to key receptors in an effort to further understand the mechanistic processes. Collectively, these data are required to understand if PBDE exposure is a risk factor for autism.
2.2.4 Reproductive Toxicity
Several studies have evaluated the downstream impact of endocrine disruption, genetic disturbance, and other potential adverse effects on reproductive toxicity. Main et al. [29] assessed the potential association between concentrations of PBDEs and cryptorchidism in newborn boys; Akutsu et al. [30] reported on findings from a pilot study evaluating PBDE concentrations and potential associations with sperm quality in ten Japanese study participants. A third study has found that maternal PBDE serum concentrations were associated with decreases in fecundability [31]. Furthermore, one study examined house dust PBDE levels and reproductive hormone analyses on men at an infertility clinic [23], though this study did not quantify serum PBDE concentrations.
The authors of the study on cryptorchidism [29] pursued the investigation because of the increasing prevalence of undescended testicles in some areas of the world, and the suspected role of environmental factors – particularly those that interfere with hormonal function. Both breast milk (n = 130) and placenta samples (n = 280) were analyzed as part of a longitudinal cohort study conducted between 1997 and 2001 in Finland and Denmark. In addition to measuring the levels of 14 BDE congeners (28, 47, 66, 71, 75, 77, 85, 99, 100, 119, 138, 153, 154, and 183), in both biological media, levels of gonadotropin, sex hormone-binding globulin (SHBG), testosterone, and inhibin B were also measured. All newborns in the study were evaluated clinically, with specific focus on the position and function of the testes. Serum samples were also drawn from infants at 3 months of age and analyzed for follicle-stimulating hormone (FSH), luteinizing hormone (LH), and SHBG.
Only seven of the fourteen BDE congeners were detected in breast milk samples. Median concentrations of BDE congeners 47, 100, 28, 66, and 154 in breast milk were higher in Danish newborns with cryptorchidism relative to controls, though this trend was not observed in Finnish newborns (who have higher incidences of cryptorchidism). When evaluated together (newborns from both countries), the sum of the seven detected congeners was higher in all newborns with cryptorchidism relative to controls. Serum levels of LH were also correlated with the sum of the seven detected congeners as well as with BDEs 47, 100, and 154; when evaluated by country, this trend was only observed in Finnish newborns. No other endpoints evaluated were significantly associated and correlated with PBDEs.
Very different results were obtained when placental tissue was assessed. Only five BDE congeners were detectable (thus analyses were based on a sum of five vs. seven with breast milk). However, no significant differences in the placenta concentrations of BDES and cryptorchidism were observed. There were also no correlations between placental PBDEs and serum reproductive hormones in the infants. The authors specifically noted that it was not clear why the findings were not in agreement. It is of interest to note that placental lipid content was not correlated with the sum of PBDEs, and that there were positive correlations between measurements in placenta and breast milk, but absolute concentrations in the placenta were approximately three times lower. Clearly, additional analyses are needed to clarify the findings in this study and to further characterize potential effects of PBDE exposures in early life stages.
Findings reported by Akutsu et al. [30] were generally in line with those reported by Main et al. [29]. In this pilot study of sperm quality in ten Japanese participants, only 4 of 29 BDE congeners were consistently detected (47, 99, 100, and 153). The sum concentration of these four congeners was less than 5 ng/g lipid in all participants except one (8.6 ng/g lipid), demonstrating generally very low levels. Individual congeners were evaluated for trends with sperm concentrations and testis size. No significant trends were observed for BDEs 47, 99, and 100. However, the authors reported a significant inverse relationship between both endpoints for BDE 153 (the data was not shown for testis size). These limited data may suggest BDE congeners 47, 99, 100, and 153 act via different mechanisms and/or demonstrate differential potencies with respect to various endpoints. The trend between BDE 153 concentrations and decreased sperm concentrations warrants further investigation.
In a study mentioned earlier in relation to changes in free T4, a group of researchers evaluated PBDEs in house dust and hormone levels in a small group of men (n = 24) recruited from an infertility clinic [23]. With adjusted, multivariable regression models, the authors observed inverse relationships between dust PBDE concentrations and free androgen index, luteinizing hormone and FSH, as well as positive relationships between PBDE concentrations in house dust and levels of inhibin B and SHBG. Again, because the authors did not evaluate levels of PBDEs in serum, it is difficult to interpret these findings.
Harley et al. [31] designed a study aimed at determining potential associations between maternal PBDE serum concentrations during pregnancy and time to pregnancy as well as various menstrual cycle characteristics. The authors focused on BDE congeners 47, 99, 100, 153, and total PBDEs in approximately 200 women from California, USA. Fecundability odds ratios were reduced for BDE 100, 153, and the sum of PBDEs; no effects were noted for the other congeners. No effects were noted for any congeners, or sum congeners, when various parameters associated with the menstrual cycle were examined.
2.2.5 Sensitization
Data characterizing sensitization to PBDEs is limited to two studies with the most fully brominated congener, though details on these studies are limited. One study reported that skin irritation was noted in 9 of 50 human subjects who were exposed to a repeated application of 5% Deca in petrolatum, though the applications did not result in sensitization [32]. Similar findings were reported in a separate study involving repeated Deca exposures to the skin of 200 volunteers; irritation was noted in some participants but no evidence of skin sensitization was observed [32].
2.2.6 Interpretation of Studies in Humans
Data characterizing potential effects association with exposures to PBDEs in humans are becoming increasingly available as initial studies indicate several potential causes for concern. The variability in findings inhibits the ability to make a definitive conclusion; however, when the data are considered collectively, it appears that human populations may be at risk of health effects, primarily endocrine disrupting effects that may manifest as neurotoxic or reproductive outcomes. However, additional research is clearly needed to more fully understand the mechanistic aspects of toxicity following exposures, as well as to more fully understand the quantitative dose–response relationships between exposure and response. A key component to further assessments may also include discussion of both clinical and public health relevance. Furthermore, these data collectively suggest that some BDE congeners are more potent or operate via different mechanisms than others. Investigators should be urged to analyze and publish data on both a congener-specific basis (including BDE209 and other highly brominated congeners) in addition to the sum PBDEs such that the public health arena can better understand and protect humans from adverse effects resulting from PBDE exposure.
2.3 Mechanistic Studies In Vitro Using Human Cell Lines
Many mechanistic studies have been published in the last decade describing responses in human cells or human cell lines following exposures to PBDEs. These can generally be divided into those that characterize toxicity and those that characterize metabolism in vitro. The studies that evaluated toxicity generally focused on key events associated with genotoxicity, endocrine disruption, neurotoxicity, and changes in development, though the majority of such are aimed at determining key events associated with neurotoxicity. These studies have been conducted in a number of cell lines and evaluate a variety of different endpoints, and also evaluate a number of different individual BDE congeners as well as commercial mixtures. Collectively, these studies provide data that aid in understanding the mechanism(s) of action (MOA) associated with the toxicities of PBDEs.
2.3.1 Toxicity
In an effort to understand potential MOA(s) associated with potential neurotoxic effects in vivo and apoptosis in vitro (based on previous studies), Yu et al. [33] evaluated the action of DE-71 on a human neuroblastoma cell line. Dose-dependent effects in cell viability were noted (based on an increase in lactate dehydrogenase leakage and 3-4,5,-dimethylthia-zol-2-yl-2,5-diphenyl-tetrazolium bromide reduction). Using morphological examination and flow cytometry, the authors also reported treatment-related apoptosis and DNA degradation in the cell cycle. Further evaluation suggested that apoptosis was caused by a caspase-dependent pathway (but was not related to oxidative stress). The authors also evaluated intracellular calcium, noting a time-dependent increase in intracellular levels – an effect also noted in many rodent cell culture studies. Additional assessments on cellular mechanisms indicated that DE-71 increased the level of Bax translocation to the mitochondria and stimulated the release of cytochrome c. Although it is difficult to directly translate the findings of this in vitro study in a human cell line to human health risk, the results provide important information regarding potential mechanisms of toxicity following exposure in humans.
Using a somewhat similar approach, He et al. [34] also conducted a mechanistic study in a cell line derived from a human neuroblastoma (SH-SY5Y cells) to evaluate apoptosis in association with exposures to BDE 47 both in the presence and absence of PCB 153. The authors reported that BDE 47 induced apoptosis via multiple pathways. Furthermore, co-exposure to PCB 153 enhanced the effects. The authors suggested that these findings contribute further to understanding potential neurotoxicity associated with PBDE exposures. The effects of BDE 47 were also assessed by Tagliaferri et al. [35], who used two mathematical models to evaluate the interaction between BDE 47 and BDE 99 on viability of neuronal cells. The model suggested synergistic effects below the threshold concentrations of both compounds.
Schreiber et al. [36] used primary fetal human neural progenitor cells (hNPCs) as an in vitro model of neural development to evaluate the potential toxicity of BDEs 47 and 99. The behavior of the selected cell line mimics proliferation, migration, and differentiation, basic processes in brain development. Using micromolar concentrations, the authors reported that these congeners did not alter proliferation, but did cause treatment-related effects on ion migration and differentiation, specifically differentiation into neurons and oligodendrocytes. Because numerous previous studies in rodents have suggested that thyroid hormones play a role in PBDE-induced toxicity, the authors simultaneously exposed the cells to a thyroid hormone receptor agonist and showed that negative effects on migration and differentiation were eliminated. However, addition of an antagonist did not exert an additive or synergistic effect; thus the role of thyroid hormones in this system was unclear. These findings demonstrate that the primary BDE congeners measured in humans have the potential to cause toxicity via this mechanism, though additional research is needed to link the findings from this in vitro study to exposures in the human population.
In an effort to more fully understand PBDE-induced endocrine disruption, developmental neurotoxicity, and changes in fetal development observed in rodent studies, Song et al. [37] evaluated the potential toxicity of two hydroxylated PBDEs in a human adrenocortical carcinoma cell line (H295R). Cells were exposed to 2-OH-BDE47 or 2-OH-BDE85 and evaluated for cell viability/proliferation, DNA damage, cell cycle distribution, and gene expression profiling. Both of the compounds demonstrated dose-dependent cytotoxic effects, though the hydroxylated BDE 85 was more potent. At the micromolar concentrations tested, no DNA damage was observed, thus suggesting a non-genotoxic mechanism of toxicity for these compounds.
Several studies have directly evaluated genotoxic effects in human cell lines. One of the first studies was reported by Reistad and Mariussen [38], in which the authors assessed the formation of reactive oxygen species (ROS) and calcium levels in human neutrophils following exposure to DE-71, OctaBDE, or BDE 47 in vitro. Both DE-71 and BDE 47 induced a dose-dependent production of ROS, whereas no ROS were observed following OctaBDE exposure. Additional investigations of cell signaling indicated a calcium-dependent activation of PKC. Based on the collective findings, the authors postulated that ROS formation was generated via an initial tyrosine kinase-mediated activation of P13K and enhanced activation of calcium-dependent PKC by enhanced PLC activity, which results in a release of intracellular calcium and ROS formation in neutrophils. This information is particularly useful, given the absence of findings with commercial OctaBDE, and positive findings with DE-71 and BDE 47, further supporting the need for congener-based assessment.
A series of similar studies were published by He and colleagues in 2007 and 2008. Hu et al. [43] reported on the antiproliferative, apoptotic properties of BDE 209 in the human hepatoma Hep G2 cell line. Following 72 h of exposure, BDE 209 inhibited cell viability, increased the release of lactate dehydrogenase, and generated ROS, in a concentration-dependent manner (10–100 μM). Morphological changes, cell cycle alterations, and apoptosis supported antiproliferative effects. These findings are in contrast to the trend observed by Reistad and Mariussen [38] in which the higher brominated compounds did not induce ROS in a dose-dependent manner. He et al. [39] also evaluated cytotoxicity and genotoxicity of BDE 47 in human neuroblastoma cells (SH-SY5Y cells) in vitro. Cells were exposed for 24 h to BDE 47 concentrations ranging from 1 to 8 μg/ml, and then evaluated for cell viability, proliferation, lactate dehydrogenase leakage, ROS formation, cell apoptosis, DNA breakage, and cytogenic damage. Under the conditions of this assay, BDE 47 inhibited cell viability, increased LDH leakage, and induced cell apoptosis at concentrations ≥4 μg/ml. Concentration-dependent increases in ROS and DNA damage were observed. Based on these findings, the authors concluded that BDE 47 was cytotoxic and genotoxic in SH-SY5Y cells in vitro.
In a separate study, He et al. [39] reported on the findings of a bridging the gap between genetic and functional changes following exposures to PBDEs. The authors evaluated gene expression and enzymatic and hormone levels in a human adrenocortical carcinoma cell line (H295R) following exposure to 1 of 20 PBDE metabolites (hydroxylated, methoxylated, and/or chlorinated derivatives). Most compounds tested altered the expression of CYP11B2, which is involved in the synthesis of aldosterone. Expression of CYP19 (aromatase) was also altered, though it was much less sensitive to exposure to the PBDE metabolites. Treatment-related effects on aromatase activity and 17β-estradiol activity were observed, though a consistent or dose-dependent relationship was unclear. The authors concluded that several metabolites adversely impacted steroidogenesis in vitro in this cell line.
Another group of researchers had previously reported on aromatase activity (and other endpoints) following exposures to PBDEs and other BFRs in vitro [40] using the same human adrenocortical carcinoma cells (H295R cell line). Micromolar concentrations of 19 PBDE congeners, 5 hydroxylated PBDEs, 1 methoxylated PBDE, TBBPA, TBBPA-DBPE, 2,4,6-tribromophenol (TBP), 4-bromophenol (4BP), and 2,4,6-tribromoanisole (TBA) were evaluated for inhibitory effects on aromatase activity. 6-OH-BDE47 and 6-OH-BDE99 demonstrated concentration-dependent inhibition of activity (though the authors note that some of this inhibition may have been due to cytotoxicity). TBP and the methoxy-PBDE also caused treatment-related inhibition of aromatase activity. The authors noted that chemical structure influenced toxicity, demonstrating the importance of structure–activity relationships for these compounds. This study provides useful information concerning the synthesis of estrogens resulting from exposure to BFRs.
This same group of researchers [41] published additional findings on a potential mechanism of action associated with CYP17 enzymatic activities following exposures to various PBDE congeners and their hydroxylated derivatives in the same cell line (H295R cells). CYP17 is involved in sex hormone steroidogenesis and is required for the biosynthesis of DHEA and androstenedione. Using an in vitro system designed by the authors, various endpoints were evaluated, each aimed at understanding key events in CYP17 activity following exposures. Results indicated that some hydroxylated PBDEs had the potential to disrupt CYP17 activity in the in vitro system. Effects were clearly congener specific and did not demonstrate a clear structure–activity relationship. The authors further noted that the relevance of these events in vivo has not been adequately determined, and thus additional research is required to further understand the impact of this propose mechanism of action in humans.
A fourth study reported on changes to aromatase activity, though the findings reported by these authors [42] were not as consistent as those reported by Hu and colleagues [43]. In this study, 15 PBDE metabolites, 2 commercial PBDE mixtures (DE-71 and DE-79), and TBBPA were evaluated for the potential to induce changes in gene expression, aromatase activity, and levels of testosterone and 17β-estradiol in the H295R human adrenocortical carcinoma cell line. Of all the compounds evaluated, only selected hydroxylated PBDE metabolites induced changes in expression of steroidogenic genes. Similarly, only selected PBDE metabolites induced changes in aromatase activity. None of the compounds impacted sex hormone production at the concentrations tested. Thus, the important finding of this study demonstrated that the observed changes in gene expression did not result in functional changes in enzyme activity.
In an effort to more fully understand toxicity during fetal development, Shao et al. [44] evaluated the mechanisms associated with BDE-47-mediated injury in primary human fetal liver hematopoeitic stem cells. Exposure to BDE 47 at concentrations in the low micromolar range led to a loss of mitochondrial membrane potential and apoptosis. At a high concentration (50 μM), a loss of viability and generation of ROS were observed. While the authors noted that the findings supported the role for oxidative stress in the cytotoxicity of BDE 47, they also noted that the findings should be interpreted with caution, given the in vitro model and relevance of high concentrations.
2.3.2 Metabolism
Two important studies have been published characterizing the metabolism of selected PBDE congeners. One of the most important scientific data gaps in the health assessment of these compounds revolves around understanding the kinetics of the various BDE congeners in humans, given the widespread, ongoing use of commercial Deca relative to the discontinued production of the lower brominated commercial mixtures, Penta and Octa. BDE 47 remains the most commonly measured congener in human biomonitoring exercises, followed by other lower brominated congeners. Thus, characterizing the scientific rationale for its dominance (despite the low international usage) is very important, particularly considering that the lower brominated congeners may have greater toxicity.
A key study characterized the capacity of human liver cells to metabolize BDE congeners 99 and 209 [45], the primary congeners found in the PentaBDE and DecaBDE commercial mixtures. Specifically, the objective was to determine whether reductively debrominated and/or hydroxylated metabolites occurred. The study authors also reported changes in gene expression in an effort to identify and/or examine genes coding for enzymes involved in PBDE metabolism via oxidative and reductive pathways. Hepatocytes from three human donors (two cryopreserved and one fresh) were exposed to BDE 99 or 209 for up to 72 h at a concentration of ~10 μM. The majority of BDE 209 was recovered, suggesting little metabolism or perhaps little uptake into the cell, whereas much less BDE 99 was recovered, suggesting metabolism of the parent compound. No reductively debrominated metabolites were identified with exposures to either BDE compound. The authors noted that these findings were in contrast to in vitro studies in fish. Several oxidative metabolites were identified following exposures to BDE 99, but not 209.
Results of the gene expression component of this study demonstrated upregulation of mRNA expression of CYP1A2, CYP3A4, deiodinase type 1 (DI1), and glutathione S-transferase M1 (GSTM1) by both BDE congeners. The authors suggested that the measurement of oxidative metabolites of BDE 99 and upregulation of CYP enzymes support a role for CYP-mediated metabolism. The upregulation of deiodinase enzymes is also of interest, given their role in thyroid homeostasis. These data also further demonstrate the need for congener-specific assessment in humans, given that the metabolism of BDE 99 and 209 is clearly different.
Lupton et al. [46] reported similar findings: the more fully brominated congener BDE 153 was not metabolized by human liver microsomes, yet BDE 47 and 99 were. In this study, exposures were limited to 120 min. Multiple metabolites were identified for both BDEs 47 and 99. Importantly, the authors also reported large interindividual differences.
2.3.3 Interpretation of Mechanistic Studies in Human Cells
With respect to neurotoxicity, the studies generally demonstrate treatment-related effects on toxicity, including apoptosis, decreased cell viability, and altered differentiation in human neuroblastoma and primary fetal hNPCs following exposures to the lower brominated congeners typically found in the environment (i.e., BDEs 47 and 99). Several other congeners, including hydroxylated congeners, were investigated in studies assessing cell viability, proliferation, DNA damage (often assessed by measuring ROS), cell signaling, and gene expression. Similar to the neurotoxicity studies, BDE 47 and the commercial mixture DE-71 appeared to be the most potent in these assays, though one study found that BDE 209 inhibited cell viability and generated ROS. Because of the inconsistencies among the studies, it is difficult to determine with confidence whether PBDEs are directly genotoxic, though generally data lean toward non-genotoxic mechanisms. Several BDE congeners were also associated with alterations in steroidogenic genes.
One of the primary uncertainties associated with interpreting data derived from in vitro systems involves extrapolation of the doses used in the studies to environmental exposures. This is of particular importance when the findings of Mundy et al. [47] are considered. This group of authors evaluated the concentration and time-dependent accumulation of BDE 47 in primary cultures of rat cortical neurons in an effort to more fully understand the findings from studies published using in vitro cell culture models. The authors reported that approximately 15% of the BDE 47 was associated with the cells, 55% was in the medium, and 30% was in the culture dish. Addition of serum proteins decreased accumulation, and the total volume of exposure also influenced accumulation. Thus, these factors can greatly influence the accumulation of BDE 47 in cells. The authors estimated that the use of the concentration in the medium underestimates tissue concentrations in the cells by up to two orders of magnitude.
Despite the shortcomings associated with the in vitro data, the mechanistic information provided is very useful, particularly considering that the studies were conducted in human-based cell lines or in primary cells. The data generally indicate that some PBDE congeners have the potential to cause toxic effects in vitro. These may translate into downstream effects associated with endocrine disruption, neurotoxicity, and developmental toxicity – findings that are consistent with the data in human studies. And, importantly, these mechanistic studies indicate that BDE congeners induce differential effects, may act through different mechanisms, and clearly have different relative potencies.
3 Tetrabromobisphenol A
In this section, an overview of the data published in animal studies is provided, followed by a detailed discussion of the health effects observed in humans, primarily in human cell lines. Despite the widespread, high volume use of this compound, there are relatively few studies available examining toxicity.
3.1 Studies in Laboratory Animals
Data are available to characterize a number of endpoints following exposures to TBBPA in laboratory animals, including acute toxicity, skin sensitization, neurotoxicity, reproductive toxicity, genotoxicity, and endocrine disruption. This research has been conducted in a number of species, including rats, mice, and rabbits, and ranges from very short exposures to chronic 90-day exposures. Many of the studies have used rather high doses, and toxicity has been seen mainly following oral exposures. TBBPA is generally considered to act via different mechanisms/elicit differential toxicity as compared to other commonly studied BFRs, given its structure and kinetic properties.
TBBPA demonstrates low acute toxicity by all routes of exposure in all species evaluated. Studies in rats provide LC50 and oral LD50 values of >1.3 mg/l (1 h) and >50 g/kg, respectively, and studies on mice resulted in a similarly high LD50 of >10 g/kg [48–52]. LD50 values from dermal exposure to rabbits were >10 g/kg [49, 53]. No significant toxic effects were noted after administration of TBBPA via any route of exposure in these studies. Furthermore, TBBPA is not considered to be irritating to the eye, skin, or respiratory tract, and is not a corrosive agent [48].
Dietary levels of 0.05–100 mg TBBPA/kg body weight/day in 30- and 90-day rodent studies did not produce any effects on behavior, appearance, food consumption, body weight gain, or mortality [54], and more recent 90-day repeated-dose studies showed that oral exposures did not cause adverse effects at doses up to 1,000 mg/kg [55–57]. No adverse effect on fertility, reproductive performance, development, or neurobehavioral effects were noted in rats in a two-generational study [48, 58, 59]. However, more recent studies have also shown that prenatal and postnatal exposure can result in lipid metabolic disorders and hepatic or kidney lesions [60, 61], as well as changes in behavior, locomotion, and hearing [62, 63]. However, Williams and DeSesso [64] found no adverse developmental neurotoxic effects associated with exposure to TBBPA. Further research is clearly warranted in this area.
TBBPA has produced negative results in several in vitro mutagenicity assays [65, 66], a chromosomal aberration study [67], and an intragenic recombination assay [68] using bacterial strains, yeast, and mammalian cells, and is therefore not considered genotoxic. No studies have yet addressed the carcinogenic potential of TBBPA.
In vitro, TBBPA is toxic to cerebellar granule cells, induces calcium influx, inhibits dopamine, generates free radicals, and induces cell death (LC50 = 7 μM) [69–71]. In isolated liver cells, exposure also results in membrane dysfunction and inhibits the activity of a key mixed-function oxidase, cytochrome P450 2C9 (CYP2C9) [72], although no effects on rat hepatic CYP levels were seen in vivo [73]. TBBPA is also highly immunotoxic in culture, which is demonstrated by its ability to specifically inhibit the expression of CD25 at concentrations as low as 3 μM [129].
Some concerns regarding the potential for adverse effects from TBBPA focus on the possibility that TBBPA may act as an endocrine disruptor by two mechanisms: competitively binding to estrogen receptors, which was postulated due to the structural similarities of TBBPA to a known weak estrogen, bisphenol A; and disruption of thyroid homeostasis. Some in vitro estrogen assays showed that TBBPA does not display estrogenic activity [74, 75]; however, TBBPA exhibited estrogenic effects in a mouse uterotropic assay [76]. TBBPA was a potent inhibitor of E2 sulfation in an E2SULT in vitro assay with an IC50 of 0.016 μM, making it almost 13 times more potent than PCP [77]. Very recently, Li et al. [78] showed that TBBPA is an estrogen receptor (ERα) agonist and progesterone receptor (PR) antagonist in yeast.
The central mechanism of TBBPA toxicity is thought to be through disruption of thyroid homeostasis [3]. This is of primary importance during development when small thyroidal changes in the mother can result in cognitive defects in the children [79]. TBBPA inhibited T3 and thyroid hormone receptor binding, enhanced proliferation of rat pituitary GH3 cells stimulating their production of growth hormone, and enhanced the proliferation of MtT/E-2 cells, whose growth is estrogen dependent [80]. A recent in vitro assay suggested that TBBPA can evoke a receptor-mediated thyroidal response based on evidence that TBBPA acts as a weak agonist up to 1 μM, but exhibits an antagonistic effect on the thyroid hormone receptor above 5 μM [81]. TBBPA shows considerable binding ability to TTR, a key T4 transport protein in the blood, with an affinity up to ten times greater than that of T4 [74, 77]. An in vivo study showed no effect of TBBPA on maternal or fetal T3, T4, or TTR levels; however, TSH levels in fetal plasma were increased, indicating a distinct mechanism of thyroid homeostasis disruption in vivo [82]. In addition, a 14-week reproduction study in mice showed an increase in T3 and decrease in circulating T4 [83]. This study also observed brainstem auditory evoked potentials (BAEP) and saw responses indicative of changes in hearing latency and hearing threshold [62].
3.2 Studies in Humans
Human studies of TBBPA are generally limited to in vitro assays evaluating mechanisms associated with toxicities observed in laboratory species. However, TBBPA was evaluated in a multiple insult sensitization test conducted on 54 human subjects and was not found to be a skin sensitizer [48]. In vitro studies have demonstrated that TBBPA induces a dose-dependent formation of ROS and calcium levels in human neutrophils [84] and anti-estrogenic activity against 17β-estradiol in a human breast cancer cell line [85]. TBBPA was also shown to compete for binding to the estrogen receptor and to induce proliferation in human breast cell lines [86]. Other data based on assessments in human cell lines, discussed below, demonstrate important kinetic parameters and immunotoxicity associated with exposures to TBBPA.
Schauer et al. [87] characterized metabolic capacities across species. Both humans and rats were exposed to TBBPA via oral administration, and similar metabolite profiles were reported in both species. However, the presence of TBBPA-sulfate was not measured, whereas TBBPA-glucuronide was detected in the blood of all human subjects. Additional metabolites were measured in rats, but this may have been associated with the differential dose levels (0.1 mg/kg in humans and 300 mg/kg in rats). Based on time course analysis, TBBPA was absorbed and rapidly conjugated, suggesting that TBBPA has low systemic bioavailability in both humans and rats. Zalko et al. [88] also reported important toxicokinetic findings related to TBBPA metabolism in both rats and humans using an in vitro approach. No major qualitative differences in in vitro metabolism using human and rat subcellular fractions (microsomes and S9) were observed following exposure to 20–200 μM TBBPA. Two primary metabolites were noted in both species: a hepta-brominated dimer-like compound and a hexa-brominated compound with three aromatic rings. These data are useful in evaluating human health risk, particularly when the majority of data are in animal models.
Data reported by Kibakaya et al. [89] suggest the potential for TBBPA to induce the immunosuppressive effects in human natural killer cells. Cells were exposed to TBBPA at varying concentrations for up to 6 days and then evaluated for lytic function, tumor-target-binding function, and ATP levels. TBBPA exposures resulted in dose-dependent decreases in all parameters evaluated; however, at concentrations ≤2.5 μM, ATP concentration was not impacted. Additional assays in which cells were only exposed to TBBPA for 1 h and then left in TBBPA-free media for up to 6 days resulted in decreased lytic function, but did not impact binding or ATP levels. These data are important as interference with natural killer cell function could increase the risk of viral infection or other adverse effects (e.g., tumor promotion).
4 Hexabromocyclododecane
In this section, an overview of the data published in animal studies is provided, followed by a discussion of the health effects observed in humans (primarily human cell lines). Despite the widespread, high volume use of this compound, there are relatively few studies available characterizing toxicity. Even fewer studies fully characterized the compound with respect to stereoisomer composition, which may be of particular importance with respect to both exposure and toxicity.
4.1 Studies in Laboratory Animals
Data are available to characterize a number of endpoints following exposure to HBCD in laboratory animals, including acute toxicity, skin irritation/sensitization, hepatic and thyroid toxicity, neurotoxicity, reproductive toxicity, and genotoxicity. This research has been conducted in a number of species, including rats, mice, and rabbits, and ranges from very short exposures to chronic 90-day exposures. Many of the studies have used rather high oral doses.
HBCD has very low acute toxicity following oral, inhalation, or dermal exposures. Two early studies addressing dermal toxicity of HBCD on white New Zealand rabbits documented no effects after occluded patch exposure at the highest dose of 20 g/kg [90, 91]. When mice and rats were administered doses of 20–40 g/kg of HBCD by gavage, no deaths were observed though some studies noted animals with slight diarrhea, transitory hypoactivity, trembling, and body weight reduction [91–95]. In acute inhalation studies in rats, no deaths were observed following exposure to 202 mg/l for 4 h, or 200 mg/l for 1 h [90, 91].
Several guideline-based studies have been conducted evaluating the irritation and sensitization potential of HBCD. Results generally indicate that although some mild irritation occurred, effects were not significant enough for HBCDD to be classified as an irritant or corrosive [96]. HBCD is also not considered a skin sensitizer based on output from both the Magnusson–Kligmann test and Local Lymph Node (LLN) assay [97, 98].
Repeated-dose oral toxicity studies collectively point to the liver and thyroid as target organs for HBCD toxicity; these data are generally supported by in vitro assays. Early 28- and 90-day feeding studies in rats showed significant, dose-related, increased relative liver weights [99, 100]. In the 28-day study only, both sexes exhibited thyroid hyperplasia at the lowest administered dose (940 mg/kg-day). Increased liver weight was also observed by Chengelis [101] following a 28-day exposure in rats. Additionally, thyroid weight was increased in females (300 mg/kg-day), and changes in serum T4 and TSH were apparent in all rats administered 100 mg/kg-day or higher. A similar 28-day study found that female rats exhibited significant increased absolute liver and thyroid weight and decreased serum T4 levels, with effect-specific NOAELs of 23, 2, and 55 mg/kg-day, respectively [102]. The most recent 28-day study focused on changes in hepatic gene expression, identifying lipid metabolism, cholesterol biosynthesis, and phase I and II metabolism as affected pathways [103].
Several studies have shown that HBCD does not have substantial mutagenic or cytotoxic potential [104–109]. Additionally, an in vivo micronucleus test in mice showed no clastogenic activity [110]. Additionally, a chronic feeding study on mice evaluated the effects of up to 1,300 mg/kg-day HBCD after 18 months [96]. While various types of tumors were observed in several organs, incidences were sporadic and the authors determined them not to be substance related. Collectively, these data indicate that HBCD lacks significant genotoxic potential in vitro as well as in vivo.
A two-generation, reproductive toxicity study on rats suggested a NOAEL of 10 mg/kg-day based on decreased fertility index and number of primordial follicles [111]. Although this study demonstrated increased pup mortality during lactation, there was no evidence of fetotoxicity, teratogenicity, or adverse effects on postpartum development; this is confirmed in two other studies [112, 113]. A recent study identified several adverse effects in F1 offspring, including decreased bone density, testis weight, and fraction of nuclear granulocytes [114]. Neonatal HBCD exposure has been shown to have adverse effects on neurodevelopment [69, 111, 115, 116, 130]. HBCD has also been shown to block dopamine uptake in rat brain synaptosomes in vitro [69] and inhibit neurotransmitter release [117].
4.2 Studies in Humans
A handful of in vitro studies in human cell lines have reported on the cytotoxicity, receptor binding, and changes in gene expression associated with HBCD exposures. These studies underscore the importance of evaluating specific stereoisomers as there are clearly differences in toxicokinetic profiles [118] and toxicity. For example, using a cell line derived from human liver tissue, Zhang et al. [119] evaluated the cytotoxicity of the six α-, β-, and γ-HBCD (+/−) enantiomers. Various release assays were used to evaluate cytotoxicity following exposures to HBCD in Hep G2 cells, resulting in a potency of γ > β > α. The authors further noted that Hep G2 cells exposed to (+) enantiomers expressed significantly lower cell viability than those exposed to (−) enantiomers. Additional assays revealed a positive correlation between LDH release and ROS formation, leading the authors to posit that HBCD toxicity may be mediated via oxidative damage.
Changes in gene expression and DNA methylation were also evaluated in HepG2 cells as well as in primary human hepatocytes [120]. At the concentrations tested, HBCD exposures did not impact DNA methylation globally, though it did cause a lack of promoter demethylation in specific regions in primary hepatocytes. Expression of mRNA from specific genes associated with key events in the cell cycle was also evaluated for potential correlations with DNA methylation status. In primary hepatocytes, N-cym was upregulated by HBCD, whereas p16, RB1, ERα, ERβ, and N-cym were downregulated in HepG2 cells. Given these findings, the authors concluded that there was no correlation between proliferation and DNA methylation. The findings of this study also provide important information regarding the differential responses between a human-derived tumor cell line and primary human cells.
Hinkson and Whalen [121] evaluated the immunotoxicity of HBCD in human natural killer cells in vitro; the authors noted that adverse effects in these cells could be associated with an increased risk of tumor development and/or viral infections. Cells were exposed for various lengths of time to concentrations of HBCD, resulting in decreased lytic function and decreases in ATP. The lack of a consistent relationship between the two, or a relationship with time or dose, makes the findings only qualitatively useful with respect to potential impacts on the human immune system. These researchers posited that these findings were due to decreased binding and cell-surface marker expression [122] in human NK cells. Using the same cell line, HBCD exposures caused a significant decrease in NK cell binding and expression of multiple cell-surface proteins; these effects appeared to have a strong relationship with dose and time.
Using an in vitro system based on transfected human liver cells (HeLaTR), Yamada-Okabe et al. [123] assessed activation of the thyroid receptor by HBCD (and other compounds). Results indicated that the receptor was activated in the presence of T3, though at a relatively low level compared to other activators. This study also included an assessment of cytotoxicity; authors reported that HBCD did not cause toxicity or proliferation in this cell line at the doses tested.
The only human study evaluating the toxicity of HBCD was performed in 1972 and evaluated skin sensitization [96, 124]. Patches of fabric soaked in 10% HBCD were worn for 6 days, removed for 2 weeks, and reapplied for 48 h. No skin reactions were reported in any subjects at any evaluation.
5 Assessment of Human Health Risk by Regulatory Agencies
In an effort to put into perspective the health effects observed in laboratory studies and in humans following exposures to PBDEs, HBCD, and TBBPA, we have provided a short discussion on the health assessments conducted by regulatory bodies for these compounds. Information is provided regarding assessments issued in the USA and Europe. Although these regulatory bodies take different approaches when evaluating risk, both consider the weight of the evidence available, focus on a critical effect, and then quantitatively evaluate safe levels of exposure.
5.1 The United States
In the USA, the Environmental Protection Agency (USEPA) developed various toxicological benchmarks for several PBDE congeners, but not HBCD or TBBPA, as part of the Integrated Risk Information System [1, 2, 6, 8]. This human health assessment program evaluated quantitative and qualitative risk information on effects that may result from exposure to a specific chemical in the environment. When supported by available data, information to characterize hazard and dose–response relationships is used to develop cancer and noncancer toxicological benchmarks (e.g., oral reference dose for noncancer and an oral slope factor for cancer). These toxicological benchmarks are then used to quantify health risk. For BDEs 47, 99, 153, and 209, oral reference doses (RfDs) were developed. RfDs are defined as an estimate (with uncertainty spanning perhaps an order of magnitude) of a daily exposure to the human population (including sensitive subgroups) that is likely to be without an appreciable risk of deleterious effects during a lifetime (expressed as milligram of substance/kilogram body weight-day) [125]. For BDE 209, the USEPA also derived an oral cancer slope factor (note: it was the only congener with data for carcinogenic assessment). A slope factor is defined as an upper bound, approximating a 95% confidence limit, on the increased cancer risk from a lifetime exposure to an agent by ingestion (expressed as units of proportion affected per milligram of substance/kilogram body weight-day) [125].
Because no human studies were available when the assessment was conducted, all toxicological benchmarks derived by the USEPA were based on animal studies. For each congener, a critical study was first selected and then a principal effect for the point of departure (e.g., no observed adverse effect level) was identified. Standard mathematical equations were then used to derive the benchmarks; for the noncancer assessment, uncertainty factors (UFs) were included in the calculation. The approach and resulting toxicological benchmark values are described below:
-
BDE 47: RfD = 0.0001 mg/kg-day based on decreased habituation in mice in a neurobehavioral study reported by Eriksson et al. [126]. Benchmark dose modeling was applied to this dataset to develop a POD (0.35 mg/kg). An UF of 3,000 was then applied to develop the RfD [intraspecies variability (10), interhuman variability (10), extrapolation from subchronic to chronic (3), and database deficiencies (10)].
-
BDE 99: RfD = 0.0001 mg/kg-day based on rearing habituation in a neurobehavioral study in mice reported by Viberg et al. [127]. Benchmark dose modeling was applied to this dataset to develop a POD (0.29 mg/kg). An UF of 3000 was then applied (based on the UFs described for BDE 47) to develop the RfD.
-
BDE 153: RfD = 0.0002 mg/kg-day based on spontaneous motor behavior and learning ability in mice as reported by Viberg et al. [7]. USEPA concluded that this was the only available study appropriate for dose–response. As such, the USEPA relied on the NOAEL of 0.45 mg/kg as the POD. As for BDEs 47 and 99, an UF of 3,000 was then applied to develop the RfD.
-
BDE 209: RfD = 0.007 mg/kg-day based neurobehavioral changes in mice as reported by Viberg et al. [7]. USEPA relied on NOAEL of 2.22 mg/kg-day as the POD and applied UFs for interhuman variability (10), interspecies variability (10), and extrapolation from subchronic to chronic exposures (3). The oral CSF of 7 × 10−4/mg/kg-day was based on neoplastic nodules or carcinomas (combined) in the liver of male rats in a 2-year bioassay conducted by the National Toxicology Program [13].
5.2 Europe
The European Union (EU) has issued Risk Assessment Reports (RARs) for the PentaBDE, OctaBDE, and DecaBDE commercial mixtures. Based on an overall evaluation of the data, selection of critical endpoints and studies, and assessment of the margin of safety (MOS) between exposures and effects, conclusions regarding human health effects are assigned. In the final RAR for Deca [32], the EU determined that with respect to human health, there is at present no need for further information and/or testing and no need for risk reduction measures beyond those that were already being applied. For octabromo derivatives, the EU reported that there was a need for further information and/or testing, and that there was a need for limiting the risk in workers and in humans exposed via the environment [128]. This conclusion was based on the data demonstrating potential endocrine disruption (primarily thyroid hormones) with specific considerations regarding exposures during sensitive life stages such as breast feeding.
In the RAR for pentabromodiphenyl ethercongeners, it was determined that there was a need for further information and/or testing for occupationally exposed humans [14]. This was based on hepatic effects observed in laboratory studies with considerations related to the bioaccumulative potential of these compounds in combination with exposure levels. The lack of data characterizing toxicity following dermal exposures was also considered a significant gap when determining risk. Because of these same uncertainties, the EU assigned two conclusions regarding human exposed indirectly via the environment: (a) there is a need for further information and/or testing and (b) there is at present no need for further information and/or testing for risk reduction measures beyond those which are being applied already, as the synthesis and use of this compound were banned in the EU in 2004, and production voluntarily ceased in the USA that same year. The EU suggested the need for data on potential effects associated with lifelong exposures as well as the need to characterize exposure data from local sources. Furthermore, when considering combined exposures, the EU concluded that there was a clear need for further information and/or testing due to the MOS (described as unacceptably low) associated with both liver effects and behavioral effects. When evaluating exposures to infants via breast milk, the EU identified many data gaps that resulted in a need for further information or testing. The data needs included data on pharmacokinetics, more data on developmental effects, and more data on repeated-dose exposures (note: many of these data gaps were related to extrapolating observed effects in laboratory studies to potential effects in humans).
5.3 Stockholm Convention
Over the past several years, many of the PBDEs have been added to the United Nations Stockholm Convention on POPs. Commercial PentaBDE was the first to be added in 2005, followed by HexaBDE and HeptaBDE (identified as the main components of the commercial octabromodiphenyl ether mixture). The later compounds are listed under Annex A with a specific exemption for use in articles containing these chemicals for recycling. TetraBDE and PentaBDE (identified as commercial pentabromodiphenyl ether mixture compounds) are also listed under Annex A with an exemption for use as articles containing these chemicals for recycling. More recently, HBCD was nominated for inclusion as a POP under the Stockholm Convention. The review committee determined that because of its persistence, adverse effects, bioaccumulative properties, and long range transport, further evaluations would be conducted with the intention of future inclusion.
6 Conclusions
The widespread production and use of BFRs, and strong evidence of increasing contamination of the environment and people by these chemicals heighten the importance of identifying emerging issues and data gaps, and of generating a future research agenda. Available data clearly indicate that exposures to PBDEs, TBBPA, and HBCD can result in adverse effects. Although the effects are compound- and dose-dependent, the primary endpoint of concern appears to be disruption of the endocrine system. The mechanism(s) are not well delineated but may include estrogenic activity, androgenic activity, variations in receptor binding (CAR and PXR), and, most likely, disruptions to thyroid hormones. Other effects of concern include hepatotoxicity and neurotoxicity, the later particularly during development. However, more studies are needed to elucidate the dose–response relationship for these effects in humans. For example, it has been stated that due to species differences in thyroid metabolism, it is unlikely that effects on the thyroid status via an induction of phase II hepatic enzymes would occur in humans. However, mechanisms other than hepatic metabolism cannot be disregarded, particularly in light of findings reported in several epidemiological studies on PBDEs. Further research is also needed to understand potential health effects associated with PBDE congeners not typically studied, and in particular, higher brominated congeners that may be associated with the breakdown of BDE 209. More toxicity studies are also needed on HBCD and TBBPA – particularly carcinogenicity studies and studies including in utero exposures, as well as a number of alternative BFRs that are replacing these compounds in commerce.
References
USEPA (2008) IRIS Health Assessment of 2,2',4,4'-Tetrabromodiphenyl Ether (BDE-47) CASRN 5436-43-12. U.S. Environmental Protection Agency, Washington, DC, 2008. EPA/635/R-07/005F
USEPA (2008) IRIS Health Assessment of 2',4,4',5-Pentabromodiphenyl Ether (BDE-99) CASRN 60348-60-92. U.S. Environmental Protection Agency, Washington, DC, 2008. EPA/635/R-07/006F
Birnbaum LS, Staskal DF (2004) Brominated flame retardants: cause for concern? Environ Health Perspect 112:9–17
Birnbaum LS, Hubal EAC (2006) Polybrominated diphenyl ethers: a case study for using biomonitoring data to address risk assessment questions. Environ Health Perspect 114:1770–1775
Dunnick JK, Nyska A (2009) Characterization of liver toxicity in F344/N rats and B6C3F1 mice after exposure to a flame retardant containing lower molecular weight polybrominated diphenyl ethers. Exp Toxicol Pathol 61(1):1–12
USEPA (2008) IRIS Health Assessment of 2',4,4',5,5'-Hexabromodiphenyl Ether (BDE-153) CASRN 68631-49-22. U.S. Environmental Protection Agency, Washington, DC, 2008. EPA/635/R-07/007F
Viberg H, Fredriksson A, Jakobsson E, Orn U, Eriksson P (2003) Neurobehavioral derangements in adult mice receiving decabrominated diphenyl ether (PBDE 209) during a defined period of neonatal brain development. Toxicol Sci 76:112–120
USEPA (2008) IRIS Health Assessment of 2',3,3',4,4',5,5',6,6'-Decabromodiphenyl Ether (BDE-209) CASRN 1163-19-5. U.S. Environmental Protection Agency, Washington, DC, 2008. EPA/635/R-07/008F
Rice DC, Reeve EA, Herlihy A, Zoeller RT, Thompson WD, Markovich VP (2007) Developmental delays and locomotor activity in the C57BL6/J mouse following neonatal exposure to the fully-brominated PBDE, decabromodiphenyl ether. Neurotoxicol Teratol 29(4):511–520
Rice DC, Thompson WD, Reeve EA, Onos KD, Assadollahzadeh M, Markovich VP (2009) Behavioral changes in aging but not young mice after neonatal exposure to the polybrominated flame retardant decaBDE. Eviron Health Perspect 117(12):1903–1911
Viberg H, Fredriksson A, Eriksson P (2007) Changes in spontaneous behaviour and altered response to nicotine in the adult rat, after neonatal exposure to the brominated flame retardant, decabrominated diphenyl ether (PBDE 209). Neurotoxicology 28(1):136–142
Xing T, Chen L, Tao Y, Wang M, Chen J, Ruan DY (2010) Effects of decabrominated diphenyl ether (PBDE 209) exposure at different developmental periods on synaptic plasticity in the dentate gyrus of adult rats In vivo. Toxicol Sci 110(2):401–410
NTP (National Toxicology Program) (1986) Toxicology and carcinogenesis studies of decabromodiphenyl oxide (CAS No 1163-19-5) in F344/N rats and B6C3F mice (feed studies). NTP TR 309
EU (2001) European Union Risk Assessment Report (RAR): Diphenyl ether, pentabromo derivative (pentabromodiphenyl ether). EUR 19730 EN
Hagmar L, Bjork J, Sjodin A, Bergman A, Erfurth EM (2001) Plasma levels of persistent organohalogens and hormone levels in adult male humans. Arch Environ Health 56(2):138–143
Mazdai A, Dodder NG, Abernathy MP, Hites RA, Bigsby RM (2003) Polybrominated diphenyl ethers in maternal and fetal blood samples. Environ Health Perspect 111(9):1249–1252
Julander A, Karlsson M, Hagstrom K, Ohlson CG, Engwall M, Bryngelsson IL, Westberg H, van Bavel B (2005) Polybrominated diphenyl ethers-plasma levels and thyroid status of workers at an electronic recycling facility. Int Arch Occup Environ Health 78:584–592
Yuan J, Chen L, Chen D, Guo H, Bi X, Ju Y, Jiang P, Shi J, Li L, Jiang Q, Sheng G, Fu J, Wu T, Chen X (2008) Elevated serum polybrominated diphenyl ethers and thyroid-stimulating hormone associated with lymphocytic micronuclei in Chinese workers from an E-waste dismantling site. Environ Sci Technol 42:2195–2200
Wang H, Zhang Y, Liu Q, Wang F, Nie J, Qian Y (2010) Examining the relationship between brominated flame retardants (BFR) exposure and changes of thyroid hormone levels around e-waste dismantling sites. Int J Hyg Environ Health 231(5):369–380
Turyk ME, Persky VW, Imm P, Knobeloch L, Chatterton R, Anderson HA (2008) Hormone disruption by PBDEs in adult male sport fish consumers. Environ Health Perspect 116:1635–1641
Herbstman JB, Sjodin A, Apelberg BJ, Witter FR, Halden RU, Patterson DG, Panny SR, Needham LL, Goldman LR (2008) Birth delivery mode modifies the associations between prenatal polychlorinated biphenyl (PCB) and polychlorinated diphenyl ether (PBDE) and neonatal thyroid hormone levels. Environ Health Perspect 116(19):1376–1382
Chevrier J, Harley KG, Bradman A, Gharbi M, Sjodin A, Eskanzi B (2010) Polybrominated diphenylether (PBDE) flame retardants and thyroid hormone during pregnancy. Environ Health Perspect 118:1444–1449
Meeker JD, Johnson PI, Camann D, Hauser R (2009) Polybrominated diphenyl ether (PBDE) concentrations in house dust are related to hormone levels in men. Sci Total Environ 407(10):3425–3429
Lim JS, Lee DK, Jacobs DRJ (2008) Association of brominated flame retardants with diabetes and metabolic syndrome on the U.S. population, 2003–2004. Diabetes Care 31(9):1802–1807
Costa LG, Giordano G (2007) Developmental neurotoxicity of polybrominated diphenyl ether (PBDE) flame retardants. Neurotox 28(6):1047–1067
Roze E, Meijer L, Bakker A, Van Braeckel KN, Sauer PJ, Bos AF (2009) Prenatal exposure to organohalogens, including brominated flame retardants, influences motor, cognitive, and behavioral performance at school age. Environ Health Perspect 117:1953–1958
Herbstman JB, Sjodin A, Kurzon M, Lederman SA, Jones RS, Rauh V, Needham LL, Tang D, Niedzwiecki M, Wang RY, Perera F (2010) Prenatal exposure to PBDEs and neurodevelopment. Environ Health Perspect 118(5):712–719
Messer A (2010) Mini-review: polybrominated diphenyl ether (PBDE) flame retardants as potential autism risk factors. Physiol Behav 100:245–249
Main KM, Kiviranta H, Virtanen HE, Sundqvist E, Tuomisto JT, Tuomisto J, Vartiainen T, Skakkebaek NE, Toppari J (2007) Flame retardants in placenta and breast milk and cryptorchidism in newborn boys. Environ Health Perspect 115:1519–1526
Akutsu K, Takatori S, Noxawa S, Toshiike M, Nakazawa H, Hayakawa K, Makino T, Iwamoto T (2008) Polybrominated diphenyl ethers in human serum and sperm quality. Bull Environ Contam Toxicol 80:345–350
Harley K, Marks AR, Chevrier J, Bradman A, Sjodin A, Eskenazi B (2010) PBDE concentrations in women’s serum and fecundability. Environ Health Perspect 118(5):699–704
EU (2002) European Union Risk Assessment Report (RAR): bis(pentabromophenyl) ether. EUR 20402 EN
Yu K, He Y, Yeung LW, Lam PK, Wu RS, Zhou B (2008) DE-71-induced apoptosis involving intracellular calcium and the Bax-mitochondria-caspase protease pathway in human neuroblastoma cells in vitro. Toxicol Sci 104:341–351
He P, Wang AG, Xia T, Gao P, Niu Q, Guo LJ, Xu BY, Chen XM (2009) Mechanism of the neurotoxic effect of PBDE-47 and interaction of PBDE-47 and PCB153 in enhancing toxicity in SH-SY5Y cells. Neurotoxicology 30:10–15
Tagliaferri S, Caglieri A, Goldoni M, Pinelli S, Alinovi R, Poli D, Pellacani C, Giordano G, Mutti A, Costa LG (2010) Low concentrations of the brominated flame retardants BDE-47 and BDE-99 induce synergistic oxidative stress-mediated neurotoxicity in human neuroblastoma cells. Toxicol In Vitro 24:116–122
Schreiber T, Gassmann K, Gotz C, Hubenthal U, Moors M, Krause G, Merk HF, Nguyen NH, Scanlan TS, Abel J, Rose CR, Fritsche E (2010) Polybrominated diphenyl ethers induce developmental neurotoxicity in a human in vitro model: evidence for endocrine disruption. Environ Health Perspect 118:572–578
Song R, Duarte TL, Almeida GM, Farmer PB, Cooke MS, Zhang W, Sheng G, Fu J, Jones GD (2009) Cytotoxicity and gene expression profiling of two hydroxylated polybrominated diphenyl ethers in human H295R adrenocortical carcinoma cells. Toxicol Lett 185:23–31
Reistad T, Mariussen E (2005) A commercial mixture of the brominated flame retardant pentabrominated diphenyl ether (DE-71) induces respiratory burst in human neutrophil granulocytes in vitro. Toxicol Sci 87:57–65
He W, He P, Wang A, Xia T, Xu B, Chen X (2008) Effects of PBDE-47 on cytotoxicity and genotoxicity in human neuroblastoma cells in vitro. Mutat Res 649:62–70
Canton RF, Sanderson JT, Letcher RJ, Bergman A, van den Berg M (2005) Inhibition and induction of aromatase (CYP19) activity by brominated flame retardants in H295R human adrenocortical carcinoma cells. Toxicol Sci 88:447–455
Canton RF, Sanderson JT, Nijmeijer S, Bergman A, Letcher RJ, van den Berg M (2006) In vitro effects of brominated flame retardants and metabolites on CYP17 catalytic activity: a novel mechanism of action? Toxicol Appl Pharmacol 216:274–281
Song R, He Y, Murphy MB, Yeung LW, Yu RM, Lam MH, Lam PK, Hecker M, Giesy JP, Wu RS, Zhang W, Sheng G, Fu J (2008) Effects of fifteen PBDE metabolites, DE71, DE79 and TBBPA on steroidogenesis in the H295R cell line. Chemosphere 71:1888–1894
Hu XZ, Xu Y, Hu DC, Hui Y, Yang FX (2007) Apoptosis induction on human hepatoma cells Hep G2 of decabrominated diphenyl ether (PBDE-209). Toxicol Lett Jun 15;171(1-2):19–28. Epub 2007 Apr 10
Shao J, White CC, Dabrowski MJ, Kavanagh TJ, Eckert ML, Gallagher EP (2008) The role of mitochondrial and oxidative injury in BDE 47 toxicity to human fetal liver hematopoietic stem cells. Toxicol Sci 101:81–90
Stapleton HM, Kelly SM, Pei R, Letcher RJ, Gunsch C (2009) Metabolism of polybrominated diphenyl ethers (PBDEs) by human hepatocytes in vitro. Environ Health Perspect 117:197–202
Lupton SJ, McGarrigle BP, Olson JR, Wood TD, Aga DS (2009) Human liver microsome-mediated metabolism of brominated diphenyl ethers 47, 99, and 153 and identification of their major metabolites. Chem Res Toxicol 22:1802–1809
Mundy WR, Freudenrich TM, Crofton KM et al (2004) Accumulation of PBDE-47 in primary cultures of rat neocortical cells. Toxicol Sci 82:164–169
EU (2006) European Union Risk Assessment Report (RAR): 2,2’,6,6’-tetrabromo-4.4’isopropylindenediphenol (tetrabromobisphenol-A or TBBP-A) Part II – Health Assessment. EUR 22161 EN
Hill Top Research, Inc (1966) Acute toxicity and irritation studies in Tetrabromobisphenol A (unpublished)
International Research and Development Corporation (1978) Acute oral toxicity (LD50) study in mice (unpublished)
Leberco Laboratories (1958) Acute oral toxicity test (unpublished)
Pharmakon Laboratories (1981) Acute oral toxicity study in rats (14 day) (unpublished report no. PH 402-ET-001-81)
Pharmakon Laboratories (1981) Acute dermal toxicity study in rabbits (unpublished report no. PH 422-ET-001-81)
WHO (1995) Tetrabromobisphenol A and derivatives. Environmental Health Criteria 172. World Health Organization, Geneva
MPI Research (2002) A 90-day oral toxicity study of tetrabromobisphenol-A in rats with a recovery group (unpublished)
Noda T, Morita S, Ohgaki S, Shimizu M (1985) Safety evaluation of chemicals for use in household products (VII) teratological studies on tetrabromobisphenol-A in rats. Annual report of the Osaka Institute of Public Health and Environmental Sciences 48:106–112
MPI Research (2001) Final report – an oral prenatal developmental toxicity study with tetrabromobisphenol-A in rats (unpublished)
MPI Research (2002) An oral two generation reproductive, fertility and developmental neurobehavioural study of tetrabromobisphenol-A in rats (unpublished)
MPI Research (2003) Amendment to the final report. An oral two generation reproductive, fertility and developmental neurobehavioural study of tetrabromobisphenol-A in rats (Unpublished report)
Fukuda N, Ito Y, Yamaguchi M, Mitumori K, Koizumi M, Hasegawa R, Kamata E, Ema M (2004) Unexpected nephotoxicity induced by tetrabromobisphenol A in newborn rats. Toxicol Lett 150:145–155
Tada Y, Fujitani T, Yano N, Takahashi H, Yuzawa K, Ando H, Kubo Y, Nagasawa A, Ogata A, Kaminmura H (2006) Effects of tetrabromobisphenol A, brominated flame retardant, in ICR mice after prenatal and postnatal exposure. Food Chem Toxicol 44(8):1408–1413
Lilienthal H, Verwer CM, van der Ven LT, Piersma AH, Vos JG (2008) Exposure to tetrabromobisphenol A (TBBPA) in Wistar rats: neurobehavioral effects in offspring from a one-generation reproduction study. Toxicology 246:45–54
Nakajima A, Saigusa D, Tetsu N, Yamakuni T, Tomioka Y, Hishinuma T (2009) Neurobehavioral effects of tetrabromobisphenol A, a brominated flame retardant, in mice. Toxicol Lett 189(1):78–83
Williams AL, DeSesso JM (2010) The potential of selected brominated flame retardants to affect neurological development. J Toxicol Environ Health B Crit Rev 13(5):441–448
Ethyl Corporation (1981) Salmonella/microsomal assay-tetrabromobisphenol A EPA/OTS Doc Number 878216192
Mortelmans K, Haworth S, Lawlor T, Speck W, Tainer B, Zeigler E (1986) Salmonella mutagenicity test: II. Results from the testing of 270 Chemicals. Environ Mutagen 8(7):1–119
BioReliance (2001) An in vitro mammalian chromosome aberration test with tetrabromobisphenol-A (unpublished)
Helleday T, Tuominen K, Bergman A, Jenseen D (1999) Brominated flame retardants induce intragenic recombination in mammalian cells. Mutat Res 439:137–147
Mariussen E, Fonnum F (2002) The effect of pentabromodiphenyl ether, hexabromocyclododecane and tetrabromobisphenol- A on dopamine uptake into rat brain synaptosomes. Organohalogen Compounds 57:395–399
Reistad T, Mariussen E, Fonnum F (2002) The effect of brominated flame retardants on cell death and free radical formation in cerebellar granule cells. Organohalogen Compounds 57:391–394
Reistad T, Mariussen E, Ring A, Fonnum F (2007) In vitro toxicity of tetrabromobisphenol-A on cerebellar granule cells: cell death, free radical formation, calcium influx and extracellular glutamate. Toxicol Sci 96:268–278
Boecker RH, Schwind B, Kraus V, Pullen S, Tiegs G (2001). Cellular disturbances by various brominated flame retardants [Abstract]. Presented at the Second International Workshop on Brominated Flame Retardants, 14–16 May 2001, Stockholm, Sweden
Germer S, Piersma AH, van der Ven L, Kamyschnikov A, Fery Y, Schmitz H-J, Schrenk D (2006) Subacute effects of the brominated flame retardants hexabromocyclododecane and tetrabisphenol A on hepatic cytochrome P450 levels in rats. Toxicology 218:229–236
Meerts IATM, Letcher RL, Hoving S, Bergman A, Lemmen JG, van der Burg B, Brouwer A (2001) In vitro estrogenicity of polybrominated diphenyl ethers, hydroxylated PBDEs and polybrominated bisphenol A compounds. Environ Health Perspect 109(4):399–407
Miller D, Wheals BB, Beresford N, Sumpter JP (2001) Estrogenic activity of phenolic additives determined by an in vitro yeast bioassay. Environ Health Perspect 109(2):133–138
Kitamura S, Kato T, Iida M, Jinno N, Suzuki T, Ohta S, Fujimoto N, Hanada H, Kashiwaga K, Kashiwaga A (2005) Anti-thyroid hormonal activity of tetrabromobisphenol A, a flame retardant, and related compounds: affinity to the mammalian thyroid hormone receptor, and effect on tadpole metamorphosis. Life Sci 76:1589–1601
Hamers T, Kamstra JH, Sonneveld E, Murk AJ, Kester MHA, Andersson P, Legler J, Brouwer A (2006) In vitro profiling of the endocrine disrupting potency of brominated flame retardants. Toxicol Sci 92(1):157–173
Li J, Ma M, Wang Z (2010) In vitro profiling of endocrine disrupting effects of phenols. Toxicol In Vitro 24(1):201–207
Haddow JE, Palomaki GE, Allan WC, Williams JR, Knight GJ, Gagnon J et al (1999) Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child. N Engl J Med 341:549–555
Kitamura S, Jinno N, Ohta S, Kuroki H, Fujimoto N (2002) Thyroid hormonal activity of the flame retardants tetrabromobisphenol A and tetrachlorobisphenol A. Biochem Biophys Res Commun 293:554–559
Freitas J, Cano P, Craig-Veit C, Goodson ML, Furlow JD, Murk AJ (2011) Detection of thyroid hormone receptor disruptors by a novel stable in vitro reporter gene assay. Toxicol In Vitro 25:257–266
Meerts IATM, Assink Y, Cenijin PH, Weijers BM, van den Berg HHJ (1999) Distribution of the flame retardant tetrabromobisphenol A in pregnant and fetal rats and effect on thyroid hormone homeostasis. Brominated Flame Retardants P068/. Organohalogen Compounds 40:375–378
Van der Ven LT, Ven de Kuil T, Verhoef A, Verwer CM, Lilienthal H, Leonards PE et al (2008) Endocrine effects of tetrabromobisphenol- A (TBBPA) in Wistar rats as tested in a one-generation reproduction study and a subacute toxicity study. Toxicology 260(1–3):150–152
Reistad T, Mariussen E, Fonnum F (2005) The effect of a brominated flame retardant, tetrabromobisphenol-A, on free radical formation in human neutrophil granulocytes: the involvement of the MAP kinase pathway and protein kinase C. Toxicol Sci 83:89–100
Kitamura S, Suzuki T, Sanoh S, Kohta R, Jinno N, Sugihara K, Yoshihara S, Fujimoto N, Watanabe H, Ohta S (2005) Comparative study of the endocrine-disrupting activity of bisphenol A and 19 related compounds. Toxicol Sci 84:249–259
Samuelsen M, Olsen C, Holme JA, Meussen-Elhoom E, Bergmann A, Hongslo JK (2001) Estrogen-like properties of brominated analogs of bisphenol A in the MCF-7 human breast cancer cell line. Cell Biol Toxicol 14:139–151
Schauer UM, Volkel W, Dekant W (2006) Toxicokinetics of tetrabromobisphenol a in humans and rats after oral administration. Toxicol Sci 91:49–58
Zalko D, Prouillac C, Riu A, Perdu E, Dolo L, Jouanin I, Canlet C, Debrauwer L, Cravedi JP (2006) Biotransformation of the flame retardant tetrabromo-bisphenol A by human and rat sub-cellular liver fractions. Chemosphere 64:318–327
Kibakaya EC, Stephen K, Whalen MM (2009) Tetrabromobisphenol A has immunosuppressive effects on human natural killer cells. J Immunotoxicol 6:285–292
Lewis AC, Palanker AL (1978) A dermal LD50 study in albino rabbits and an inhalation LC50 study in albino rats. Test material GLS-S6-41A. Client: Saytech Inc. (not published). 78385-2, Consumer product testing
Wilson PD, Leong BKJ (1977) Acute toxicity studies in rabbits and rats. Test material Firemaster 100 Lot 53 77.902. Sponsored by: Velsicol Chemical Corporation (not published). pp 163–499, International Research and Development Corporation
Lewis AC and Palanker AL (1978) A primary dermal irritation study, a dermal corrosion study, and an ocular irritation study in albino rabbits and an oral LD50 study in albino rats. Test material GLS-S6-41A. Client: Saytech Inc. (not published). 78385-1, Concumer Product Testing
Ogaswara S, Fukushi A, Midorikawa Y (1983) Report on acute toxicity test of pyroguard SR-103 in rats (not published)
Tobe et al (1984) Acute toxicity test of hexabromocyclododecane (not published). Research Center for Biological Safety National Public Health Research Institute
USEPA (1990) Report on the study of the acute oral toxicity of hexabromocyclododecane in the mouse. Letter from BASF. 86-900000383, EPT/OTS Doc
EU (2008) European Union Risk Assessment Report (RAR): Hexabromocyclododecane
Wenk ML (1996) Maximization test in guinea pigs. Test article: Hexabromocyclododecane; p 43. Microbiologial Associates, Inc., Rockvill, MD, USA
Wolhiser MR, Anderson PK (2003) Hexabromocyclododecane: contact sensitization potential via the local lymph node assay (including a primary irritancy screen) using CBA/J mice. Study ID 031013, p 24. Toxicology & Environmental Research and Consulting, The Dow Chemical Company, Midland, Michigan, USA
Zeller H, Kirsch P (1969) Hexabromocyclododecane: 28-day feeding trials with rats. BASF (not published)
Zeller H, Kirsch P (1970) Hexabromocyclododecane: 90-day feeding trials with rats. BASF (not published)
Chengelis CP (2001). A 90-day oral (gavage) toxicity study of HBCD in rats. WIL-186012, p 1527. Wil Research Laboratories, Inc., Ashland, Ohio, USA
Van der Ven LTM, Verhoef A, van de Kuil T, Slob W, Leonards PEG, Visser TJ, Hamers T, Håkansson H, Olausson H, Piersma AH, Vos JG (2006) A 28-day oral dose toxicity study of hexabromocyclododecane (HBCD) in Wistar rats. Toxicol Sci 94:281–292
Canton RF, Peijnenburg AA, Hoogenboom RL, Piersma AH, van der Ven LT, van den Berg M, Heneweer M (2008) Subacute effects of hexabromocyclododecane (HBCD) on hepatic gene expression profiles in rats. Toxicol Appl Pharmacol 231(2):267–272
Baskin AD, Phillips BM (1977) Mutagenicity of two lots of FM-100, Lot 53 and residue of lot 3322 in the absence and presence of metabolic activation. Sponsored by: Velsicol Chemical Corporation (not published). Industrial BIO TEST Laboratories, Inc
GSRI (1979) Mutagenicity test of GLS-S6-41A (not published). Gulf South Research Institute
Hossack DJN, Richold M, Jones E, Bellamy RP (1978) Ames metabolic activation test to assess the potential mutagenic effect of compound no. 49. pp 1–2. Huntingdon Research Centre
Simmon VF, Poole DC, Newell GW, Skinner WA (1976) In vitro microbiological mutagenicity studies of four CIBA-GEIGY corporation compounds. Prepared for CIBAGeigy Corporation (not published). 5702, SRI Project LSC
USEPA (1990) Ames test with hexabromides. Letter from BASF. 86-900000379, EPA/OTS Doc
Zeiger E, Anderson B, Haworth S, Lawlor T, Mortelmans K, Speck W (1987) Salmonella mutagenicity tests: III. Results from the testing of 255 chemicals. Environ Mutagen 9(Suppl 9):1–110
Engelhardt and Hoffman (2000) Cytogenetic study in vivo with of hexabromocyclododecane in the mouse micronucleus test after two intraperitoneal administrations. BASF, Ludwigshafen, Germany
Ema M, Fujii S, Hirata-Koizumi M, Matsumoto M (2008) Two-generation reproductive toxicity study of the flame retardant hexabromocyclododecane in rats. Reprod Toxicol 25(3):335–351
Murai T, Kawasaki H, Kanoh S (1985) Studies on the toxicity of insecticides and food additives in pregnant rats (7). Fetal toxicity of hexabromocyclododekane. Oyo Yakuri 29:981–986
Stump DG (1999) Prenatal developmental toxicity study of hexabromocyclododecane (HBCD) in rats. WIL Research Laboratories, Inc, Ashland, Ohio, USA, p 410
Van der Ven LT, van de Kuil T, Leonards PEG, Slob W, Lilienthal H, Litens S, Herlin M, Hakansson H et al (2009) Endocrine effects of hexabromocyclododecane (HBCD) in a one-generation reporoduction study in Wistar rats. Toxicol Lett 185:51–62
Lilienthal H, van der Ven L, Roth-Haerer A, Hack A, Piersma A, Vos J (2006) Neurobehavioral toxicity of brominated flame retardants: differential effects of PBDE-99, TBBPA and HBCD and endocrine relation. Dioxin Conference 2006 Oslo. Organohalogen Compounds 68: 3 pages
Lilienthal H, van der Ven LT, Piersma AH, Vos JG (2009) Effects of the brominated flame retardant hexabromocylcododecane (HBCD) on dopamine-dependent behavior and brainstem auditory evoked potentials in a one-generation reproduction study in Wistar rats. Toxicol Lett 185(1):63–72
Dingemans MML, Heusinkveld HJ, de Groot A, Bergman A, van de Berg M, Westerink RHS (2009) Hexabromocylcododecane inhibits depolarization-induced increase in intracellular calcium levels and neurotransmitter release in PC12 cells. Toxicol Sci 107(2):490–497
Szabo DT, Diliberto JJ, Hakk H, Huwe JK, Birnbaum LS (2010) Toxicokinetics of the flame retardant hexabromocyclododecane gamma: effect of dose, timing, route, repeated exposure, and metabolism. Toxicol Sci 117(2):282–293
Zhang X, Yang F, Xu C, Liu W, Wen S, Xu Y (2008) Cytotoxicity evaluation of three pairs of hexabromocyclododecane (HBCD) enantiomers on Hep G2 cell. Toxicol In Vitro 22:1520–1527
Aniagu SO, Williams TD, Chipman JK (2009) Changes in gene expression and assessment of DNA methylation in primary human hepatocytes and HepG2 cells exposed to the environmental contaminants-Hexabromocyclododecane and 17-beta oestradiol. Toxicology 256:143–151
Hinkson NC, Whalen MM (2009) Hexabromocyclododecane decreases the lytic function and ATP levels of human natural killer cells. J Appl Toxicol 29:656–661
Hinkson NC, Whalen MM (2010) Hexabromocyclododecane decreases tumor-cell-binding capacity and cell-surface protein expression of human natural killer cells. J Appl Toxicol 30:302–309
Yamada-Okabe T, Sakai H, Kashima Y, Yamada-Okabe H (2005) Modulation at a cellular level of the thyroid hormone receptor-mediated gene expression by 1, 2, 5, 6, 9, 10- hexabromocyclododecane (HBCD), 4, 4´-diiodobiphenyl (DIB), and nitrofen (NIP). Toxicol Lett 155:127–133
McDonnell (1972) Human Patch Test, Haskell Laboratory Report. p. 185-72, Haskell Laboratory for toxicology and Industrial Medicine, E.I. du Pont de Nemours and Company
USEPA (2010) IRIS glossary/Acronyms and Abbreviations. Available: http://www.epa.gov/ncea/iris/help_gloss.htm. Accessed 29 Nov 2010
Eriksson P, Jakobsson E, Fredriksson A (2001) Brominated flame retardants: a novel class of developmental neurotoxicants in our environment? Environ Health Perspect 109:903–908
Viberg H, Fredriksson A, Eriksson P (2004) Investigations of strain and/or gender differences in developmental neurotoxic effects of polybrominated diphenyl ethers in mice. Toxicol Sci 81:344–353
EU (2003) European Union Risk Assessment Report (RAR): Diphenyl ether, octabromo derivative. EUR 20403 EN
Pullen S, Boecker R, Tiegs G (2003) The flame retardants tetrabromobisphenol A and tetrabromobisphenol A-bisallylether suppress the induction of interleukin-2 receptor alpha chain (CD25) in murine splenocytes. Toxicology Feb 14;184(1):11–22
Eriksson P, Fischer C, Fredriksson A (2006) Polybrominated diphenyl ethers, a group of brominated flame retardants, can interact with polychlorinated biphenyls in enhancing developmental neurobehavioral defects. Toxicol Sci Dec;94(2):302–9. Epub 2006 Sep 15
Disclaimer
This chapter does not reflect the opinions or policies of the National Institutes of Health. The use of trade, firm, or corporation names in this publication is for the information and convenience of the reader. Such use does not constitute an official endorsement or approval by the NIH.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Wikoff, D.S., Birnbaum, L. (2011). Human Health Effects of Brominated Flame Retardants. In: Eljarrat, E., Barceló, D. (eds) Brominated Flame Retardants. The Handbook of Environmental Chemistry(), vol 16. Springer, Berlin, Heidelberg. https://doi.org/10.1007/698_2010_97
Download citation
DOI: https://doi.org/10.1007/698_2010_97
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-19268-5
Online ISBN: 978-3-642-19269-2
eBook Packages: Earth and Environmental ScienceEarth and Environmental Science (R0)