Abstract
Biofilm formation in wounds can lead to increased inflammation, infection and delayed wound healing. Additionally, biofilms show increased recalcitrance to antimicrobials compared to their planktonic counterparts making them difficult to manage and treat. Biofilms are frequently polymicrobial, consisting of aerobic and anaerobic bacteria, as well as fungi and yeasts. The aim of this study was to evaluate the effects of a concentrated surfactant gel with antibacterial preservative agents (CSG) against wound relevant opportunistic pathogens, including an aerobic biofilm, anaerobic biofilm and multispecies biofilm. The CSG was added to a 48 h anaerobic biofilm of Bacteroides fragilis, a 24 h multispecies biofilm of Acinetobacter baumannii, Staphylococcus aureus and Staphylococcus epidermidis and a 24 h biofilm of Pseudomonas aeruginosa grown in an in vitro wound relevant environment. Following a contact time of 24 h with the CSG, the bacterial cell density of the biofilms was reduced by 2–4 log in comparison to an untreated control. The results demonstrate the ability of the CSG to disrupt wound relevant biofilms and support the use of the CSG in the clinic to treat wounds caused by biofilm related infections.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Biofilms are formed when microbial cells adhere to a surface and each other and secrete extracellular polymeric substances (EPS), encasing themselves in an extracellular matrix (ECM) (Percival et al. 2014). Biofilms can form on medical devices such as catheters leading to infection (Donelli and Vuotto 2014). There is also increasing evidence showing an association of biofilm formation in chronic wounds, such as diabetic foot ulcers and also acute wounds, such as surgical sites (Banu et al. 2015; Malone et al. 2017; Percival et al. 2017a; Suryaletha et al. 2018). Biofilm formation in wounds leads to increased inflammation, infection and delayed wound healing causing a large burden on healthcare (Attinger and Wolcott 2012; Zhao et al. 2013).
Staphylococcus aureus and Staphylococcus epidermidis are Gram-positive bacteria that often exist as commensal organisms on the skin; however, they are a common cause of skin and soft tissue infections and medical device related infections (Rogers et al. 2009; Mork et al. 2020). Pseudomonas aeruginosa and Acinetobacter baumannii are Gram-negative bacteria that are highly associated with nosocomial infections and are often multi drug resistant (MDR) (Esposito and De Simone 2017). S. aureus and P. aeruginosa are the most common microorganisms isolated from chronic wounds (Serra et al. 2015). Although aerobic bacteria such as S. aureus and P. aeruginosa are frequently isolated from wounds, anaerobic bacteria, such as Bacteroides fragilis are also present. B. fragilis has been found in a number of different wound types including diabetic foot ulcers (DFUs) and surgical site wounds (Percival et al. 2018; Alexiou et al. 2017).
Although biofilms can consist of a single species, often they comprise of multiple species including aerobic bacteria, anaerobic bacteria and fungal/yeast species (Omar et al. 2017). The multispecies nature of biofilms can create a reservoir of resistance genes and an environment for genetic exchange (Savage et al. 2013; Balcazar et al. 2015; Aguila-Arcos et al. 2017). Due to the close proximity of cells and increased cell-to-cell contact, genetic exchange can occur via plasmid conjugation and DNA transformation following secretion during ECM formation (Molin and Tolker-Nielsen 2003; Madsen et al. 2012; Stalder and Top 2016).
Biofilms are also difficult to treat as they have inherent tolerance to antimicrobials at therapeutic levels that their planktonic counterparts are generally susceptible to. This can be attributed to several factors including the ECM, presence of persister cells, changes in gene expression and slow growth rate (Stewart et al. 2015; Hall and Mah 2017; Singh et al. 2017). The ECM consists of proteins, polysaccharides, lipids and extracellular DNA and often constitutes around 80–90% of the biofilm (Flemming 2016). The ECM has been shown to increase the tolerance of biofilms to antimicrobials through several different mechanisms including reducing the diffusion rate of antimicrobials and subsequently reducing the concentration reaching sessile microbial cells, resulting in exposure to sub-therapeutic levels (Van Acker et al. 2014). The heterogeneity of cells in a biofilm, resulting in differences in gene expression and growth rate and also increases the tolerance of biofilms to antimicrobials (Stewart et al. 2015; Pestrak et al. 2018). Persister cells are present in a biofilm and exist in a dormant state; therefore, they show high tolerance to antimicrobials and antibiotics that target replication and metabolic pathways (Lewis 2010; Pang et al. 2018). Persister cells are hypothesised to reside in infected and non-healing chronic wounds, posing a challenge for treatment (Percival et al. 2011).
Previous studies have demonstrated the ability of the concentrated surfactant gel with antibacterial preservative agents (CSG) included in this study to reduce monoculture biofilms of aerobic strains in various biofilm models (Salisbury et al. 2019b; Percival et al. 2017b). The aim of this study was to evaluate the ability of the CSG to reduce the biofilm cell density of relevant wound pathogens including an anaerobic biofilm of B. fragilis, a multispecies biofilm of A. baumannii, S. aureus and S. epidermidis and an aerobic biofilm of P. aeruginosa grown in an in vitro wound dressing model.
2 Materials and Methods
2.1 Test Articles
PluroGel® Burn and Wound Dressing, a concentrated surfactant gel with antibacterial preservative agents (CSG) including phenoxyethanol and potassium sorbate, was provided by Medline Industries Inc. (Chicago, IL).
2.2 Anaerobic Direct Contact Method
The effects of the CSG against a 48 h biofilm of Bacteroides fragilis ATCC 25285 was evaluated by growing the biofilm in 12 well plates and adding the CSG directly to it.
Briefly, a single colony of B. fragilis was inoculated into Tryptone Soya broth (TSB) (Scientific Laboratory Supplies, UK) + 5% laked horse blood (Scientific Laboratory Supplies, UK) and incubated anaerobically at 37 °C and 125 rpm for 24 h. The overnight culture was added to a 12 well plate, which was then incubated anaerobically at 37 °C for 48 h.
After incubation, the liquid was removed and the CSG was added to the biofilm in triplicate by adding 3 g per well to ensure complete coverage of the biofilms. Phosphate buffered saline (PBS) (Scientific Laboratory Supplies, UK) was also added to the biofilm in triplicate by adding 2 mL per well for an untreated control group. The plates were then incubated anaerobically at 37 °C for 24 h.
After the challenge period, the contents of each well were transferred to falcon tubes containing 10 mL Dey-Engley neutralising broth (Scientific Laboratory Supplies, UK) and sonicated on full power for 30 min. Samples were then vortexed briefly, serial diluted 1:10 in PBS and plated onto Tryptone Soya agar (TSA) (Scientific Laboratory Supplies, UK) + 5% sheep defibrinated blood (Scientific Laboratory Supplies, UK) in duplicate. The plates were incubated anaerobically at 37 °C for 48 h. After incubation, colonies were enumerated to calculate average CFU/mL.
2.3 Multispecies Biofilm Direct Contact Method
The effects of the CSG against a 24 h biofilm of Staphylococcus aureus ATCC 29213, Staphylococcus epidermidis ATCC 35984 and Acinetobacter baumannii ATCC 19606 was evaluated by growing the biofilm on membrane filter discs utilising a hydrogel as a nutrient source and adding the CSG directly to it.
The hydrogel was prepared by dissolving 3-sulfopropyl acrylate potassium salt (polymer) in PBS and then adding PEG dissolved in PBS, foetal bovine serum (FBS) and 1% 1-hydroxy cyclohexyl phenol ketone prepared in 70% ethanol (photo-initiator) to it. The mixture was added to a 12 well plate (2 mL/well) and set by exposing the hydrogel to 366 nm UV light.
An overnight inoculum of S. aureus ATCC 29213, S. epidermidis ATCC 35984 and A. baumannii ATCC 19606 was set up by inoculating 10 mL of TSB with a single colony and incubating at 37 °C and 125 rpm. Overnight cultures were adjusted to 1 × 108 CFU/mL before adding all 3 strains together in TSB at a final concentration of 1 × 106 CFU/mL. Durapore 13 mm (1 μM) membrane filter discs (Merck, UK) were incubated with the adjusted culture for 2 h at 37 °C and 125 rpm. Following this, the filters were transferred to a 12 well plate containing the hydrogel (1 filter/well) and incubated at 37 °C for 24 h.
Following 24 h biofilm growth, the filters were transferred to fresh 12 well plates and treated with the CSG by adding 3 g directly to each well to ensure complete coverage of the biofilm (n = 3). PBS was added to the untreated control by adding 2 mL per well. Biofilms were treated for 24 h at 37 °C.
To determine bacterial cell density, the contents of each well were transferred to 10 mL Dey-Engley neutralising broth and sonicated at full power for 30 min. Samples were vortexed briefly, serial diluted 1:10 in PBS and plated out onto TSA. The plates were incubated overnight at 37 °C and the following day counts were enumerated to calculate average CFU/mL.
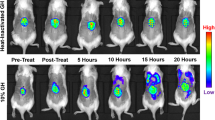
2.4 Drip Flow Bioreactor Wound Dressing Model
The effects of the CSG was evaluated against a 24 h biofilm of Pseudomonas aeruginosa ATCC 700888 by growing the biofilm in the drip flow bioreactor. The biofilm was grown at an air/liquid interface, under low fluid shear conditions to represent an exuding wound environment.
The drip flow bioreactor was prepared by adding a clean borosilicate microscope slide, with a 2.5 cm2 absorbent pad attached, to each channel of the bioreactor. The drip flow bioreactor was then autoclaved at 121 °C.
An overnight inoculum was set up by inoculating 10 mL TSB with a single colony of P. aeruginosa ATCC 700888 and incubating at 37 °C and 125 rpm. The following day the absorbent pads were moistened with TSB and 2 cm2 membrane filter discs were added to each pad. The overnight culture was adjusted to 1 × 108 CFU/mL and used to inoculate the filter membrane discs. The inoculated discs were air dried for 30 min before connecting the drip flow to a nutrient flow of 270 mg/L TSB at 5 mL/h/channel.
After 24 h, sterile gauze was cut into 2 cm2 sections and 4 g of the CSG was added to each gauze to completely coat it. The coated gauze was added to the biofilm in triplicate before reconnecting the drip flow to the nutrient flow. A biofilm growth control group was included and remained untreated (n = 3). Treatment was applied for 24 h.
To determine bacterial cell density, each membrane filter disc was transferred to 10 mL Dey-Engley neutralising broth and sonicated on full power for 30 min. Samples were then vortexed briefly, serial diluted 1:10 in PBS and plated onto TSA. The plates were incubated overnight at 37 °C and the following day bacterial colonies were enumerated.
2.5 Statistical Analysis
Raw data was entered into Microsoft Excel and average CFU/mL was calculated. To determine if there was a statistical difference between the untreated control and the CSG treated biofilms the unpaired t-test was carried out using Prism 7 software.
3 Results
3.1 Effects on Anaerobic Bacteria
Following growth of a 48 h biofilm of B. fragilis ATCC 25285, the untreated control had a bacterial cell density of 1.01 × 109 CFU/mL (Fig. 1). In comparison, biofilms treated with the CSG had a bacterial cell density of 3.47 × 107 CFU/mL, showing nearly a 2 log reduction in cell count. The log reduction in bacterial cell count of B. fragilis following 24 h treatment with the CSG was significant in comparison to the untreated control (p 0.0432).
3.2 Effects on a Multispecies Biofilm
Following growth of a 24 h multispecies biofilm of S. aureus, S. epidermidis and A. baumannii the untreated control had a bacterial cell density of 6.43 × 108 CFU/mL (Fig. 2). Following treatment with the CSG a bacterial cell density of 2.74 × 104 CFU/mL was found, showing a 4 log reduction in cell count. The log reduction in bacterial cell count of the multispecies biofilm following 24 h treatment with the CSG was significant in comparison to the untreated control (p 0.0014).
Log10 cell density of a 24 h multispecies biofilm of Staphylococcus aureus ATCC 29213, Staphylococcus epidermidis ATCC 35984 and Acinetobacter baumannii ATCC 19606 following 24 h treatment with the CSG. Error bars represent the standard error of the mean. * = a significant log reduction in comparison to the untreated control (p 0.0014)
3.3 Effects on a Biofilm Grown in a Wound Dressing Model
Following growth of a 24 h P. aeruginosa biofilm in a wound dressing model, the untreated control had a bacterial cell density of 9.72 × 108 CFU/mL (Fig. 3). Biofilms treated with the CSG showed a bacterial cell density of 1.09 × 107 CFU/mL showing ~2 log reduction in cell count. Although a ~ 2 log reduction in the P. aeruginosa biofilm cell density was found in this model the difference was not deemed as statistically significant (p 0.1762).
Log10 cell density of P. aeruginosa ATCC 700888 24 h biofilm grown in the drip flow bioreactor wound dressing model following 24 h treatment with the CSG. Error bars represent standard error of the mean. No significant difference was found between the CSG treated biofilm and the untreated biofilm (p 0.1762)
4 Discussion
In this study the effects of a CSG on an anaerobic biofilm of B. fragilis, a multispecies biofilm of S. aureus, S. epidermidis and A. baumannii and a P. aeruginosa biofilm grown in an in vitro wound dressing environment was evaluated.
B. fragilis is a common anaerobic strain isolated from wounds, with it being one of the most frequent strains isolated from patients with diabetic foot ulcers (DFUs) in several clinical studies (Ramani et al. 1991; Percival et al. 2018; Al Benwan et al. 2012). B. fragilis is also a common anaerobic strain isolated from surgical site infections (SSIs). In a recent study B. fragilis was the fourth main pathogen isolated from patients with SSIs, with the other strains being aerobic strains (Alexiou et al. 2017). In this study, treatment of a B. fragilis biofilm with the CSG resulted in nearly a 2 log reduction in bacterial cell density (p 0.0432), showing the ability of the CSG to reduce the bacterial cell count of the anaerobic biofilm and potentially disruption of the biofilm.
Clinical studies have demonstrated that biofilms present in wounds, such as surgical site wounds, are often multispecies (Alexiou et al. 2017). The ability of A. baumannii, S. epidermidis and S. aureus to form biofilms is well documented (de Oliveira et al. 2016; Pakharukova et al. 2018; Olwal et al. 2018). Additionally, A. baumannii and S. aureus are both included on the list of ESKAPE pathogens, a list of the most common MDR (multi drug resistant) bacterial species causing nosocomial infections (Esposito and De Simone 2017). The presence of S. aureus, including methicillin resistant S. aureus (MRSA), is frequently reported as a predominant organism colonising wounds, such as surgical sites, diabetic foot ulcers and chronic wounds (Krishna and Gibb 2010; Banu et al. 2015; Serra et al. 2015; Obermeier et al. 2018). Additionally, increasing incidents of A. baumannii infection have been found, particularly in military unit associated wounds has been found (Davis et al. 2005; Schafer and Mangino 2008; Aurora et al. 2018). S. epidermidis is a commensal bacterium that is part of the normal skin flora; however, it has been shown to be a common cause of nosocomial infections in the immunocompromised, being associated with medical device related infections (Ziebuhr et al. 2006). It is estimated that up to 80% of infections of medical implant devices are caused by S. epidermidis biofilms (Rogers et al. 2009). In this study, the CSG reduced a multispecies biofilm by 4 log in comparison to an untreated control (p 0.0014), showing a reduction in the biofilm bacterial cell count and potentially disruption of the biofilm.
The ability of the CSG to disrupt a P. aeruginosa biofilm grown in the drip flow bioreactor was also evaluated. The drip flow bioreactor test method, ASTM E2647–13, is designed to grow a biofilm close to the air/liquid interface in an environment with continuous nutrient flow under low shear conditions (ASTM 2013). In this study, the method was adapted to represent a highly exudative wound environment, as described previously (Bourdillon et al. 2017; Lipp et al. 2010). The constant flow of proteinaceous media allows the formation of a robust biofilm, while potentially washing away antimicrobials, which could occur in an exuding wound environment (Bourdillon 2016). In this model, the CSG reduced the P. aeruginosa biofilm cell density by ~2 log, showing a reduction in bacterial cell count and potentially disruption of a pre-formed biofilm in an in vitro model simulating the exuding wound environment.
The authors have previously shown a 3 log reduction in monoculture A. baumannii 24 h biofilms of clinical isolates grown in the CDC bioreactor model following treatment with the CSG (Salisbury et al. 2019b). Additionally, a reduction in biofilm cell density of P. aeruginosa, S. aureus, Methicillin resistant S. aureus (MRSA), S. epidermidis and Enterococcus faecalis has also been demonstrated in various biofilm models, but no antimicrobial activity was found against the same strains in the zone of inhibition assay, suggesting a potential detachment or dispersion effect in the biofilm models (Percival et al. 2017b). A more recent study demonstrated that treatment of a P. aeruginosa biofilm with the CSG reduced components of the biofilm ECM, particularly the extracellular DNA (eDNA) (Salisbury et al. 2019a).
Several publications have demonstrated the importance of eDNA for bacterial adhesion, structure of the biofilm and maturation of the biofilm (Whitchurch et al. 2002; Yu et al. 2019; Blakeman et al. 2019; Cherny and Sauer 2019). Therefore, the ability of the CSG in this study to disrupt the biofilm may be through its ability to reduce eDNA present in the ECM (Salisbury et al. 2019a). Presence of eDNA in the ECM has also been shown to contribute to biofilm mediated antimicrobial resistance of certain antibiotic classes. One study showed the presence of eDNA increased resistance to cationic antimicrobial peptides and aminoglycosides, but not fluoroquinolones or β-lactams, by upregulating PA3552-PA3559 cationic antimicrobial peptide resistance operon (Mulcahy et al. 2008). Therefore, the CSG in this study could potentially be used in combination to increase the susceptibility of biofilms to certain antimicrobials and improve treatment outcome of chronic wounds.
The data presented in this study highlights the potential ability of a CSG to disrupt wound related biofilms, with it demonstrating a reduction in bacterial cell count of an anaerobic biofilm of B. fragilis by nearly 2 log (p 0.0432) and a multispecies biofilm of S. aureus, S. epidermidis and A. baumannii by 4 log (p 0.0014). The CSG also exhibited a potential ability to disrupt P. aeruginosa reducing a biofilm grown in an in vitro model simulating the exuding wound environment by ~2 log, but this outcome was not deemed significant (p 0.1762). Previous studies support the ability of the CSG to cause biofilm disruption, with treatment of biofilm with the CSG resulting in reduction of biofilm ECM components. However, to further confirm biofilm disruption, it would be useful to carry out additional studies such as fluorescent staining of the ECM and bacterial cells and visualisation using confocal scanning laser microscopy. Additionally, to further investigate the activity of the CSG on biofilms, it would be interesting to compare the CSG to control gels, for example one without the antimicrobial preservatives, to evaluate the components having the largest impact on biofilm disruption. The data helps to support the use of the CSG in the clinic to aid in the management of biofilms in chronic wounds.
References
Aguila-Arcos S, Alvarez-Rodriguez I, Garaiyurrebaso O, Garbisu C, Grohmann E, Alkorta I (2017) Biofilm-forming clinical Staphylococcus Isolates Harbor horizontal transfer and antibiotic resistance genes. Front Microbiol 8:2018
Al Benwan K, Al Mulla A, Rotimi VO (2012) A study of the microbiology of diabetic foot infections in a teaching hospital in Kuwait. J Infect Public Health 5:1–8
Alexiou K, Drikos I, Terzopoulou M, Sikalias N, Ioannidis A, Economou N (2017) A prospective randomised trial of isolated pathogens of surgical site infections (SSI). Ann Med Surg (Lond) 21:25–29
ASTM (2013) E2647–13 standard test method for quantification of Pseudomonas aeruginosa biofilm grown using the drip flow biofilm reactor with low shear and continuous flow. ASTM, West Conshohocken
Attinger C, Wolcott R (2012) Clinically addressing biofilm in chronic wounds. Adv Wound Care (New Rochelle) 1:127–132
Aurora A, Le TD, Akers KS, Blyth DM, Graybill JC, Clemens MS, Chung KK, Rizzo JA (2018) Recurrent bacteremia: a 10-year retrospective study in combat-related burn casualties. Burns 45(3):579–588
Balcazar JL, Subirats J, Borrego CM (2015) The role of biofilms as environmental reservoirs of antibiotic resistance. Front Microbiol 6:1216
Banu A, Noorul Hassan MM, Rajkumar J, Srinivasa S (2015) Spectrum of bacteria associated with diabetic foot ulcer and biofilm formation: a prospective study. Australas Med J 8:280–285
Blakeman JT, Morales-Garcia AL, Mukherjee J, Gori K, Hayward AS, Lant NJ, Geoghegan M (2019) Extracellular DNA provides structural integrity to a Micrococcus luteus biofilm. Langmuir 35:6468–6475
Bourdillon KA (2016) Dressings and biofilms: interpreting evidence from in vitro biofilm models. Wounds Int 7:9–14
Bourdillon KA, Delury CP, Cullen BM (2017) Biofilms and delayed healing – an in vitro evaluation of silver- and iodine-containing dressings and their effect on bacterial and human cells. Int Wound J 14:1066–1075
Cherny KE, Sauer K (2019) Pseudomonas aeruginosa requires the DNA-specific endonuclease EndA to degrade extracellular genomic DNA to disperse from the biofilm. J Bacteriol 201:e00059-19
Davis KA, Moran KA, Mcallister CK, Gray PJ (2005) Multidrug-resistant Acinetobacter extremity infections in soldiers. Emerg Infect Dis 11:1218–1224
De Oliveira A, Cataneli Pereira V, Pinheiro L, Moraes Riboli DF, Benini Martins K, Ribeiro de Souza da Cunha Mde L (2016) Antimicrobial resistance profile of planktonic and biofilm cells of Staphylococcus aureus and coagulase-negative staphylococci. Int J Mol Sci 17:1423
Donelli G, Vuotto C (2014) Biofilm-based infections in long-term care facilities. Future Microbiol 9:175–188
Esposito S, De Simone G (2017) Update on the main MDR pathogens: prevalence and treatment options. Infez Med 25:301–310
Flemming HC (2016) EPS-then and now. Microorganisms 4:41
Hall CW, Mah TF (2017) Molecular mechanisms of biofilm-based antibiotic resistance and tolerance in pathogenic bacteria. FEMS Microbiol Rev 41:276–301
Krishna BV, Gibb AP (2010) Use of octenidine dihydrochloride in meticillin-resistant Staphylococcus aureus decolonisation regimens: a literature review. J Hosp Infect 74:199–203
Lewis K (2010) Persister cells. Annu Rev Microbiol 64:357–372
Lipp C, Kirker K, Agostinho A, James G, Stewart P (2010) Testing wound dressings using an in vitro wound model. J Wound Care 19:220–226
Madsen JS, Burmolle M, Hansen LH, Sorensen SJ (2012) The interconnection between biofilm formation and horizontal gene transfer. FEMS Immunol Med Microbiol 65:183–195
Malone M, Bjarnsholt T, Mcbain AJ, James GA, Stoodley P, Leaper D, Tachi M, Schultz G, Swanson T, Wolcott RD (2017) The prevalence of biofilms in chronic wounds: a systematic review and meta-analysis of published data. J Wound Care 26:20–25
Molin S, Tolker-Nielsen T (2003) Gene transfer occurs with enhanced efficiency in biofilms and induces enhanced stabilisation of the biofilm structure. Curr Opin Biotechnol 14:255–261
Mork RL, Hogan PG, Muenks CE, Boyle MG, Thompson RM, Sullivan ML, Morelli JJ, Seigel J, Orscheln RC, Bubeck Wardenburg J, Gehlert SJ, Burnham CD, Rzhetsky A, Fritz SA (2020) Longitudinal, strain-specific Staphylococcus aureus introduction and transmission events in households of children with community-associated meticillin-resistant S aureus skin and soft tissue infection: a prospective cohort study. Lancet Infect Dis 20:188–198
Mulcahy H, Charron-Mazenod L, Lewenza S (2008) Extracellular DNA chelates cations and induces antibiotic resistance in Pseudomonas aeruginosa biofilms. PLoS Pathog 4:e1000213
Obermeier A, Schneider J, Harrasser N, Tubel J, Muhlhofer H, Pforringer D, Deimling CV, Foehr P, Kiefel B, Kramer C, Stemberger A, Schieker M, Burgkart R, Von Eisenhart-Rothe R (2018) Viable adhered Staphylococcus aureus highly reduced on novel antimicrobial sutures using chlorhexidine and octenidine to avoid surgical site infection (SSI). PLoS One 13:e0190912
Olwal CO, Ang’ienda PO, Onyango DM, Ochiel DO (2018) Susceptibility patterns and the role of extracellular DNA in Staphylococcus epidermidis biofilm resistance to physico-chemical stress exposure. BMC Microbiol 18:40
Omar A, Wright JB, Schultz G, Burrell R, Nadworny P (2017) Microbial biofilms and chronic wounds. Microorganisms 5:9
Pakharukova N, Tuittila M, Paavilainen S, Malmi H, Parilova O, Teneberg S, Knight SD, Zavialov AV (2018) Structural basis for Acinetobacter baumannii biofilm formation. Proc Natl Acad Sci U S A 115:5558–5563
Pang Z, Raudonis R, Glick BR, Lin TJ, Cheng Z (2018) Antibiotic resistance in Pseudomonas aeruginosa: mechanisms and alternative therapeutic strategies. Biotechnol Adv 37:177–192
Percival SL, Hill KE, Malic S, Thomas DW, Williams DW (2011) Antimicrobial tolerance and the significance of persister cells in recalcitrant chronic wound biofilms. Wound Repair Regen 19:1–9
Percival SL, Mccarty S, Hunt JA, Woods EJ (2014) The effects of pH on wound healing, biofilms, and antimicrobial efficacy. Wound Repair Regen 22:174–186
Percival SL, Mayer D, Malone M, Swanson T, Gibson D, Schultz G (2017a) Surfactants and their role in wound cleansing and biofilm management. J Wound Care 26:680–690
Percival SL, Mayer D, Salisbury AM (2017b) Efficacy of a surfactant-based wound dressing on biofilm control. Wound Repair Regen 25:767–773
Percival SL, Malone M, Mayer D, Salisbury AM, Schultz G (2018) Role of anaerobes in polymicrobial communities and biofilms complicating diabetic foot ulcers. Int Wound J 15:776–782
Pestrak MJ, Chaney SB, Eggleston HC, Dellos-Nolan S, Dixit S, Mathew-Steiner SS, Roy S, Parsek MR, Sen CK, Wozniak DJ (2018) Pseudomonas aeruginosa rugose small-colony variants evade host clearance, are hyper-inflammatory, and persist in multiple host environments. PLoS Pathog 14:e1006842
Ramani A, Ramani R, Shivananda PG, Kundaje GN (1991) Bacteriology of diabetic foot ulcers. Indian J Pathol Microbiol 34:81–87
Rogers KL, Fey PD, Rupp ME (2009) Coagulase-negative staphylococcal infections. Infect Dis Clin N Am 23:73–98
Salisbury AM, Chen R, Mullin M, Foulkes L, Percival SL (2019a) The effects of a concentrated surfactant gel on biofilm EPS. Surg Technol Int 36:31–35
Salisbury AM, Mullin M, Chen R, Percival SL (2019b) Efficacy of Poloxamer-based wound dressings on Acinetobacter baumanni biofilms. Adv Wound Care (New Rochelle) 8:463–468
Savage VJ, Chopra I, O’neill AJ (2013) Staphylococcus aureus biofilms promote horizontal transfer of antibiotic resistance. Antimicrob Agents Chemother 57:1968–1970
Schafer JJ, Mangino JE (2008) Multidrug-resistant Acinetobacter baumannii osteomyelitis from Iraq. Emerg Infect Dis 14:512–514
Serra R, Grande R, Butrico L, Rossi A, Settimio UF, Caroleo B, Amato B, Gallelli L, De Franciscis S (2015) Chronic wound infections: the role of Pseudomonas aeruginosa and Staphylococcus aureus. Expert Rev Anti-Infect Ther 13:605–613
Singh S, Singh SK, Chowdhury I, Singh R (2017) Understanding the mechanism of bacterial biofilms resistance to antimicrobial agents. Open Microbiol J 11:53–62
Stalder T, Top E (2016) Plasmid transfer in biofilms: a perspective on limitations and opportunities. NPJ Biofilms Microbiomes 2:16022
Stewart PS, Franklin MJ, Williamson KS, Folsom JP, Boegli L, James GA (2015) Contribution of stress responses to antibiotic tolerance in Pseudomonas aeruginosa biofilms. Antimicrob Agents Chemother 59:3838–3847
Suryaletha K, John J, Radhakrishnan MP, George S, Thomas S (2018) Metataxonomic approach to decipher the polymicrobial burden in diabetic foot ulcer and its biofilm mode of infection. Int Wound J 15:473–481
Van Acker H, Van Dijck P, Coenye T (2014) Molecular mechanisms of antimicrobial tolerance and resistance in bacterial and fungal biofilms. Trends Microbiol 22:326–333
Whitchurch CB, Tolker-Nielsen T, Ragas PC, Mattick JS (2002) Extracellular DNA required for bacterial biofilm formation. Science 295:1487
Yu MK, Kim MA, Rosa V, Hwang YC, Del Fabbro M, Sohn WJ, Min KS (2019) Role of extracellular DNA in Enterococcus faecalis biofilm formation and its susceptibility to sodium hypochlorite. J Appl Oral Sci 27:e20180699
Zhao G, Usui ML, Lippman SI, James GA, Stewart PS, Fleckman P, Olerud JE (2013) Biofilms and inflammation in chronic wounds. Adv Wound Care (New Rochelle) 2:389–399
Ziebuhr W, Hennig S, Eckart M, Kranzler H, Batzilla C, Kozitskaya S (2006) Nosocomial infections by Staphylococcus epidermidis: how a commensal bacterium turns into a pathogen. Int J Antimicrob Agents 28(Suppl 1):S14–S20
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Salisbury, AM., Mullin, M., Foulkes, L., Chen, R., Percival, S.L. (2021). The Ability of a Concentrated Surfactant Gel to Reduce an Aerobic, Anaerobic and Multispecies Bacterial Biofilm In Vitro. In: Donelli, G. (eds) Advances in Microbiology, Infectious Diseases and Public Health. Advances in Experimental Medicine and Biology(), vol 1323. Springer, Cham. https://doi.org/10.1007/5584_2020_609
Download citation
DOI: https://doi.org/10.1007/5584_2020_609
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-71201-3
Online ISBN: 978-3-030-71202-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)