Abstract
Waste collectors are exposed to a heterogeneous mixture of bioaerosols able to induce health effects. The study aim was to evaluate inflammatory processes in blood and in the respiratory tract via analysis of atopy and club cell secretory protein 16 (CC16) in serum, exhaled nitric oxide (FeNO), and cellular and soluble mediators in nasal lavage fluid (NALF) and induced sputum (IS). Sixty nine current waste collectors (48% smokers) and 28 former waste collectors (25% smokers) were included in the cross-sectional study. In both groups, 63 and 64% of workers reported complaints of the eyes, nose and/or upper airways. Thirty two percent of the current and 25% of the former workers were classified as atopics. More atopics suffered from rhinitis and conjunctivitis than non-atopics (64% vs. 40% in current workers; 71% vs. 40% in former workers). CC16 values of present non-smokers were significantly higher compared to smokers. In total, FeNO values of 31 participants were lower than 10 ppb, 94% of them were smokers and 85% had respiratory symptoms of lower airways. Most of the IS biomarkers were significantly higher in smokers than in non-smokers. Non-smoking workers with respiratory symptoms of lower airways had slightly elevated mediator IS concentrations compared to asymptomatic non-smokers. We conclude that inflammatory changes in waste collectors are detectable in the content of IS biomarkers, exhaled NO, and serum CC16, which all are influenced by the smoking habit. No significant differences in biomarkers are detectable between current and former waste collectors.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Club cell
- Exhaled nitric oxide
- Induced sputum
- Inflammatory markers
- Nasal lavage
- Non-invasive methods
- Occupational exposure
- Secretory protein
- Waste collectors
1 Introduction
Professional collection of municipal solid waste is a task with heavy physical activities and exposure to a heterogeneous mixture of bioaerosols, gases, and vapours such as microbial and non-microbial volatile organic compounds (Wouters et al. 2002; Poulsen et al. 1995). These multiple work demands and hazards result in a higher incidence of health problems and injuries compared to other occupations (Velasco et al. 2015). In addition to occupational accidents and musculoskeletal problems, workers in the waste collection industry may have elevated incidence rates of work-related pulmonary, gastrointestinal, and skin problems compared to the entire work force (Poulsen et al. 1995). An important occupational hazard for waste collectors is exposure to bioaerosols because of the handling of organic material (Neumann 2014; Widmeier et al. 2007). Collection of household waste, separation, and composting generate organic dust which may contain high amounts of endotoxin and (1–3)β-D-glucan, depending on storage conditions (Neumann 2015). There is evidence that diseases caused by organic dust are mainly of inflammatory nature (Schantora et al. 2015; Raulf et al. 2015). Cross-sectional and cohort studies (van Kampen et al. 2012, 2016; Bünger et al. 2000, 2007) have shown that workers exposed to organic dust from composting plants had a higher prevalence of inflammatory upper airway and eye responses, the so-called mucous membrane irritation syndrome (MMIS). In addition, cases of hypersensitivity pneumonitis, organic dust toxic syndrome (ODTS), and allergic bronchopulmonary aspergillosis are reported (Bünger et al. 2007; Allmers et al. 2000). Non-invasive methods, such as the measurement of fractional exhaled nitric oxide (FeNO) and the collection and analysis of exhaled breath condensate (Hoffmeyer et al. 2014; Hoffmeyer et al. 2009), nasal lavage fluid (NALF) (Wouters et al. 2002), and induced sputum (IS) are useful in the assessment of inflammatory responses in the upper and lower respiratory tract in exposed workers (Raulf et al. 2015; Raulf-Heimsoth et al. 2011). Several studies have also demonstrated that exposure to organic dust components increases permeability of the bronchoalveolar epithelial barrier, causing leakage of pneumoproteins such as club cell secretory protein (CC16) or surfactant protein A (Daneshzadeh Tabrizi et al. 2010; Widmeier et al. 2007; Steiner et al. 2005). Thus, determination of these proteins in the bloodstream is a suitable option to assess inflammatory processes in the respiratory tract.
The objective of the present study was to evaluate inflammatory processes in blood and in the upper and lower respiratory tract in current and former waste collectors. Additional aspects of the study dealt with the correlation between clinical symptoms (e.g. rhinitis, chronic bronchitis, etc.) and the profile of inflammatory cellular and soluble markers in NALF and IS samples and with the evaluation of factors influencing the content of inflammatory markers.
2 Methods
The study design and protocol were created in accordance with the Declaration of Helsinki for Human Research. In May 2012, the Ethics committee of the Ruhr-University Medical School Bochum approved the implementation of all necessary examinations. All study participants gave written informed consent to participate in the study.
2.1 Study Group and Data Collection
In this cross-sectional study, 69 current waste collectors (mean weekly working time 39 h) were examined, representing six municipal solid waste management companies of the Ruhr area in North Rhine-Westphalia, Germany. In addition, 28 former waste collectors were also included in the study. The protocol and exposure circumstances of the study group were recently published (Hoffmeyer et al. 2016; Schantora et al. 2015; Neumann 2014, 2015). All current and former workers visited the Institute for Prevention and Occupational Medicine of the German Social Accident Insurance, Institute of the Ruhr-University Bochum (IPA) for clinical examination and data assessment. To ensure realistic measurements, all current workers were examined in an afternoon during a working week after their shift. All subjects were male. Smoking status was based on self-assessed information by interview and justified by cotinine concentrations in urine according to Xu et al. (2004). Study participants were classified as present, former, and never-smokers. For classification of the study group according to their clinical symptoms, such as mucus membrane irritation, cough, and chronic bronchitis, questionnaire data were used (Schantora et al. 2015). Diagnosis of COPD was based on FEV1/FVC ratio below the lower limits of normal (LLN) as provided by the Global Lung Initiative (GLI) (Quanjer et al. 2012).
2.2 Measurements
Serological Parameters
Serum of each worker was collected to determine total and specific immunoglobulin E (sIgE) in response to a variety of ubiquitous aero-allergens (atopy screen sx1 Phadiatop), and a mold mix (mx1) using the ImmunoCAP system of ThermoFisher Scientific/Phadia (Uppsala, Sweden). Allergen sIgE values ≥0.35 kU/L were considered positive and in the case of sx1 it was used to assess the atopy status of the workers. Additionally, concentration of CC16 secretory protein (former CC10, uteroglobin, or urinary protein 1) was also determined using a sandwich ELISA from BioVendor (Brno, Czech Republik) with a standard range of 1.57–50 ng/mL.
Nitric Oxide in Exhaled Breath
FeNO was measured using a portable electrochemical analyser (NIOX Mino; Aerocrine, Solna, Sweden) according to the 2015 guidelines of the American Thoracic Society and European Respiratory Society (Hoffmeyer et al. 2016).
Nasal Lavage Fluid (NALF) and Induced Sputum (IS)
NALF was collected by introducing a syringe with a suitable adapter with 7 mL of sterile physiological saline solution into a nostril, followed by its aspiration; the procedure repeated five times (Raulf et al. 2016; Raulf-Heimsoth et al. 2011). The residual fluid volume of NALF was recorded, centrifuged (5 min at 1300 rpm), the cell-free supernatant was divided into portions and frozen at −80 °C until further analysis of soluble biomarkers. The cell pellets were re-suspended and the total cell number was determined using the Neubauer counting chamber. For differential cell counts, slides were prepared by cytospin (Cytospin 2; Shandon Corp., Pittsburgh, PA) and stained with May-Grünwald-Giemsa. Two independent observers counted 200 cells on each slide under light microscopy. Their results were expressed as the percentage of a total cell number and the absolute cell count.
IS of each subject was collected after inhalation of isotonic (0.9%) saline aerosol, generated by an ultrasonic nebulizer for 10 min as described earlier (Raulf et al. 2015; Raulf-Heimsoth et al. 2011). The subjects were motivated to cough actively, clear their throat, and expectorate sputum. The IS volume was determined and a 2.5-fold quantity of 0.1% sputulysin (dithiothreitol) was added. The samples were gently vortexed and incubated for 30 min at 37 °C to ensure a complete homogenization. After centrifugation, cell-free supernatants were aliquoted, stored at −80 °C under argon protection until further analysis of soluble markers. Cell pellets were further processed for the determination of the total cell number and for differential cytology, using the procedure described above for NALF.
The inflammatory mediators in NALF and IS were determined in the thawed cell-free supernatants. All samples underwent only a single freeze-thaw cycle. In both IS and NALF samples, the following soluble markers were measured: interleukin (IL)-8, total protein content, 8-isoprostane (8-iso-PGF2α), soluble (s)CD14, matrix metalloproteinase (MMP)-9, and tissue inhibitors of metalloproteinases (TIMP)-1. IL-8 was measured with the OptEIA™ ELISA (BD Biosciences Pharmingen; Heidelberg, Germany) in a standard range of 3–200 pg/mL. 8-isoprostane was quantified with a competitive immunoassay (Assay Design; Ann Arbor, CA) in a standard range of 6.1–100 ng/mL. Determinations of sCD14, TIMP-1, and MMP-9 were performed with the DuoSet™ ELISA Development system (R&D Systems; Wiesbaden Germany) in a standard range of 62.5–4,000 pg/mL for sCD14 and 31.2–2000 pg/mL for both MMP-9 and TIMP-1. Eosinophilic cationic protein (ECP) was quantified with the ImmunoCAP system from Thermo Fisher Scientific (Phadia AB, Uppsala, Sweden). Total protein content was determined according to the method of Bradford (1976) with bovine serum albumin as standard solution (range 10–100 μg/mL).
2.3 Statistical Analysis
Data were expressed as median with min-max range (tables) or interquartile range (figures). Data distribution was assessed using the D’Agostino and Pearson omnibus normality test. Values below the limit of quantification (LOQ) were set 2/3 of the LOQ. Comparison of unpaired data was performed with Mann-Whitney U or Kruskal-Wallis test and that of habits, e.g. smoking, between different groups with the Dunn multiple comparison test. A two-sided significance level of 0.05 was chosen for all tests. Data were analyzed using GraphPad Prism version 5.01 for Windows (GraphPad Software, San Diego, CA).
3 Results
Table 1a presents the characteristics of the study group. The median age of the 69 current workers was 48 yr (range 23–63 yr) and median duration of employment was 22 yr (range 2–36 yr). The former waste collectors were older (median age 62 yr) at the time of examination with the median of 25 yr of employment (range 11–38 yr). Forty eight percent of current and 25% of former workers were present smokers. A high percentage (63% and 64%, respectively) of the workers reported complaints from the eyes, nose and/or upper airways (Table 1b). Ten percent of current waste workers had COPD and all of them were present smokers. Four out of the 28 (14%) of the former waste workers had COPD and one of them never smoked. A higher prevalence of current and former waste collectors with employment duration ≤20 yr reported symptoms from the upper respiratory tract (Table 1c). Although the percentage of current waste workers with symptoms from the lower respiratory tract was independent of employment duration, the percentage of present non-smokers (never and former smokers) in the group with longer employment was higher.
Data on the serum total and specific IgE and CC16 are summarized in Table 2. Elevated levels (>100 kU/L) of total IgE were present in 20 and 21% of current and former workers, respectively. Specific IgE values against the mold mixture were rare. Only 9% of current workers and 3.6% of former workers had a positive IgE response to the mold mixture. According to the sIgE-values in the inhalation atopy screening, 32% of current and 25% of former workers were classified as having atopy, without significant differences concerning smoking status. Rhinitis and/or conjunctivitis were more often reported in atopics than in non-atopics (64% vs. 40% in current workers and 71% vs. 40% in former workers). The serum CC16 concentration was significantly higher in never smokers than in present smokers in both current and former workers. In the current workers, former smokers also had a significant higher CC16 concentration than the present smokers. In the current workers, CC16 concentration was >2 ng/mL (limit of quantification) in just 52% of smokers, whereas CC16 exceeded that level in 84% of the never smokers. Similar differences were observed in the group of former waste collectors.
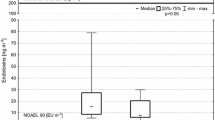
Since the serum CC16 concentration was not different between former and never smokers, both groups are combined for further CC16 comparison with present non-smokers and smokers. Figure 1 shows the median CC16 concentration in present smokers and non-smokers, representing both current and former workers, with or without symptoms from the lower respiratory tract. The CC16 concentration of present smokers with symptoms was significantly lower compared with present non-smokers with (p < 0.05) or without (p < 0.001) symptoms. The CC16 concentration of present smokers without symptoms was not significantly different compared with present non-smokers with symptoms. There was no difference in CC16 concentration between present non-smokers with and without lower respiratory tract symptoms.
Club cell protein (CC16) concentration in the study group (n = 97) stratified by smoking and symptoms from lower respiratory tract. P < 0.001 for differences among all four groups using Kruskal-Wallis test with Gaussian approximation and Dunn’s multiple comparison test. Additionally, significant differences exist between present smokers with symptoms vs. present non-smokers with (p < 0.05) and without symptoms (p < 0.001)
There were no significant differences in FeNO level between current and former workers (Table 3). The FeNO of 26 current workers was lower than 10 ppb, 92% of them were smokers and one half them had symptoms from the lower respiratory tract. Classification of all workers examined according to their smoking habits into present smokers and non-smokers, taking also into account the presence or absence of symptoms from the lower respiratory tract demonstrated that present smokers with or without symptoms had significantly lower FeNO values than the present non-smokers (Fig. 2). FeNO values of present non-smokers with or without symptoms were not different. Two non-smoking workers out of the 11 with symptoms from the lower respiratory tract had the FeNO exceeding 25 ppb.
Influence of smoking habits and symptoms from lower respiratory tract on exhaled nitric oxide content (FeNO). There were significant differences between present non-smokers, with or without symptoms, and present smokers (p < 0.001). No difference was observed between non-smokers with and without symptoms
The results of cellular and soluble biomarkers measured in NALF samples of current workers are summarized in Table 4a and those of former workers are in Table 4b. There were no significant differences in the current waste collectors depending on the smoking habits, although the concentration of soluble biomarkers and the percentage of neutrophils tended to be lower in present smokers than in never smokers. The same trend was observed in former workers, although here two parameters reached significance, i.e., the percentage of neutrophils was significantly lower in present smokers than in never and former smokers and the sCD14-concentrations were significantly lower in present smokers than in former smokers. Comparison of NALF parameters between current and former waste collectors was inconspicuous. Classification of the subjects according to the presence of nasal symptoms (rhinitis yes or no) and their smoking habits showed no differences regarding the biomarkers in NALF (data not shown).
Table 5a summarizes the results of soluble biomarkers measured in IS samples of current waste collectors classified into never, former, and present smokers. The percentage of neutrophils, IL-8, TIMP-1, and total protein concentrations were significantly higher in smokers than in never or former smokers. Although all other IS parameters were higher in smokers than in never or former smokers, the differences did not reach statistical significance. A similar trend was observed in the former waste collectors (Table 5b), i.e., there were higher values in present smokers, but only the IL-8 level was significantly different between smokers and former smokers. In both groups, there were no significant differences in IS parameters between never and former smokers and, additionally, no differences between the current and former waste collectors. Therefore, to clarify the association between symptoms from the lower respiratory tract (cough, chronic bronchitis, or COPD) and inflammatory IS markers the study group was divided into four groups: present smokers with (A) and without (B) lower respiratory tract symptoms and present non-smokers with (C) and without (D) lower respiratory tract symptoms (Table 5c).
A significantly higher percentage of neutrophils (p < 0.05) was measured in IS samples of smoking subjects suffering from lower respiratory tract symptoms (group A) compared with non-smoking healthy subjects (group D). A similar pattern was detected for IL-8, i.e., significantly higher IL-8 concentration in both groups of smokers (groups A and C) and increasing, but not statistically different, IL-8 concentration between non-smokers with and without respiratory symptoms (group C vs. D). The level of the sputum immunoreactive MMP-9, TIMP-1, ECP, and sCD14 did not differ among the four groups. However, different concentrations of 8-isoprostane and total protein were found between groups B and D, both without clinical symptoms, with higher levels in smoking subjects (group B).
4 Discussion
Household waste collectors are exposed on a daily basis to significantly higher concentrations of bioaerosols than that present in the general living environment. In addition to our recently published data concerning health complaints of waste collectors (Hoffmeyer et al. 2016), here we studied the inflammatory propensity as evaluated from the content of serum total and specific IgE and CC16, and FeNO, and biomarkers in NALF and IS samples in current and former waste collectors. Since cigarette smoking is a well-known inducer of lung inflammatory processes, smoking habits were taken into account for all data analysis.
Specific IgE responses against the mold mix were rare in both current and former waste collectors and the number of subjects classified as atopics was nearly the same. The findings demonstrate that serum concentration of CC16, a sensitive biomarker of lung injury (Heldal et al. 2013), was not different between current and former waste collectors, but it was highly affected by smoking. CC16 is released by epithelial cells into the serum and provides an indication of acute exposure processes. Under chronic exposures causing tissue damage, CC16 concentration tends to be low. This is the case in chronic exposure to cigarette smoke, which damages club cells resulting in decreased serum CC16 (Hermans and Bernard 1999). The present findings demonstrate that the smoking current and former waste collectors had a significantly lower CC16 concentration than never smokers. Additionally, CC16 concentration of present smokers with symptoms from the lower respiratory tract was significantly lower than that of present non-smokers with and without symptoms from the lower respiratory tract. No significant difference in CC16 content was found in waste collectors with or without symptoms from the lower respiratory tract. Norwegian workers exposed to sewage dust, containing a high content of a complex mix of microorganisms and their components, chemicals and gases, had a lower serum concentration of CC16 compared to the referents, also pointing to a long-term effect on secretion of this pneumoprotein (Heldal et al. 2013). That study has also shown that exposure to bacteria is associated with CC16 concentration, which may reflect a transient increased permeability of the lung-blood barrier. One reason for such results may be enhanced bioaerosol exposure, especially to endotoxin, in workers exposed to sewage dust (Heldal et al. 2016) compared to household waste collectors (Neumann 2014, 2015). Additionally, it should be taken into account that CC16 content is controlled by other factors, such as CC16 production by club cells, release into the alveolar space, renal clearance, and diffusion into the serum affected by pulmonary epithelial barrier permeability. Therefore, interpretation of CC16 content should be considered with caution (Lakind et al. 2007). A strong effect of smoking on the CC16 content also could be due to smoking-induced inhibition of activity of NO synthases (NOS), measurable as a lower level of fractional exhaled nitric oxide (FeNO) in smokers. In the present study, the majority of FeNO values were below 10 ppb in present smokers. The level of FeNO, as a biomarker of lower airway eosinophilic inflammation, was not different in present non-smokers, with and without clinical symptoms from the respiratory tract. Additionally, only two non-smokers with lower respiratory tract symptoms had FeNO above 25 ppb, indicating that eosinophilic Th2 driven (allergic) inflammation is not predominant in household waste collectors.
In this study we used a simple non-invasive technique of nasal lavage to evaluate inflammatory reactions in the upper airways. The findings demonstrate no appreciable differences in cellular and soluble markers of NALF between current or former workers or between workers with and without clinical symptoms from the upper airways. Conspicuously, however, content of biomarkers was lower in present smokers than that in non-smokers. In contrast to our results, which likely reflected subchronic effects of exposure to cigarette smoke, Heldal et al. (2003) have found an acute increase in NALF biomarkers in waste handlers, associated with neutrophil infiltration, after three working days from Monday to Thursday after a weekend break. Those authors have not observed any cigarette smoking dependencies.
In the present study we detected pronounced inflammatory effects concerning the cellular and soluble sputum biomarkers. There were apparent differences between present and never or former smokers. Akin to previous studies conducted in composting plant workers (Raulf et al. 2015) and bitumen exposed workers (Raulf-Heimsoth et al. 2011), immunoreactive MMP-9 concentration in sputum was higher in smokers than in present non-smokers. We failed to confirm signs of remission of a subchronic inflammatory state in workers exposed to bioaerosols once exposure is terminated, observed in our previous study in composting plant workers (Raulf et al. 2015) and in a study of Sikkeland et al. (2012) in workers exposed to organic dust. Some sputum biomarkers such as neutrophils, IL-8, MMP-9, TIMP-1, and 8-isoprostane, were higher in former than never smoking waste collectors, which however failed to reach statistical significance. Taking lower airway symptoms into account, as expected, smoking caused greater effects on the biomarker content. Although IL-8, MMP-9, TIMP-1, and 8-isoprostane concentrations tended to be higher in non-smokers with lower airway symptoms compared with non-smokers without the symptoms, no significant difference were detectable.
The cross-sectional design of the present study, without a control group, is a weakness. Longitudinal studies consisting of a non-invasive assessment of inflammatory biomarkers should be performed in waste collectors to examine the possible causal relationship between working environment, exposure, and respiratory health problems. However, a strength of the present study is that all measurements were done with standardized, validated procedures in 69 current waste collectors and 28 former waste collectors, and the potential confounding factors such as smoking, age, and atopy were taken into consideration. Our results also provide an indication that allergic Th2-triggered inflammation was not the primary health problem in the workers with a median employment of 22 yr. This may be a result of a not more explained “healthy worker effect.” Although the inflammatory effects measured were not statistically different between non-smokers with or without respiratory symptoms, implementation of the biomarker measurement using different matrices is useful to assess the airway condition in waste collectors exposed to bioaerosols. In this population of blue-color workers anti-smoking and dust reduction programs should be implemented to avoid airway inflammation and respiratory health problems.
References
Allmers H, Huber H, Baur X (2000) Two year follow-up of a garbage collector with allergic bronchopulmonary aspergillosis (ABPA). Am J Ind Med 37(4):438–442
Bradford MM (1976) A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72:248–254
Bünger J, Antlauf-Lammers M, Schulz TG, Westphal GA, Muller MM, Ruhnau P, Hallier E (2000) Health complaints and immunological markers of exposure to bioaerosols among biowaste collectors and compost workers. Occup Environ Med 57(7):458–464
Bünger J, Schappler-Scheele B, Hilgers R, Hallier E (2007) A 5-year follow-up study on respiratory disorders and lung function in workers exposed to organic dust from composting plants. Int Arch Occup Environ Health 80(4):306–312
Daneshzadeh Tabrizi R, Bernard A, Thommen AM, de Winter F, Oppliger A, Hilfiker S, Tschopp A, Hotz P (2010) Surfactant protein-D and exposure to bioaerosols in wastewater and garbage workers. Int Arch Occup Environ Health 83(8):879–886
Heldal KK, Halstensen AS, Thorn J, Djupesland P, Wouters IM, Eduard W, Halstensen TS (2003) Upper airway inflammation in waste handlers exposed to bioaerosols. Occup Environ Med 60(6):444–450
Heldal KK, Barregard L, Larsson P, Ellingsen DG (2013) Pneumoproteins in sewage workers exposed to sewage dust. Int Arch Occup Environ Health 86(1):65–70
Heldal KK, Barregard L, Ellingsen DG (2016) Biomarkers of inflammation in workers exposed to compost and sewage dust. Int Arch Occup Environ Health 89(5):711–718
Hermans C, Bernard A (1999) Lung epithelium-specific proteins: characteristics and potential applications as markers. Am J Respir Crit Care Med 159(2):646–678
Hoffmeyer F, Raulf-Heimsoth M, Brüning T (2009) Exhaled breath condensate and airway inflammation. Curr Opin Allergy Clin Immunol 9(1):16–22
Hoffmeyer F, van Kampen V, Taeger D, Deckert A, Rosenkranz N, Kassen M, Schantora AL, Brüning T, Raulf M, Bünger J (2014) Prevalence of and relationship between rhinoconjunctivitis and lower airway diseases in compost workers with current or former exposure to organic dust. Ann Agric Environ Med 21(4):705–711
Hoffmeyer F, van Kampen V, Schantora AL, Deckert A, Neumann HD, Brüning T, Raulf M, Bünger J (2016) Gesundheitsbeeinträchtigungen bei aktuell und ehemals Beschäftigten der Abfallsammlung. ASU Arbeitsmed Sozialmed Umweltmed 51:276–285. Article in German
Lakind JS, Holgate ST, Ownby DR, Mansur AH, Helms PJ, Pyatt D, Hays SM (2007) A critical review of the use of Clara cell secretory protein (CC16) as a biomarker of acute or chronic pulmonary effects. Biomarkers 12(5):445–467
Neumann HD (2014) Schimmelpilzbelastung bei der Abfallsammlung. Gefahrstoffe – Reinhaltung der Luft 74:483–491. Article in German
Neumann HD (2015) Staub-, Endotoxin- und Antigenkonzentrationen bei der Abfallsammlung. Gefahrstoffe – Reinhaltung der Luft 75(7/8):275–284. Article in German
Poulsen OM, Breum NO, Ebbehoj N, Hansen AM, Ivens UI, van Lelieveld D, Malmros P, Matthiasen L, Nielsen BH, Nielsen EM (1995) Collection of domestic waste. Review of occupational health problems and their possible causes. Sci Total Environ 170(1–2):1–19
Quanjer PH, Stanojevic S, Cole TJ, Baur X, Hall GL, Culver BH, Enright PL, Hankinson JL, Ip MSM, Zheng J, Stocks J (2012) Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J 40(6):1324–1343
Raulf M, Hoffmeyer F, van Kampen V, Deckert A, Brüning T, Bünger J (2015) Cellular and soluble inflammatory markers in induced sputum of composting plant workers. Adv Exp Med Biol 858:19–29
Raulf M, Weiss T, Lotz A, Lehnert M, Hoffmeyer F, Liebers V, van Gelder R, Käfferlein HU, Hartwig A, Pesch B, Brüning T (2016) Analysis of inflammatory markers and metals in nasal lavage fluid of welders. J Toxicol Environ Health A 79(22–23):1144–1157
Raulf-Heimsoth M, Pesch B, Kendzia B, Spickenheuer A, Bramer R, Marczynski B, Merget R, Brüning T (2011) Irritative effects of vapours and aerosols of bitumen on the airways assessed by non-invasive methods. Arch Toxicol 85(Suppl 1):41–52
Schantora AL, Casjens S, Deckert A, van Kampen V, Neumann HD, Brüning T, Raulf M, Bünger J, Hoffmeyer F (2015) Prevalence of work-related rhino-conjunctivitis and respiratory symptoms among domestic waste collectors. Adv Exp Med Biol 834:53–61
Sikkeland LIB, Eduard W, Skogstad M, Alexis NE, Kongerud J (2012) Recovery from workplace-induced airway inflammation 1 year after cessation of exposure. Occup Environ Med 69(10):721–726
Steiner D, Jeggli S, Tschopp A, Bernard A, Oppliger A, Hilfiker S, Hotz P (2005) Clara cell protein and surfactant protein B in garbage collectors and in wastewater workers exposed to bioaerosols. Int Arch Occup Environ Health 78(3):189–197
van Kampen V, Deckert A, Hoffmeyer F, Taeger D, Brinkmann E, Brüning T, Raulf-Heimsoth M, Bünger J (2012) Symptoms, spirometry, and serum antibody concentrations among compost workers exposed to organic dust. J Toxicol Environ Health A 75(8–10):492–500
van Kampen V, Hoffmeyer F, Deckert A, Kendzia B, Casjens S, Neumann HD, Buxtrup M, Willer E, Felten C, Schoneich R, Brüning T, Raulf M, Bünger J (2016) Effects of bioaerosol exposure on respiratory health in compost workers: a 13-year follow-up study. Occup Environ Med 73:829–837
Velasco GM, Bittner C, Harth V, Preisser AM (2015) Health status and health-related quality of life of municipal waste collection workers – a cross-sectional survey. J Occup Med Toxicol 10:22
Widmeier S, Bernard A, Tschopp A, Jeggli S, Dumont X, Hilfiker S, Oppliger A, Hotz P (2007) Surfactant protein a, exposure to endotoxin, and asthma in garbage collectors and in wastewater workers. Inhal Toxicol 19(4):351–360
Wouters IM, Hilhorst SKM, Kleppe P, Doekes G, Douwes J, Peretz C, Heederik D (2002) Upper airway inflammation and respiratory symptoms in domestic waste collectors. Occup Environ Med 59(2):106–112
Xu X, Iba MM, Weisel CP (2004) Simultaneous and sensitive measurement of anabasine, nicotine, and nicotine metabolites in human urine by liquid chromatography-tandem mass spectrometry. Clin Chem 50(12):2323–2330
Acknowledgment
The study was conducted with the help of the German Social Accident Insurance, Institution for the public sector in North Rhine-Westphalia, Düsseldorf, Germany. We would like to thank the waste collectors for participating in the study. We gratefully acknowledge the support of the laboratory and clinical staff for their skilful technical assistance. Supported in part by the German Social Accident Insurance (project IPA-94).
Conflicts of Interest
The authors declare no conflicts of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Raulf, M. et al. (2017). Airway and Blood Inflammatory Markers in Waste Collectors. In: Pokorski, M. (eds) Pulmonary Care and Clinical Medicine. Advances in Experimental Medicine and Biology(), vol 1021. Springer, Cham. https://doi.org/10.1007/5584_2017_25
Download citation
DOI: https://doi.org/10.1007/5584_2017_25
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-65468-3
Online ISBN: 978-3-319-65469-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)