Abstract
For several solid human malignancies, currently available serum biomarkers are insufficiently reliable to distinguish patients from healthy individuals. Metabonomics, the study of metabolic processes in biologic systems, is based on the use of 1H-NMR spectroscopy and multivariate statistics for biochemical data generation and interpretation and may provide a characteristic fingerprint in disease. Here we review our initial experiences utilizing the metabonomic approach for discriminating sera from women with epithelial ovarian cancer (EOC) from healthy controls. 1H-NMR spectroscopic analysis was performed on preoperative serum specimens of 38 EOC patients, 12 patients with benign ovarian cysts and 53 healthy women. PCA analysis allowed correct separation of all serum specimens from 38 patients with EOC (100%) from all of the 21 premenopausal normal samples (100%) and from all the sera from patients with benign ovarian disease (100%). In addition, it was possible to correctly separate 37 of 38 (97.4%) cancer specimens from 31 of 32 (97%) postmenopausal control sera. ROC analysis indicated that the sera from patients with and without disease could be identified with 100% sensitivity and specificity at the 1H-NMR regions 2.77 parts per million (ppm) and 2.04 ppm from the origin (AUC of ROC curve = 1.0). These findings indicate that the 1H-NMR metabonomic approach deserves further evaluation as a potential novel strategy for the early detection of EOC.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
- Epithelial Ovarian Cancer
- Principal Component Analysis Model
- Epithelial Ovarian Cancer Patient
- Receiver Operate Characteristic Curve Analysis
- Receiver Operate Characteristic Curve Curve
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Background
Cancer is a major public health problem. Current estimates suggest that approximately three out of every ten individuals will be diagnosed with cancer at some point during their lifetime (Wingo et al. 1995). Screening and early detection are two strategies with the potential to reduce morbidity and mortality from a particular cancer among the screened population. Although significant advances have been made in screening/early detection of cancers of the breast, cervix, skin, and colon, there are no reliable early detection strategies for cancers of the pancreas, lungs and epithelial ovarian cancer (EOC). This review focuses on the use of 1H-NMR-based metabonomics as a potential method for early detection of EOC.
Ovarian cancer is the leading cause of death from gynecologic malignancies. There are more than 23,000 cases annually in the United States, and approximately 14,000 women can be expected to die from the disease in 2007. Survival rates remain disappointing for patients with advanced EOC and primary peritoneal carcinomas despite modest improvements in response rates, progression-free survival and median survival using adjuvant platinum and paclitaxel chemotherapy following cytoreductive surgery (Armstrong et al. 2006; McGuire et al. 1996). This has been attributed to two important reasons. First, in contrast to most other solid tumors, more than 75% of EOC patients present with advanced-stage disease (FIGO III or IV). Whereas the small proportion of patients with accurately diagnosed stage I disease have 5-year survival rates in excess of 90% (Young et al. 1990), the survival rate for women diagnosed with distant disease is only 25%. Secondly, although most patients with advanced disease initially respond to platinum- and paclitaxel-based chemotherapy including complete responses, the relapse rate is approximately 85% (Greenlee et al. 2001). Within 2 years of cytoreductive surgery and systemic chemotherapy, tumors usually recur and once relapse occurs, there is no known curative therapy. The link between stage and mortality suggests that early detection may have a significant impact on disease morbidity and mortality in EOC. The need for early detection is especially acute in women who have a high risk of ovarian cancer due to family or personal history of cancer, and for women with a genetic predisposition to cancer due to abnormalities in predisposition genes such as BRCA1 and BRCA2.
Although a number of potential early detection strategies have been studied in EOC (Menon and Jacobs 2000), these have shown only limited promise. The ideal test for the early detection of EOC should be noninvasive, acceptable to the screened population, have high validity, and have a relatively low cost. The application of novel approaches such as functional genomics, proteomics and metabonomics may improve the ability to detect EOC at an early stage, with the potential of reducing morbidity and mortality from the disease.
2 Current Status of Early Detection of EOC in the General Population
The majority of patients with EOC come from low-risk families and are usually diagnosed due to symptoms of advanced disease. Current candidate strategies for early detection of EOC in this population are based on biochemical tumor markers evaluated mainly in the blood and biophysical markers assessed by ultrasound and/or Doppler imaging of the ovaries. The only biomarker that has been extensively studied for possible use in the early detection of EOC is CA125, a high-molecular-weight glycoprotein of unknown function (Dorum et al. 1996; Fures et al. 1999). Although CA-125 has good utility for monitoring effects of treatment and for recurrence of ovarian cancer, its effectiveness as a screening tool is limited. A systematic review of the performance of the multimodal strategies of CA125 and ultrasound indicated that approximately 50% (95% confidence interval [CI] 23; 77) and 75% (95% CI 35; 97) of patients were diagnosed at stage I in CA-125-based and ultrasound screening studies, respectively (Reviews 2003). Unfortunately, the positive predictive values (PPV) of these strategies for the early detection of EOC using these modalities have been consistently less than 10% (Reviews 2003; van Nagell et al. 2000). Attempts to improve the PPV of these early detection strategies in EOC have met with limited success. These include the utilization of complex longitudinal algorithms for CA125 (McIntosh et al. 2002; Skates et al. 1995, 2003; Zhang et al. 1999), sequential testing (Berek and Bast 1995; Jacobs et al. 1999) and the addition of newer markers such as OVX-1 (Bast et al. 1983), M-CSF (Suzuki et al. 1993), lysophosphatidic acid (Xu et al. 1998), osteopontin (Kim et al. 2002) and Kallikrein 11 (McIntosh et al. 2007). In light of these considerations, novel approaches are needed for the early detection of EOC.
3 NMR-Based Metabonomics for the Analysis of Biofluids
An alternative approach for early detection of EOC is to utilize a novel and unique strategy that provides a coherent perspective of the complete metabolic response of organisms to pathophysiological insult or genetic modification (Nicholson et al. 1999). This approach to the study of metabolic processes in biological systems has been termed metabonomics (Nicholson et al. 1999) and is the focus of this paper. We have hypothesized that the analysis of a global view of metabolites in serum would enhance the possibility of identifying metabonomic signatures for EOC. Metabonomics is based on the use of NMR (and other spectroscopic methods) and multivariate statistics for biochemical data generation and interpretation. NMR spectroscopy is based on using nuclear spins to probe their chemical environment when placed in a static external magnetic field. Nuclei with a spin quantum number 1/2 are best suited and include 1H, 13C, 15N and 31P. Since protons are present in almost all metabolites in body fluids, a 1H-NMR spectrum allows the simultaneous detection and quantification of thousands of proton-containing, low-molecular-weight species within a biological matrix, resulting in the generation of an endogenous profile that may be altered in disease to provide a characteristic fingerprint (Lindon et al. 1999, 2000; Nicholson et al. 1999, 2002).
There are several advantages of NMR-based metabonomics in a clinical setting. It can be performed on standard preparations of serum, plasma, saliva or urine, circumventing the need for specialist preparations of cellular RNA and protein required for genomics and proteomics, respectively (Lindon et al. 2000, 2001; Nicholson and Wilson 1989; Holmes et al. 2001). Moreover, since cancer is now known to be a product of the tumor–host microenvironment (Liotta and Kohn 2001), the organ-specific milieu can generate, and enzymatically modify, multiple proteins, peptides, metabolites, and cleavage products at much higher concentrations than for molecules derived only from the tumor cells.
4 1H-NMR Analysis of Plasma and Cancer Detection
The initial report indicating that 1H-NMR spectroscopy of plasma might be useful for cancer detection was published in 1986 by Fossel et al. (Fossel et al. 1986). The report was based on the measurements of 1H-NMR spectra of plasma samples (at either 360 or 400 MHz 1H resonance frequency and at 20–22°C) for 331 subjects, including controls, patients with various types of malignant and benign tumors and pregnant women, and examination of the spectra by applying a parameter, Fossel Index (FI) which is calculated as a mean of the approximate widths at half-height of the methylene and methyl resonance envelopes. Although it appeared possible to clearly and reliably distinguish between normal controls (FI = 39.5 ± 1.6 Hz) and patients with malignant tumors (FI = 29.9 ± 2.5 Hz), in many subsequent studies, a remarkable overlap between cancer patients and controls was noted. This led to an intensive interlaboratory evaluation of the reproducibility and accuracy of the NMR human blood test for cancer by Chmurny et al. (Chmurny et al. 1988). This test was found to be reproducible but not accurate for screening a general asymptomatic population for cancer.
There are several limitations of these early studies. First, affected subjects in these studies had cancer of different organ sites and histologies. Clearly, there is great variability in the biology, invasiveness and metastatic potential of different tumors, and it would be surprising to find a single test that could reliably detect all or even a large number of cancers (Chmurny et al. 1988). Secondly, the predictive value of a positive screening test for cancer needs to be considered not only in the context of sensitivity and specificity, but also the prevalence of disease in the population (for example, the prevalence of EOC is relatively low). Finally, and most importantly, the early NMR studies are different from metabonomics because of the significant improvements in high-resolution NMR technology and novel computationally intense and robust analytic methods for 1H-NMR spectroscopic data interpretation. These approaches, previously unavailable, have opened new avenues for disease diagnosis and management, as evidenced by the recent successful application of metabonomics to coronary heart disease (Brindle et al. 2002) and hypertension (Brindle et al. 2003), and in our studies of women with ovarian cancer.
5 1H-NMR-Based Metabonomics for Ovarian Cancer Detection
We recently conducted a study to evaluate the utility of using 1H-NMR-based metabonomic analysis to discriminate samples from women with EOC from healthy controls, and women with benign ovarian diseases (Odunsi et al. 2005). Preoperative serum samples of 38 patients with EOC undergoing surgery at the Roswell Park Cancer Institute (RPCI) were collected under an approved institutional review board (IRB) protocol. The stage distribution of the EOC patients were as follows: stage I: two patients; stage IIIC: 34 patients; stage IV: two patients. Among patients with advanced disease (stages IIIC and IV), four (11%) had normal preoperative serum CA125 levels (<35 units/ml). In addition, preoperative CA125 was normal in one of the two patients with stage I disease. The age range of the study patients was 46–86 years. For controls, the sera of 53 normal healthy women (pre- and postmenopausal controls), and 12 patients with benign ovarian cysts were collected under two additional IRB protocols at RPCI. The age range of the healthy premenopausal controls was 22–44 years, while the remaining 32 postmenopausal controls had an age range of 45–75 years. The age range of the 12 patients with benign ovarian cysts was 22–68.There were no significant differences between the study subjects and postmenopausal controls with respect to age, parity and use of oral contraceptives. Aliquots of serum were stored at −80°C until assayed.
5.1 1H-NMR Spectroscopic Analysis of the Serum Samples
Samples (100 μl) were diluted with solvent solution (99.9% D2O) (450 μl) in 5-mm precision NMR tubes (Norell, Inc., Landisville, NJ, USA). Conventional 1H-NMR spectra of the serum samples were measured at 600.22 MHz on a Bruker AMX-600 spectrometer (Billerica, MA) operating at 600 MHz 1H frequency, using the pulse sequence: RD–90°–t1–90°–tm–90°, acquire free induction decay (FID) (i.e., the NOESYPR1D pulse sequence). RD represents a relaxation delay of 1.5 s during which the water resonance is selectively irradiated, and t1 corresponds to a fixed interval of 4 μs. The water resonance is irradiated for a second time during the mixing time (tm, 100 ms). For each sample, 128 FIDs were collected into 64 k data points using a spectral width of 12.2 kHz and an acquisition time of 2.69 s. The FIDs were multiplied by an exponential weighting function corresponding to a line broadening of 0.25 Hz before Fourier transformation. The acquired NMR spectra were corrected for phase and baseline distortions using UXNMR (version 97) and referenced to lactate (CH3δ1.33). Chemical components were assigned to the spectra on the basis of previously published data (Ala-Korpela 1995; Nicholson et al. 1995). Figure 1a shows the 600-MHz 1H-NMR spectra of serum from a postmenopausal patient with stage 1 EOC, Fig. 1b shows the spectra from a healthy postmenopausal patient, Fig. 1c shows the spectra from a healthy premenopausal patient, while Fig. 1d shows the spectra from a patient with ovarian endometriosis. In order to remove any ambiguity in assigned chemical shift values, samples were spiked with a small amount of three reference compounds to test whether perfect superposition of the signals could be achieved. A sample of alanine was added first, followed by valine, and then glucose with spectra acquired after each addition. In each case, the resonances of the reference fell directly on top of the assigned resonances in the biofluid.
Comparison of patients with EOC with healthy subjects. The 600-MHz 1H-NMR spectra of serum samples from a postmenopausal stage 1 EOC patient (a), a premenopausal healthy subject (b), a postmenopausal healthy subject (c), and a patient with benign ovarian cyst (endometriosis) (d). The chemical shifts of a selection of major metabolites are indicated, based on comparison with published metabolites (Pretsch et al. 1989)
5.2 Data Reduction of NMR Data
The 1H-NMR spectra (δ10–0.2) were automatically data-reduced to 200–250 integral segments of equal length (δ0.04) using NutsPro (version 20021122, Acorn NMR, Inc., Livermore, CA, USA). Each segment consisted of the integral of the NMR region to which it was associated. To remove the effects of variation in the suppression of the water resonance, the region δ5.5 to 4.75 was set to zero integral. The data were normalized to total spectral area and centered scaling was applied.
5.3 Pattern Recognition Analysis of the 1H-NMR Spectra
Principal component analysis (PCA) is an unsupervised method (i.e., analysis performed without use of knowledge of the sample class) that reduces the dimensionality of the data input while expressing much of the original n-dimensional variance in a 2D or 3D map (Eriksson et al. 1999). Prior to PCA analysis, all NMR data were mean-centered and pareto-scaled (Wold et al. 1998) to give each variable a variance numerically equal to its standard deviation. PCA was carried out on the 1H-NMR data from the sera of EOC patients and controls to plot data in order to indicate relationships between samples in the multidimensional space. The principal components were displayed as a set of scores (t), which highlight clustering or outliers, and a set of loadings (p), which highlight the influence of input variables on t. This data set of NMR spectra displayed good discrimination between EOC patients and controls. Thus, we were able to correctly separate all of the 38 cancer specimens (100%) and all of the 21 premenopausal normal samples (100%) (Fig. 2a). In addition, it was possible to correctly separate 37 of 38 (97.4%) cancer specimens and 31 of 32 (97%) postmenopausal control serum specimens (Fig. 2b). When patients with benign ovarian disease were included in the PCA analysis, it was still possible to correctly separate all of 38 cancer specimens (100%) from the sera of all 12 patients with benign ovarian disease (Fig. 2c). Although sera from patients with benign disease overlapped with sera from the healthy controls, it was possible to achieve separation of cancer versus noncancer cases. All PCA plots indicated that most of the variation occurred in the first two principal components.
PCA plots of factor scores for the first two principal components (t[1], t[2]) showing the considerable separation achieved between EOC serum samples (X, ■), healthy postmenopausal controls (▼) and benign ovarian cysts (○). Note that optimum separation occurred in the second principle component. Patients with stage I EOC are denoted by X
5.4 Soft Independent Modeling of Class Analogy
In order to provide validation of the results, a supervised analysis of the data was performed based on soft independent modeling of class analogy (SIMCA). Since the majority of EOC patients in our study and in clinical practice are postmenopausal, we chose to perform further analysis by comparing the benign and cancer patients with healthy postmenopausal controls. SIMCA utilizes the features of PCA to construct significance limits for specified classes of samples in the scores and the residual direction. Mapping of unknown samples onto the calculated models provides the class identity based on similarity between the unknown samples and the samples in the predefined class models. A method of visualizing the SIMCA approach is the Cooman's plot (Coomans et al. 1984), which plots class distances against each other. We built separate PCA models for the sera of EOC patients and postmenopausal healthy controls. SIMCA was then applied to the models using the Cooman's plot and the classification performance was assessed by predicting class membership in terms of distance from the model. The critical distance from the model used corresponded to a 0.05 level, and defined a 95% tolerance interval. The resulting Cooman's plot demonstrated that sera classes from patients with EOC, benign ovarian cysts and the postmenopausal healthy controls did not share multivariate space, providing validation for the class separation (Fig. 3). Therefore, it should be possible to predict whether future samples can be classified as cancer or noncancer. This preliminary data demonstrated that 1H-NMR-based metabonomic analysis of serum samples could achieve a clinically useful performance for the identification of serum samples of patients with EOC.
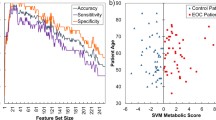
5.5 Receiver Operating Characteristic Curve Analysis
Univariate receiver operating characteristic curve (ROC) analyses were carried out via individual logistic regressions for each of 219 1H-NMR regions in order to examine their utility for predicting EOC. The sensitivity and specificity trade-offs were summarized for each variable using the area under the ROC curve denoted AUC, and calculated using the trapezoidal rule. An AUC value of 1.0 corresponds to a prediction model with 100% sensitivity and 100% specificity, while an AUC value of 0.5 corresponds to a poor predictive model (see Pepe et al. 1997 for an overview of ROC analyses via logistic regression modeling). The best two variable models were then fit starting from the univariate information via a forward stepwise selection using the AUC as the criteria for a variable's entry into the model. The data showed that a two variable model consisting of 1H-NMR regions 2.77 ppm from the origin and 2.04 ppm from the origin provided a perfect fitting model, i.e., AUC = 1.0. A scatterplot is provided in Fig. 4, which clearly illustrates the delineation between the two groups. Of note, the univariate model that considered only region 2.04 ppm gave an AUC = 0.942, while the AUC for the univariate model for region 2.77 ppm gave an AUC = 0.689, i.e., prediction based upon region 2.04 is enhanced conditional upon the information contained in region 2.77 ppm. We hypothesize that the preliminary information that we have derived from this ROC analysis will allow us to refine this model for early-stage EOC, and that this approach could represent a novel strategy for the early detection of EOC.
5.6 Analysis of Spectral Pattern Differences
Based on the promising results showing complete separation of patients with EOC and controls using unsupervised PCA, supervised SIMCA, and ROC analyses applied to 1H-NMR spectra of sera, we have proceeded to identify the molecules responsible for the differences in spectral patterns utilizing a previously described methodology (Gavaghan et al. 2000). The regions of the NMR spectrum that most strongly influence separation between EOC and healthy controls are indicated by the regression coefficients (data not shown). The coefficients were derived from the PCA models and each bar represents a spectral region covering 0.04 ppm, showing how the 1H-NMR profile of the EOC samples differed from the 1H-NMR profile of the healthy serum samples. A negative value indicates a relatively greater concentration of metabolite (assigned using NMR chemical shift assignment tables) present in EOC samples and a positive value indicates a relatively lower concentration, with respect to EOC samples. In general, the regression coefficients, or loadings, most influential for the EOC samples compared with postmenopausal controls lie around δ3.7 ppm (due to various sugar hydrogens) while the loadings most influential for the EOC samples compared with premenopausal controls lie around δ2.25 (due to acetoacetate). Other loadings suggest greater amounts of 3-hydroxybutyrate and isobutyrate in the sera of EOC patients compared with pre- and postmenopausal controls. These differences are also readily apparent on visual inspection of the spectra. The biological significance of these observations is currently unclear.
5.7 Validation of EOC Results in an Independent Set of Serum Specimens
In an effort to validate the results described above, we recently examined an independent set of specimens from the Databank and Biorepository core facility at Roswell Park Cancer Institute. We compared 20 patients with stage III ovarian cancer with age-matched controls. The results confirm our original data and indicate considerable separation of EOC patients from healthy controls by PCA and PLS-DA methods (Fig. 5a and b).
5.8 Mass Spectrometry-Based Metabolic Profiling in Ovarian Cancer
In a recent study, the combination of gas chromatography/time-of-flight mass spectrometry (GC-TOF MS) was used to analyze 66 invasive ovarian carcinomas and nine borderline tumors of the ovary (Denkert et al. 2006). After automated mass spectral deconvolution, 291 metabolites were detected, of which 114 (39.1%) were annotated as known compounds. Principal component analysis (PCA) revealed four principal components that were significantly different between the two groups, with the highest significance found for the second component (p = 0.00000009). PCA as well as additional supervised predictive models allowed a separation of 88% of the borderline tumors from the carcinomas. Using the KEGG database, the authors linked metabolic changes to putative key enzymes that play an important role in the corresponding pathways. These include enzymes that regulate pyrimidine metabolism such as dihydropyrimidine dehydrogenase and thymidine phosphorylase. The unique aspect of the study is the demonstration that metabolic profiling using GC-TOF MS is suitable for analysis of fresh frozen human tumor samples. Moreover, there appears to be a consistent and significant change in primary metabolism of ovarian tumors, which can be detected using multivariate statistical approaches.
In another recent study, peptides were extracted from frozen tissues of 25 ovarian carcinomas (stages III and IV) and 23 benign ovaries; and analyzed using MALDI-TOF MS, nanoESI MS and MS/MS (Lemaire et al. 2007). A marker with anm/z of 9744 corresponding to 84 amino acid residues from the 11S proteasome activator complex (PA28 or Reg-alpha) was identified. This marker was subsequently validated using MALDI imaging, classical immunocytochemistry with an antibody raised against the C-terminal part of the protein, and Western blot analysis. Together these two studies (Denkert et al. 2006; Lemaire et al. 2007) indicate that direct tissue analysis by mass spectrometry-based strategies can facilitate biomarker discovery and validation in human cancers.
6 Conclusions and Future Directions
There have been remarkable efforts by several groups of investigators to identify reliable markers for early detection of a wide range of solid tumors, including epithelial ovarian cancer (EOC). High-throughput metabolite profiling and protein expression analysis aimed at the identification of metabolites that are generated as a consequence of tumor–host interaction could provide a strategy for (a) discriminating cancer cases from healthy control candidates and (b) identifying a panel of metabolites that could be useful as biomarkers of early detection and targets of therapy. The rapid development of metabonomics and proteomics-based technologies are bringing new perspectives that will likely integrate both approaches leading to a comprehensive and global view of cancer cell behavior. Widespread and routine use of metabonomics for cancer diagnosis will require the implementation of carefully developed SOPs based on larger studies in various cancer types. The identification of a repertoire of metabolites and proteins that mark the transition from normal to the transformed phenotype should allow detection of cancer at a preclinical stage, where the chances for cure would be highest.
References
Ala-Korpela M (1995) 1H-NMR spectroscopy of human blood plasma. Prog Nucl Magn Reson Spectrosc 27:475–554
Armstrong DK, Bundy B, Wenzel L, Huang HQ, Baergen R, Lele S, Copeland LJ, Walker JL, Burger RA (2006) Intraperitoneal cisplatin and paclitaxel in ovarian cancer. N Engl J Med 354:34–43
Bast RC Jr, Klug TL, St John E, Jenison E, Niloff JM, Lazarus H, Berkowitz RS, Leavitt T, Griffiths CT, Parker L, Zurawski VR Jr, Knapp RC (1983) A radioimmunoassay using a monoclonal antibody to monitor the course of epithelial ovarian cancer. N Engl J Med 309:883–887
Berek JS, Bast RC Jr (1995) Ovarian cancer screening. The use of serial complementary tumor markers to improve sensitivity and specificity for early detection. Cancer 76:2092–2096
Brindle JT, Antti H, Holmes E, Tranter G, Nicholson JK, Bethell HW, Clarke S, Schofield PM, McKilligin E, Mosedale DE, Grainger DJ (2002) Rapid and noninvasive diagnosis of the presence and severity of coronary heart disease using 1H-NMR-based metabonomics. Nat Med 8:1439–1444
Brindle JT, Nicholson JK, Schofield PM, Grainger DJ, Holmes E (2003) Application of chemometrics to 1H NMR spectroscopic data to investigate a relationship between human serum metabolic profiles and hypertension. Analyst 128:32–36
Chmurny GN, Hilton BD, Halverson D, McGregor GN, Klose J, Issaq HJ, Muschik GM, Urba WJ, Mellini ML, Costello R et al (1988) An NMR blood test for cancer: a critical assessment. NMR Biomed 1:136–150
Coomans D, Broeckaert I, Derde MP, Tassin A, Massart DL, Wold S (1984) Use of a microcomputer for the definition of multivariate confidence regions in medical diagnosis based on clinical laboratory profiles. Comput Biomed Res 17:1–14
Denkert C, Budczies J, Kind T, Weichert W, Tablack P, Sehouli J, Niesporek S, Konsgen D, Dietel M, Fiehn O (2006) Mass spectrometry-based metabolic profiling reveals different metabolite patterns in invasive ovarian carcinomas and ovarian borderline tumors. Cancer Res 66:10795–10804
Dorum A, Kristensen GB, Abeler VM, Trope CG, Moller P (1996) Early detection of familial ovarian cancer. Eur J Cancer 32A:1645–1651
Eriksson L, Johansson E, Kettaneh-Wold N, Wold S (1999) Introduction to multi- and megavariate data analysis using projection methods (PCA, PLS) Umetrics, Umea, Sweden
Fossel ET, Carr JM, McDonagh J (1986) Detection of malignant tumors. Water-suppressed proton nuclear magnetic resonance spectroscopy of plasma. N Engl J Med 315:1369–1376
Fures R, Bukovic D, Hodek B, Klaric B, Herman R, Grubisic G (1999) Preoperative tumor marker CA125 levels in relation to epithelial ovarian cancer stage. Coll Antropol 23:189–194
Gavaghan CL, Holmes E, Lenz E, Wilson ID, Nicholson JK (2000) An NMR-based metabonomic approach to investigate the biochemical consequences of genetic strain differences: application to the C57BL10J, Alpk:ApfCD mouse. FEBS Lett 484:169–174
Greenlee RT, Hill-Harmon MB, Murray T, Thun M (2001) Cancer statistics, 2001. CA Cancer J Clin 51:15–36
Holmes E, Nicholson JK, Tranter G (2001) Metabonomic characterization of genetic variations in toxicological and metabolic responses using probabilistic neural networks. Chem Res Toxicol 14:182–191
Jacobs IJ, Skates SJ, MacDonald N, Menon U, Rosenthal AN, Davies AP, Woolas R, Jeyarajah AR, Sibley K, Lowe DG, Oram DH (1999) Screening for ovarian cancer: a pilot randomised controlled trial. Lancet 353:1207–1210
Kim JH, Skates SJ, Uede T, Wong KK, Schorge JO, Feltmate CM, Berkowitz RS, Cramer DW, Mok SC (2002) Osteopontin as a potential diagnostic biomarker for ovarian cancer. JAMA 287:1671–1679
Lemaire R, Menguellet SA, Stauber J, Marchaudon V, Lucot JP, Collinet P, Farine MO, Vinatier D, Day R, Ducoroy P, Salzet M, Fournier I (2007) Specific MALDI imaging and profiling for biomarker hunting and validation: fragment of the 11S proteasome activator complex reg alpha fragment is a new potential ovary cancer biomarker. J Proteome Res 6:4127–4134
Lindon JC, Nicholson JK, Everett JR (1999) NMR spectroscopy of biofluids. Annu Rep NMR Spectrosc 38:1–88
Lindon JC, Nicholson JK, Holmes E, Everett JR (2000) Metabonomics: metabolic processes studied by NMR spectroscopy of biofluids. Concepts Magn Reson 12:289–320
Lindon JC, Holmes E, Nicholson JK (2001) Pattern recognition methods and applications in biomedical magnetic resonance. Prog Nucl Magn Reson Spectrosc 39:1–40
Liotta LA, Kohn EC (2001) The microenvironment of the tumour-host interface. Nature 411:375–379
McGuire WP, Hoskins WJ, Brady MF, Kucera PR, Partridge EE, Look KY, Clarke-Pearson DL, Davidson M (1996) Cyclophosphamide and cisplatin versus paclitaxel and cisplatin: a phase III randomized trial in patients with suboptimal stage III/IV ovarian cancer (from the Gynecologic Oncology Group). Semin Oncol 23:40–47
McIntosh MW, Urban N, Karlan B (2002) Generating longitudinal screening algorithms using novel biomarkers for disease. Cancer Epidemiol Biomarkers Prev 11:159–166
McIntosh MW, Liu Y, Drescher C, Urban N, Diamandis EP (2007) Validation and characterization of human kallikrein 11 as a serum marker for diagnosis of ovarian carcinoma. Clin Cancer Res 13:4422–4428
Menon U, Jacobs IJ (2000) Recent developments in ovarian cancer screening. Curr Opin Obstet Gynecol 12:39–42
Nicholson JK, Wilson ID (1989) High resolution proton magnetic resonance spectroscopy of biological fluids. Prog Nucl Magn Reson Spectrosc 21:449–501
Nicholson JK, Foxall PJ, Spraul M, Farrant RD, Lindon JC (1995) 750 MHz 1H and 1H-13C NMR spectroscopy of human blood plasma. Anal Chem 67:793–811
Nicholson JK, Lindon JC, Holmes E (1999) `Metabonomics': understanding the metabolic responses of living systems to pathophysiological stimuli via multivariate statistical analysis of biological NMR spectroscopic data. Xenobiotica 29:1181–1189
Nicholson JK, Connelly J, Lindon JC, Holmes E (2002) Metabonomics: a platform for studying drug toxicity and gene function. Nat Rev Drug Discov 1:153–161
Odunsi K, Wollman RM, Ambrosone CB, Hutson A, McCann SE, Tammela J, Geisler JP, Miller G, Sellers T, Cliby W, Qian F, Keitz B, Intengan M, Lele S, Alderfer JL (2005) Detection of epithelial ovarian cancer using 1H-NMR-based metabonomics. Int J Cancer 113:782–788
Pepe MS (1997) A regression modeling framework for receiver operating characteristic curves in medical diagnostic testing. Biometrika 84:595–608
Pretsch E, Seibl J, Simon W, Clerc T (1989) Spectral data for structure determination of organic compounds. Springer-Verlag, Berlin Heidelberg New York
Reviews E (2003) Database of abstracts of reviews of effects NHS Centre for Reviews and Dissemination. Screening for ovarian cancer. Database of Absracts of Reviews of Effectiveness
Skates SJ, Xu FJ, Yu YH, Sjovall K, Einhorn N, Chang Y, Bast RC Jr, Knapp RC (1995) Toward an optimal algorithm for ovarian cancer screening with longitudinal tumor markers. Cancer 76:2004–2010
Skates SJ, Menon U, MacDonald N, Rosenthal AN, Oram DH, Knapp RC, Jacobs IJ (2003) Calculation of the risk of ovarian cancer from serial CA-125 Values for preclinical detection in postmenopausal women. J Clin Oncol 21:206–210
Suzuki M, Ohwada M, Aida I, Tamada T, Hanamura T, Nagatomo M (1993) Macrophage colony-stimulating factor as a tumor marker for epithelial ovarian cancer. Obstet Gynecol 82:946–950
van Nagell JR Jr, DePriest PD, Reedy MB, Gallion HH, Ueland FR, Pavlik EJ, Kryscio RJ (2000) The efficacy of transvaginal sonographic screening in asymptomatic women at risk for ovarian cancer. Gynecol Oncol 77:350–356
Wingo PA, Tong T, Bolden S (1995) Cancer statistics, 1995. CA Cancer J Clin 45:8–30
Wold S, Antti H, Lindgren F, Ohman J (1998) Orthogonal signal correction of near-infrared spectra. Chemom Intell Lab Syst 44:175–185
Xu Y, Shen Z, Wiper DW, Wu M, Morton RE, Elson P, Kennedy AW, Belinson J, Markman M, Casey G (1998) Lysophosphatidic acid as a potential biomarker for ovarian and other gynecologic cancers. JAMA 280:719–723
Young RC, Walton LA, Ellenberg SS, Homesley HD, Wilbanks GD, Decker DG, Miller A, Park R, Major F Jr (1990) Adjuvant therapy in stage I and stage II epithelial ovarian cancer. Results of two prospective randomized trials. N Engl J Med 322:1021–1027
Zhang Z, Barnhill SD, Zhang H, Xu F, Yu Y, Jacobs I, Woolas RP, Berchuck A, Madyastha KR, Bast RC Jr (1999) Combination of multiple serum markers using an artificial neural network to improve specificity in discriminating malignant from benign pelvic masses. Gynecol Oncol 73:56–61
Acknowledgements
I thank Dr. Thomas Szyperski for helpful discussions. Supported by the Oshei Foundation, Roswell Park Cancer Center Support Grant P30CA16056 and R21 CA106949–01A1 from the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Editor information
Rights and permissions
Copyright information
© 2008 Springer-Verlag Berlin Heidelberg
About this paper
Cite this paper
Odunsi, K. (2008). Cancer Diagnostics Using 1H-NMR-Based Metabonomics. In: Kroemer, G., Mumberg, D., Keun, H., Riefke, B., Steger-Hartmann, ., Petersen, K. (eds) Oncogenes Meet Metabolism. Ernst Schering Foundation Symposium Proceedings, vol 2007/4. Springer, Berlin, Heidelberg. https://doi.org/10.1007/2789_2008_095
Download citation
DOI: https://doi.org/10.1007/2789_2008_095
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-540-79477-6
Online ISBN: 978-3-540-79478-3
eBook Packages: MedicineMedicine (R0)