Abstract
Approximately one third of depressed patients fail to respond to currently available antidepressant therapies. Therefore, new conceptual frameworks are needed to identify pathophysiologic pathways and neurobiological targets for the development of novel treatment strategies. In this regard, recent evidence suggests that inflammation may contribute to symptoms relevant to a number of psychiatric disorders and particularly depression. Numerous studies (including meta-analyses) have found elevated peripheral and central inflammatory cytokines and acute phase proteins in depression. Chronic exposure to increased inflammation is thought to drive changes in neurotransmitters and neurocircuits that lead to depressive symptoms and that may also interfere with or circumvent the efficacy of antidepressants. Indeed, patients with high inflammation have been shown to exhibit poor response to conventional antidepressant therapies. Recent developments in our ability to understand and measure the effects of inflammation on the brain in patients have opened new doors for the testing of novel treatment strategies that target the immune system or its consequences on neurotransmitter systems. Such recent developments in the field of behavioral immunology and their translational implications for the treatment of depression are discussed herein.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Anhedonia
- Anti-inflammatories
- Anxiety
- Cytokines
- Depression
- Dopamine
- Glutamate
- Inflammation
- Motor slowing
- Neuroimaging
1 Introduction
A growing body of evidence suggests that inflammation plays a role in psychiatric illnesses and especially major depressive disorder (MDD) (Howren et al. 2009; Miller et al. 2017). Inflammatory markers, including cytokines, chemokines, and acute phase reactants like C-reactive protein (CRP), are reliably increased in a number of depressed patients with respect to controls (Howren et al. 2009; Maes et al. 1997; Haapakoski et al. 2015). Furthermore, elevated CRP and other peripheral blood markers of inflammation have been found to predict future development of depression (Wium-Andersen et al. 2013; Gimeno et al. 2009; Au et al. 2015). Although not every patient with MDD has increased inflammation, it is thought that elevated levels of inflammation may contribute to the disease process and to specific symptoms in a subgroup of patients within this complex and heterogeneous disease.
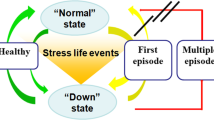
Recent data indicate that increasing plasma CRP (as well as cytokines and their soluble receptors) is associated with decreased functional connectivity within corticostriatal reward and motor circuitry and with increased central nervous system (CNS) glutamate in patients with MDD, which correlates with symptoms of anhedonia and motor slowing (Felger et al. 2016; Haroon et al. 2016). These findings in depressed patients with elevated levels of inflammation are strikingly similar to the effects of peripheral administration of inflammatory stimuli on neural activity in reward and motor circuitry, as well as the effects of exogenously administered inflammatory stimuli on CNS neurotransmitters such as glutamate and dopamine (DA) (Felger et al. 2013a; Capuron et al. 2012; Eisenberger et al. 2010; Harrison et al. 2015a; Haroon et al. 2015). Therefore, elevated levels of inflammation in the blood of patients with MDD may reflect increased inflammatory activity in the CNS and its effects on neural systems and neurotransmitters (Felger et al. 2018). Interestingly in this regard, MDD patients with high levels of CRP and other markers of peripheral inflammation have been found to exhibit resistance to conventional antidepressant therapies (Strawbridge et al. 2015; Cattaneo et al. 2013, 2016). This chapter will review the sources of inflammation in depression, its consequences on the brain, and how it has led to trials of novel immune-based therapies and treatments that reverse the effects of inflammation on neurotransmitter systems (Fig. 1).
Mechanisms of inflammation effects on the brain and behavior and targets for intervention in depression. Inflammation is increased in patients with major depressive disorder (MDD) due to environmental exposures, genetics, psychosocial stressors, diet, and other lifestyle factors (i.e., smoking) and medical illnesses. Innate immune cell activation and the release of inflammatory cytokines cause both increased CRP production from the liver and effects on brain neurotransmitters and circuits to drive relevant behavioral changes. Evidence indicates that inflammation and cytokines may preferentially affect dopamine and glutamate systems to disrupt circuits involved in reward and motor activity, as well as those involved anxiety and emotional regulation. In terms of potential novel therapies that may target inflammation or its effects on the brain, there is current interest in treatment strategies that affect the immune system to decrease inflammation (1), drugs that increase dopamine synthesis or synaptic availability or that decrease glutamate signaling (2), and lifestyle changes or alternative therapies that modify the sources of inflammation in MDD patients (3). CRP C-reactive protein, dACC dorsal anterior cingulate cortex, vmPFC ventromedial prefrontal cortex
2 Evidence of Increased Inflammation in Depression and Treatment Implications
2.1 Increased Peripheral and Central Inflammation
Numerous studies have reported increased circulating inflammatory cytokines, such as interleukin (IL)-1, IL-6, and tumor necrosis factor (TNF), their soluble receptors, and acute phase reactants, like C-reactive protein (CRP), in patients with MDD (Maes 1999; Maes et al. 1992; Sluzewska 1999). These findings have been corroborated by meta-analyses (Howren et al. 2009; Dowlati et al. 2010). The American Heart Association considers peripheral CRP >3 mg/L, e.g., “high CRP,” to be associated with the greatest risk for development of cardiovascular disease relative to concentrations considered low (<1 mg/L) and moderate (1–3 mg/L) (Ridker 2003). These guidelines for risk of heart disease are consistent with emerging evidence that inflammation serves as a common mechanism of disease affecting multiple bodily systems, including the brain (Couzin-Frankel 2010). Not every MDD patient exhibits high concentrations of inflammatory markers or CRP, yet “high” CRP >3 mg/L is detected in a substantial proportion of patients, 20–50% depending on the sample. Even higher CRP concentrations are observed in patients who are resistant to standard antidepressant therapies (Felger et al. 2016; Haroon et al. 2016; Rapaport et al. 2016; Raison et al. 2013a; Uher et al. 2014). CRP, an acute phase reactant produced by the liver in response to innate immune cytokines, notably IL-6 and TNF, is used in clinical practice as a biomarker of systemic inflammation. Although CRP does play a role in activating the complement system (Rhodes et al. 2011; Devaraj et al. 2009), it is not thought to be a primary driver of inflammation effects on the brain. Rather, cytokines and downstream inflammatory mediators are known to exert effects on neurons and glia, which then drive changes in brain function. Nevertheless, CRP is associated with the activity of other inflammatory molecules, is routinely measured across medical centers and research laboratories (Aziz et al. 2003; Coventry et al. 2009), and is being used in clinical trials in MDD to target anti-cytokine therapies in patients with elevated levels of inflammation (Miller et al. 2017; Raison et al. 2013a).
With such strong evidence for increased inflammatory markers in the periphery of patients with psychiatric illness, there has been growing interest in finding ways to more directly measure the activation of inflammatory processes in the brain. Increased inflammatory cytokine concentrations in the cerebrospinal fluid (CSF) of patients with MDD have been observed (Levine et al. 1999; Schwieler et al. 2015; Garver et al. 2003; Soderlund et al. 2009, 2011). Additionally, increased CSF cytokines have been associated with the severity of depression and with improvement in symptoms in response to successful treatment (Levine et al. 1999; Lindqvist et al. 2009; Martinez et al. 2012). Despite intense efforts to measure inflammation in the brain by neuroimaging, positron emission tomography (PET) for imaging upregulation of the translocator protein (TSPO) on activated microglia and macrophages using ligands such as [11C]PK 11195 (Venneti et al. 2007; Cagnin et al. 2007), [11C]PBR28 (Imaizumi et al. 2007), and [18F]FEPPA (Wilson et al. 2008) in MDD patients has yielded mixed results. For example, in a sample of patients with mild to moderate MDD using [11C]PBR28, no differences were found between patients and controls, though the sample was small and the depression severity was relatively low (Hannestad et al. 2012a). In contrast, the use of [18F]FEPPA in a more severely depressed sample showed significantly increased binding in the striatum, hippocampus, insula, and prefrontal cortex (Setiawan et al. 2015), yet no significant relationship was found between peripheral inflammatory markers and central TSPO binding. These findings are in contrast to studies in nonhuman primates (NHP) and in healthy humans where peripheral inflammatory cytokines were increased in response to a peripheral inflammatory challenge in association with increased [11C]PBR28 (Hannestad et al. 2012a; Sandiego et al. 2015), which was found primarily in microglia (Hannestad et al. 2012a). These data raise questions regarding what specifically TSPO binding is measuring in patients. More studies are likely needed prior to the use of such techniques in clinical trials exploring novel anti-inflammatory therapies.
2.2 Sources of Innate Immune Activation and Inflammation
Depressed patients who are otherwise medically healthy may experience chronic levels of increased innate immune system activation and inflammation due to a variety of environmental exposures including psychosocial stress (and particularly early life stress and trauma), sleep disturbance, inflammatory diet, gastrointestinal permeability, obesity, and other lifestyle factors such as smoking (Berk et al. 2013). History of childhood trauma is often associated with elevated inflammatory biomarkers and higher rates of depression as adults (Danese et al. 2008). Thus a “biological embedding” or imprinting of stress through inflammatory processes in childhood has been described (Danese et al. 2011). MDD patients with a history of early life stress have been shown to respond to psychological stress (the Trier Social Stress Test) with exaggerated circulating IL-6 production and increased DNA binding of nuclear factor (NF)-kB in peripheral blood mononuclear cells compared to non-depressed controls (Pace et al. 2006). In adolescents with a history of childhood adversity, high IL-6 production has been shown to precede subsequent development of depression 6 months later (Miller and Cole 2012), indicating causal relationships between early life stress, increased inflammation, and depression. Regarding mechanisms, recent work has demonstrated that stress can activate the inflammatory response through sterile inflammatory processes using signals called damage-associated molecular patterns (DAMPs), as well as by bacteria and bacterial products such as microbial-associated molecular patterns (MAMPs) leaked from the gut (Wong et al. 2016; Fleshner 2011, 2013). DAMPS refer to molecules produced as a function of cellular stress and accelerated metabolism, such as uric acid, adenosine triphosphate (ATP), glucose, and heat shock proteins (Fleshner 2013; Maslanik et al. 2012). DAMPS and MAMPS can then lead to stimulation of the NLRP3 inflammasome and NF-kB in monocytes, ultimately leading to the production of inflammatory cytokines including IL-1, IL-18, IL-6, and TNF (Maslanik et al. 2012; Iwata et al. 2013).
Additional environmental and lifestyle factors such as sleep disturbance may also contribute to increased inflammation in depression (Opp et al. 2007; Suarez 2008). Disturbed sleep increases circulating IL-6, TNF, and CRP (Meier-Ewert et al. 2004; Vgontzas et al. 2004), and sleep impairments in psychiatric illnesses such as depression have been associated with increased inflammation (Opp et al. 2007; Motivala et al. 2005). Furthermore, inflammatory diets that promote gut permeability and changes in the microbiota, smoking, and increased body mass index (BMI) all contribute to increased inflammation and may interact with genetics and stress to contribute to behavioral symptoms and poor overall health outcomes in patients with psychiatric illness (Berk et al. 2013; Jamal et al. 2014). For example, obesity from consumption of a high-fat diet in rodents induces changes in the gut microbiota and increases ileal inflammation and permeability (de La Serre et al. 2010). Obesity and high BMI are associated with increased concentrations of IL-6 and other inflammatory markers in humans (Khaodhiar et al. 2004; Lim et al. 2005) thought to be the result of macrophage accumulation in adipose tissue, and especially visceral adiposity, which can release cytokines into the portal circulation (Weisberg et al. 2003; Suganami and Ogawa 2010; Park et al. 2005).
2.3 Gene Expression and Genetic Predisposition
Several functional allelic variants and single-nucleotide polymorphisms (SNPs) of genes encoding immune and inflammatory molecules have been associated with depression, including those encoding expression of inflammatory cytokines, major histocompatibility complex proteins, B and T cells, and inflammatory mediators like cyclooxygenase-2 (Bosker et al. 2011; Raison and Miller 2013; Bufalino et al. 2012). These findings have engendered speculation as to whether alleles that promote enhanced inflammatory cytokine secretion were evolutionarily advantageous and thus conserved (Raison and Miller 2013). Indeed, heightened inflammatory responses to environmental stimuli may have improved survival by conferring greater protection from bacterial and viral infection (Raison and Miller 2013). Further, genetic priming to respond to stress and the environment with increased inflammatory and antiviral responses could contribute to the high prevalence of psychiatric disorders comorbid with medical illnesses that are associated with inflammation (e.g., cardiovascular disease, metabolic disorders, and autoimmune disorders) (Yirmiya et al. 1999, 2000; Raison and Miller 2003; Evans et al. 1999; Pollak and Yirmiya 2002; Shelton and Miller 2010). In addition to genetic polymorphisms, increased inflammatory gene expression has been found in circulating immune cells80 as well as in brains of patients with MDD (Shelton et al. 2011).
2.4 Influence of High Inflammation on Antidepressant Treatment Response
Current antidepressant therapies are effective for many patients with MDD. However, up to 30% fail to achieve remission, and even antidepressant responders often exhibit significant residual symptoms consistent with many of those caused by exposure to cytokines and inflammation, such as anhedonia, fatigue, and psychomotor retardation (Targum and Fava 2011; Rush 2007; Dunlop and Nemeroff 2007; Trivedi et al. 2008; Nierenberg 2015). Nonresponsiveness of inflammation-related symptoms to standard antidepressant therapies has been exemplified in cancer patients and in those patients receiving IFN-α therapy treated with SSRIs to alleviate inflammation-related depression and fatigue (Bower et al. 2002; Miller et al. 2008; Ahles et al. 2002). SSRIs alleviated cancer-related or IFN-α-induced anxiety and some depressive symptoms, but not those of fatigue or psychomotor retardation (Capuron et al. 2002a; Raison et al. 2005a; Morrow et al. 2003). A similar lack of response to SSRIs in patients with increased inflammation has also been observed in MDD. For instance, patients with higher levels of CRP (>1 mg/L) have been found to demonstrate worse response to the SSRI escitalopram but to have more favorable responses to the noradrenergic antidepressant nortriptyline (Uher et al. 2014; Jha et al. 2017). Measurement of inflammatory cytokine mRNA expression in peripheral immune cells was even more predictive than CRP of this effect (Cattaneo et al. 2013, 2016). Additionally, MDD patients with high inflammation have been shown to respond better to adjuvant or novel therapies that boost monoamine availability or that target glutamate (Jha et al. 2017; Yang et al. 2015; Shelton et al. 2015). Therefore, it is important to better understand the mechanisms by which inflammation affects the brain in order to develop novel therapies or to appropriately target existing therapies to patients with elevated levels of inflammation.
3 Inflammation Effects on the Brain and Behavior
3.1 Immunologic Mechanisms
Immune Signaling in the Brain
Peripheral inflammation and cytokines may signal the CNS to initiate local immune activation by several mechanisms, including (1) passage of cytokines through leaky regions in the blood-brain barrier at circumventricular organs (Katsuura et al. 1990; Pan and Kastin 2003), (2) active uptake mechanisms of cytokines across the blood-brain barrier (Banks and Erickson 2010; Banks et al. 1995, 2002), and (3) local actions at peripheral vagal nerve afferents that relay inflammatory signals to relevant brain regions, including the nucleus of the solitary tract and hypothalamus (the so-called neural route) (Bluthe et al. 1994; Ericsson et al. 1994; Watkins et al. 1994, 1995). However, recent translational data indicate that during peripheral inflammation, activated monocytes/macrophages traffic to the brain in response to monocyte chemoattractant protein (MCP-1), a chemokine produced by activated microglial cells in response to cytokine signaling from the periphery (D’Mello et al. 2009, 2015). These monocytes/macrophages traffic primarily to perivascular and meningeal spaces and have been shown to contribute to behavioral changes in rodent models of stress-induced depressive and anxiety behaviors (Wohleb et al. 2012, 2014; Hodes et al. 2014). Interestingly, patterns of gene expression in the peripheral blood of patients with psychiatric disorders exhibit increased signatures consistent with pro-inflammatory “M1” activation of monocyte/macrophages (Mostafavi et al. 2014; Brambilla et al. 2014; Drago et al. 2015). Furthermore, recruitment of activated peripheral macrophages to perivascular spaces, as well as localized activation of microglia neighboring these blood vessels and increased expression of MCP-1, has been observed in the dorsal anterior cingulate cortex (dACC) of postmortem tissue from patients with depression (MDD or bipolar disorder) who completed suicide (Steiner et al. 2011; Torres-Platas et al. 2014). These findings indicate that accumulation of peripheral immune cells in vascular compartments in association with restricted and/or regionally specific activation of microglia may be characteristic of patients with depression who exhibit elevated levels of inflammation.
T Cells and Cytokines Promote Cognition and Plasticity
A large body of work has found that CD4 T effector cells that traffic to the brain vasculature have beneficial effects on brain function by promoting tissue repair processes after injury, boosting cognitive function, reducing depressive or anxiety behaviors, and increasing neurogenesis (Derecki et al. 2010; Wolf et al. 2009; Schwartz and Shechter 2010; Lewitus et al. 2008). Relevant to depression and behavior, T cells traffic to the brain to reduce stress-induced anxiety-like behavior and reverse stress-induced decreases in brain-derived neurotrophic factor (BDNF), which is known to stimulate neurogenesis and possess antidepressant effects (Lewitus et al. 2008). T cells may also be required for normal cognitive function considering that T cell-deficient animals exhibit impaired learning and memory in water tests and mazes that can be reversed by the adoptive transfer of T cells (Kipnis et al. 2004; Ziv et al. 2006). T cells trafficking to the brain vasculature and meningeal space can produce IL-4 which stimulates astrocytes to produce growth factors including BDNF while also leading to the skewing of meningeal macrophages from a pro-inflammatory M1 phenotype to an anti-inflammatory, neuroprotective M2 phenotype (Derecki et al. 2010). A rich literature has also described the impact of a cytokines, including TNF and IL-1, on synaptic plasticity and learning and memory (del Rey et al. 2013). For example, mice depleted of the IL-1 type 1 receptor exhibit significant decreases in learning and memory and impaired long-term potentiation (LTP) (Yirmiya and Goshen 2011). Similar to IL-1, deletion of TNF receptors 1 and 2 has been associated with cognitive deficits (Naude et al. 2014), which may be due to their role in strengthening of excitatory synapses and plasticity by induction of surface expression of AMPA receptors (Stellwagen and Malenka 2006; Beattie et al. 2002) and stimulation of synaptic scaling (Stellwagen and Malenka 2006).
3.2 Neurobiological Mechanisms: Inflammation Effects on Circuits
A wealth of clinical and translational work has demonstrated that peripheral inflammation impacts brain regions relevant to both reward and threat sensitivity. PET and fMRI neuroimaging studies in humans have involved either the acute administration of inflammatory stimuli, such as endotoxin or vaccination, or chronic exposure to inflammatory cytokines, such as interferon [IFN]-α, as therapy for cancers and infectious diseases like hepatitis C virus (Capuron et al. 2007, 2012). Inflammation has consistently been found to affect both corticostriatal reward and motor circuits to drive reduced motivation and motor activity, as well as anxiety-related brain regions including the amygdala, insula, and ACC, which may result from cytokine effects on monoamines and glutamate (Fig. 1). Recent work has aimed to translate these findings to the investigation of relationships between increased inflammation and altered neurocircuits in patients with MDD.
Reward and Motor Circuits
Findings from numerous laboratories have consistently indicated that innate immune activation and the release of inflammatory cytokines preferentially affect reward and motor circuits and DA in the basal ganglia to contribute to reduced motivation and motor slowing (Capuron et al. 2007, 2012; Eisenberger et al. 2010; Harrison et al. 2015a; Felger and Miller 2012; Brydon et al. 2008; Majer et al. 2008; Goldsmith et al. 2016). Much of this work has stemmed from patients administered with IFN-α, up to 50% of whom met symptom criteria for major depression (depending on the dosing) and up to 80% of whom experienced significant fatigue, lack of energy, and motor slowing during treatment (Capuron et al. 2002a, b, 2003; Donnelly 1998; Musselman et al. 2001; Raison et al. 2005b, 2009, 2010a). Reduced motivation and anhedonia were also frequently reported in IFN-α-treated patients (Capuron et al. 2002a, 2012; Majer et al. 2008). Indeed, the Snaith-Hamilton Pleasure Scale (SHAPS) and the Reduced Motivation subscale of the Multidimensional Fatigue Inventory (MFI) yielded comparable effect sizes (all r = 0.47–0.49) for increases in self-reported depression or fatigue scores after chronic IFN-α treatment (Capuron et al. 2012; Majer et al. 2008). In IFN-α-treated patients, whole-brain analysis of fluorine-18-labeled fluorodeoxyglucose (FDG) PET found that, in addition to decreased metabolism in PFC, increased glucose metabolism was found in the basal ganglia and particularly the DA-rich putamen (Capuron et al. 2007; Juengling et al. 2000). Increased glucose metabolism in the left putamen and left nucleus accumbens (NAcc) correlated with fatigue in these patients, as assessed by the “energy” subscale of the Visual Analog Scale of Fatigue (VAS-F) (Capuron et al. 2007). This pattern of increased glucose metabolism in the basal ganglia is similar to that seen in Parkinson’s disease (PD) (Spetsieris et al. 1995; Eidelberg et al. 1994; Mentis et al. 2002), where it is thought to reflect increased oscillatory burst activity in relevant nuclei secondary to loss of inhibitory nigral DA input (Wichmann and DeLong 1999, 2003). Interestingly, this pattern of increased metabolism in the striatum is also similar to the effects of transient catecholamine depletion in patients with MDD, which correlated with anhedonic symptoms (Hasler et al. 2008). Functional magnetic resonance imaging (fMRI) has also demonstrated decreased neural activation in the basal ganglia, including ventral striatum, with unexpected delivery of reward (winning in a gambling task) (Reuter et al. 2005) in patients undergoing IFN-α administration, which correlated with reduced motivation (Capuron et al. 2012). Acute administration of IFN-α has also been shown to induce a change in striatal microstructure, as measured by quantitative magnetization transfer (qMT) imaging that predicted development of fatigue symptoms during treatment (Dowell et al. 2016).
Administration of the cytokine inducers endotoxin and typhoid vaccination to healthy volunteers produces similar effects on the ventral striatum in response to rewarding stimuli, suggesting that findings from IFN-α generalize to other inflammatory stimuli (Eisenberger et al. 2010; Harrison et al. 2015a). Indeed, endotoxin administration led to reduced activation of the ventral striatum to reward-predicting cues during a monetary incentive delay task (MIDT), which was associated with increases in self-reported depressed mood as measured by the Profile of Mood States (POMS) depression subscale (Eisenberger et al. 2010). Similar blunting of neural responses to reward anticipation has been observed following dietary depletion of precursors for DA synthesis (Bjork et al. 2014). Moreover, typhoid vaccination was found to cause a shift in reward versus punishment sensitivity in a probabilistic instrumental learning task combined with fMRI (Harrison et al. 2015a). Compared to saline control, typhoid vaccination reduced the behavioral attractiveness of rewards while making punishments more aversive, effects that were related to decreased neural activation of the ventral striatum to reward prediction errors and increased activation of the anterior insula to punishment prediction errors (Harrison et al. 2015a). Of relevance to the potential effects of inflammation on DA, the magnitude of response to prediction error signaling is fundamentally modulated by DA-dependent striatal activity as determined by the administration of drugs that enhance (l-DOPA) or inhibit (haloperidol) DAergic function (Pessiglione et al. 2006). Additionally, typhoid vaccination compared with saline has been shown to affect activity in the substantia nigra, including increased activation during a cognitive Stroop task and decreased activation in response to visual or novel stimuli, which correlated with both psychomotor slowing and increased peripheral blood concentrations of IL-6 (Brydon et al. 2008; Harrison et al. 2015b).
In medically stable patients with MDD, a relationship was observed between increased inflammation and decreased functional connectivity within reward-related corticostriatal neurocircuitry (Felger et al. 2016). Indeed, increased inflammation (plasma concentrations of CRP as well as cytokines and their soluble receptors) was associated with decreased functional connectivity between the ventral striatum and vmPFC and decreased connectivity between the dorsal striatum and the vmPFC and pre-supplementary motor area (pre-SMA), which correlated with self-reported symptoms of anhedonia and objective measures of psychomotor slowing, respectively (Felger et al. 2016). Interestingly, dorsal striatum and pre-SMA/SMA are key components of corticostriatal circuitry involved in linking motivation to motor output (Haber and Knutson 2010; Samanez-Larkin and Knutson 2015). Like the ventral striatum, vmPFC is part of the classic reward circuitry that receives significant mesocorticolimbic DA innervation (Russo and Nestler 2013; Diekhof et al. 2012).
Fear and Anxiety Circuits
A number of studies have examined the effects of inflammation on the activation of brain regions that contribute to fear, anxiety, and emotional processing, such as the amygdala, insula, or dorsal anterior cingulate cortex (dACC). In addition, other studies have examined changes in the function of circuitry involving these regions. Inflammation has been shown to not only increase amygdala activity but to also increase amygdala responsiveness to stress that drives increased production of inflammatory cytokines (Harrison et al. 2009a; Inagaki et al. 2012; Muscatell et al. 2015). Increased IL-6 and TNF after administration of endotoxin to healthy subjects has been shown to increase amygdala activity in response to socially threatening images, which was associated with enhanced feelings of social disconnection (Inagaki et al. 2012). Administration of typhoid vaccination, which increases IL-6 and induces behavioral changes including cognitive disturbances and fatigue, also increased activation of the amygdala during presentation of congruent and incongruent stimuli (Harrison et al. 2009b). In terms of stress sensitivity and neural pathways involved in the inflammatory response to stress, heightened neural activity in the amygdala in response to a psychosocial laboratory stressor was associated with greater stress-induced increases in IL-6 (Muscatell et al. 2015).
Several studies have also reported relationships between peripheral inflammatory cytokines and activity of medial prefrontal cortical regions, including the subgenual ACC, either in individuals undergoing stress or following administration of cytokine inducers (Harrison et al. 2009a; O’Connor et al. 2009c). Indeed, administration of typhoid vaccination to healthy controls induced mood changes that correlated with enhanced activity within the subgenual ACC during an implicit emotional face perception task. Typhoid vaccination also reduced task-related functional connectivity of the subgenual ACC to the amygdala and other medial prefrontal cortical regions, as well as the NAcc and superior temporal sulcus, which correlated with peripheral blood IL-6 (Harrison et al. 2009a). As mentioned above, heightened neural activity in the amygdala was associated with increased IL-6 responses to a psychosocial laboratory stressor. Functional connectivity analyses also indicated that individuals who showed a heightened inflammatory response to the stressor exhibited stronger coupling between the amygdala and the dorsomedial prefrontal cortex (Muscatell et al. 2015). In addition to activation of the amygdala, administration of typhoid vaccination increased activation of the insula during presentation of congruent and incongruent stimuli (Harrison et al. 2009b). Among females but not males administered endotoxin, increases in IL-6 were associated with increases in neural activity in brain regions including the anterior insula in response to social exclusion during a virtual ball-tossing game (Eisenberger et al. 2009). Endotoxin administration has also been shown to increase cerebral glucose metabolism in the insula as measured by PET (Hannestad et al. 2012b). Therefore, heightened sensitivity of the insula to inflammatory cytokines in the periphery, particularly in the presence of emotional stimuli, may contribute to altered neural circuitry involving the amygdala, medial prefrontal cortex, and ACC to precipitate symptoms of anxiety and emotional disturbance that contribute to MDD.
3.3 Neurobiological Mechanisms: Inflammation Effects on Neurotransmitters
Inflammation Effects on Monoamine Metabolism and Neurotransmission
Although most recent studies examining the effect of cytokines or inflammatory stimuli on monoamine release, tissue content, or turnover in animal studies have focused on DA, some studies have observed changes in the other monoamines, especially serotonin (5-HT). Acutely, monoamines are released in the hypothalamus and other limbic structures to mediate fever and early behavioral changes associated with sickness behavior (Dunn et al. 2005; O’Connor et al. 2009a). Administration of inflammatory cytokines also increase early 5-HT turnover in the cortex and NAcc (Song et al. 1999; De La Garza and Asnis 2003) in association with later, more persistent depressive-like behaviors (O’Connor et al. 2009a; Frenois et al. 2007). Additionally, both chronic administration of cytokines and chronic low-grade inflammation in humans have been shown to increase indoleamine-2,3-dioxygenase (IDO) activity and the metabolisms of tryptophan, the primary amino acid precursor of serotonin, to kynurenine (KYN) in the periphery (Capuron et al. 2003, 2011; Raison et al. 2010b). In patients treated with IFN-α for hepatitis C virus, CSF concentrations of IL-6 negatively correlated with 5-hydroxyindoleacetic acid (5-HIAA) concentrations, which in turn negatively correlated with IFN-α-induced depression severity (Raison et al. 2009). However, in a separate study, increased CSF KYN and QUIN concentrations were observed to correlate with depressive symptoms and with CSF cytokines, yet tryptophan concentrations were not decreased in the CSF despite decreased blood tryptophan concentrations (Raison et al. 2010b). These findings are consistent with recent work in rodents indicating that KYN administration alone was sufficient to induce depressive-like behavior and pharmacological inhibition of IDO with 1-methyl-tryptophan prevented lipopolysaccharide (LPS/endotoxin)-induced depressive-like behavior but did not prevent changes in 5-HT turnover (O’Connor et al. 2009a, b; Salazar et al. 2012). These findings suggest that neuroactive KYN metabolite effects on glutamate signaling are likely responsible for the behavioral changes associated with cytokine-induced IDO activity.
With regard to DA, some studies reported increases (Kumai et al. 2000; Sato et al. 2006), while others have reported decreases (Kamata et al. 2000; Kitagami et al. 2003; Shuto et al. 1997) in brain DA and/or metabolites following acute or sub-chronic IFN-α administration, which has been reviewed elsewhere (Felger and Miller 2012; Felger and Treadway 2017). These discrepancies were likely due to differences in dosing, length of exposure, and, most importantly, the fact that species-specific IFN-α was variably used and rodents do not respond to human IFN-α with activation of classic type I IFN receptor signaling (Loftis et al. 2006a, b; Wang et al. 2008). However, in monkeys chronically administered IFN-α, which causes similar behavioral responses as in humans, stimulated DA release was decreased in the striatum and correlated with reduced effort-based sucrose consumption (Felger et al. 2013a). Furthermore, IFN-α-induced decreases in striatal DA release were reversed by the DA precursor levodopa (l-DOPA) administered via reverse in vivo microdialysis (Felger et al. 2015). These findings were consistent with results from PET imaging with [F18]Fluorodopa in IFN-α-treated patients indicating that cytokines reduce DA synthesis and availability (Felger et al. 2015).
Indeed, inflammation and cytokines may decrease DA (and 5-HT) availability and release by decreasing tetrahydrobiopterin (BH4), an inflammation and oxidative stress-sensitive enzyme cofactor required for conversion of phenylalanine (Phe) to tyrosine (Tyr) by Phe hydroxylase and Tyr to l-DOPA by Tyr hydroxylase (as well as tryptophan to 5-HT) (Neurauter et al. 2008; Cunnington and Channon 2010). We and others have examined biomarkers of the DA synthetic pathway in IFN-α-treated patients, including the plasma Phe/Tyr ratio, which goes up when BH4 is low. We observed increased plasma Phe/Tyr and evidence of reduced cerebrospinal fluid (CSF) BH4 activity in IFN-α-treated patients (Kitagami et al. 2003; Felger et al. 2013b; Zoller et al. 2012), which correlated with decreased CSF DA and its major metabolite homovanillic acid (HVA) and with IFN-α-induced depressive symptoms (Felger et al. 2013b). Similarly, intramuscular injection of rats with IFN-α has been shown to decrease CNS concentrations of BH4 through inflammation-related stimulation of nitric oxide, whereas inhibition of nitric oxide synthase (which usurps BH4 during inflammation) was found to reverse IFN-α’s inhibitory effects on brain concentrations of both BH4 and DA (Kitagami et al. 2003). Moreover, in a study of healthy elderly persons with low-grade inflammation, peripheral blood concentrations of Phe and Tyr and an increased Phe/Tyr ratio were associated with neuropsychiatric symptoms including anhedonia and altered sleep (Capuron et al. 2011).
Finally, attention has been paid to the effects of cytokines and inflammatory signaling pathways on monoamine reuptake mechanisms and particularly the 5-HT transporter (Moron et al. 2003; Zhu et al. 2005, 2006, 2010). Both in vitro and in vivo data have established that stimulation of p38 mitogen-activated protein kinase (MAPK), a primary signaling pathway activated by IFN-α and other cytokines, can increase the expression and function of the serotonin transporter, leading to increased serotonin reuptake (Zhu et al. 2005, 2006, 2010). MAPK pathways have also been found to influence DAT. For example, DAT-expressing cells transfected with constitutively activate MAPK kinase (MEK) show increased DA reuptake (Vmax), whereas treatment of rat striatal synaptosomes with MEK inhibitors decreased DA reuptake in a concentration- and time-dependent manner (Moron et al. 2003). Therefore, reduced synaptic monoamines following chronic exposure to inflammatory cytokines may be mediated, in part, by increased transporter expression or function.
Inflammation Effects on Glutamate
Another mechanism by which cytokines may influence behavior is through stimulation of IDO and downstream KYN pathway metabolites on glutamate neurotransmission in the brain (Dantzer and Walker 2014; Dantzer et al. 2011). Immune-mediated activation of IDO catabolizes tryptophan, the primary amino acid precursor of serotonin, to KYN. KYN is further catabolized into the neuroactive metabolites kynurenic acid (KA) (in astrocytes) and quinolinic acid (QUIN) (in microglia), both of which have been found to be increased in the plasma and CSF of IFN-α-treated patients (Capuron et al. 2003; Raison et al. 2010b; Schwarcz and Pellicciari 2002; Bonaccorso et al. 2002). Of note, CSF QUIN significantly correlated with depressive symptoms during IFN-α administration, as measured by MADRS (Raison et al. 2010b). In addition to increasing oxidative stress (Santamaria et al. 2003; Behan et al. 1999), the neurotoxic metabolite QUIN can also directly activate the n-methyl-d-aspartate (NMDA) receptor to further induce the release of glutamate to lead to excitotoxicity in the brain (Schwarcz and Pellicciari 2002; Tavares et al. 2005). In contrast to QUIN, KA reduces glutamate release and has been shown to be an antagonist of NMDA and α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors (Stone 2000). DA release is in part under glutamatergic control, and thereby KA may exert downstream effects that further decrease DA to contribute to inflammation-induced depressive behavior (Schwarcz and Pellicciari 2002). Indeed, intrastriatal administration of KA to rodents leads to marked reductions in extracellular DA concentrations, as determined by in vivo microdialysis (Wu et al. 2007).
Finally, cytokines and inflammation have been shown to increase glutamate by effects on microglia and astrocytes (Haroon et al. 2017). A rich literature has shown that cytokines can decrease the astrocytic expression of glutamate transporters and increase release of glutamate from astrocytes and activated microglia in vitro (Dantzer and Walker 2014; Tilleux and Hermans 2007; Ida et al. 2008; Takaki et al. 2012). Of note, glutamate released from glia may have preferential access to extrasynaptic NMDA receptors, which lead to decreased production of trophic factors including brain-derived neurotrophic factor (BDNF) (Hardingham et al. 2002; Haydon and Carmignoto 2006). Increased glutamate, as measured by magnetic resonance spectroscopy (MRS), has been observed in patients chronically administered INF-α, which correlated with symptoms of reduced motivation and psychomotor slowing (Haroon et al. 2014, 2015). Likewise, increased glutamate was also observed in MDD patients with increased inflammation that correlated with anhedonia and psychomotor slowing (Haroon et al. 2016).
4 Potential Treatment Targets for Depressed Patients with Increased Inflammation
As described above, the neurobiological effects of inflammation on the brain, particularly via decreased monoamine synthesis and availability or increased reuptake, may circumvent or interfere with standard antidepressant therapies such as SSRIs. Therefore, there is a need to consider new therapies or a combination of treatments that reduce inflammation or that target its sources or consequences on the brain (Fig. 1). Indeed, the preferential effects of inflammation on DA and glutamate in reward and motor circuits and related behaviors indicate that patients with increased inflammation may respond better to DA- and glutamate-relevant therapies (Fig. 1). Reviewed below is current information regarding the clinical and/or translational use of relevant pharmacological strategies to reduce inflammation or its effects on the brain, as well as results from trials in MDD, if available (Table 1). Many potential new therapies exist, and results to date are encouraging; however additional studies using better trial design (i.e., targeting of therapies to patients with high inflammation) are warranted.
4.1 Therapies That Affect the Immune System
Anti-inflammatories
A number of recent studies have begun to test the potential of anti-inflammatory compounds as possible antidepressant therapies (Target 1, Fig. 1). Most studies to date have focused on compounds such as cyclooxygenase (COX)-2 inhibitors that block the production of prostaglandins, which are the primary downstream mediators of the inflammatory response that are increased in the peripheral blood of patients with depression (Lieb et al. 1983). Recent meta-analyses have reported modest effect sizes indicating a benefit of COX-2 inhibitors in reducing symptom severity. However, there was high heterogeneity across studies and mostly small sample sizes (Na et al. 2014; Kohler et al. 2014; Faridhosseini et al. 2014). Of the included studies, only a handful assessed the efficacy of nonsteroidal anti-inflammatories (NSAIDs) compared to placebo, whereas the majority used celecoxib or acetylsalicylic acid (aspirin) as adjuvants to conventional antidepressant therapies. Moreover, these studies did not select patients based on increased inflammation, and only a few measured peripheral inflammatory markers to establish the anti-inflammatory activity of the treatments. It should also be noted that these NSAID therapies convey relatively mild anti-inflammatory activity and numerous “off-target” effects that may confound data interpretation (Miller et al. 2017; Miller and Raison 2015).
More specific therapies inhibiting cytokine activity that are used to treat inflammatory illnesses have shown efficacy for reducing depressive symptoms in medically ill patients or in medically stable persons with MDD (Miller et al. 2017; Kohler et al. 2014). For example, a recent study tested the efficacy of infliximab, a highly selective TNF antagonist, in treatment-resistant patients with MDD as a function of peripheral inflammation. Treatment with infliximab was associated with robust decreases in plasma CRP concentrations, as well as a strong antidepressant effect, but only in patients with elevated CRP at baseline (Raison et al. 2013a). Moreover, the greatest area of symptom improvement was related to motivation (Raison et al. 2013a), which is consistent with the hypothesis that inflammation affects corticostriatal reward circuits as described elsewhere in this chapter. An ongoing clinical trial is examining the efficacy of infliximab in patients with bipolar depression and a CRP >5 mg/L (NCT02363738), and a Phase II trial of an anti-IL-6 mAb (sirukumab) is being run in patients with depression and a CRP >3 mg/L (NCT02473289).
Lastly, strategies aim to stimulate the production of IL-4-producing T cells, which has been accomplished in animal studies by administration of organisms such as helminths or cell therapies such as mesenchymal stem cells (MSCs), both of which have been shown to promote tolerant and anti-inflammatory responses. Helminths have been shown to stimulate IL-4 and regulatory “M2” macrophages in the gut via effects on the microbiome in a mouse model of inflammatory bowel disease (Ramanan et al. 2016). In an emerging field of immunomodulatory treatments involving stem cell therapies, MSCs have been shown to promote the development and differentiation of regulatory T cells and production of immunomodulatory and anti-inflammatory molecules such as TGF-beta, IL-10, and IL-1ra (Shi et al. 2011; Francois et al. 2012). Ongoing trials are testing the efficacy of MSC therapy in inflammatory and autoimmune disorders, and one study is examining the impact of a single infusion of allogeneic human MSCs for patients with treatment-resistant depression and increased inflammation (CRP >3 mg/L) (NCT02675556).
4.2 Compounds That Improve DA Synthesis, Availability, or Signaling
Considering the strong evidence presented above indicating that inflammation can inhibit key components of DA synthesis and availability, pharmacologic strategies that increase DA availability or signaling may effectively treat MDD in patients with high inflammation (Target 2, Fig. 1). Relevant pharmacologic agents include DA agonists, stimulants, bupropion, adenosine A2A receptor antagonists, and drugs that support DA synthesis through stimulation of BH4 activity. Such therapies that increase BH4 include saproterin and folic acid, l-methylfolate, and S-adenosylmethionine (SAMe) (Table 1), many of which help convert inactive BH2 to BH4. Of relevance to low BH4 activity in MDD, low serum folate has been associated with increased risk of depression as well as nonresponse to antidepressant treatment and an increased likelihood of depression relapse (Papakostas et al. 2004). Clinical trials have been conducted using l-methylfolate (marketed as Deplin and Zervalx) and SAMe in depression with mixed results (Papakostas et al. 2012; Sarris et al. 2015). Interestingly, however, a post hoc analysis of two parallel-sequential adjuvant trials of l-methylfolate in patients with MDD (Papakostas et al. 2012) was conducted while considering the influence of inflammatory markers. It was found that BMI >30 as well as increased concentrations of TNF, IL-8, CRP, and leptin over the median, alone or in combination with each other or with IL-6, predicted greater symptom improvement (Shelton et al. 2015). Stratified analyses based on inflammatory biomarkers have not been conducted with SAMe, yet these findings with l-methylfolate support the value of targeting such therapies to MDD patients with high inflammation. Furthermore, whether strategies that augment BH4 restore DA function or improve inflammation-related symptoms of reduced motivation or motor slowing remain to be determined. Replacement of DA with the precursor l-DOPA is known to improve motor function and has also been shown to increase motivation in patients with PD (Czernecki et al. 2002). An ongoing trial will determine whether l-DOPA administration has an antidepressant effect in aged persons with motor slowing (NCT02744391).
Although classical stimulant medications that increase DA release and/or block DA reuptake increase motivation in rodent models (Yohn et al. 2015; Randall et al. 2015), they have demonstrated only limited efficacy in chronically treating fatigue and other DA-related symptoms in trials for patients with cancer and other medical illnesses that are associated with inflammation (Mar Fan et al. 2008; Moraska et al. 2010; Butler et al. 2007; Sugawara et al. 2002; Pucci et al. 2007; Stankoff et al. 2005; Bruera et al. 2013; Ruddy et al. 2014; Escalante et al. 2014; Gong et al. 2014). Since stimulants act to increase DA release and block DAT function to increase synaptic levels of available DA, these drugs may not provide long-term efficacy in the context of inflammation during medical illness. However, new evidence indicates that in MDD patients with high inflammation (as measured by CRP) exhibit a greater antidepressant response to SSRIs used in combination with the DAT blocker bupropion compared to SSRI monotherapy (Jha et al. 2017). Although no data exists in humans, adenosine A2A receptor antagonists (which facilitate DA receptor signaling) reverse the effects of IL-1beta on effort-based sucrose preference (Nunes et al. 2014). Furthermore, DA agonists, such as pramipexole, have demonstrated efficacy in patients with treatment-resistant depression (Cassano et al. 2004; Cusin et al. 2013; Franco-Chaves et al. 2013). Although it is unknown whether this effect is specific to high inflammation in MDD patients, it has been shown to block endotoxin-induced degeneration of nigrostriatal DA cells in rodents (Iravani et al. 2008).
4.3 Therapies That Target Glutamate
Inhibition of glutamate signaling may be an important target in reversing the impact of inflammation in the brain (Target 2, Fig. 1). With regard to preventing activation of the KYN pathway, the IDO antagonist, 1-methyl-tryptophan (1-MT), has been shown to abrogate the impact of LPS, as well as an attenuated form of Mycobacterium bovis, on depressive-like behavior (O’Connor et al. 2009a, b). Given that inflammation can cause neurotoxic effects via increased QUIN and excessive glutamate (Schwarcz and Pellicciari 2002; Tavares et al. 2002, 2005), glutamate receptor antagonists may be useful in preventing excitotoxicity and oxidative stress and may reverse or prevent inflammation-related behavioral change. Indeed, one study in rodents demonstrated that the NMDA antagonist ketamine was able to reverse LPS-induced depressive-like behavior including sucrose preference, a measure of anhedonia (Walker et al. 2013). Ketamine had no effect on LPS-induced inflammation in the brain or CNS activation of IDO or decreases in BDNF expression. Moreover, blockade of AMPA receptors was able to reverse ketamine’s effects on LPS-induced depressive-like behavior, indicating that the effects of ketamine were specific to its impact on glutamate signaling. In humans, administration of the NMDA antagonist ketamine has potent antidepressant effects in MDD patients who are resistant to standard therapies and who often exhibit increased inflammation (aan het Rot et al. 2010; Price et al. 2009; Raison et al. 2013b). Interestingly, a recent study in treatment-resistant depression found that patients who were most responsive to ketamine were those with the highest concentrations of serum IL-6 (Yang et al. 2015). However, another study found that although treatment-resistant depressed patients exhibited increased IL-6 compared to controls, IL-6 and other inflammatory cytokines were not associated with treatment response to ketamine (Kiraly et al. 2017). There are also drugs available or in development that influence glutamate reuptake (e.g., riluzole); however there have been no studies examining their ability to reverse the effects of inflammation in patients with MDD. In sum, future therapies that block KYN pathways or modulate glutamate may confer protection against inflammation and/or IDO-mediated behavioral symptoms in patients with MDD.
4.4 Diet, Supplements, and Alternative Strategies
In terms of modifying the environmental exposures and lifestyle factors that contribute to inflammation in depression (Target 3, Fig. 1), studies have investigated the efficacy of exercise, weight reduction, certain diets, as well as supplements such as omega-3 fatty acids, yoga, massage, tai chi, cognitive behavioral therapy, and meditation to reduce psychiatric symptoms such as depression and anxiety. Many of these interventions have been shown to induce a variety of immune changes including a reduction in inflammation (Bower and Irwin 2016). For example, mindfulness meditation has been shown to increase functional connectivity between the posterior cingulate cortex and the left dorsolateral prefrontal cortex, which in turn was associated with decreases in IL-6 over a 4-month period (Creswell et al. 2016). In addition, both cognitive behavioral therapy and tai chi were associated with reduced levels of CRP, monocyte production of inflammatory cytokines, and inflammatory gene expression in elderly patients with insomnia (Irwin et al. 2015). Both diet and exercise programs have been shown to have antidepressant and antianxiety effects (Schuch et al. 2016; Fabricatore et al. 2011) and to reduce a variety of inflammatory markers in longitudinal studies (Forsythe et al. 2008; Woods et al. 2009). A hatha yoga program was also shown to reduce LPS-induced peripheral blood mononuclear cell production of TNF, IL-6, and IL-1beta as well as fatigue at 3 months in breast cancer survivors (Kiecolt-Glaser et al. 2014). These studies have, however, failed to determine whether changes in inflammation or immune function are required for the efficacy of these interventions (Miller et al. 2017).
The impact of the vast array of dietary supplements including curcumin, resveratrol, and ginger supplementation on the immune system and inflammation has been studied, yet the most common supplements studied in MDD patients involve omega-3 fatty acids. Meta-analyses have shown significant antidepressant efficacy especially for eicosapentaenoic acid (EPA) (Mocking et al. 2016). A recent study demonstrated that patients with a compilation of inflammatory markers including increased CRP and IL-1ra had a greater antidepressant response to EPA, whereas individuals with increased CRP and IL-6 were less responsive to placebo (Rapaport et al. 2016). Although there is some in vitro and in vivo data supporting anti-inflammatory effects of omega-3 fatty acids in humans (Rangel-Huerta et al. 2012), data linking these effects to their impact on behavior including depression is warranted. Therefore, an ongoing trial is currently investigating links between the antidepressant effects of omega-3 fatty acids and anti-inflammatory responses (NCT02553915). Antioxidant supplements such as N-acetyl-d-cysteine have also been included in meta-analyses of the antidepressant efficacy of anti-inflammatory drugs (Rosenblat et al. 2016), even though ability to specifically modulate inflammation has yet to be determined.
5 Summary and Conclusions
This chapter has presented evidence that inflammation is increased in a subset of patients with MDD and that it may play a role in depressive symptoms and influence response to antidepressants in these patients. In addition to observations regarding lack of response to conventional antidepressants in patients with increased peripheral blood markers of inflammation, such as CRP, a vast literature has described the effects that inflammation and cytokines have on neurotransmitters and circuits in the brain. These findings stem largely from over a decade of clinical and translational neuroimaging studies examining the effects of the acute and chronic administration of inflammatory stimuli on the brain. Results have indicated that inflammation affects brain regions relevant to reward, motor activity, and threat sensitivity to lead to symptoms of reduced motivation, motor slowing, and anxiety and these changes are largely driven by effects on monoamines, like DA, and glutamate. These findings are now being translated to better understand the role of inflammation in behavioral symptoms in patients with psychiatric illness and especially MDD.
The current data indicate that novel strategies to block inflammation or reverse its effects on the brain are promising, yet incomplete, and much additional work is needed in the area to move treatment development forward. More informed trials using drugs with known targets and selecting patients based on peripheral inflammation levels using markers such as CRP will contribute to progress in this regard. Another challenge in this area is the ability to image the effects of such treatments on the brain. Although attempts have been made to image local activation of CNS immune cells in these patients, evidence described herein of the functional and neurotransmitter effects of increased inflammation on the brain as measured by fMRI, PET, and MRS have most consistently been associated with increased peripheral inflammatory markers as well as behavior and may be best suited for use in future treatment trials. Coupling measures of target engagement in the brain – for both pharmacological and behavioral intervention studies – with outcome variables based on behaviors that are known to be impacted by inflammation (e.g., motivation, motor activity, or anxiety), will significantly strengthen the interpretation of future results. A number of trials that embrace at least some of these features are under way and may reveal additional information regarding novel therapies for patients with a wide variety of psychiatric disorders and evidence of increased inflammation.
References
aan het Rot M, Collins KA, Murrough JW et al (2010) Safety and efficacy of repeated-dose intravenous ketamine for treatment-resistant depression. Biol Psychiatry 67(2):139–145
Ahles TA, Saykin AJ, Furstenberg CT et al (2002) Neuropsychologic impact of standard-dose systemic chemotherapy in long-term survivors of breast cancer and lymphoma. J Clin Oncol 20(2):485–493
Au B, Smith KJ, Gariepy G, Schmitz N (2015) The longitudinal associations between C-reactive protein and depressive symptoms: evidence from the English Longitudinal Study of Ageing (ELSA). Int J Geriatr Psychiatry 30(9):976–984
Aziz N, Fahey JL, Detels R, Butch AW (2003) Analytical performance of a highly sensitive C-reactive protein-based immunoassay and the effects of laboratory variables on levels of protein in blood. Clin Diagn Lab Immunol 10(4):652–657
Banks WA, Erickson MA (2010) The blood-brain barrier and immune function and dysfunction. Neurobiol Dis 37(1):26–32
Banks WA, Kastin AJ, Broadwell RD (1995) Passage of cytokines across the blood-brain barrier. Neuroimmunomodulation 2(4):241–248
Banks WA, Farr SA, Morley JE (2002) Entry of blood-borne cytokines into the central nervous system: effects on cognitive processes. Neuroimmunomodulation 10(6):319–327
Beattie E, Stellwagen D, Morishita W et al (2002) Control of synaptic strength by glial TNFalpha. Science 295(5563):2282–2285
Behan WM, McDonald M, Darlington LG, Stone TW (1999) Oxidative stress as a mechanism for quinolinic acid-induced hippocampal damage: protection by melatonin and deprenyl. Br J Pharmacol 128(8):1754–1760
Berk M, Williams LJ, Jacka FN et al (2013) So depression is an inflammatory disease, but where does the inflammation come from? BMC Med 11:200
Bjork JM, Grant SJ, Chen G, Hommer DW (2014) Dietary tyrosine/phenylalanine depletion effects on behavioral and brain signatures of human motivational processing. Neuropsychopharmacology 39(3):595–604
Bluthe RM, Walter V, Parnet P et al (1994) Lipopolysaccharide induces sickness behaviour in rats by a vagal mediated mechanism. C R Acad Sci III 317(6):499–503
Bonaccorso S, Marino V, Puzella A et al (2002) Increased depressive ratings in patients with hepatitis C receiving interferon-alpha-based immunotherapy are related to interferon-alpha-induced changes in the serotonergic system. J Clin Psychopharmacol 22(1):86–90
Bosker FJ, Hartman CA, Nolte IM et al (2011) Poor replication of candidate genes for major depressive disorder using genome-wide association data. Mol Psychiatry 16(5):516–532
Bower JE, Irwin MR (2016) Mind-body therapies and control of inflammatory biology: a descriptive review. Brain Behav Immun 51:1–11
Bower JE, Ganz PA, Aziz N, Fahey JL (2002) Fatigue and proinflammatory cytokine activity in breast cancer survivors. Psychosom Med 64(4):604–611
Brambilla P, Bellani M, Isola M et al (2014) Increased M1/decreased M2 signature and signs of Th1/Th2 shift in chronic patients with bipolar disorder, but not in those with schizophrenia. Transl Psychiatry 4:e406
Bruera E, Yennurajalingam S, Palmer JL et al (2013) Methylphenidate and/or a nursing telephone intervention for fatigue in patients with advanced cancer: a randomized, placebo-controlled, phase II trial. J Clin Oncol 31(19):2421–2427
Brydon L, Harrison NA, Walker C, Steptoe A, Critchley HD (2008) Peripheral inflammation is associated with altered substantia nigra activity and psychomotor slowing in humans. Biol Psychiatry 63(11):1022–1029
Bufalino C, Hepgul N, Aguglia E, Pariante CM (2012) The role of immune genes in the association between depression and inflammation: a review of recent clinical studies. Brain Behav Immun 31:31–47
Butler JM Jr, Case LD, Atkins J et al (2007) A phase III, double-blind, placebo-controlled prospective randomized clinical trial of d-threo-methylphenidate HCl in brain tumor patients receiving radiation therapy. Int J Radiat Oncol Biol Phys 69(5):1496–1501
Cagnin A, Kassiou M, Meikle SR, Banati RB (2007) Positron emission tomography imaging of neuroinflammation. Neurotherapeutics 4(3):443–452
Capuron L, Gumnick JF, Musselman DL et al (2002a) Neurobehavioral effects of interferon-alpha in cancer patients: phenomenology and paroxetine responsiveness of symptom dimensions. Neuropsychopharmacology 26(5):643–652
Capuron L, Hauser P, Hinze-Selch D, Miller AH, Neveu PJ (2002b) Treatment of cytokine-induced depression. Brain Behav Immun 16(5):575–580
Capuron L, Neurauter G, Musselman DL et al (2003) Interferon-alpha-induced changes in tryptophan metabolism. Relationship to depression and paroxetine treatment. Biol Psychiatry 54(9):906–914
Capuron L, Pagnoni G, Demetrashvili MF et al (2007) Basal ganglia hypermetabolism and symptoms of fatigue during interferon-alpha therapy. Neuropsychopharmacology 32(11):2384–2392
Capuron L, Schroecksnadel S, Feart C et al (2011) Chronic low-grade inflammation in elderly persons is associated with altered tryptophan and tyrosine metabolism: role in neuropsychiatric symptoms. Biol Psychiatry 70:175–182
Capuron L, Pagnoni G, Drake DF et al (2012) Dopaminergic mechanisms of reduced basal ganglia responses to hedonic reward during interferon alfa administration. Arch Gen Psychiatry 69(10):1044–1053
Cassano P, Lattanzi L, Soldani F et al (2004) Pramipexole in treatment-resistant depression: an extended follow-up. Depress Anxiety 20(3):131–138
Cattaneo A, Gennarelli M, Uher R et al (2013) Candidate genes expression profile associated with antidepressants response in the GENDEP study: differentiating between baseline ‘predictors’ and longitudinal ‘targets’. Neuropsychopharmacology 38(3):377–385
Cattaneo A, Ferrari C, Uher R et al (2016) Absolute measurements of macrophage migration inhibitory factor and interleukin-1-beta mRNA levels accurately predict treatment response in depressed patients. Int J Neuropsychopharmacol 19(10):pyw045
Couzin-Frankel J (2010) Inflammation bares a dark side. Science 330(6011):1621
Coventry BJ, Ashdown ML, Quinn MA, Markovic SN, Yatomi-Clarke SL, Robinson AP (2009) CRP identifies homeostatic immune oscillations in cancer patients: a potential treatment targeting tool? J Transl Med 7:102
Creswell JD, Taren AA, Lindsay EK et al (2016) Alterations in resting-state functional connectivity link mindfulness meditation with reduced interleukin-6: a randomized controlled trial. Biol Psychiatry 80:53–61
Cunnington C, Channon KM (2010) Tetrahydrobiopterin: pleiotropic roles in cardiovascular pathophysiology. Heart 96(23):1872–1877
Cusin C, Iovieno N, Iosifescu DV et al (2013) A randomized, double-blind, placebo-controlled trial of pramipexole augmentation in treatment-resistant major depressive disorder. J Clin Psychiatry 74(7):e636–e641
Czernecki V, Pillon B, Houeto JL, Pochon JB, Levy R, Dubois B (2002) Motivation, reward, and Parkinson’s disease: influence of dopatherapy. Neuropsychologia 40(13):2257–2267
Danese A, Moffitt TE, Pariante CM, Ambler A, Poulton R, Caspi A (2008) Elevated inflammation levels in depressed adults with a history of childhood maltreatment. Arch Gen Psychiatry 65(4):409–415
Danese A, Caspi A, Williams B et al (2011) Biological embedding of stress through inflammation processes in childhood. Mol Psychiatry 16(3):244–246
Dantzer R, Walker AK (2014) Is there a role for glutamate-mediated excitotoxicity in inflammation-induced depression? J Neural Transm 121:925–932
Dantzer R, O’Connor JC, Lawson MA, Kelley KW (2011) Inflammation-associated depression: from serotonin to kynurenine. Psychoneuroendocrinology 36(3):426–436
De La Garza RI, Asnis GM (2003) The non-steroidal anti-inflammatory drug diclofenac sodium attenuates IFN-alpha induced alterations to monoamine turnover in prefrontal cortex and hippocampus. Brain Res 977(1):70–79
de La Serre CB, Ellis CL, Lee J, Hartman AL, Rutledge JC, Raybould HE (2010) Propensity to high-fat diet-induced obesity in rats is associated with changes in the gut microbiota and gut inflammation. Am J Physiol Gastrointest Liver Physiol 299(2):G440–G448
del Rey A, Balschun D, Wetzel W, Randolf A, Besedovsky HO (2013) A cytokine network involving brain-borne IL-1beta, IL-1ra, IL-18, IL-6, and TNFalpha operates during long-term potentiation and learning. Brain Behav Immun 33:15–23
Derecki NC, Cardani AN, Yang CH et al (2010) Regulation of learning and memory by meningeal immunity: a key role for IL-4. J Exp Med 207(5):1067–1080
Devaraj S, Yun JM, Duncan-Staley C, Jialal I (2009) C-reactive protein induces M-CSF release and macrophage proliferation. J Leukoc Biol 85(2):262–267
Diekhof EK, Kaps L, Falkai P, Gruber O (2012) The role of the human ventral striatum and the medial orbitofrontal cortex in the representation of reward magnitude – an activation likelihood estimation meta-analysis of neuroimaging studies of passive reward expectancy and outcome processing. Neuropsychologia 50(7):1252–1266
D’Mello C, Le T, Swain MG (2009) Cerebral microglia recruit monocytes into the brain in response to tumor necrosis factoralpha signaling during peripheral organ inflammation. J Neurosci 29(7):2089–2102
D’Mello C, Ronaghan N, Zaheer R et al (2015) Probiotics improve inflammation-associated sickness behavior by altering communication between the peripheral immune system and the brain. J Neurosci 35(30):10821–10830
Donnelly S (1998) Patient management strategies for interferon alfa-2b as adjuvant therapy of high-risk melanoma. Oncol Nurs Forum 25(5):921–927
Dowell NG, Cooper EA, Tibble J et al (2016) Acute changes in striatal microstructure predict the development of interferon-alpha induced fatigue. Biol Psychiatry 79(4):320–328
Dowlati Y, Herrmann N, Swardfager W et al (2010) A meta-analysis of cytokines in major depression. Biol Psychiatry 67(5):446–457
Drago A, Crisafulli C, Calabro M, Serretti A (2015) Enrichment pathway analysis. The inflammatory genetic background in bipolar disorder. J Affect Disord 179:88–94
Dunlop BW, Nemeroff CB (2007) The role of dopamine in the pathophysiology of depression. Arch Gen Psychiatry 64(3):327–337
Dunn AJ, Swiergiel AH, de Beaurepaire R (2005) Cytokines as mediators of depression: what can we learn from animal studies? Neurosci Biobehav Rev 29(4–5):891–909
Eidelberg D, Moeller JR, Dhawan V et al (1994) The metabolic topography of parkinsonism. J Cereb Blood Flow Metab 14(5):783–801
Eisenberger NI, Inagaki TK, Rameson LT, Mashal NM, Irwin MR (2009) An fMRI study of cytokine-induced depressed mood and social pain: the role of sex differences. NeuroImage 47(3):881–890
Eisenberger NI, Berkman ET, Inagaki TK, Rameson LT, Mashal NM, Irwin MR (2010) Inflammation-induced anhedonia: endotoxin reduces ventral striatum responses to reward. Biol Psychiatry 68(8):748–754
Ericsson A, Kovacs KJ, Sawchenko PE (1994) A functional anatomical analysis of central pathways subserving the effects of interleukin-1 on stress-related neuroendocrine neurons. J Neurosci 14(2):897–913
Escalante CP, Meyers C, Reuben JM et al (2014) A randomized, double-blind, 2-period, placebo-controlled crossover trial of a sustained-release methylphenidate in the treatment of fatigue in cancer patients. Cancer J 20(1):8–14
Evans DL, Staab JP, Petitto JM et al (1999) Depression in the medical setting: biopsychological interactions and treatment considerations. J Clin Psychiatry 60(Suppl 4):40–55, discussion 56
Fabricatore AN, Wadden TA, Higginbotham AJ et al (2011) Intentional weight loss and changes in symptoms of depression: a systematic review and meta-analysis. Int J Obes 35:1363–1376
Faridhosseini F, Sadeghi R, Farid L, Pourgholami M (2014) Celecoxib: a new augmentation strategy for depressive mood episodes. A systematic review and meta-analysis of randomized placebo-controlled trials. Hum Psychopharmacol 29(3):216–223
Felger JC, Miller AH (2012) Cytokine effects on the basal ganglia and dopamine function: the subcortical source of inflammatory malaise. Front Neuroendocrinol 33(3):315–327
Felger JC, Treadway MT (2017) Inflammation effects on motivation and motor activity: role of dopamine. Neuropsychopharmacology 42(1):216–241
Felger JC, Mun J, Kimmel HL et al (2013a) Chronic interferon-alpha decreases dopamine 2 receptor binding and striatal dopamine release in association with anhedonia-like behavior in nonhuman primates. Neuropsychopharmacology 38(11):2179–2187
Felger JC, Li L, Marvar PJ et al (2013b) Tyrosine metabolism during interferon-alpha administration: association with fatigue and CSF dopamine concentrations. Brain Behav Immun 31:153–160
Felger JC, Hernandez CR, Miller AH (2015) Levodopa reverses cytokine-induced reductions in striatal dopamine release. Int J Neuropsychopharmacol 18(4):pyu084
Felger JC, Li Z, Haroon E et al (2016) Inflammation is associated with decreased functional connectivity within corticostriatal reward circuitry in depression. Mol Psychiatry 21(10):1358–1365
Felger JC, Haroon E, Patel TA et al (2018) What does plasma CRP tell us about peripheral and central inflammation in depression? Mol Psychiatry
Fleshner M (2011) The gut microbiota: a new player in the innate immune stress response? Brain Behav Immun 25(3):395–396
Fleshner M (2013) Stress-evoked sterile inflammation, danger associated molecular patterns (DAMPs), microbial associated molecular patterns (MAMPs) and the inflammasome. Brain Behav Immun 27(1):1–7
Forsythe LK, Wallace JM, Livingstone MB (2008) Obesity and inflammation: the effects of weight loss. Nutr Res Rev 21(2):117–133
Franco-Chaves JA, Mateus CF, Luckenbaugh DA, Martinez PE, Mallinger AG, Zarate CA Jr (2013) Combining a dopamine agonist and selective serotonin reuptake inhibitor for the treatment of depression: a double-blind, randomized pilot study. J Affect Disord 149(1–3):319–325
Francois M, Romieu-Mourez R, Li M, Galipeau J (2012) Human MSC suppression correlates with cytokine induction of indoleamine 2,3-dioxygenase and bystander M2 macrophage differentiation. Mol Ther 20(1):187–195
Frenois F, Moreau M, O’Connor J et al (2007) Lipopolysaccharide induces delayed FosB/DeltaFosB immunostaining within the mouse extended amygdala, hippocampus and hypothalamus, that parallel the expression of depressive-like behavior. Psychoneuroendocrinology 32(5):516–531
Garver DL, Tamas RL, Holcomb JA (2003) Elevated interleukin-6 in the cerebrospinal fluid of a previously delineated schizophrenia subtype. Neuropsychopharmacology 28(8):1515–1520
Gimeno D, Kivimaki M, Brunner EJ et al (2009) Associations of C-reactive protein and interleukin-6 with cognitive symptoms of depression: 12-year follow-up of the Whitehall II study. Psychol Med 39(3):413–423
Goldsmith DR, Haroon E, Woolwine BJ et al (2016) Inflammatory markers are associated with decreased psychomotor speed in patients with major depressive disorder. Brain Behav Immun 56:281–288
Gong S, Sheng P, Jin H et al (2014) Effect of methylphenidate in patients with cancer-related fatigue: a systematic review and meta-analysis. PLoS One 9(1):e84391
Haapakoski R, Mathieu J, Ebmeier KP, Alenius H, Kivimaki M (2015) Cumulative meta-analysis of interleukins 6 and 1beta, tumour necrosis factor alpha and C-reactive protein in patients with major depressive disorder. Brain Behav Immun 49:206–215
Haber SN, Knutson B (2010) The reward circuit: linking primate anatomy and human imaging. Neuropsychopharmacology 35(1):4–26
Hannestad J, Gallezot JD, Schafbauer T et al (2012a) Endotoxin-induced systemic inflammation activates microglia: [11C]PBR28 positron emission tomography in nonhuman primates. NeuroImage 63(1):232–239
Hannestad J, Subramanyam K, Dellagioia N et al (2012b) Glucose metabolism in the insula and cingulate is affected by systemic inflammation in humans. J Nucl Med 53(4):601–607
Hardingham GE, Fukunaga Y, Bading H (2002) Extrasynaptic NMDARs oppose synaptic NMDARs by triggering CREB shut-off and cell death pathways. Nat Neurosci 5(5):405–414
Haroon E, Woolwine BJ, Chen X et al (2014) IFN-alpha-induced cortical and subcortical glutamate changes assessed by magnetic resonance spectroscopy. Neuropsychopharmacology 39(7):1777–1785
Haroon E, Felger JC, Woolwine BJ et al (2015) Age-related increases in basal ganglia glutamate are associated with TNF, reduced motivation and decreased psychomotor speed during IFN-alpha treatment: preliminary findings. Brain Behav Immun 46:17–22
Haroon E, Fleischer CC, Felger JC et al (2016) Conceptual convergence: increased inflammation is associated with increased basal ganglia glutamate in patients with major depression. Mol Psychiatry 21(10):1351–1357
Haroon E, Miller AH, Sanacora G (2017) Inflammation, glutamate, and glia: a trio of trouble in mood disorders. Neuropsychopharmacology 42(1):193–215
Harrison NA, Brydon L, Walker C, Gray MA, Steptoe A, Critchley HD (2009a) Inflammation causes mood changes through alterations in subgenual cingulate activity and mesolimbic connectivity. Biol Psychiatry 66(5):407–414
Harrison NA, Brydon L, Walker C et al (2009b) Neural origins of human sickness in interoceptive responses to inflammation. Biol Psychiatry 66(5):415–422
Harrison NA, Voon V, Cercignani M, Cooper EA, Pessiglione M, Critchley HD (2015a) A Neurocomputational account of how inflammation enhances sensitivity to punishments versus rewards. Biol Psychiatry 80:73–81
Harrison NA, Cercignani M, Voon V, Critchley HD (2015b) Effects of inflammation on hippocampus and substantia nigra responses to novelty in healthy human participants. Neuropsychopharmacology 40(4):831–838
Hasler G, Fromm S, Carlson PJ et al (2008) Neural response to catecholamine depletion in unmedicated subjects with major depressive disorder in remission and healthy subjects. Arch Gen Psychiatry 65(5):521–531
Haydon PG, Carmignoto G (2006) Astrocyte control of synaptic transmission and neurovascular coupling. Physiol Rev 86(3):1009–1031
Hodes GE, Pfau ML, Leboeuf M et al (2014) Individual differences in the peripheral immune system promote resilience versus susceptibility to social stress. Proc Natl Acad Sci U S A 111(45):16136–16141
Howren MB, Lamkin DM, Suls J (2009) Associations of depression with C-reactive protein, IL-1, and IL-6: a meta-analysis. Psychosom Med 71(2):171–186
Ida T, Hara M, Nakamura Y, Kozaki S, Tsunoda S, Ihara H (2008) Cytokine-induced enhancement of calcium-dependent glutamate release from astrocytes mediated by nitric oxide. Neurosci Lett 432(3):232–236
Imaizumi M, Kim HJ, Zoghbi SS et al (2007) PET imaging with [11C]PBR28 can localize and quantify upregulated peripheral benzodiazepine receptors associated with cerebral ischemia in rat. Neurosci Lett 411(3):200–205
Inagaki TK, Muscatell KA, Irwin MR, Cole SW, Eisenberger NI (2012) Inflammation selectively enhances amygdala activity to socially threatening images. NeuroImage 59(4):3222–3226
Iravani MM, Sadeghian M, Leung CC et al (2008) Continuous subcutaneous infusion of pramipexole protects against lipopolysaccharide-induced dopaminergic cell death without affecting the inflammatory response. Exp Neurol 212(2):522–531
Irwin MR, Olmstead R, Breen EC et al (2015) Cognitive behavioral therapy and tai chi reverse cellular and genomic markers of inflammation in late-life insomnia: a randomized controlled trial. Biol Psychiatry 78(10):721–729
Iwata M, Ota KT, Duman RS (2013) The inflammasome: pathways linking psychological stress, depression, and systemic illnesses. Brain Behav Immun 31:105–114
Jamal O, Aneni EC, Shaharyar S et al (2014) Cigarette smoking worsens systemic inflammation in persons with metabolic syndrome. Diabetol Metab Syndr 6:79–86
Jha MK, Minhajuddin A, Gadad BS et al (2017) Can C-reactive protein inform antidepressant medication selection in depressed outpatients? Findings from the CO-MED trial. Psychoneuroendocrinology 78:105–113
Juengling FD, Ebert D, Gut O et al (2000) Prefrontal cortical hypometabolism during low-dose interferon alpha treatment. Psychopharmacology 152(4):383–389
Kamata M, Higuchi H, Yoshimoto M, Yoshida K, Shimizu T (2000) Effect of single intracerebroventricular injection of alpha-interferon on monoamine concentrations in the rat brain. Eur Neuropsychopharmacol 10(2):129–132
Katsuura G, Arimura A, Koves K, Gottschall PE (1990) Involvement of organum vasculosum of lamina terminalis and preoptic area in interleukin 1 beta-induced ACTH release. Am J Phys 258(1 Pt 1):E163–E171
Khaodhiar L, Ling PR, Blackburn GL, Bistrian BR (2004) Serum levels of interleukin-6 and C-reactive protein correlate with body mass index across the broad range of obesity. JPEN J Parenter Enteral Nutr 28(6):410–415
Kiecolt-Glaser JK, Bennett JM, Andridge R et al (2014) Yoga’s impact on inflammation, mood, and fatigue in breast cancer survivors: a randomized controlled trial. J Clin Oncol 32(10):1040–1049
Kipnis J, Cohen H, Cardon M, Ziv Y, Schwartz M (2004) T cell deficiency leads to cognitive dysfunction: implications for therapeutic vaccination for schizophrenia and other psychiatric conditions. Proc Natl Acad Sci U S A 101(21):8180–8185
Kiraly DD, Horn SR, Van Dam NT et al (2017) Altered peripheral immune profiles in treatment-resistant depression: response to ketamine and prediction of treatment outcome. Transl Psychiatry 7(3):e1065
Kitagami T, Yamada K, Miura H, Hashimoto R, Nabeshima T, Ohta T (2003) Mechanism of systemically injected interferon-alpha impeding monoamine biosynthesis in rats: role of nitric oxide as a signal crossing the blood-brain barrier. Brain Res 978(1–2):104–114
Kohler O, Benros ME, Nordentoft M et al (2014) Effect of anti-inflammatory treatment on depression, depressive symptoms, and adverse effects: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiat 71(12):1381–1391
Kumai T, Tateishi T, Tanaka M, Watanabe M, Shimizu H, Kobayashi S (2000) Effect of interferon-alpha on tyrosine hydroxylase and catecholamine levels in the brain of rats. Life Sci 67(6):663–669
Levine J, Barak Y, Chengappa KN, Rapoport A, Rebey M, Barak V (1999) Cerebrospinal cytokine levels in patients with acute depression. Neuropsychobiology 40(4):171–176
Lewitus GM, Cohen H, Schwartz M (2008) Reducing post-traumatic anxiety by immunization. Brain Behav Immun 22(7):1108–1114
Lieb J, Karmali R, Horrobin D (1983) Elevated levels of prostaglandin E2 and thromboxane B2 in depression. Prostaglandins Leukot Med 10(4):361–367
Lim W, Hong S, Nelesen R, Dimsdale JE (2005) The association of obesity, cytokine levels, and depressive symptoms with diverse measures of fatigue in healthy subjects. Arch Intern Med 165(8):910–915
Lindqvist D, Janelidze S, Hagell P et al (2009) Interleukin-6 is elevated in the cerebrospinal fluid of suicide attempters and related to symptom severity. Biol Psychiatry 66(3):287–292
Loftis JM, Hauser P, Macey TA, Lowe JD (2006a) Can rodents be used to model interferon-alpha-induced depressive symptoms? Prog Neuro-Psychopharmacol Biol Psychiatry 30(7):1364–1365 author reply 1366
Loftis JM, Wall JM, Pagel RL, Hauser P (2006b) Administration of pegylated interferon-alpha-2a or -2b does not induce sickness behavior in Lewis rats. Psychoneuroendocrinology 31(10):1289–1294
Maes M (1999) Major depression and activation of the inflammatory response system. Adv Exp Med Biol 461:25–46
Maes M, Lambrechts J, Bosmans E et al (1992) Evidence for a systemic immune activation during depression: results of leukocyte enumeration by flow cytometry in conjunction with monoclonal antibody staining. Psychol Med 22(1):45–53
Maes M, Bosmans E, De Jongh R, Kenis G, Vandoolaeghe E, Neels H (1997) Increased serum IL-6 and IL-1 receptor antagonist concentrations in major depression and treatment resistant depression. Cytokine 9(11):853–858
Majer M, Welberg LA, Capuron L, Pagnoni G, Raison CL, Miller AH (2008) IFN-alpha-induced motor slowing is associated with increased depression and fatigue in patients with chronic hepatitis C. Brain Behav Immun 22(6):870–880
Mar Fan HG, Clemons M, Xu W et al (2008) A randomised, placebo-controlled, double-blind trial of the effects of d-methylphenidate on fatigue and cognitive dysfunction in women undergoing adjuvant chemotherapy for breast cancer. Support Care Cancer 16(6):577–583
Martinez JM, Garakani A, Yehuda R, Gorman JM (2012) Proinflammatory and “resiliency” proteins in the CSF of patients with major depression. Depress Anxiety 29(1):32–38
Maslanik T, Mahaffey L, Tannura K, Beninson L, Greenwood BN, Fleshner M (2012) The inflammasome and danger associated molecular patterns (DAMPs) are implicated in cytokine and chemokine responses following stressor exposure. Brain Behav Immun 28:54–62
Meier-Ewert HK, Ridker PM, Rifai N et al (2004) Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol 43(4):678–683
Mentis MJ, McIntosh AR, Perrine K et al (2002) Relationships among the metabolic patterns that correlate with mnemonic, visuospatial, and mood symptoms in Parkinson’s disease. Am J Psychiatry 159(5):746–754
Miller GE, Cole SW (2012) Clustering of depression and inflammation in adolescents previously exposed to childhood adversity. Biol Psychiatry 72(1):34–40
Miller AH, Raison CL (2015) Are anti-inflammatory therapies viable treatments for psychiatric disorders? Where the rubber meets the road. JAMA Psychiat 72(6):527–528
Miller AH, Ancoli-Israel S, Bower JE, Capuron L, Irwin MR (2008) Neuroendocrine-immune mechanisms of behavioral comorbidities in patients with cancer. J Clin Oncol 26(6):971–982
Miller AH, Haroon E, Felger JC (2017) Therapeutic implications of brain-immune interactions: treatment in translation. Neuropsychopharmacology 42(1):334–359
Mocking RJ, Harmsen I, Assies J, Koeter MW, Ruhe HG, Schene AH (2016) Meta-analysis and meta-regression of omega-3 polyunsaturated fatty acid supplementation for major depressive disorder. Transl Psychiatry 6:e756
Moraska AR, Sood A, Dakhil SR et al (2010) Phase III, randomized, double-blind, placebo-controlled study of long-acting methylphenidate for cancer-related fatigue: North Central Cancer Treatment Group NCCTG-N05C7 trial. J Clin Oncol 28(23):3673–3679
Moron JA, Zakharova I, Ferrer JV et al (2003) Mitogen-activated protein kinase regulates dopamine transporter surface expression and dopamine transport capacity. J Neurosci 23(24):8480–8488
Morrow GR, Hickok JT, Roscoe JA et al (2003) Differential effects of paroxetine on fatigue and depression: a randomized, double-blind trial from the University of Rochester Cancer Center Community Clinical Oncology Program. J Clin Oncol 21(24):4635–4641
Mostafavi S, Battle A, Zhu X et al (2014) Type I interferon signaling genes in recurrent major depression: increased expression detected by whole-blood RNA sequencing. Mol Psychiatry 19(12):1267–1274
Motivala SJ, Sarfatti A, Olmos L, Irwin MR (2005) Inflammatory markers and sleep disturbance in major depression. Psychosom Med 67(2):187–194
Muscatell KA, Dedovic K, Slavich GM et al (2015) Greater amygdala activity and dorsomedial prefrontal-amygdala coupling are associated with enhanced inflammatory responses to stress. Brain Behav Immun 43:46–53
Musselman DL, Lawson DH, Gumnick JF et al (2001) Paroxetine for the prevention of depression induced by high-dose interferon alfa. N Engl J Med 344(13):961–966
Na KS, Lee KJ, Lee JS, Cho YS, Jung HY (2014) Efficacy of adjunctive celecoxib treatment for patients with major depressive disorder: a meta-analysis. Prog Neuro-Psychopharmacol Biol Psychiatry 48:79–85
Naude PJ, Dobos N, van der Meer D et al (2014) Analysis of cognition, motor performance and anxiety in young and aged tumor necrosis factor alpha receptor 1 and 2 deficient mice. Behav Brain Res 258:43–51
Neurauter G, Schrocksnadel K, Scholl-Burgi S et al (2008) Chronic immune stimulation correlates with reduced phenylalanine turnover. Curr Drug Metab 9(7):622–627
Nierenberg AA (2015) Residual symptoms in depression: prevalence and impact. J Clin Psychiatry 76(11):e1480
Nunes EJ, Randall PA, Estrada A et al (2014) Effort-related motivational effects of the pro-inflammatory cytokine interleukin 1-beta: studies with the concurrent fixed ratio 5/chow feeding choice task. Psychopharmacology 231(4):727–736
O’Connor JC, Lawson MA, Andre C et al (2009a) Lipopolysaccharide-induced depressive-like behavior is mediated by indoleamine 2,3-dioxygenase activation in mice. Mol Psychiatry 14:511–522
O’Connor JC, Lawson MA, Andre C et al (2009b) Induction of IDO by bacille Calmette-Guerin is responsible for development of murine depressive-like behavior. J Immunol 182(5):3202–3212
O’Connor MF, Irwin MR, Wellisch DK (2009c) When grief heats up: pro-inflammatory cytokines predict regional brain activation. NeuroImage 47(3):891–896
Opp MR, Born J, Irwin MR (2007) Sleep and the immune system. In: Ader R (ed) Psychoneuroimmunology. Academic Press, New York, pp 570–618
Pace TW, Mletzko TC, Alagbe O et al (2006) Increased stress-induced inflammatory responses in male patients with major depression and increased early life stress. Am J Psychiatry 163(9):1630–1633
Pan W, Kastin AJ (2003) Interactions of cytokines with the blood-brain barrier: implications for feeding. Curr Pharm Des 9(10):827–831
Papakostas GI, Petersen T, Mischoulon D et al (2004) Serum folate, vitamin B12, and homocysteine in major depressive disorder, part 1: predictors of clinical response in fluoxetine-resistant depression. J Clin Psychiatry 65(8):1090–1095
Papakostas GI, Shelton RC, Zajecka JM et al (2012) L-methylfolate as adjunctive therapy for SSRI-resistant major depression: results of two randomized, double-blind, parallel-sequential trials. Am J Psychiatry 169(12):1267–1274
Park HS, Park JY, Yu R (2005) Relationship of obesity and visceral adiposity with serum concentrations of CRP, TNF-alpha and IL-6. Diabetes Res Clin Pract 69(1):29–35
Pessiglione M, Seymour B, Flandin G, Dolan RJ, Frith CD (2006) Dopamine-dependent prediction errors underpin reward-seeking behaviour in humans. Nature 442(7106):1042–1045
Pollak Y, Yirmiya R (2002) Cytokine-induced changes in mood and behaviour: implications for ‘depression due to a general medical condition’, immunotherapy and antidepressive treatment. Int J Neuropsychopharmacol 5(4):389–399
Price RB, Nock MK, Charney DS, Mathew SJ (2009) Effects of intravenous ketamine on explicit and implicit measures of suicidality in treatment-resistant depression. Biol Psychiatry 66(5):522–526
Pucci E, Branas P, D’Amico R, Giuliani G, Solari A, Taus C (2007) Amantadine for fatigue in multiple sclerosis. Cochrane Database Syst Rev 1:CD002818
Raison CL, Miller AH (2003) Depression in cancer: new developments regarding diagnosis and treatment. Biol Psychiatry 54(3):283–294
Raison CL, Miller AH (2013) The evolutionary significance of depression in pathogen host defense (PATHOS-D). Mol Psychiatry 18(1):15–37
Raison CL, Demetrashvili M, Capuron L, Miller AH (2005a) Neuropsychiatric adverse effects of interferon-alpha: recognition and management. CNS Drugs 19(2):105–123
Raison CL, Borisov AS, Broadwell SD et al (2005b) Depression during pegylated interferon-alpha plus ribavirin therapy: prevalence and prediction. J Clin Psychiatry 66(1):41–48
Raison CL, Borisov AS, Majer M et al (2009) Activation of central nervous system inflammatory pathways by interferon-alpha: relationship to monoamines and depression. Biol Psychiatry 65(4):296–303
Raison CL, Rye DB, Woolwine BJ et al (2010a) Chronic interferon-alpha administration disrupts sleep continuity and depth in patients with hepatitis C: association with fatigue, motor slowing, and increased evening cortisol. Biol Psychiatry 68(10):942–949
Raison CL, Dantzer R, Kelley KW et al (2010b) CSF concentrations of brain tryptophan and kynurenines during immune stimulation with IFN-alpha: relationship to CNS immune responses and depression. Mol Psychiatry 15(4):393–403
Raison CL, Rutherford RE, Woolwine BJ et al (2013a) A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression: the role of baseline inflammatory biomarkers. JAMA Psychiat 70(1):31–41
Raison CL, Felger JC, Miller AH (2013b) Inflammation and treatment resistance in major depression: a perfect storm. Psychiatric Times, 12 Sept
Ramanan D, Bowcutt R, Lee SC et al (2016) Helminth infection promotes colonization resistance via type 2 immunity. Science 352(6285):608–612
Randall PA, Lee CA, Podurgiel SJ et al (2015) Bupropion increases selection of high effort activity in rats tested on a progressive ratio/chow feeding choice procedure: implications for treatment of effort-related motivational symptoms. Int J Neuropsychopharmacol 18(2):pyu017
Rangel-Huerta OD, Aguilera CM, Mesa MD, Gil A (2012) Omega-3 long-chain polyunsaturated fatty acids supplementation on inflammatory biomakers: a systematic review of randomised clinical trials. Br J Nutr 107(Suppl 2):S159–S170
Rapaport MH, Nierenberg AA, Schettler PJ et al (2016) Inflammation as a predictive biomarker for response to omega-3 fatty acids in major depressive disorder: a proof-of-concept study. Mol Psychiatry 21(1):71–79
Reuter J, Raedler T, Rose M, Hand I, Glascher J, Buchel C (2005) Pathological gambling is linked to reduced activation of the mesolimbic reward system. Nat Neurosci 8(2):147–148
Rhodes B, Furnrohr BG, Vyse TJ (2011) C-reactive protein in rheumatology: biology and genetics. Nat Rev Rheumatol 7(5):282–289
Ridker PM (2003) Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation 107(3):363–369
Rosenblat JD, Kakar R, Berk M et al (2016) Anti-inflammatory agents in the treatment of bipolar depression: a systematic review and meta-analysis. Bipolar Disord 18(2):89–101
Ruddy KJ, Barton D, Loprinzi CL (2014) Laying to rest psychostimulants for cancer-related fatigue? J Clin Oncol 32(18):1865–1867
Rush AJ (2007) STAR*D: what have we learned? Am J Psychiatry 164(2):201–204
Russo SJ, Nestler EJ (2013) The brain reward circuitry in mood disorders. Nat Rev Neurosci 14(9):609–625
Salazar A, Gonzalez-Rivera BL, Redus L, Parrott JM, O’Connor JC (2012) Indoleamine 2,3-dioxygenase mediates anhedonia and anxiety-like behaviors caused by peripheral lipopolysaccharide immune challenge. Horm Behav 62(3):202–209
Samanez-Larkin GR, Knutson B (2015) Decision making in the ageing brain: changes in affective and motivational circuits. Nat Rev Neurosci 16(5):278–289
Sandiego CM, Gallezot JD, Pittman B et al (2015) Imaging robust microglial activation after lipopolysaccharide administration in humans with PET. Proc Natl Acad Sci U S A 112(40):12468–12473
Santamaria A, Flores-Escartin A, Martinez JC et al (2003) Copper blocks quinolinic acid neurotoxicity in rats: contribution of antioxidant systems. Free Radic Biol Med 35(4):418–427
Sarris J, Price LH, Carpenter LL et al (2015) Is S-adenosyl methionine (SAMe) for depression only effective in males? A re-analysis of data from a randomized clinical trial. Pharmacopsychiatry 48(4–5):141–144
Sato T, Suzuki E, Yokoyama M, Semba J, Watanabe S, Miyaoka H (2006) Chronic intraperitoneal injection of interferon-alpha reduces serotonin levels in various regions of rat brain, but does not change levels of serotonin transporter mRNA, nitrite or nitrate. Psychiatry Clin Neurosci 60(4):499–506
Schuch FB, Vancampfort D, Richards J, Rosenbaum S, Ward PB, Stubbs B (2016) Exercise as a treatment for depression: a meta-analysis adjusting for publication bias. J Psychiatr Res 77:42–51
Schwarcz R, Pellicciari R (2002) Manipulation of brain kynurenines: glial targets, neuronal effects, and clinical opportunities. J Pharmacol Exp Ther 303(1):1–10
Schwartz M, Shechter R (2010) Protective autoimmunity functions by intracranial immunosurveillance to support the mind: the missing link between health and disease. Mol Psychiatry 15(4):342–354
Schwieler L, Larsson MK, Skogh E et al (2015) Increased levels of IL-6 in the cerebrospinal fluid of patients with chronic schizophrenia – significance for activation of the kynurenine pathway. J Psychiatry Neurosci 40(2):126–133
Setiawan E, Wilson AA, Mizrahi R et al (2015) Role of translocator protein density, a marker of neuroinflammation, in the brain during major depressive episodes. JAMA Psychiat 72:268–275
Shelton RC, Miller AH (2010) Eating ourselves to death (and despair): the contribution of adiposity and inflammation to depression. Prog Neurobiol 91(4):275–299
Shelton RC, Claiborne J, Sidoryk-Wegrzynowicz M et al (2011) Altered expression of genes involved in inflammation and apoptosis in frontal cortex in major depression. Mol Psychiatry 16(7):751–762
Shelton RC, Pencina MJ, Barrentine LW et al (2015) Association of obesity and inflammatory marker levels on treatment outcome: results from a double-blind, randomized study of adjunctive L-methylfolate calcium in patients with MDD who are inadequate responders to SSRIs. J Clin Psychiatry 76(12):1635–1641
Shi M, Liu ZW, Wang FS (2011) Immunomodulatory properties and therapeutic application of mesenchymal stem cells. Clin Exp Immunol 164(1):1–8
Shuto H, Kataoka Y, Horikawa T, Fujihara N, Oishi R (1997) Repeated interferon-alpha administration inhibits dopaminergic neural activity in the mouse brain. Brain Res 747(2):348–351
Sluzewska A (1999) Indicators of immune activation in depressed patients. Adv Exp Med Biol 461:59–73
Soderlund J, Schroder J, Nordin C et al (2009) Activation of brain interleukin-1beta in schizophrenia. Mol Psychiatry 14(12):1069–1071
Soderlund J, Olsson SK, Samuelsson M et al (2011) Elevation of cerebrospinal fluid interleukin-1ss in bipolar disorder. J Psychiatry Neurosci 36(2):114–118
Song C, Merali Z, Anisman H (1999) Variations of nucleus accumbens dopamine and serotonin following systemic interleukin-1, interleukin-2, or interleukin-6 treatment. Neuroscience 88(3):823–836
Spetsieris PG, Moeller JR, Dhawan V, Ishikawa T, Eidelberg D (1995) Visualizing the evolution of abnormal metabolic networks in the brain using PET. Comput Med Imaging Graph 19(3):295–306
Stankoff B, Waubant E, Confavreux C et al (2005) Modafinil for fatigue in MS: a randomized placebo-controlled double-blind study. Neurology 64(7):1139–1143
Steiner J, Walter M, Gos T et al (2011) Severe depression is associated with increased microglial quinolinic acid in subregions of the anterior cingulate gyrus: evidence for an immune-modulated glutamatergic neurotransmission? J Neuroinflammation 8:94
Stellwagen D, Malenka RC (2006) Synaptic scaling mediated by glial TNF-alpha. Nature 440(7087):1054–1059
Stone TW (2000) Development and therapeutic potential of kynurenic acid and kynurenine derivatives for neuroprotection. Trends Pharmacol Sci 21(4):149–154
Strawbridge R, Arnone D, Danese A, Papadopoulos A, Herane Vives A, Cleare AJ (2015) Inflammation and clinical response to treatment in depression: a meta-analysis. Eur Neuropsychopharmacol 25(10):1532–1543
Suarez EC (2008) Self-reported symptoms of sleep disturbance and inflammation, coagulation, insulin resistance and psychosocial distress: evidence for gender disparity. Brain Behav Immun 22(6):960–968
Suganami T, Ogawa Y (2010) Adipose tissue macrophages: their role in adipose tissue remodeling. J Leukoc Biol 88(1):33–39
Sugawara Y, Akechi T, Shima Y et al (2002) Efficacy of methylphenidate for fatigue in advanced cancer patients: a preliminary study. Palliat Med 16(3):261–263
Takaki J, Fujimori K, Miura M, Suzuki T, Sekino Y, Sato K (2012) L-glutamate released from activated microglia downregulates astrocytic L-glutamate transporter expression in neuroinflammation: the ‘collusion’ hypothesis for increased extracellular L-glutamate concentration in neuroinflammation. J Neuroinflammation 9:275
Targum SD, Fava M (2011) Fatigue as a residual symptom of depression. Innov Clin Neurosci 8(10):40–43
Tavares RG, Tasca CI, Santos CES et al (2002) Quinolinic acid stimulates synaptosomal glutamate release and inhibits glutamate uptake into astrocytes. Neurochem Int 40(7):621–627
Tavares RG, Schmidt AP, Abud J, Tasca CI, Souza DO (2005) In vivo quinolinic acid increases synaptosomal glutamate release in rats: reversal by guanosine. Neurochem Res 30(4):439–444
Tilleux S, Hermans E (2007) Neuroinflammation and regulation of glial glutamate uptake in neurological disorders. J Neurosci Res 85(10):2059–2070
Torres-Platas SG, Cruceanu C, Chen GG, Turecki G, Mechawar N (2014) Evidence for increased microglial priming and macrophage recruitment in the dorsal anterior cingulate white matter of depressed suicides. Brain Behav Immun 42:50–59
Trivedi MH, Hollander E, Nutt D, Blier P (2008) Clinical evidence and potential neurobiological underpinnings of unresolved symptoms of depression. J Clin Psychiatry 69(2):246–258
Uher R, Tansey KE, Dew T et al (2014) An inflammatory biomarker as a differential predictor of outcome of depression treatment with escitalopram and nortriptyline. Am J Psychiatry 171:1278–1286
Venneti S, Lopresti BJ, Wang G et al (2007) A comparison of the high-affinity peripheral benzodiazepine receptor ligands DAA1106 and (R)-PK11195 in rat models of neuroinflammation: implications for PET imaging of microglial activation. J Neurochem 102(6):2118–2131
Vgontzas AN, Zoumakis E, Bixler EO et al (2004) Adverse effects of modest sleep restriction on sleepiness, performance, and inflammatory cytokines. J Clin Endocrinol Metab 89(5):2119–2126
Walker AK, Budac DP, Bisulco S et al (2013) NMDA receptor blockade by ketamine abrogates lipopolysaccharide-induced depressive-like behavior in C57BL/6J mice. Neuropsychopharmacology 38(9):1609–1616
Wang J, Campbell IL, Zhang H (2008) Systemic interferon-alpha regulates interferon-stimulated genes in the central nervous system. Mol Psychiatry 13(3):293–301
Watkins LR, Wiertelak EP, Goehler LE et al (1994) Neurocircuitry of illness-induced hyperalgesia. Brain Res 639(2):283–299
Watkins LR, Goehler LE, Relton JK et al (1995) Blockade of interleukin-1 induced hyperthermia by subdiaphragmatic vagotomy: evidence for vagal mediation of immune-brain communication. Neurosci Lett 183(1–2):27–31
Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW Jr (2003) Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest 112(12):1796–1808
Wichmann T, DeLong MR (1999) Oscillations in the basal ganglia. Nature 400(6745):621–622
Wichmann T, DeLong MR (2003) Functional neuroanatomy of the basal ganglia in Parkinson’s disease. Adv Neurol 91:9–18
Wilson AA, Garcia A, Parkes J et al (2008) Radiosynthesis and initial evaluation of [18 F]-FEPPA for PET imaging of peripheral benzodiazepine receptors. Nucl Med Biol 35(3):305–314
Wium-Andersen MK, Orsted DD, Nielsen SF, Nordestgaard BG (2013) Elevated C-reactive protein levels, psychological distress, and depression in 73, 131 individuals. JAMA Psychiat 70(2):176–184
Wohleb ES, Fenn AM, Pacenta AM, Powell ND, Sheridan JF, Godbout JP (2012) Peripheral innate immune challenge exaggerated microglia activation, increased the number of inflammatory CNS macrophages, and prolonged social withdrawal in socially defeated mice. Psychoneuroendocrinology 37(9):1491–1505
Wohleb ES, McKim DB, Shea DT et al (2014) Re-establishment of anxiety in stress-sensitized mice is caused by monocyte trafficking from the spleen to the brain. Biol Psychiatry 75(12):970–981
Wolf SA, Steiner B, Akpinarli A et al (2009) CD4-positive T lymphocytes provide a neuroimmunological link in the control of adult hippocampal neurogenesis. J Immunol 182(7):3979–3984
Wong ML, Inserra A, Lewis MD et al (2016) Inflammasome signaling affects anxiety- and depressive-like behavior and gut microbiome composition. Mol Psychiatry 21:797–805
Woods JA, Vieira VJ, Keylock KT (2009) Exercise, inflammation, and innate immunity. Immunol Allergy Clin N Am 29(2):381–393
Wu HQ, Rassoulpour A, Schwarcz R (2007) Kynurenic acid leads, dopamine follows: a new case of volume transmission in the brain? J Neural Transm 114(1):33–41
Yang JJ, Wang N, Yang C, Shi JY, Yu HY, Hashimoto K (2015) Serum interleukin-6 is a predictive biomarker for ketamine’s antidepressant effect in treatment-resistant patients with major depression. Biol Psychiatry 77(3):e19–e20
Yirmiya R, Goshen I (2011) Immune modulation of learning, memory, neural plasticity and neurogenesis. Brain Behav Immun 25(2):181–213
Yirmiya R, Weidenfeld J, Pollak Y et al (1999) Cytokines, “depression due to a general medical condition,” and antidepressant drugs. Adv Exp Med Biol 461:283–316
Yirmiya R, Pollak Y, Morag M et al (2000) Illness, cytokines, and depression. Ann N Y Acad Sci 917:478–487
Yohn SE, Thompson C, Randall PA et al (2015) The VMAT-2 inhibitor tetrabenazine alters effort-related decision making as measured by the T-maze barrier choice task: reversal with the adenosine A2A antagonist MSX-3 and the catecholamine uptake blocker bupropion. Psychopharmacology 232(7):1313–1323
Zhu CB, Carneiro AM, Dostmann WR, Hewlett WA, Blakely RD (2005) p38 MAPK activation elevates serotonin transport activity via a trafficking-independent, protein phosphatase 2A-dependent process. J Biol Chem 280(16):15649–15658
Zhu CB, Blakely RD, Hewlett WA (2006) The proinflammatory cytokines interleukin-1beta and tumor necrosis factor-alpha activate serotonin transporters. Neuropsychopharmacology 31(10):2121–2131
Zhu CB, Lindler KM, Owens AW, Daws LC, Blakely RD, Hewlett WA (2010) Interleukin-1 receptor activation by systemic lipopolysaccharide induces behavioral despair linked to MAPK regulation of CNS serotonin transporters. Neuropsychopharmacology 35:2510–2520
Ziv Y, Ron N, Butovsky O et al (2006) Immune cells contribute to the maintenance of neurogenesis and spatial learning abilities in adulthood. Nat Neurosci 9(2):268–275
Zoller H, Schloegl A, Schroecksnadel S, Vogel W, Fuchs D (2012) Interferon-alpha therapy in patients with hepatitis C virus infection increases plasma phenylalanine and the phenylalanine to tyrosine ratio. J Interf Cytokine Res 32(5):216–220
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Felger, J.C. (2018). Role of Inflammation in Depression and Treatment Implications. In: Macaluso, M., Preskorn, S. (eds) Antidepressants. Handbook of Experimental Pharmacology, vol 250. Springer, Cham. https://doi.org/10.1007/164_2018_166
Download citation
DOI: https://doi.org/10.1007/164_2018_166
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-10948-6
Online ISBN: 978-3-030-10949-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)