Abstract
In this chapter we introduce the relevance of CAP for infection treatment and the role of this new tool in the management of multiresistant pathogens. Cap can be used for decolonization of patients e.g. with multiresistant Staphylococci (MRSA), enterococci (VRE) and gramnegative rods like ESBL-coli therewith demonstrating a role beside conventional antiseptics. It can be shown how CAP efficacy is related to the pathogen’s drug susceptibility and depends on gram stain behavior. Additionally, despite principal suitability killing all kind of tested pathogens that can be found in patients so far, clear differences in CAP efficacy towards different species can be elucidated and also significantly depending on the device type. To compare CAP devices testing susceptibility of a set of important pathogens is recommended, comparing also time and distance for successful treatment in vitro. The different test options are discussed in comparison with conventional drug susceptibility test methods (agar diffusion, bouillon dilution). Options and limitations of CAP application are presented to understand what we can await from practical use and where conventional treatment still is justified.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Summary
Cold plasma is now available since a lot of years and since approval apart from a multitude of in vitro experiments many patients have undergone plasma therapy. Actually tumor and antimicrobial skin and wound treatment seem the most attractive treatment options with an urgent need for alternative therapies. This is also valid for recalcitrant ulcer wounds , whereby actually no valid multicenter studies but promising observations with good results of plasma therapy are available. Before general recommendations are to be made regarding use of “plasma antisepsis ” and treatment of recalcitrant wounds evidence based studies must show the clinical suitability of the intervention. Own studies show excellent results of plasma in the treatment of nosocomial pathogens on skin and wounds as well as of dermal precancerosis . It must be emphasized to ever keep sight of ethical aspects of any use of new methods in medicine: Less marketing and more serious results of valid tolerability as well as efficacy studies should persuade the doctor in practice to assume responsibility for his patients and to let. This will be a mutual benefit for patients and public health as well.
2 Introduction
The new medical field plasma medicine is celebrating its decennial birthday [1, 2].
Beside multiple applications in technology and biology cold and plasmas are worldwide under investigation to create innovative applications.
This is possible since already known “hot” plasma could be domesticated to skin tolerated treatments.
On the other hand “cold” plasmas were already sold about 100 years ago in USA and Europe as high-frequency therapy and at the moment still two companies offer “high-frequency” related plasma devices in Germany. The antimicrobial activity was one of the mostly claimed properties of these devices, and meanwhile could be approved in vitro for important pathogens of bacteria, fungi, viruses and parasites [3]. Even the background being not fully understood, it can be assumed that this activity of the plasma is responsible for the effectiveness of most clinical applications, except antitumor efficacy, which currently is under vigorous investigation.
3 Why Plasma
Physical treatments to defeat microbial challenges have a long-standing tradition and many medical applications focus on broad antimicrobial activity by distance. However up to date no device with pure physical antimicrobial efficacy has entered medical business and potential treatments with potent antimicrobial properties like UV photons are to be dropped out because of safety reasons.
In contrast to all kind of physical skin and wound treatments up to day in use now cold plasma offers a wide spectrum of effective species with potent antimicrobial properties allowing disinfection of skin and wounds.
CAP effects include
-
reactive oxidative and nitrogen species (ROS and RNS),
-
free radicals,
-
ions,
-
electric fields,
-
electrons
These species justify antimicrobial applications of CAP inducing bacteriocidic effects based upon membrane oxidation, cell wall and DNA disintegration [6]. In comparison with other means like UV radiation the “cocktail” offered by CAP can be realized with far less energy dosage which enables safer clinical applicability. Not any of the mentioned reactive species alone could be applied without the danger of harmful skin effects because the need for much higher doses.
4 Worldwide Problems with Multi Drug Resistance
The actual situation regarding multi drug resistance is far from being desirable.
Despite some efforts fighting MRSA , these bugs still represent a relevant challenge up to day and in the US ambulant variants CA-MRSA (community-acquired) meanwhile have supplanted hospital-acquired MRSA (HA-MRSA) as first pathogen in patients with wound infections [7].
Coincident with worldwide decreasing MRSA incidence now another group of multi drug resistant pathogens, the MRGN (multi drug resistant gramnegative rods , mostly enterobacteriaceae ) have entered the stage and pose significant problems in intensive care units [8].
Additionally regarding new antibiotic development the situation seems not optimistic. In parallel to lacking approvals of new therapeutics decreasing investments for antibiotic research can be noticed.
A way out could be realized by CAP, because its antimicrobial properties rely on completely different mechanisms compared with any conventional antimicrobial chemotherapeutic.
Therefore a benefit using CAP in the fight against multi drug resistance can be assumed, i.e. treating wound infections caused by MDR bugs but also decolonizing colonized skin in the hospital. Although full susceptibility of pathogens to CAP can be expected and was supported by first experiments we now can differentiate some distinct variations between species, which are further discussed in Chaps. 6.9–6.11.
5 Not Only Bacteria To Be Focused
Apart from bacteria many more microorganisms causing infections worldwide still pose substantial problems, thereof among others atypical mycobacteria , fungi (yeasts and also molds), chlamydia , mycoplasma and viruses like hepatitis virus and some parasites such as toxoplasma gondii, leishmania spp. and entamoeba histolyticum. A special case are cryptosporidia , which can cause important gastrointestinal diseases exhibiting important resistance towards disinfectants in the environment. Against Leishmania Fridman et al. could demonstrate CAP efficacy [9], our group was able to show potent CAP-efficacy against Demodex folliculorum [10]. In contrast to antibacterial efficacy with multidrug resistance as main problem, the problem with parasites means to find at all effective treatments with good tolerability.
6 Antimicrobial Applications
For CAP as for any other new treatment option a clear indication based upon evidence of efficacy is recommended and for clinical practice the treatment of choice is this one with best efficacy together with best tolerability. When both treatments fulfill these recommendations the product with best price will be advised.
Therefore before a treatment is planned alternatives and potential adverse effects and costs have to be weighted prior to use. As an example it makes no sense to use CAP as a disinfectant on surfaces where simple ethanol based disinfectants make the same job over 30 s exposure. CAP applications seem meaningful when conventional procedures are not (fully) successful, i.e. MRSA sanitization on human skin in case of recalcitrant colonization. Another purpose is CAP application for wound healing after successful elimination of those factors which were responsible for impaired healing capacity like chronic venous insufficiency or bacterial biofilms. At the moment CAP is clinically mainly used to improve healing in patients with chronic wounds.
7 Less Antimicrobial Susceptibility Under Cap-Treatment?
Since antimicrobial CAP activity is not related to the mechanisms described for chemotherapeutic drugs it can be assumed that the feared selection of resistant strains which are propagated throughout the world may be omitted. The mode of action by CAP which can be compared most likely with antiseptics and disinfectants is based upon biophysical attack together with strong oxidation and follows an overkill model. Only at low concentrations disinfectants do not work and allow survival of pahogens thus promoting spread situations in hospitals. At right concentrations not one cell can survive providing high confidence in routine disinfection procedures. This is the only condition highly recommended during CAP use treating i.e. biofilms and the lack of resistance development now is referenced by several groups. However, since up to day no standardized method for susceptibiity testing of CAP is available, implementation of such a test model and larger studies with species and strains from different regions are strongly warranted.
8 Susceptibility Testing of CAP In Vitro
Over decades standard tests exist to evaluate susceptibility of bacteria towards antibiotics with different methods following national and international proceeding guidelines. Over years microbouillon dilution methods were developed to gold standard in susceptibility testing resulting in minimal inhibitory concentrations (MIC) , which are tested as break point values in routine testing. This test procedure has replaced the former used agar diffusion method (Agardiffusionstest nach Bauer und Kirby; [11]) which is much easier to perform but provides values that cannot be related to therapeutic serum levels as MIC. Nevertheless agar diffusion still is used for special questions like ESBL-testing and as orientating test for some difficult to test organisms. Both test methods refer on stringently chosen drug but also pathogen concentrations in suspensions. For MIC testing geometric dilutions of drugs are incubated with stable pathogen suspensions and resulting growth quantified after turbidimetric measurement in microvials. Our group has undertaken MIC testing of CAP in microtiterplates by adapting standard methods, resulting in doses by which complete killing of a known pathogen is achieved. This method seems valid but needs copious validation. The main problem is standardisation with exposure times of half a second changing significantly test results which causes larger experimental effort to gain stable data. Therefore most experimentators experience modifications of Bauer and Kirby’s agar diffusion method which is much easier to perform. It has to be mentioned that both methods were worked out for solids but per se not for radiation testing and (see above) up to we still have no standard test for CAP susceptibility testing. Even when CAP is assumed as working by oxidizing species, the complexity of such mode of action (chemical reactions cannot be reduced to a simple calculable value) causes the described difficulties resulting from MIC testing in suspensions [12].
When CAP was tested on agar, we could show that CAP efficacy rapidly decreased with increasing concentrations but also with maturity of colonies, a phenomenon which may be related to physical density (“shadow effect”) [12]. This has to be mentioned for better understanding and estimation of CAP effects in complex situations (biofilms, wound secretions) and underline the importance to correlate inhibition zones to clinical outcome in larger studies.
Up to now a multitude of species was tested against CAP including all kind of clinical relevant pathogens causing acute and chronic skin and wound infections and septcemia. With the important restriction that we can conclude that by no author CAP resistant strains or species were recorded (means no inhibition zone obtained after 1–60 s on solid media like agar) [13, 14]. Our group tested some thousands of strains and neither with the most in use CAP device, the Argon fed kINPen (INP Greifswald, Germany) nor different DBD (i.e. CINOGY, Duderstadt, Germany, TEFRA, Berlin, Germany, PMS, Bad Ems, Germany) showed resistant strains.
The lack of resistant strains does not mean that all strains show identic inhibition zones or MICs. We found significant and not significant differences between gram positive and negative species and also between strains with different susceptibility towards chemotherapeutic drugs. I.e. for some enterococci and also S. aureus the degree of drug resistance determined the susceptibility towards CAP, in detail VRE and HLGR were less susceptible to CAP (for more details see also the following chapters) [12].
Other authors published less CAP susceptibility of spore forming bacteria [15], what was explained by the envelope lacking water.
Also Lee et al. found differences in susceptibility between gram positive and gram negative bacteria with gram negative bacteria exhibiting better susceptibility to CAP [16], other authors could not verify these differences [17]. Our group found that the described differences depend on the CAP technique, with Argon fed jets we found no significant differences, but using DBD we did (see above, [18]).
9 Technique of CAP Treatment
Our group in Greifswald uses the following CAP devices
-
APPJ, gepulsed and non-pulsed Modus (kINPen Med, INP Greifswald, Germany),
-
DBD (PlasmaDerm®, CINOGY, Duderstadt, Germany)
-
DBD with glass electrode (plasma MEDICAL SYSTEMS, Bad Ems, Germany),
-
DBD with glass electrode (TEFRA, Berlin, Germany)
-
Argonplasma-Jet (Maxium®-Beamer, KLS Martin, Tuttlingen, Germany)
The above mentioned CAP devices produced very similar antimicrobial efficacy as tested on semisolid media in vitro against all up to now tested clinical strains and species independently of the chemotherapeutic drug susceptibility and after 3–60 s of treatment in vitro [10, 18, 19]. Albeit principally susceptibility, some important differences could be noted [12, 18].
Except most relevant clinical bacterial species also clinical relevant fungi and molds were tested against CAP. As examples with excellent susceptibility to CAP here Trichophyton (interdigitale zoophil and anthropophil, rubrum and verrucosum), Microsporum canis, Candida (albicans, glabrata and krusei), Penicillium and Aspergillus should be mentioned.
In representative in vitro study we investigated the dependence of the degree of multi drug resistance of a strain on the susceptibility to CAP and tested 194 multi drug resistant wound isolates against two CAP sources (DBD and pulsed and non-pulsed Argon fed jet).The following 13 species were tested:
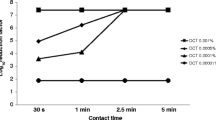
Escherichia coli, Pseudomonas aeruginosa, Extended spectrum beta-lactamase builder (ESBL) , Staphylococcus epidermidis, Staphylococcus aureus (Methicillin-susceptible, MSSA, Methicillin-resistant, MRSA, Methicillin-resistant Staphylococcus epidermidis, MRSE, Acinetobacter spp., Klebsiella group (Klebsiella pneumoniae ssp. pneumoniae, Klebsiella oxytoca), Enterococcus faecalis, Enterococcus faecium, Vancomycin resistant enterococci VRE and High level gentamycin resistant enterococci HLGR [19]. In general we could show that the pulsed jet was less effective than the non-pulsed variant (p < 0.001) when the inhibition zones on growth agar were compared showing larger zones with the non pulsed jet and best susceptibility of the Gram negative species P. aeruginosa (Figs. 6.1 and 6.2)Additionally we found gram positive species significantly more susceptible to DBD plasma than gram negative species (p < 0.001) (Fig. 6.1). Jet plasma showed another pattern with best susceptibility of the gram negative P. aeruginosa followed by the gram positive S.aureus (MSSA) for both sources (Fig. 6. 2 and 6.3). Interestingly with increasing multi drug resistance (number of classes of antibiotics showing resistance as obtained by conventional susceptibility testing) of a species, susceptibility to CAP decreased when DBD and increased when jets were used (Fig. 6.4 and 6.5) underlining the potential suitability of CAP (DBD) in case of multi drug resistant bacteria bacteria in wounds or elsewhere.
Increasing antimicrobial resistance against antibiotics (number of classes of antibiotics to which a species showed resistance, x axis) an related inhibition zones (y axis) obtained after 3 s of DBD plasma treatment and trendline (calculated via method of least squares). CAP susceptibility increased with degree of multi drug resistance
Increasing antimicrobial resistance against antibiotics (number of classes of antibiotics to which a species showed resistance, x axis) and related inhibition zones (y axis) obtained after 3 s of jet plasma (non pulsed and pulsed) treatment and trendline (calculated via method of least squares). CAP susceptibility decreased with degree of multi drug resistance
Additionally we found that gras were significantly more susceptible than gram positive ones, regardless the CAP jet source used (p < 0.001) (Fig. 6.2) and when DBD was compared with the jets, gram positive species showed more susceptibility to the DBD (p < 0.001) (Figs. 6.1, 6.2 and 6.3).
10 Efficacy Against MRSA In Vitro
Several authors report different CAP susceptibility of MRSA and MSSA in vitro testing some strains and species. In a larger collective of clinically defined strains we investigated 50 MRSA (48 HA-MRSA, 1 LA-MRSA, 1 CA-MRSA) and 168 MSSA [20]. Both bacterial groups MRSA and MSSA showed good susceptibility to CAP (all three sources) but some important differences could be noted. The DBD was the CAP source with the largest electrode surface and showed the largest inhibition zones, however the activity against MRSA was less pronounced in comparison with the jets, what cannot be explained up to now. One explanation could be the thicker cell wall of some strains of MRSA as described by Kawai et al. [21].
11 Efficacy Against Enterococci In Vitro
Having demonstrated important differences between Staphylococci we intended to investigate also the group of clinically most relevant gram positive cocci, the enterococci.
We further would correlate the influence of conventional drug susceptibility of these bacteria on CAP susceptibility.
As for MRSA and MSSA we could demonstrate different susceptibility to the CAP device in the tests. All tested 39 isolates (including VRE, HLGR) showed 100% susceptibility to any of the three CAP devices but with DBD the anti enterococcal efficacy against the more resistant strains was less strong compared with both jets [12]. In detail using DBD Vancomycin-resistant enterocci (VRE) were significantly more resistant than all other enterococci. Also HLGR-isolates showed significantly smaller inhibition areas than other enterococci when treated with the DBD. Surprisingly with both jets HLGR proved significantly more resistant compared with all other enterococci. When both jets were compared generally the non pulsed was more effective than the pulsed variant. With DBD it was shown for all enterocci that with increasing drug resistance (MIC as tested in routine susceptibility testing) the susceptibility to CAP decreased.
12 Efficacy In Vivo
Ex vivo Maisch et al. [22] could demonstrate a significant decolonization of MRSA by CAP, in vivo , Isbary et al. [23] and Brehmer et al. [24] found significant bacterial reduction (more than 30%) in patients with chronic wounds. Our group investigated antmicrobial CAP activity in chronic wounds with a CAP device used over decades in surgery (plasma knife, thermocoagulation) and which can be also used in a cold plasma mode (Maxium®-beamer, KLS Martin, Germany). Eighteen chronic wounds (included infected ones) from 11 patients were treated with CAP [14], the effect quantified evaluating the microbial load of wounds after swabbing using a modified Levine-technique [25]. In total 24 bacterial pathogens were recorded thereof 17 (71%) multi drug resistant. CAP exhibited strong antimicrobial effects reducing significantly or eliminating the pathogen load.
Differences of efficacy against different species with and without multi resistance were not found, however, most prominent effects were found regarding gram negative species, interestingly markedly against Pseudomonas aeruginosa and Serratia marcescens) [14]. Al referenced by other authors (Isbary et al. [23] Brehmer et al. [24]) we found excellent tolerability by patients.
13 Practical Points of View
In the context of a multimodal wound treatment concept CAP can provide important supportive benefit especially in chronic wounds colonized with multi drug resistant pathogens.
CAP treatment allows elimination or strong reduction of microbial load within seconds of treatment including highly resistant strains and species. This works using all CAP devices up to now certified as medical products following the referenced data an own experiences. However, different CAP variants can exhibit varying results regarding inhibition zones and killing kinetics using identical treatment times. Because up to now no practical measurements for comparable dosage (output power) are available it is very difficult and often impossible to adjust two CAP devices for comparing purpose. Since unexpectedly technically quite differing CAP sources and techniques (DBD, jets) in many experiments show very similar antimicrobial effects (same exposure time) we conclude robust and similar reaction products. All kind of clinical species seem highly susceptible to CAP, pointing at a working mechanism independent of biochemical acting like conventional drugs. Meanwhile we have found differences in CAP-susceptibility with better susceptibility of strains with low grade multi drug resistance challenging this supposition. In opposite to principally CAP susceptibility, this phenomenon was only observed for specific CAP techniques which now has to be further analyzed in detail. It is important to point at the good susceptibility of bacteria, which also can be experienced by treating bacteria with plasma activated solutions [25, 26]. These solutions (including buffer) were shown to have good effects in vitro and in vivo trials i.e. for antisepsis are promising.
For clinical practice CAP electrodes are important and determine the wound type to be treated. The jets predestinate for point treatment of smaller wounds, and the larger DBD electrodes for larger wound areas. When several cm2 of a wound are to be treated by CAP-jets, with the need of about 60 s of treatment (beam contact to the wound surface) per cm2 several minutes may be necessary for total wound treatment, with typical DBD (2–3 cm electrode diameter) this time will be shorter. However, this treatment time needs further shortening and electrodes with larger surfes (DBD dressing electrodes) are under investigation. Up to now plasma technology of jets is limited to a certain diameter thus larger treatment zones can be reached by completing two or more jets to bundle-jets (“revolver jet” actual under investigation).
13.1 Overview
Facts antimicrobial CAP treatment
-
All common clinical species and strains highly CAP susceptible
-
Also multi drug resistant strains susceptible
-
Also effective against fungi, molds and parasites
-
From 3 s treatment microbiocidal CAP-effects possible,
-
Proteins (blood, secretions) can lower CAP efficacy
-
Good biofilm activity, not yet in vivo fully satisfying
-
No selection of resistant strains
-
Treating staphylococci and enterococci less efficacy towards higher drug resistant strains (dependent on CAP source type)
14 Open Questions
The impressing antimicrobial properties of CAP are the base of treatment of colonized and infected skin and wounds. (▸ Abschn. 4.9, ▸ Abschn. 4.10) Most wounds show reduction to elimination of bacterial load thus supporting healing. Why some wounds do not respond well to CAP treatment has to be investigated in larger studies with stratification of the wound type.
No resistant strains or species but differences in susceptibility to CAP may occur, depend on the CAP type and can be compensated by longer treatment. The role of this phenomenon has to be further evaluated (Relations between cell wall robustness, escape mechanisms and peroxide effects).
Another important effect is the different susceptibility to CAP in dependence on Gram stain ability [27] which also has to be further analyzed questionnating the role of cell membrane and wall stability.
Mainstays of ongoing research are
-
DBD more effective against gram positive pathogens?
-
Jets more effective against gram negative pathogens?
-
DBD less effective towards MRSA than MSSA?
Since CAP sources can exhibit quite different and unexpected antimicrobial effect variations in future all CAP devices should undergo as technical as well as biologic examination during the course of certification by authorities in order to better compare the suitness for the intended use in clinical practice. This analysis should include tests against defined panels of clinical pathogens including multi drug resistant strains like MRSA, VRE and ESBL. Before such a recommendation can be realized, the implementation for normative test methods is strongly warranted.
References
Fridman G, Friedman G, Gutsol A, Shekhter AB, Vasilets VN, Fridman A. Applied plasma medicine. Plasma Process Polym. 2008;5:503–33.
Laroussi M. Low temperature plasmas for medicine? IEEE Trans Plasma Sci. 2009;37(6):714–25.
Daeschlein G, Napp M, Lutze S, Arnold A, von Podewils S, Guembel D, Jünger M. Skin and wound decontamination of multidrug-resistant bacteria by cold atmospheric plasma coagulation. J Dtsch Dermatol Ges. 2015c;13(2):143–50.
Hury S, Vidal DR, Desor F, Pelletier J, Lagarde T. A parametric study of the destruction efficiency of Bacillus spores in low pressure oxygen-based plasmas. Lett Appl Microbiol. 1998;26:417–21.
Lassen KS, Nordby B, Grün R. The dependence of the sporicidal effects on the power and pressure of RF-generated plasma processes. J Biomed Mater Res B Appl Biomater. 2005;74:553–9.
Lerouge S, Wertheimer MR, Marchand R, Tabrizian M, Yahia L. Effect of gas composition on spore mortality and etching during low-pressure plasma sterilization. J Biomed Mater Res. 2000;51:128–35.
Cosgrove SE, Sakoulas G, Perencevich EN, Schwaber MJ, Karchmer AW, Carmeli Y. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis. 2003;36:53–9.
Pasternack MS. Decontamination strategies for MRSA-colonized patients. Curr Infect Dis Rep. 2008;10(5):385–6.
Fridman G, Shereshevsky A, Peddinghaus M, Gutsol A, Vasilets V, Brooks A, Balasubramanian M, Friedman G, Fridman A. Bio-medical applications of non-thermal atmospheric pressure plasma. In: 37th AIAA plasmadynamics and lasers conference, fluid dynamics and co-located conferences, San Francisco, CA; 2006. https://doi.org/10.2514/6.2006-2902.
Daeschlein G, Scholz S, Arnold A, von Woedtke T, Kindel E, Niggemeier M, Weltmann KD, Jünger M. In vitro activity of atmospheric pressure plasma jet (APPJ) against clinical isolates of Demodex folliculorum. IEEE Trans Plasma Sci. 2010b;38(10):2969–73.
Bauer AW, Kirby WM, Sherris JC, Turck M. Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol. 1966;36:493–6.
Daeschlein G, Napp M, von Podewils S, Klare I, Haase H, Kasch R, Ekkernkamp A, Jünger M. Does antibiotic susceptibility impair plasma susceptibility of multi drug resistant enterococci in vitro? Gut Pathog. 2015b;8(1):41.
Daeschlein G, von Woedtke T, Kindel E, Brandenburg R, Weltmann KD, Jünger M. Antibacterial activity of an atmospheric pressure plasma jet against relevant wound pathogens in vitro on a simulated wound environment. Plasma Process Polym. 2010a;7(3–4):224–30.
Daeschlein G, Napp M, von Podewils S, Scholz S, Arnold A, Emmert S, Haase H, Napp J, Spitzmüller R, Gümbel D, Jünger M. Antimicrobial efficacy of a historical high-frequency plasma apparatus in comparison with 2 modern, cold atmospheric pressure plasma devices. Surg Innov. 2015a;22(4):394–400.
Hong YF, Kang JG, Lee HY, Uhm HS, Moon E, Park YH. Sterilization effect of atmospheric plasma on Escherichia coli and Bacillus subtilis endospores. Lett Appl Microbiol. 2009;48:33–7.
Lee K, Paek K, Ju W, Lee Y. Sterilization of bacteria, yeast, and bacterial endospores by atmospheric-pressure cold plasma using helium and oxygen. J Microbiol. 2006;44:269–75.
Kayes MM, Critzer FJ, Kelly-Wintenberg K, Roth JR, Montie T, Golden DA. Inactivation of foodborne pathogens using a one atmosphere uniform glow discharge plasma. Foodborne Pathog Dis. 2007;4:50–9.
Daeschlein G, Scholz S, Arnold A, von Podewils S, Haase H, Emmert S, von Woedtke T, Weltmann KD, Jünger M. In vitro susceptibility of important skin and wound pathogens against low temperature atmospheric pressure plasma jet (APPJ) and dielectric barrier discharge plasma (DBD). Plasma Process Polym. 2012;9(4):380–9.
Daeschlein G, Napp M, von Podewils M, Lutze S, Emmert S, Lange A, Klare I, Haase H, Gümbel D, von Woedtke T, Jünger M. In vitro susceptibility of multidrug resistant skin and wound pathogens against low temperature atmospheric pressure plasma jet (APPJ) and dielectric barrier disc harge plasma (DBD). Plasma Process Polym. 2014;11(2):175–83. https://doi.org/10.1002/ppap.201300070.
Napp M, Daeschlein G, von Podewils S, Hinz P, Emmert S, Haase H, Spitzmueller R, Gümbel D, Katsch R, Jünger M. In vitro susceptibility of methicillin-resistant and methicillin-sensitive strains of Staphylococcus aureus to two different cold atmospheric plasma sources. Infection. 2016;44(4):531–7.
Kawai M, Yamada S, Ishidoshiro A, et al. Cell-wall thickness: possible mechanism of acriflavine resistance in 05.16 – 17:59 Springer-book-ProfMed Seite 11 von 11 meticillin-resistant Staphylococcus aureus. J Med Microbiol. 2009;58(3):331–6.
Maisch T, Shimizu T, Li YF, Heinlin J, Karrer S, Morfill G, Zimmermann JL. Decolonisation of MRSA, S. aureus and E. coli by cold-atmospheric plasma using a porcine skin model in vitro. PLoS One. 2012;7(4):e34610.
Isbary G, Morfill G, Schmidt HU, Georgi M, Ramrath K, Heinlin J, Karrer S, Landthaler M, et al. A first prospective randomized controlled trial to decrease bacterial load using cold atmospheric argon plasma on chronic wounds in patients. Br J Dermatol. 2010;163(1):78–82.
Brehmer F, Haenssle HA, Daeschlein G, et al. Alleviation of chronic venous leg ulcers with a hand-held dielectric barrier discharge plasma generator (PlasmaDerm® VU-2010): results of a monocentric, two-armed, open, prospective, randomized and controlled trial (NCT01415622). J Eur Acad Dermatol Venereol. 2015;29(1):148–55. https://doi.org/10.1111/jdv.12490.
Daeschlein G, Kramer A. Microbiological sampling in chronic wounds. GMS Krankenhaushyg Interdiszip. 2006;1(1):Doc10.
Traylor MJ, Pavlovich MJ, Karim S, Hait P, Sakiyama Y, Clark DS, Graves DB. Long-term antibacterial efficacy of air plasma-activated water. J Phys D. 2011;44:1–4.
Ermolaeva SA, Varfolomeev AF, Chernukha MY, Yurov DS, Vasiliev MM, Kaminskaya AA, et al. Bactericidal effects of non-thermal argon plasma in vitro, in biofilms and in the animal model of infected wounds. J Med Microbiol. 2011;60:75–83.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Daeschlein, G. (2018). Antimicrobial Activity of Plasma. In: Metelmann, HR., von Woedtke, T., Weltmann, KD. (eds) Comprehensive Clinical Plasma Medicine. Springer, Cham. https://doi.org/10.1007/978-3-319-67627-2_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-67627-2_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-67626-5
Online ISBN: 978-3-319-67627-2
eBook Packages: MedicineMedicine (R0)