Abstract
Background and Objective
Danoprevir, a potent, selective inhibitor of the hepatitis C virus (HCV) NS3/4A protease, is metabolized by cytochrome P450 (CYP) Clinical studies in HCV patients have shown a potential need for a high danoprevir daily dose and/or dosing frequency. Ritonavir, an HIV-1 protease inhibitor (PI) and potent CYP3 A inhibitor, is used as a pharmacokinetic enhancer at subtherapeutic doses in combination with other HIV PIs. Coadministering danoprevir with ritonavir as a pharmacokinetic enhancer could allow reduced danoprevir doses and/or dosing frequency. Here we evaluate the impact of ritonavir on danoprevir pharmacokinetics.
Methods
The effects of low-dose ritonavir on danoprevir pharmacokinetics were simulated using Simcyp, a population-based simulator. Following results from this drug-drug interaction (DDI) model, a crossover study was performed in healthy volunteers to investigate the effects of acute and repeat dosing of low-dose ritonavir on danoprevir single-dose pharmacokinetics. Volunteers received a single oral dose of danoprevir 100 mg in a fixed sequence as follows: alone, and on the first day and the last day of 10-day dosing with ritonavir 100 mg every 12 hours.
Results
The initial DDI model predicted that following multiple dosing of ritonavir 100 mg every 12 hours for 10 days, the danoprevir area under the plasma concentration-time curve (AUC) from time zero to 24 hours and maximum plasma drug concentration (Cmax) would increase by about 3.9- and 3.2-fold, respectively. The clinical results at day 10 of ritonavir dosing showed that the plasma drug concentration at 12 hours postdose, AUC from time zero to infinity and Cmax of danoprevir increased by approximately 42-fold, 5.5-fold and 3.2-fold, respectively, compared with danoprevir alone. The DDI model was refined with the clinical data and sensitivity analyses were performed to better understand factors impacting the ritonavir-danoprevir interaction.
Conclusion
DDI model simulations predicted that danoprevir exposures could be successfully enhanced with ritonavir coadministration, and that a clinical study confirming this result was warranted. The clinical results demonstrate that low-dose ritonavir enhances the pharmacokinetic profile of low-dose danoprevir such that overall danoprevir exposures can be reduced while sustaining danoprevir trough concentrations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Danoprevir (RG7227 or ITMN-191) is a potent, selective inhibitor of the hepatitis C virus (HCV) serine protease encoded by the nonstructural gene 3/4A (NS3/4A), a protease critical for HCV polypeptide post-translational modification and viral replication. Danoprevir has potent activity against isolated HCV NS3/4A proteases derived from HCV genotypes 1 through 6.[1] The safety, tolerability, pharmacokinetics and/or antiviral activity of danoprevir alone or in combination with pegylated interferon (PEG-IFN)-α and ribavirin have been characterized in healthy volunteers and treatment-naive patients with chronic HCV genotype 1.[2–7] Danoprevir phase I studies showed that monotherapy dosing every 8 hours resulted in greater HCV RNA reductions from baseline than dosing every 12 hours, and that high doses up to 900 mg every 12 hours, in combination with PEG-IFN and ribavirin, resulted in robust antiviral activity.[4,5] Given the potential need for a high daily dose and/or dosing frequency, the option of coadministering danoprevir with a pharmacokinetic enhancer was explored.
HIV-1 protease inhibitor (PI) ritonavir is used as a pharmacokinetic enhancer at doses of 100–400 mg/day in combination with other HIV PIs.[8,9] Although ritonavir displays inhibition and induction of cytochrome P450 (CYP) 3A, its inhibitory effect is predominant.[10] Coadministration with subtherapeutic ritonavir enhances the pharmacokinetics of HIV PIs, substrates of CYP3A, allowing for simplification of the dosing regimen of most HIV PIs, including a reduced dosing frequency and/or a decrease in doses needed to maintain therapeutic drug concentrations. Definitive reaction phenotyping studies conducted in recombinant CYP and human liver microsomes with selective CYP inhibitors at multiple substrate concentrations showed that CYP3A is the primary isozyme responsible for metabolism of danoprevir.[11] Since danoprevir metabolism is mediated primarily by CYP3A, ritonavir has the potential to enhance danoprevir pharmacokinetics, allowing reduced dosing frequency.
This work illustrates the use of drug-drug interaction (DDI) modelling to explore whether ritonavir can be used to improve the therapeutic window for danoprevir. The potential impact of low-dose ritonavir on danoprevir pharmacokinetics was first simulated using Simcyp (Simcyp Ltd, Sheffield, UK), a population-based clinical trial simulator for pharmacokinetics and DDI predictions.[12] The prospective DDI prediction was performed early in danoprevir phase I and so there were data gaps (e.g. a human mass balance study had not been conducted). Sensitivity analysis was used for understanding the implications of key uncertainties. Following simulation results, a confirmative phase I clinical DDI study was conducted in healthy volunteers to assess the effects of acute and repeat dosing of low-dose ritonavir on danoprevir pharmacokinetics. Finally, the clinical data were used to refine the DDI model to allow better understanding of the impact of ritonavir on danoprevir pharmacokinetics.
Methods
Drug-Drug Interaction (DDI) Modelling
Effects of low-dose ritonavir on danoprevir pharmacokinetics were predicted using Simcyp.[13] The initial model was developed in version 8.01, and the refined model in version 10.00. Model parameters (table I) include the contribution of CYP3A to the fraction of drug metabolism (fm, CYP3A) and enzyme kinetic parameters (maximum rate [Vmax] and Michaelis-Menten constant [Km]) derived from in vitro enzyme kinetic studies, in which metabolite formation could only be quantified for CYP3A. Values for in vitro parameters were obtained either from in vitro experiments or by using the software’s built-in calculation methods. A factor of active uptake into hepatocytes was incorporated into the simulations based on preclinical data. The liver-to-plasma ratio in monkeys and rats were about 127 and 10, respectively, which could be attributed to differences in plasma protein binding (i.e. the fraction of unbound drug in plasma [fu, p] is about 0.1% in rats and 7.5% in monkeys).[1] The estimated human liver-to-plasma ratio for danoprevir, which has protein binding between the rat and monkey value (table I), was estimated to be 45 using linear regression. Microsomal binding data were not available, and the free fraction in microsomes (fu,mic) was estimated using an in silico algorithm. Gut extraction was estimated based on enzyme kinetic parameters, permeability, and liver blood flow.[14] Weak acids such as danoprevir tend to have less binding to microsomes than bases or neutrals,[15,16] i.e. fu,mic is about 1 unless logP is greater than about 4, which makes a precise value less important.
The initial model was developed to describe danoprevir pharmacokinetics in healthy volunteers from a previous phase I study in which subjects received danoprevir 100 mg under fed conditions. Absorption was simulated using a first-order rate constant (ka) derived from the clinical data. Fraction absorbed (fa) was estimated based on preclinical data. Renal clearance of drug from plasma (CLR), estimated as fu × the human glomerular filtration rate, was a low value consistent with the low CLR observed in preclinical species. The volume of distribution at steady state was estimated based on preclinical data.
Default model parameters were used for ritonavir. Ritonavir can inhibit and induce CYP3A. Whether a net induction or inhibition effect is observed is variable, hard to predict and depends on many factors.[17] The inhibitory effect was expected to be predominant for a low 100 mg dose.[10] Competitive inhibition was included in the model, but the model did not include time-dependent inhibition (TDI) or induction, an approach that has also been used by others.[18,19] The possible effect of ritonavir on transporters was not considered even though ritonavir inhibits organic anion-transporting polypeptide liver uptake transporters in vitro. The concentration of drug producing 50% inhibition/inhibition constant values for ritonavir in several transporter assays are above the free maximum plasma drug concentration (Cmax) by about 180- to 470-fold for a ritonavir 100 mg every 12 hours dose.[20,21]
DDI simulations were performed to predict the fold increase in danoprevir area under the plasma concentration-time curve (AUC) from time zero to 24 hours (AUC24) and Cmax in the presence of ritonavir 100 mg given every 12 hours on the first and tenth day of dosing. Ritonavir 100 mg every 12 hours is the most common dosing regimen for pharmacokinetic enhancement, and steady-state ritonavir pharmacokinetics are reached within 10 days of dosing. The simulated clinical trials were performed for a virtual population of 28 healthy volunteers aged 18–45 years old, with an equal gender distribution. The median and population extremes (5th and 95th percentiles) were determined. Possible variations in DDI predictions due to absorption lag time (tlag) resulting from variable stomach emptying times and differences in dissolution with food were assessed using sensitivity analysis. The classical absorption model in Simcyp uses only two parameters, ka and fa. The lag time was specified by simulating the time of danoprevir administration at tlag after the ritonavir administration. Also, in another sensitivity analysis aimed at understanding the risk of an incorrect result from limited information on the mechanism of clearance (i.e. since no human mass balance data were available), a range of values for fm, CYP3A was assessed to examine the implications of potential non-CYP3A clearance.
The clinical trial data were used to refine the initial model. The refined model was not developed as a fitting exercise. Rather, selected input parameters known with limited confidence were adjusted so that the model more closely described danoprevir concentrations when administered alone or with acute ritonavir. Model parameters adjusted to better describe the data included tlag, ka, fa and fm,CYP3A, as listed in table I. Absorption model parameters were adjusted due to danoprevir’s high variability in terms of oral absorption (e.g. absorption for this weak acid depends on the stomach transit time, which can vary significantly between subjects). Additionally, TDI of CYP3A by ritonavir was included in the model as described by Wang.[22] There was some uncertainty about mechanisms impacting the DDI with long-term ritonavir administration (see Discussion), and therefore the refined model was not used to simulate danoprevir kinetics with long-term ritonavir administration. The refined model was used to understand mechanisms impacting the ritonavir-danoprevir DDI.
Clinical Study
Study Design
This single-centre, open-label, fixed-sequence, crossover study investigated the effects of acute and repeat dosing of low-dose ritonavir on single-dose pharmacokinetics of danoprevir in healthy volunteers. Subjects were screened for participation within 21 days of dosing. Fourteen healthy volunteers between 18 and 45 years of age with a body mass index between 18 and 30 kg/m2 were planned for enrolment in the study. All subjects were judged to be healthy based on medical history, physical findings, ECGs, vital signs measurements and clinical laboratory test results. Subjects were prohibited from the use of any medications (prescription or over-the-counter) within 2 weeks (4 weeks for enzyme inducers) or 5 half-lives (whichever is longer) and the consumption of any nutrients known to modulate CYP enzyme activity within 7 days before the first dose of study medication and during the study.
The study was conducted at Arkansas Research Medical Testing, LLC (Little Rock, AR, USA). It was approved by the Institutional Review Board of Arkansas Research Medical Testing, LLC and performed in accordance with the current Federal Regulations, the principles of the Declaration of Helsinki and the Guideline for Good Clinical Practice International Conference on Harmonisation Tripartite Guideline. All subjects were informed about the purposes of the study and gave their written consent.
A single oral dose of danoprevir 100 mg was administered on day 1 followed by a 48-hour washout period. Ritonavir 100 mg was administered every 12 hours for 10 days from days 3 to 12. On days 3 and 12, a single oral dose of danoprevir 100 mg was coadministered with the morning dose of ritonavir. Danoprevir (alone and with ritonavir) was administered with a standard high-fat breakfast since a high-fat meal was found to increase danoprevir systemic exposure. Volunteers were required to stay in the study clinic during the study and washout period for compliance purposes and safety monitoring.
Physical examinations, ECGs, vital sign measurements and clinical laboratory tests were performed and adverse events were monitored throughout the study to assess safety and tolerability.
Pharmacokinetic Sampling and Analyses
Blood samples for the determination of danoprevir plasma concentrations were collected predose and at 0.5, 1, 1.5, 2, 2.5, 3, 3.5, 4, 6, 8, 12 and 24 hours after danoprevir administration. On days when danoprevir and ritonavir were coadministered, additional blood samples were collected at 36 and 48 hours. Blood samples were collected and processed as described previously.[23]
Measurements of danoprevir in plasma were performed using validated and specific liquid chromatography with tandem mass spectrometric detection assay by Covance Laboratories Inc. (Madison, WI, USA). Plasma samples were not assayed for ritonavir as the study was not designed to evaluate the effect of danoprevir on ritonavir’s pharmacokinetics. Danoprevir and the internal standard, ARRY-333802, were extracted from human plasma by solid-phase extraction as described previously.[23] Using 50 μL of human plasma, the lower limit of quantification for danoprevir was 0.01 ng/mL. The assays were selective, reproducible, precise and accurate for danoprevir. The average between-run precision (% coefficient of variation) and accuracy (%bias) were 7.7% and −3.3%, respectively.
Standard non-compartmental (WinNonlin v5.2.1, Pharsight Corporation, Mountain View, CA, USA) evaluation of pharmacokinetic parameters from plasma concentrations was performed for danoprevir. All calculations used actual times, where zero was substituted for concentrations below the quantification limit of the assay, except when the value appeared after the last measurable concentration or inside a series of concentration measurements constituting a reasonable profile where it was assigned as missing. Primary danoprevir pharmacokinetic parameters are maximum plasma concentrations (Cmax) and AUC from time zero to infinity (AUC∞). Secondary danoprevir pharmacokinetic parameters include time to Cmax (tmax), terminal elimination half-life (t1/2), and plasma drug concentration at 12 hours postdose (C12). Danoprevir C12 for four subjects on day 1 (danoprevir alone) were below the limit of quantification and were estimated using equation 1:[24]

where Clast is the last measurable concentration that was observed at time tlast.
To compare danoprevir pharmacokinetics with and without ritonavir, ANOVA was used to analyse AUC∞, Cmax and C12 using equation 2:

where Yij denoted the pharmacokinetic parameter to be analysed; μ was the mean of the transformed variable; τi was the fixed effect of treatment; sj was the random effect of subject; and ɛij was the error. Random deviations ɛij were assumed to be independent and normally distributed with a mean of zero and a common variance σ2. The group comparisons τ danoprevir+ritonavir − τ danoprevir, residual variance σ2 and 90% confidence limits for the group comparisons were estimated from the ANOVA model. For log-transformed variables (AUC∞, Cmax and C12), the ratio of true group means and the confidence limits for the corresponding ratio of means of the untransformed variables were calculated by exponentiation of the least squares mean differences and the confidence limits for the transformed values, respectively. A similar model was used to compare the increases in C12 with acute ritonavir dosing versus repeated ritonavir dosing.
Results
Initial DDI Model
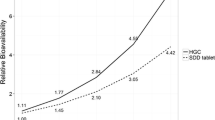
Simulations for fed-state danoprevir pharmacokinetics predicted 1.64- and 2.05-fold increases in danoprevir Cmax and AUC24, respectively, on the first day of ritonavir 100 mg (table II). Following multiple dosing of ritonavir 100 mg every 12 hours for 10 days, danoprevir Cmax and AUC24 were predicted to increase by about 3.2- and 3.9-fold, respectively. Simulations predicted a larger impact of ritonavir on C12 of about 8.3- and 18-fold increases on the first and last day of ritonavir 100 mg every 12 hours dosing, respectively. The prediction of approximately 2-fold greater interaction upon repeat dosing was primarily due to higher ritonavir concentrations at steady state than on day 1 in simulations (data not shown).
Simulations were performed to understand how prolonged gastric emptying times following a large meal might impact the DDI. Since ritonavir has a tmax of about 4 hours, sensitivity analysis indicated a slightly higher interaction effect with a delayed danoprevir tmax (e.g. as might be expected for a large meal, which can prolong gastric emptying substantially in some people). Assuming the fa was unchanged with varying tlag in the fed condition, a tlag of 3 hours with food resulted in an approximately 37% increase in the danoprevir AUC24 ratio from 2.05 to 2.81 when given with the first dose of ritonavir, or a 10% increase from 3.94 to 4.38 when coadministered with ritonavir for 10 days (table II). This calculation provided confidence that subjects with relatively long stomach emptying times would not be at risk of extremely high exposures.
In vitro data suggest CYP3A is primarily responsible for danoprevir metabolism, but other pathways could contribute to clearance in vivo. Therefore, to understand the implications/risk of a potentially inaccurate fm,CYP3A value in the absence of human disposition data, the variation of CYP3A contribution (fm,CYP3A) to total danoprevir clearance and its impact on the DDI prediction were also simulated. These simulations indicate that if the contribution of CYP3A to the overall clearance is less than 70%, the effect of ritonavir on danoprevir exposure could be markedly less (table III). The clinical study results provided additional data to elucidate the potential contribution of CYP3A in vivo.
Clinical Study
Healthy volunteers (seven male, seven female) with a baseline mean age of 35 years (range 20–44 years) and a baseline mean body weight of 74 kg (range 51–97 kg) participated in the study. Two female subjects were withdrawn due to an inability to finish the mandatory standardized high-fat breakfast within the required period of time.
The median plasma concentration-time profiles for danoprevir 100 mg single dose when given alone (day 1), with the first day of ritonavir 100 mg (day 3) and on the last day of the 10-day dosing of ritonavir 100 mg every 12 hours (day 12) are illustrated in figure 1. Both acute and repeat dosing of ritonavir 100 mg every 12 hours significantly increased danoprevir C12, while a lesser effect was observed on danoprevir AUC∞ (∼5-fold increase) and Cmax (∼3-fold increase) [table IV]. Danoprevir t1/2 was also prolonged in the presence of ritonavir (∼3–4 hours vs 1 hour) [table IV]. Acute and repeat dosing of ritonavir 100 mg every 12 hours had a similar effect on danoprevir AUC∞ and Cmax. Although the mean effect of acute ritonavir on danoprevir C12 appears to be more pronounced (∼65-fold increase) than the mean effect of ritonavir repeat dosing (∼42-fold increase), the difference is not statistically significant (p = 0.10).
In general, administration of danoprevir alone or with low-dose ritonavir was well tolerated. Nine of 14 subjects (64%) reported at least one adverse event during and up to 21 days of follow-up after treatment; all were mild or moderate in intensity. There were no reports of serious adverse events and no adverse events that led to discontinuation of treatment. There were no clinically significant changes in laboratory safety tests, vital signs or ECGs.
Refined DDI Model
In Simcyp versions 8 and 9, the turnover rate for hepatic CYP3A, kdeg, was 0.0077 h−1. A study assessing the accuracy of CYP3A TDI predictions in Simcyp reported better success across mechanism-based inhibitors (i.e. less over-estimation of TDI DDIs) using a kdeg value of 0.03 h−1.[22] If TDI had been included in the initial model developed in Simcyp version 8, the DDI would have been significantly overestimated. In Simcyp version 10, the kdeg value was 0.0193 h−1. In a recent study comparing a novel pharmacokinetic enhancer GS-9350 with ritonavir as a comparator, patients were administered midazolam 5 mg alone or with ritonavir 100 mg. As a check of the refined model incorporating TDI, the midazolam/ritonavir DDI was simulated in Simcyp version 10.[25] The reported AUC was 64.1 ng · h/mL for midazolam alone (n = 60) or 1530 ng · h/mL with ritonavir coadministration (n = 9). Without TDI included in the model, the simulated AUC ratio was 2.5 for a population representative. With TDI included and using the new kdeg of 0.0193 h−1, the predicted AUC ratio was 13, which is consistent with the observed data. Therefore, incorporating both mechanisms of CYP3A inhibition in ritonavir DDI models is important.
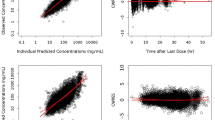
The refined model incorporating TDI described danoprevir pharmacokinetics alone or with acute ritonavir dosing (see figure 2, which shows simulations for a representative population). The observed AUC ratio on day 3 (acute ritonavir dosing) was 5.69 (table IV); the AUC ratio was underestimated by the initial model that did not consider TDI (2.05), but was in better agreement for the refined model with a value of 6.9. These results indicate that fm,CYP3A may be about 70%. The refined model incorporating TDI predicted much more CYP3A inhibition than the initial model, and fm,CYP3A had to be reduced for the simulations to match the data. For TDI the time to reach steady state must be considered, but given the high level of inhibition with the initial doses of ritonavir it is not a concern for this case.
Simulated (refined model) and median observed danoprevir plasma concentration-time profiles following single-dose administration of danoprevir 100 mg alone (day 1) and with the first day of ritonavir 100 mg every 12 hours dosing (day 3). Simulations of danoprevir with acute ritonavir dosing explored whether a slight increase in simulated ritonavir pharmacokinetics (i.e. for 130 mg every 12 hours instead of 100 mg every 12 hours) would result in a larger interaction. q12h = every 12 hours.
Another simulation was performed for ritonavir 130 mg every 12 hours (figure 2), to determine whether the DDI would be sensitive to a small change in ritonavir concentrations. For a 30% difference in simulated ritonavir levels (i.e. on the first dose simulated ritonavir Cmax increased from 0.99 to 1.3 μg/mL), the AUC ratio increased only to about 7.3, a minor change. This result is consistent with reports that the maximum effect of ritonavir as a pharmacokinetic enhancer occurs for several compounds at a dose of about 100 mg twice daily.[26]
Discussion
DDIs for High Extraction Compounds
In the clinical study, low-dose ritonavir significantly increased systemic exposure to danoprevir. Repeat dosing for 10 days resulted in a larger increase of danoprevir C12 (∼42-fold) than of AUC∞ (∼5.5-fold), but had less effect on danoprevir Cmax (∼3.2-fold) and modestly prolonged t1/2, suggesting that ritonavir predominantly inhibited the first-pass metabolism of danoprevir. The effect of low-dose ritonavir on danoprevir pharmacokinetics appears to be similar to its effect on HIV PIs, which have high first-pass metabolism.[27] For compounds such as danoprevir with high hepatic extraction, the effect of the inhibitor on clearance (and therefore on t1/2) is expected to be minor, while the effect of the inhibitor on hepatic first-pass extraction is expected to be major.[28] Since the minimum plasma drug concentration (Cmin) increased more than the Cmax and AUC with ritonavir coadministration, low-dose ritonavir enhanced the pharmacokinetic profile of danoprevir such that a lower danoprevir dose can achieve efficacious trough concentrations while overall danoprevir exposures can be reduced.
Simulation results suggested that the change in danoprevir t1/2 would be minor (i.e. about a 40% increase as expected for a high extraction compound), and that the majority of the effect of ritonavir would be through altered first-pass liver and gut extraction. But the observed t1/2 difference may reflect multiple factors. When administered alone, danoprevir had one-compartment pharmacokinetics due to plasma concentrations going below the limit of quantification after 8–12 hours postdose, before the effect of a second compartment became apparent (figure 1). When coadministered with ritonavir, danoprevir pharmacokinetic profiles exhibited two-compartment pharmacokinetics with a second distribution phase at times longer than 12 hours, and hence a longer terminal t1/2 reflecting both the impact of ritonavir and terminal distribution kinetics. This is not to suggest that ritonavir impacts distribution; in another study in which a population pharmacokinetic model was developed for danoprevir pharmacokinetics without ritonavir coadministration but with higher danoprevir doses, a two-compartment model was required to describe danoprevir pharmacokinetics.[7] Therefore, despite the observed 2.4- to 3.5-fold increase in danoprevir t1/2 in the presence of ritonavir, the behaviour is still consistent with that of a high-extraction compound.
The DDI model described danoprevir pharmacokinetics using a one-compartment model (the only classical pharmacokinetic model available in the software), and so the impact of a second compartment was not included. Therefore, the model may under-estimate the impact of ritonavir on danoprevir C12, but a significant impact on C12 was predicted despite the underestimation. The use of Simcyp in DDI modelling has primarily been validated in terms of Cmax and AUC predictions. Its use in predicting the effect of a DDI on Cmin requires more validation.
Model Limitations
Although the refined model reasonably matches day 1 and day 3 clinical data, there is still uncertainty around key mechanisms impacting danoprevir pharmacokinetics and the ritonavir/danoprevir DDI. Some limitations in the initial model are still present in the final model (e.g. one-compartment pharmacokinetic model, no ritonavir pharmacokinetic data). Wang[22] found Cmin values from repeat administration of ritonavir 200 mg to be somewhat underestimated by Simcyp. Therefore, the model should be used with caution and be further refined as additional data become available. Ritonavir pharmacokinetic data, particularly in patients with chronic HCV, additional pharmacokinetic data for danoprevir pharmacokinetics when coadministered with ritonavir for longer periods, and human mass balance study data may be useful for improving the DDI model.
The appeal of the current approach is the simple method used to deal with liver uptake at early stages of development when limited data are available. However, as the compound moves further in development a mechanistic model such as that proposed by Poirier et al.[29] may have better utility. This empirical approach for dealing with liver uptake transporters using a factor for active uptake could significantly overestimate interactions for compounds whose clearance is limited by only the rate of liver uptake.[30]
Clinical Significance
CYP3A-mediated DDI by low-dose ritonavir has been successfully exploited for PI therapy in HIV-infected patients. Ritonavir-enhanced HIV PIs have been shown to prevent or reduce emergence of resistance despite reduced doses and less dosing frequency than HIV PIs administered with no pharmacokinetic enhancement. This therapeutic benefit has been attributed to the achievement of a trough drug concentration higher than the inhibitory concentration of mutated variants, thereby raising the genetic barrier.[7] Similarly, the trough drug concentration for HCV PIs may be important in minimizing or preventing the emergence of resistance.[31] Pharmacokinetic-pharmacodynamic modelling showed that the danoprevir trough concentration has the strongest relationship with maximum change in HCV RNA compared with other pharmacokinetic parameters.[3]
Treatment of patients with danoprevir 900 mg twice daily in an ongoing phase II study was discontinued because of asymptomatic grade 4 ALT elevations (>10 times above the upper limit of normal).[6] Higher danoprevir AUC and Cmax were subsequently shown to be associated with higher probability of ALT elevations.[7] Given the substantial effect of low-dose ritonavir on danoprevir C12, which is equivalent to the trough concentration for a twice-daily regimen, a reduced danoprevir dose and overall exposure (AUC and Cmax) could be explored while still maintaining danoprevir concentrations above the efficacy threshold.
Based on the clinical DDI results, a phase Ib study was conducted to evaluate the safety, tolerability, antiviral activity and pharmacokinetics of once- and twice-daily reduced danoprevir doses with low-dose ritonavir in combination with PEG-IFN plus ribavirin.[23] This study demonstrated the success of low-dose danoprevir/ritonavir to achieve similar or improved efficacy, in terms of patients achieving undetectable HCV levels, compared with results from a phase Ib study[32] in which patients were coadministered danoprevir with PEG-IFN plus ribavirin for 14 days. Similar or improved danoprevir efficacy at lower doses when coadministered with ritonavir can be attributed to a similar or higher Cmin. As the DDI modelling and published clinical data show, low-dose ritonavir increased the Cmin and improved efficacy at a lower danoprevir dose, which is expected to reduce the probability of ALT elevations and improve the therapeutic window.
Conclusions
A model describing the DDI between ritonavir and danoprevir was developed by integrating preclinical and clinical data. Simulation results suggested that ritonavir could significantly improve danoprevir exposures, and that a clinical study was warranted. Results from the clinical study indicate that coadministration of ritonavir 100 mg twice daily significantly enhanced danoprevir pharmacokinetics. The low-dose ritonavir resulted in larger increases in danoprevir trough concentrations than in the AUC, and in marginal increases in Cmax, offering the potential to reduce danoprevir dose and overall exposure in future studies.
References
Seiwert SD, Andrews SW, Jiang Y, et al. Preclinical characteristics of the hepatitis C virus NS3/4A protease inhibitor ITMN-191 (R7227). Antimicrob Agents Chemother 2008 Dec; 52(12): 4432–41
Bradford WZ, Rubino C, Porter S, et al. A phase 1 study of the safety, toler-ability, and pharmacokinetics of single ascending oral doses of the NS3/4A protease inhibitor ITMN-191 in healthy subjects [abstract]. Hepatology 2008 Oct; 48 Suppl. 1: 1146A
Rubino C, Bradford WZ, Forrest A, et al. Pharmacokinetic-pharmacodynamic (PK-PD) relationships for ITMN-191 in a phase 1 multiple ascending dose trial in patients with genotype 1 chronic hepatitis C infection [abstract]. Hepatology 2008 Oct; 48 Suppl. 2: 1140A–1A
Forestier N, Larrey DG, Guyader D, et al. Treatment of chronic hepatitis C patients with the NS3/4A protease inhibitor danoprevir (ITMN-191/RG7227) leads to robust reductions in viral RNA: a phase 1b multiple ascending dose study. J Hepatol 2011 Jun; 54: 1130–6
Forestier N, Larrey D, Marcellin P, et al. Antiviral activity and safety of ITMN-191 in combination with peginterferon alfa-2a and ribavirin in patients with chronic C virus (HCV) [abstract]. J Hepatol 2009; 50 Suppl. 1: S35
Terrault N, Cooper C, Balart LA, et al. Phase II randomised, partially-blind, parallel-group study of oral danoprevir (RG7227) with PegIFN α-2a (PEGASYS®) plus ribavirin in treatment-naive genotype 1 patients with CHC: results of planned week 12 interim analysis of the ATLAS study [abstract]. Hepatology 2010 Oct; 52 Suppl. 4: 335A
Levi M, Frey N, Hsu JC, et al. High exposure to danoprevir (RG7227) increases the probability of ALT elevations in patients treated with danoprevir plus peginterferon alfa-2a (40KD) (PEGASYS®) plus ribavirin [abstract]. Hepatology 2010 Oct; 52 Suppl. 4: 1216A
Zeldin RK, Petruschke RA. Pharmacological and therapeutic properties of ritonavir-boosted protease inhibitor therapy in HIV-infected patients. J Antimicrob Chemother 2004 Jan; 53(1): 4–9
Moyle GJ, Back D. Principles and practice of HIV-protease inhibitor pharmacoenhancement. HIV Med 2001 Apr; 2(2): 105–13
Foisy MM, Yakiwchuk EM, Hughes CA. Induction effects of ritonavir: implications for drug interactions. Ann Pharmacother 2008 Jul; 42(7): 1048–59
Data on file, Roche, 2009
Grime KH, Bird J, Ferguson D, et al. Mechanism-based inhibition of cytochrome P450 enzymes: an evaluation of early decision making in vitro approaches and drug-drug interaction prediction methods. Eur J Pharm Sci 2009 Feb 15; 36(2–3): 175–91
Simcyp. A guide for IVIVE and PBPK modelling using the Simcyp population-based ADME simulator. Sheffield: Simcyp Limited, 2010: 394
Yang JS, Jamei M, Yeo KR, et al. Prediction of intestinal first-pass drug metabolism. Curr Drug Metab 2007 Oct; 8: 676–84
Gao H, Steyn SJ, Chang G, et al. Assessment of in silico models for fraction of unbound drug in human liver microsomes. Expert Opin Drug Metab Toxicol 2010 May; 6(5): 533–42
Turner DB, Yeo KR, Tucker GT, et al. Prediction of non-specific hepatic microsomal binding from readily available physicochemical properties [abstract no. A231]. Drug Metab Rev 2006; 38(1): 162
Cozza KL, Armstrong SC, Oesterheld JR. Concise guide to drug interaction principles for medical practice: cytochrome P450s, UGTs, P-glycoproteins. Arlington (VA): American Psychiatric Publishing, 2003 Jan
Almond L, Yeo KR, Howgate E, et al. Mechanistic prediction of HIV drug-drug interactions in virtual populations from in vitro enzyme kinetic data: ritonavir and saquinavir. International Workshop on Clinical Pharmacology of HIV Therapy, Budapest, Hungary, 16th–18th April 2007 [online]. Available from URL: http://www.simcyp.com/UploadedFiles/154/Lisa_Almond_2007_Budapest_SQVr_finalised.pdf [Accessed 2011 Nov 10]
Hyland R, Dickins M, Collins C, et al. Maraviroc: in vitro assessment of drug-drug interaction potential. Br J Clin Pharmacol 2008 Oct; 66: 498–507
Annaert P, Ye ZW, Stieger B, et al. Interaction of HIV protease inhibitors with OATP1B1, 1B3, and 2B1. Xenobiotica 2010; 40: 163–76
Jackson A, Watson V, Back D, et al. Plasma and intracellular pharmacokinetics of darunavir/ritonavir once daily and raltegravir once and twice daily in HIV-infected individuals. J Acquir Immune Defic Syndr 2011 Dec 15; 58(5): 450–7
Wang YH. Confidence assessment of the Simcyp time-based approach and a static mathematical model in predicting clinical drug-drug interactions for me-chanism-based CYP3A inhibitors. Drug Metab Dispos 2010 Apr; 38: 1094–104
Gane EJ, Rouzier R, Stedman C, et al. Antiviral activity, safety, and pharmacokinetics of danoprevir/ritonavir plus PEG-IFN α-2a/RBV in hepatitis C patients. J Hepatol 2011 Nov; 55(5): 972–9
Gabrielsson J, Weiner D. Pharmacokinetic and pharmacodynamic data analysis: concepts and applications. 4th ed. Stockholm: Swedish Pharmaceutical Press, 2007 Jul
Mathias AA, German P, Murray BP, et al. Pharmacokinetics and pharmacodynamics of GS-9350: a novel pharmacokinetic enhancer without anti-HIV activity. Clin Pharmacol Ther 2010 Mar; 87(3): 322–9
Hill A, van der Lugt J, Sawyer W, et al. How much ritonavir is needed to boost protease inhibitors? Systematic review of 17 dose-ranging pharmacokinetic trials. AIDS 2009 Nov 13; 23(17): 2237–45
Hsu A, Granneman GR, Bertz RJ. Ritonavir: clinical pharmacokinetics and interactions with other anti-HIV agents. Clin Pharmacokinet 1998 Oct; 35: 275–91
Kenny JR, McGinnity DF, Grime K, et al. Utilization of in vitro cytochrome P450 inhibition data for projecting clinical drug-drug interactions. In: Gad SC, editor. Preclinical development handbook: ADME and biopharmaceutical properties. Hoboken (NJ): Wiley, 2008 Aug: 775–828
Poirier A, Cascais AC, Funk C, et al. Prediction of pharmacokinetic profile of valsartan in human based on in vitro uptake transport data. J Pharmacokinet Pharmacodyn 2009; 36: 585–611
Watanabe T, Kusuhara H, Sugiyama Y. Application of physiologically based pharmacokinetic modeling and clearance concept to drugs showing trans-porter-mediated distribution and clearance in humans. J Pharmacokinet Pharmacodyn 2010 Dec; 37(6): 575–90
Reesink HW, Zeuzem S, Weegink CJ, et al. Rapid decline of viral RNA in hepatitis C patients treated with VX-950: a phase Ib, placebo-controlled, randomized study. Gastroenterology 2006 Oct; 131: 997–1002
Forestier N, Larrey D, Marcellin P, et al. Antiviral activity of danoprevir (ITMN-191/RG7227) in combination with pegylated interferon α-2a and ribavirin in patients with hepatitis J Infect Dis 2011 Aug; 204: 601–8
Acknowledgements
All authors were employees at Hoffmann-La Roche Inc. at the time this work was completed. Micaela Reddy, Jennifer Fretland and Patrick Smith are current employees at Hoffmann-La Roche Inc. Yuan Chen, Joshua Haznedar and Steven Blotner are current employees at Roche/Genentech. Joshua Haznedar owns stock in Roche. All authors have contributed to the design and conduct of the study; collection, management, analysis and interpretation of the data; and preparation, review or approval of the manuscript. This study was supported by Hoffmann-La Roche, Basel, Switzerland. Support for third-party writing assistance for this manuscript was provided by Hoffmann-La Roche. The authors thank Drs Karin Jorga, Thierry Lave and Li Yu for providing valuable insight during the preparation of this manuscript. Additionally, we thank Dr Petra Goelzer for sharing her knowledge of the project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reddy, M.B., Chen, Y., Haznedar, J.Ö. et al. Impact of Low-Dose Ritonavir on Danoprevir Pharmacokinetics. Clin Pharmacokinet 51, 457–465 (2012). https://doi.org/10.2165/11599700-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11599700-000000000-00000