Abstract
Objectives: Lacosamide is an anti-epileptic drug, indicated as adjunctive therapy for patients with focal seizures with or without secondary generalization. This study aims to assess the cost effectiveness of standard antiepileptic drug therapy plus lacosamide 300 mg/day compared with standard therapy alone from the perspective of the Belgian healthcare payer.
Methods: The treatment pathway of a hypothetical cohort of 1000 patients over 2 years was simulated using a decision tree. Data about health state probabilities, seizure frequency and utility values were taken from lacosamide trials or from the literature. Effectiveness measures included the number of seizures avoided and the number of quality-adjusted life-years gained. Unit costs were taken from national references. Resource use was estimated by a panel of eight neurologists with extensive experience in epilepsy. The price year was 2008. Deterministic and probabilistic sensitivity analyses were conducted.
Results: Over a 24-month period, standard anti-epileptic drug therapy plus lacosamide led to a reduction of seven seizures, an increase of 0.038 qualityadjusted life-years and a cost decrease of ¬3619 per patient compared with standard therapy alone. Using a willingness to pay of ¬30 000 per qualityadjusted life-year, the net monetary benefit of standard anti-epileptic drug therapy plus lacosamide amounted to ¬4754. The probability of standard anti-epileptic drug therapy plus lacosamide being cost effective was 97.3%, 99.8%, 99.9% and 100% at 6, 12, 18 and 24 months, respectively.
Conclusion: In patients with difficult-to-treat epilepsy, standard anti-epileptic drug therapy plus lacosamide appears to be a cost-effective option in Belgium.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Epileptic seizures can be defined as the transient occurrence of signs and/or symptoms due to abnormal neuronal activity in the brain.[1] Focal epileptic seizures (also called partial-onset seizures) are seizures originating within networks limited to one hemisphere and either discretely localized or more widely distributed.[2] The prevalence of epilepsy varies between 4 and 8 cases per 1000 individuals in developed countries,[3] and partial seizures are the predominant type of epileptic seizures.[4]
Epileptic seizures are associated with significant morbidity, impaired quality of life (QoL) and mortality,[5] and are a primary driver of hospital admissions and healthcare costs.[6] A recent literature review reported an increased mortality risk for people with epilepsy as compared with the general population.[5] QoL associated with epileptic seizures is impaired as indicated by utility values ranging from 0.66 to 0.91 (on a scale of 0–1) in epileptic patients who do not achieve seizure freedom.[7–11] A bottom-up, prevalence-based, cost-of-illness study estimated the costs of epilepsy from a societal perspective in the 27 EU member countries, plus Iceland, Norway and Switzerland.[6] The estimated total cost of the disease in Europe was €13.8 billion in 2010, consisting of €6.5 billion of direct healthcare costs, €5.6 billion of indirect costs and €1.7 billion of direct non-medical costs. The total cost per patient amounted to €5221. A systematic review of cost-of-illness studies suggested that anti-epileptic drugs (AEDs) are becoming the main driver of direct healthcare costs of epilepsy.[12]
The management of epilepsy typically begins with monotherapy with an AED. If adequate trials of two tolerated, appropriately chosen and used AEDs fail to achieve sustained seizure freedom, treatment of refractory epilepsy will move to regimens consisting of two or more AEDs.[13] In epilepsy, seizure freedom is an important outcome as it is a determinant of QoL for epilepsy sufferers.[14] A study of 155 patients showed that the addition of a new AED to the treatment regimen of refractory adults allowed 28% of patients to achieve seizure freedom.[15] Nevertheless, as the objective of seizure freedom within refractory patients can be difficult, a more realistic goal in this patient population may be to achieve a significant reduction in seizure frequency.[16]
There is an unmet need for treatment options for patients with uncontrolled partial-onset epilepsy. Lacosamide is an AED, launched in 2008 in Europe, where it is indicated as adjunctive therapy for patients from 16 years of age suffering from focal epilepsy with or without secondary generalization. In order to gain reimbursement, an economic evaluation of lacosamide was requested by the National Institute for Health and Disability Insurance (i.e. the Belgian third-party payer). The aim of this study is to assess the cost effectiveness of standard AED therapy plus lacosamide compared with standard AED therapy alone in treating partial-onset seizures from the perspective of the Belgian healthcare payer.
Methods
Decision-Analytic Model
The treatment pathway of a hypothetical cohort of 1000 patients over 2 years was simulated using a decision tree. A modelling approach was preferred to a trial-based economic evaluation since data from clinical trials following patients over 2 years were not available at the time of this study and because of the limited number of head-to-head comparisons between AEDs. The decision tree was split into four phases of 6 months during which patients could become seizure free, experience a seizure reduction or withdraw due to non-response (figure 1). If patients in the normal treatment group withdrew due to non-response, patients were assumed to change treatments. Patients withdrawing in the lacosamide treatment group were assumed to continue on standard therapy as defined in the comparator arm.
Interventions
The efficacy and safety of lacosamide have been studied in three pivotal multicentre, double-blind, placebo-controlled trials (trials SP667, SP754 and SP755) in approximately 1300 adults with partial-onset seizures.[17–19] The intervention consisted of standard AED therapy plus lacosamide (Vimpat®; UCB Pharma, Brussels, Belgium) 300 mg/day. Although trial SP754[18] included a treatment arm consisting of standard AED therapy plus lacosamide 600 mg/day, this dose was not used in the economic evaluation as the 600 mg/day dose is not registered in Europe. As lacosamide has been approved as adjunctive therapy in partial-onset epilepsy, the comparator was standard AED therapy alone. AEDs included in the standard therapy arm were extracted from the ‘placebo’ arm of the two trials SP754 and SP755.[18,19] Given that trial SP667 enrolled some patients treated with one AED only,[17] this trial was not considered in our model of refractory patients who have uncontrolled epilepsy despite treatment with at least two AEDs. The most frequently used AEDs in the two trials were carbamazepine (23%), lamotrigine (22%), levetiracetam (19%), topiramate (17%) and valproate (19%). Therefore, standard therapy reflected average treatment rather than treatment with any specific drug. This approach was taken since it was not possible to include all possible treatment pathways with available AEDs as comparators in the model in a context where strategies to treat epilepsy should be individualized.[20] To account for the change in treatments of patients who have uncontrolled seizures on standard therapy, the percentages of most frequently used AEDs making up standard therapy changed over the course of the model, i.e. percentages were randomly switched to different drugs in subsequent 6-month phases of the decision-analytic model. This approach was chosen because, although market research indicates that these five AEDs are the most commonly prescribed for refractory patients in Belgium, no published studies assess switch sequences between these AEDs.
Health State Probabilities
The decision-analytic model used two health states: seizure reduction and withdrawal due to non-response. Response to treatment was defined as a reduction in seizure frequency of at least 50% as compared with the baseline seizure frequency. Patients could also withdraw due to lack of efficacy or adverse events. Although the pivotal trials showed that an increased proportion of patients treated with lacosamide were seizure free compared with patients treated with placebo,[18,19] the model used here did not consider the health state of being seizure free.[21] This was because the study population consisted of patients who had uncontrolled epilepsy despite previous treatment with at least two other AEDs and because the trial probabilities of being seizure free with lacosamide were small. Patients in the pivotal trials SP754 and SP755 also displayed a statistically significant reduction in seizure frequency when treated with lacosamide compared with patients treated with placebo (trial SP754: 400 mg/day, p = 0.0078; 600 mg/day, p = 0.0061; trial SP755: 200 mg/day, p = 0.0223; 400 mg/day, p = 0.0325). Trials SP754 and SP755 were used to estimate the probability of seizure reduction and the probability of withdrawal due to non-response by means of a pooled analysis (see table IA).[18,19] All patients who did not experience a seizure reduction of at least 50% were assumed to withdraw due to non-response.
These data allowed estimation of the probabilities of health states used in the first phase (0–6 months) of the model (see table IB). The probability of seizure reduction of 0.194 with standard AED therapy was 47% lower than the probability of 0.368 with standard AED therapy plus lacosamide (p < 0.0001). In the subsequent phases, patients who remained on their treatment, either standard AED therapy plus lacosamide or standard AED therapy alone, were assumed to have the same probabilities as in the previous phase. This assumption was supported by data from open-label extension studies of the pivotal trials.[22]
Seizure Frequency
The baseline number of seizures was based on the mean number of seizures per 6 months experienced by all patients in the two pivotal trials at baseline.[18,19] A conservative approach was undertaken by considering the baseline seizure frequency of 42.4 (± 163.8) seizures per 6 months for standard AED therapy plus lacosamide and 31.7 (± 73.8) seizures for standard AED therapy alone.
Patients in the seizure reduction health state will be within the range of a 50–100% reduction in seizure frequency. Given that a 75% reduction in seizure frequency is the median between these two limits, seizure frequency in the seizure reduction health state was assumed to be 25% of the baseline seizure frequency value. Patients who withdrew due to non-response were assumed to have the same seizure frequency as at baseline.
Utility Values
The decision-analytic model incorporated health-related QoL through the use of utility values. This enables the estimation of quality-adjusted life-years (QALYs) associated with different treatment strategies.
Utility values have not been directly estimated for the patients included in the pivotal trials. Thus, we conducted a systematic review of the literature and identified five publications reporting utility values for people living with epilepsy.[7–11] Utility values were derived from an Italian study by Messori et al.,[10] as the authors used a validated method to derive utility values and the utility values were reported in such a way that they could easily be matched to the efficacy data from the lacosamide trials. Also, these Italian utility values appear to be applicable to our economic evaluation of adjunctive therapy with lacosamide for patients with refractory focal epilepsy given that the study population in Messori et al.[10] was similar to the population from the lacosamide trials. Messori et al.[10] conducted a prospective study in which QoL data were collected from consecutive patients who had received a diagnosis of uncontrolled epilepsy and were referred to an outpatient clinic between February 1997 and July 1997. Patients were interviewed by two neurologists, using the time trade-off technique to quantify the QoL level of the patient. A total of 81 consecutive patients (45 males, median age of 32 years) were included in this study. Patients received either monotherapy (n = 4) or combination therapy (n = 77) with AEDs. Table IC shows the health states and utility values in the study by Messori et al.[10] and in our economic evaluation.
Outcomes
The analysis considered the number of seizures avoided and the number of QALYs gained because AED treatment primarily impacts seizure frequency and health-related QoL. The model did not take into account adverse events due to the low incidence rates with AED treatment.[11] Also, the model did not consider mortality. This is because the primary objective of treatment in this population of uncontrolled patients is seizure freedom or seizure reduction,[16] and because the pivotal trials did not report mortality rates. Furthermore, other economic evaluations of AED therapy did not consider mortality.[11]
Resource Use and Costs
Resource use related to visits to the general practitioner and outpatient department, as well as hospitalization and emergency department admissions (see table IIA). In the absence of published data on Belgian resource use associated with partial-onset seizures, resource use was estimated by a Belgian panel of eight experienced neurologists using the Delphi technique. In Belgium, economic evaluations conducted from the healthcare payer perspective need to include third-party reimbursement and patient co-payment.[24] Unit costs were derived from national references.[23] The price year was 2008.
Resource use/costs per 6 months were calculated by multiplying the number of seizures per 6 months by the resource use/costs per seizure. It was assumed that all patients had general care management. The costs of general care management per 6 months were calculated as the sum of the proportions of patients in each health state multiplied by the unit cost of general care management. General care management costs were included with a view to providing a correct estimate of total costs of standard AED therapy plus lacosamide and of standard AED therapy alone, although these costs do not influence the incremental cost-effectiveness ratio as they equally apply to both treatment arms. If seizure control was not achieved on current AEDs, a change of treatment was deemed necessary and a new regimen was started.
The daily cost for each drug was calculated based on the defined daily dose and the average cost per milligram for that drug computed based on the different strengths and pack sizes available. The cost per 6 months of each drug was derived by multiplying the daily cost by 182 days (see table IIB).
The costs per 6 months of standard AED therapy plus lacosamide and standard AED therapy alone during the four phases of the decision-analytic model are presented in table IIC. This cost is calculated by multiplying the cost per 6 months of each drug by the percentage of the various drugs included in each treatment arm in each phase.
Time Horizon
The time horizon of the model was 2 years; a reasonable time point to catch any differences in consequences and costs of the interventions given the data available for lacosamide and other AEDs, as well as the natural history of epilepsy. In accordance with Belgian guidelines for economic evaluations,[24] future costs were discounted at a rate of 3% and future consequences at a rate of 1.5%.
Base Case Analysis
The incremental cost-effectiveness ratios (ICERs) were calculated for the base case analysis using the following formula: ICER = (C1 — C0)/(E1 — E0), where C1 is the cost of standard AED therapy plus lacosamide; C0 is the cost of standard AED therapy alone and E1 and E0 are respective consequences of intervention and comparator. Depending on the effectiveness measure used, ICERs referred to either the additional cost per seizure avoided or the additional cost per QALY gained. Standard AED therapy plus lacosamide ‘dominated’ standard AED therapy alone when it was both less expensive and more effective.
Sensitivity Analysis
To test the robustness of results to changes in parameter values, one-way deterministic sensitivity analyses were conducted by means of Tornado analyses. Parameter values were varied by ±10%, 20% and 30% from their base value where upper and lower bound permitted. Tornado diagrams were presented according to the net monetary benefit approach. This approach assigns a monetary value to the incremental benefit achieved. The monetary value represents the maximum amount that society is willing to pay for the incremental benefit. In our analysis, the commonly used value for willingness to pay of €30 000 per QALY was used to calculate the net monetary benefit as follows: net monetary benefit = willingness to pay (€30 000/QALY) * ΔE-ΔC, where ΔC is the incremental cost and ΔE is the incremental effectiveness of standard AED therapy plus lacosamide as compared with standard AED therapy alone.
A probabilistic sensitivity analysis was performed based on a 1000-iteration Monte Carlo simulation. This simulation explored the variability of cost-effectiveness results when key input parameters independently change according to pre-assigned probability distributions. Those probability distributions were assigned to key input parameters that best reflected the uncertainty in each parameter and that were consistent with logical bounds on parameter values (see table III).[25] Proportions and probabilities were assumed to follow β distributions, which are constrained on a 0–1 range. γ distributions were assigned to the number of healthcare resource events and to drug doses. Utilities were assumed to have β distributions, with ranges based on literature values.[7–11] For each of the 1000 iterations, the simulation drew input parameters at random from their statistical distributions and calculated cost and effectiveness pairs. At the end of the 1000 iterations, the joint statistical distribution for costs and effectiveness was represented as a cloud of points on the cost-effectiveness plane.
Results
Base Case Analysis
Table IV presents the results of the base case analysis at different time points. Standard AED therapy plus lacosamide 300 mg/day was found to be more effective that standard AED therapy alone in treating patients with partial-onset seizures uncontrolled with at least two AEDs. Treatment with standard AED therapy plus lacosamide was associated with fewer seizures, more QALYs and lower costs than standard AED therapy alone, irrespective of the time horizon. Over a period of 24 months, treatment with standard AED therapy plus lacosamide led to a reduction of seven seizures, an increase of 0.038 QALYs and a cost decrease of €3619 per patient as compared with standard AED therapy alone. Using a willingness to pay of €30 000 per QALY, the net monetary benefit of standard AED therapy plus lacosamide at 24 months amounted to €4754.
Sensitivity Analysis
The Tornado diagram in figure 2 presents the net monetary benefit of standard AED therapy plus lacosamide at 24 months when input parameters were varied by ±30% from their base case values. As seen in figure 2, the value of standard AED therapy plus lacosamide was most sensitive to changes in three parameters: seizure frequency, the probability of withdrawal due to lack of efficacy or adverse event, and the percentage decrease in the probability of seizure reduction of the comparator (i.e. standard AED therapy vs standard AED therapy plus lacosamide). The results were also sensitive to changes in the utility values associated with the health states, and the inpatient resource use associated with epilepsy management.
The intervention consisted of standard AED therapy plus lacosamide 300 mg/day. The dose of 300 mg/day was used in the economic evaluation as this corresponds with the defined daily dose. However, health state probability and seizure frequency data were derived from a pooled analysis of trial data on lacosamide 400 mg/day. When the maximum registered dose of 400 mg/day was used in a one-way sensitivity analysis, the higher drug acquisition costs of lacosamide translated into a lower cost advantage of standard AED therapy plus lacosamide as compared with standard AED therapy alone. Nevertheless, standard AED therapy plus lacosamide still dominated standard AED therapy alone (table V).
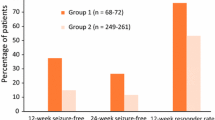
Probabilistic sensitivity analyses were carried out as incremental cost-effectiveness results expressed as cost per QALY gained. Figure 3 shows the scatter plot of 1000 ICER results comparing standard AED therapy plus lacosamide with standard AED therapy alone at 24 months. Based on cost-effectiveness acceptability, should decision makers be willing to pay a maximum amount of, for example, €30 000 per QALY, the results indicate that the probability of standard AED therapy plus lacosamide being cost effective is 97.3% at 6 months, 99.8% at 12 months, 99.9% at 18 months and 100% at 24 months.
Discussion
This economic evaluation showed that standard AED therapy plus lacosamide dominated standard AED therapy alone under the two effectiveness measures considered (seizures avoided and QALYs) and under the four time points considered. Treatment with standard AED therapy plus lacosamide was associated with fewer seizures, more QALYs and lower costs than standard AED therapy alone, irrespective of the time horizon. Thus, standard AED therapy plus lacosamide improved health outcomes and generated overall savings to the Belgian healthcare payer. The deterministic and probabilistic sensitivity analyses demonstrated the robustness of results. Standard AED therapy plus lacosamide had a probability of being cost effective of at least 97% depending on the time horizon.
The effect in the comparator arm was modelled to be similar to the effect of the placebo arm in the lacosamide trials. In real life, these patients with uncontrolled epilepsy would most likely either continue on their existing regimen or switch to a different AED combination. Ideally, the analysis would compare the effect on lacosamide with the weighted average effect for these two strategies as they occur in real life. However, a lack of relevant data did not permit this. First, for the proportion of patients who in real life would continue with their existing regime, the modelled placebo effect is most likely to be an overestimation. Indeed, the placebo effect is based on the study patients’ belief that they receive some form of active treatment, whereas patients continuing on an existing regimen would not be expected to experience any further improvement in seizure reduction. Second, for the patients who in real life would change to another AED combination, it is likely that they would experience some further improvement. How large that effect would be relative to the placebo effect included in the model is impossible to ascertain. As demonstrated by the Tornado analysis, although a decrease in the probability of seizure reduction of the comparator versus standard AED therapy plus lacosamide did affect results, the net monetary benefit remained positive. In summary, it seems reasonable to conclude that the placebo effect included in the comparator arm was an acceptable assumption given the lack of real-life comparative data.
The comparator in the economic evaluation reflected average treatment rather than treatment with any specific drug. Average treatment consisted of the most frequently used AEDs in the trials SP754 and SP755.[18,19] It was not possible to compare with an individual drug as the choice for a specific AED in refractory patients depends on multiple factors and there are numerous possible treatment pathways with available AEDs.[20]
The model reflected the findings that lacosamide treatment improves seizure control in patients with uncontrolled epilepsy. The probability of seizure reduction with lacosamide was derived from the pivotal trial results. Furthermore, it was assumed that all patients who did not achieve a 50% or higher reduction in seizure frequency would withdraw from the existing treatment. In real life, many patients experiencing lower reductions would choose to continue on their existing therapy, when they have tried one or more AEDs previously. As a result, the model overestimated the probability of withdrawal due to a lack of response and, thus, underestimated the effectiveness gain with standard AED therapy plus lacosamide. The potential overestimation of withdrawal due to lack of response reduces drug costs of lacosamide, but may increase overall healthcare costs as these patients were assumed to change treatments. Finally, the simplifying assumption was made that patients who withdraw due to non-response or adverse events have the same seizure frequency as at baseline, and thus our decision-analytic model did not allow for changes in seizure frequency following withdrawal.
The two effectiveness measures considered were the number of seizures avoided and the number of QALYs gained because AED treatment primarily impacts seizure frequency and health-related QoL. The model did not take into account adverse events due to the low incidence rates of adverse events in AED treatment.[11] Even though the rate of adverse events may be significant with older AEDs, the omission of adverse events potentially contributed to an underestimation of the cost effectiveness of standard AED therapy plus lacosamide.
As this study was carried out for the purpose of gaining reimbursement from the National Institute for Health and Disability Insurance, the economic evaluation was based on two pivotal trials of lacosamide and, thus, explored the cost effectiveness of lacosamide under trial conditions. This approach benefits from high validity, but implies that our results may not reflect real-life clinical practice or take account of factors such as patient adherence to therapy. Nevertheless, recent post-marketing surveillance studies have confirmed the efficacy and safety profile of lacosamide as observed in the pivotal trials.[26]
An additional data collection exercise was undertaken to collect resource use estimates specific to the Belgian context by eliciting values from a Belgian expert panel. The approved indication for adjunctive therapy with lacosamide is partial-onset seizures with or without secondary generalization. As such, there is considerable variation in how partial-onset seizures present clinically from patient to patient. The model included an average estimate of resources associated with seizures. The experts’ assessment of average resource use per seizure within the patient population was therefore associated with uncertainty. A more detailed evaluation of resource use associated with individual patients would have been beneficial, but this approach was not feasible due to the lack of data regarding the treatment impact on the various types of seizures. The resource estimates were tested extensively in sensitivity analyses and the results were robust.
Costs of AED therapy were calculated based on the defined daily dose. The defined daily dose may not correspond with actual doses of AEDs administered in real-life clinical practice. However, the Tornado analysis demonstrated that the dose of AEDs had little impact on the net monetary benefit of standard AED therapy plus lacosamide.
Indirect costs of productivity loss were not included in the model as this economic evaluation was carried out from the healthcare payer perspective. A major seizure often results in absence from work; therefore, inclusion of lost patient time needs to be considered. Given that previous research has shown that indirect costs are one of the major components of the total costs of epilepsy,[6] indirect costs are likely to be a key driver of the cost effectiveness of standard AED therapy plus lacosamide from a societal perspective. Data on a treatment’s impact on indirect costs were scarce and very uncertain. However, major seizures were assumed to appear more frequently in the comparator arm. Therefore, the omission of indirect costs potentially contributed to an underestimation of the cost effectiveness of standard AED therapy plus lacosamide.
Conclusions
This economic evaluation indicated that for patients who fail to respond adequately to other treatment alternatives, standard AED therapy plus lacosamide constitutes a cost-effective option in Belgium. Given the complexity of epilepsy diagnosis and management, physicians should be presented with a wide choice of therapeutic options in order to tailor AED treatment to each patient.
References
Fisher RS, van Emde Boas W, Blume W, et al. Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia 2005; 46: 470–2
Berg AT, Berkovic SF, Brodie MJ, et al. Revised terminology and concepts for organization of seizures and epilepsies: report of the ILAE Commission on Classification and Terminology, 2005–2009. Epilepsia 2010; 51: 676–85
Hauser W. Epilepsy: frequency, causes, and consequences. New York (NY): Demos Press, 1990
Kotsopoulos IA, van Merode T, Kessels FG, et al. Systematic review and meta-analysis of incidence studies of epilepsy and unprovoked seizures. Epilepsia 2002; 43(11): 1402–9
Hitiris N, Mohanraj R, Norrie J, et al. Mortality in epilepsy. Epilepsy Behav 2007; 10(3): 363–76
Gustavsson A, Svensson M, Jacobi F, et al. Cost of disorders of the brain in Europe 2010. Eur Neuropsychopharmacol 2011; 21: 718–79
King Jr JT, Sperling MR, Justice AC, et al. A cost-effectiveness analysis of anterior temporal lobectomy for intractable temporal lobe epilepsy. J Neurosurg 1997; 87(1): 20–8
Langfitt JT. Cost-effectiveness of anterotemporal lobectomy in medically intractable complex partial epilepsy. Epilepsia 1997; 38(2): 154–63
Maltoni S, Messori A. Lifetime cost-utility analysis of patients with refractory epilepsy treated with adjunctive topiramate therapy: cost-effectiveness in refractory epilepsy. Clin Drug Investig 2003; 23(4): 225–32
Messori A, Trippoli S, Becagli P, et al. Adjunctive lamotrigine therapy in patients with refractory seizures: a lifetime cost-utility analysis. Eur J Clin Pharmacol 1998; 53(6): 421–7
Wilby J, Kainth A, Hawkins N, et al. Clinical effectiveness, tolerability and cost-effectiveness of newer drugs for epilepsy in adults: a systematic review and economic evaluation. Health Technol Assess 2005; 9(15): 1–186
Strzelczyk A, Reese JP, Dodel R, et al. Cost of epilepsy: a systematic review. Pharmacoeconomics 2008; 26: 463–76
Kwan P, Arzimanoglou A, Berg AT, et al. Definition of drug resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia 2010; 51: 1069–77
Birbeck GL, Hays RD, Cui X, et al. Seizure reduction and quality of life improvements in people with epilepsy. Epilepsia 2002; 43(5): 535–8
Luciano AL, Shorvon SD. Results of treatment changes in patients with apparently drug-resistant chronic epilepsy. Ann Neurol 2007; 62: 375–81
Leppik I, Morrell M, Godfroid P, et al. Seizure-free days observed in randomized placebo-controlled add-on trials with levetiracetam in partial epilepsy. Epilepsia 2003; 44(10): 1350–2
Ben-Menachem E, Biton V, Jatuzis D, et al. Efficacy and safety of oral lacosamide as adjunctive therapy in adults with partial-onset seizures. Epilepsia 2007; 48(7): 1308–17
Chung S, Sperling MR, Biton V, et al. Lacosamide as adjunctive therapy for partial-onset seizures: a randomized controlled trial. Epilepsia 2010; 51(6): 958–67
Halász P, Kälviäinen R, Mazurkiewicz-Beldzińska M, et al. Adjunctive lacosamide for partial-onset seizures: efficacy and safety results from a randomized controlled trial. Epilepsia 2009; 50(3): 443–53
National Institute for Health and Clinical Excellence. Newer drugs for epilepsy in adults. London: National Institute for Health and Clinical Excellence, 2004
Schiller Y, Najjar Y. Quantifying the response to antiepileptic drugs: effect of past treatment history. Neurology 2008; 70(1): 54–65
Rosenfeld W, Rosenow F, Isojarvi J, et al. Long-term safety and tolerability of lacosamide for partial-onset seizures: an interim evaluation of patients exposed to lacosamide in double-blind and open-label trials. Epilepsia 2009; 50 Suppl. 11: 453
National Institute for Health and Disability Insurance. List of health care services. Brussels: National Institute for Health and Disability Insurance, 2010
Cleemput I, Van Wilder P, Vrijens F, et al. Guidelines for pharmaco-economic evaluations in Belgium. Brussels: Federaal Kenniscentrum voor de Gezondheidszorg, 2008
Briggs A. Handling uncertainty in economic evaluation and presenting the results. In: Drummond M, McGuire A, editors. Economic evaluation in health care: merging theory with practice. Oxford: Oxford University Press, 2001: 172–214
Wehner T, Bauer S, Hamer HM, et al. Six months of postmarketing experience with adjunctive lacosamide in patients with pharmacoresistant focal epilepsy at a tertiary epilepsy center in Germany. Epilepsy Behav 2009; 16: 423–5
Acknowledgements
The economic evaluation was requested by the National Institute for Health and Disability Insurance (i.e. the Belgian third-party payer), and was undertaken in collaboration with and paid for by UCB Pharma. LDN and PD are employees of UCB Pharma, the manufacturer of lacosamide. SS has no conflicts of interest that are relevant to this manuscript. LDN and PD were involved in the data collection. SS participated in the design, conduct and validation of the economic evaluation and wrote this manuscript. We acknowledge Maeva Germe for her contribution to computing the decision tree model. SS had final responsibility for the decision to submit for publication.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Simoens, S., De Naeyer, L. & Dedeken, P. Cost Effectiveness of Lacosamide in the Adjunctive Treatment of Patients with Refractory Focal Epilepsy in Belgium. CNS Drugs 26, 337–350 (2012). https://doi.org/10.2165/11599240-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11599240-000000000-00000