Abstract
Background: Pharmacists have an essential role in improving drug usage and preventing prescribing errors (PEs). PEs at the interface of care are common, sometimes leading to adverse drug events (ADEs). This was the first study to investigate, using a computerized search method, the number, types, severity, pharmacists’ impact on PEs and predictors of PEs in the context of electronic prescribing (e-prescribing) at hospital discharge.
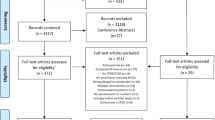
Method: This was a retrospective, observational, 4-week study, carried out in 2008 in the Medical and Elderly Care wards of a 904-bed teaching hospital in the northwest of England, operating an e-prescribing system at discharge. Details were obtained, using a systematic computerized search of the system, of medication orders either entered by doctors and discontinued by pharmacists or entered by pharmacists. Meetings were conducted within 5 days of data extraction with pharmacists doing their routine clinical work, who categorized the occurrence, type and severity of their interventions using a scale. An independent senior pharmacist retrospectively rated the severity and potential impact, and subjectively judged, based on experience, whether any error was a computer-related error (CRE). Discrepancies were resolved by multidisciplinary discussion. The Statistical Package for Social Sciences was used for descriptive data analysis. For the PE predictors, a multivariate logistic regression was performed using STATA® 7. Nine predictors were selected a priori from available prescribers’, patients’ and drug data.
Results: There were 7920 medication orders entered for 1038 patients (doctors entered 7712 orders; pharmacists entered 208 omitted orders). There were 675 (8.5% of 7920) interventions by pharmacists; 11 were not associated with PEs. Incidences of erroneous orders and patients with error were 8.0% (95% CI 7.4, 8.5 [n = 630/7920]) and 20.4% (95% CI 18.1, 22.9 [n = 212/1038]), respectively. The PE incidence was 8.4% (95% CI 7.8, 9.0 [n = 664/7920]). The top three medications associated with PEs were paracetamol (acetaminophen; 30 [4.8%]), salbutamol (albuterol; 28 [4.4%]) and omeprazole (25 [4.0%]). Pharmacists intercepted 524 (83.2%) erroneous orders without referring to doctors, and 70% of erroneous orders within 24 hours. Omission (31.0%), drug selection (29.4%) and dosage regimen (18.1%) error types accounted for >75% of PEs. There were 18 (2.9%) serious, 481 (76.3%) significant and 131 (20.8%) minor erroneous orders. Most erroneous orders (469 [74.4%]) were rated as of significant severity and significant impact of pharmacists on PEs. CREs (n = 279) accounted for 44.3% of erroneous orders. There was a significant difference in severity between CREs and non-CREs (χ2= 38.88; df=4; p<0.001), with CREs being less severe than non-CREs. Drugs with multiple oral formulations (odds ratio [OR] 2.1; 95% CI 1.25, 3.37; p = 0.004) and prescribing by junior doctors (OR 2.54; 95% CI 1.08, 5.99; p = 0.03) were significant predictors of PEs.
Conclusions: PEs commonly occur at hospital discharge, even with the use of an e-prescribing system. User and computer factors both appeared to contribute to the high error rate. The e-prescribing system facilitated the systematic extraction of data to investigate PEs in hospital practice. Pharmacists play an important role in rapidly documenting and preventing PEs before they reach and possibly harm patients. Pharmacists should understand CREs, so they complement, rather than duplicate, the e-prescribing system’s strengths.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Pharmacists have an essential role in improving drug usage and preventing prescribing errors (PEs).[1,2] It has been reported that not all PEs are intercepted by pharmacists’ interventions and, similarly, not all pharmacists’ interventions are in response to PEs.[3] The relationship between pharmacists’ interventions and PEs is poorly studied. PEs are very common in US[4,5] and UK[3,6] secondary care.[7] PEs at the interface of care, the point of hospital admission or discharge, are common and can lead to preventable adverse drug events (pADEs).[8] Errors attributable to prescribing make up the largest share of pADEs in hospitals.[9]
PEs occur at hospital discharge, during which patients’ medication orders require verification and clarification from multiple sources of information, including the best possible medication history, medications prescribed during the inpatient stage (newly prescribed, adjusted or discontinued), unchanged patient’s own medication, and the newly started medications at discharge.[10–13] PEs and ADEs after hospital discharge arise from insufficient medication reconciliation processes at discharge and inadequate information to patients regarding their pharmacotherapy.[14–18] Some studies[5,19–21] have focused on pharmacists’ interventions with PEs during or after hospital discharge of adults. However, none were specifically aimed at studying the rate, nature, potential severity and predictors of PEs in the context of electronic prescribing (e-prescribing) at hospital discharge. In addition, none of the studies investigated the relationship between pharmacists’ interventions and PEs at the care interface.
Information technology, in the form of e-prescribing systems, has been proposed to reduce PEs in hospitals.[22] Although they have many benefits, e-prescribing systems are not fully protected against PEs; they have even facilitated the introduction of new types of PEs.[2] Most of the evidence-based findings of the strengths and weaknesses of e-prescribing systems have emerged from the US,[23–26] where clinical practice and e-prescribing systems are different from the UK.[27] No previous study has investigated pharmacists’ interventions and PEs in the context of e-prescribing systems at hospital discharge using a computerized search method.
Studies have used a number of techniques and information sources to collect data for the identification of PEs, such as manual chart review, computerized search of electronic records, and trigger tool studies. Most PE studies have utilized paper-based records to detect and document error rate and types; moreover, data were manually collected, mostly by pharmacists, which may have been less efficient and more expensive[28] than a computerized search. Unsurprisingly, although these methods enjoy a number of advantages, all of them are inherently fraught with inaccuracies and systematic bias.[29]
The aim of this study was to characterize and investigate the number, types, severity and predictors of PEs in the context of an e-prescribing system at hospital discharge. Computer-related errors (CREs), high-risk medications, pharmacists’ impact on PEs, and the circumstances of independent pharmacists’ interventions were also investigated.
Methods
Setting and e-Prescribing System
The study hospital was a 904-bed teaching hospital, which cared for an average of 320000 people a year in the northwest of England. There were more than 400 doctors and 35 pharmacists working in the hospital. A comprehensive pharmaceutical service was provided between 9:00am and 5:00pm on weekdays.
An electronic patient record with an e-prescribing system (iSoft Clinical Manager™; iSoft plc, Manchester, UK) was installed in the hospital in 2000. At the time of the study, the e-prescribing system was enabled at the time of discharge only — inpatient prescribing was still paper-based. When the patient was discharged, the prescriber used the inpatient chart to select the required medication from the e-prescribing system’s drug catalogue and prepare the discharge prescription. The drug catalogue was accessed in a medicines ‘look-up’ list providing suggested default dosage regimens and formulations for most medications, which appeared upon typing the first letters of a medication’s approved name. Free-text could be entered by the prescriber if the medication or one of its characteristics did not exist in the look-up list. No further explicit clinical decision support was enabled in the system. Any pharmacist or doctor discontinuing a medication order had to select (from a pull-down menu) or type in (as free-text) a reason for discontinuation. Only one reason could be entered into the field for each discontinued medication order.
Each weekday the pharmacists routinely checked the discharge medication orders electronically prescribed by doctors and compared them with the inpatient paper-based drug chart to ensure that all orders were clear, legal, complete and clinically appropriate. Weekend prescriptions were checked by the dispensary pharmacist working on Saturdays and Sundays, supported by an on-call service. If any discrepancy, ambiguity or error existed in the discharge electronic order, the pharmacist might call the prescriber, discuss the matter and correct it (or let the prescriber correct it). Alternatively, if the pharmacist covered the ward on which the patient was located and had a complete picture about the patient’s condition, the pharmacist might change the prescription independently without consulting the prescriber.
Extraction of Data
Data were extracted from the electronic patient records using Microsoft Access® (Microsoft Access® 2003; Microsoft Corporation, Stateline, NV, USA) via SQL Server (Microsoft SQL Server, Microsoft Corporation, Redmond, WA, USA). Only medication orders prescribed by doctors and discontinued by pharmacists were included in the study. Patient characteristics (date of admission, date of discharge, age, sex, number of discharge medications and ward), medication order characteristics (drug name, strength, frequency, route and grade of prescriber) and any changes made in the subsequent discharge order (drug name, strength, frequency, route and person who made changes) stored in the system were manually collected on preset data entry forms by one of the authors (DAQ). The study was deemed service evaluation by a local Research Ethics Committee and formal review was not needed.
Study Design
This was a recently retrospective, observational, cross-sectional, process-based[30] study. For practical reasons, the busiest wards (Medical and Care of the Elderly) were chosen. PEs were identified either during routine drug chart review (paper or electronic) or dispensing of a medication. Therefore, PEs could be intercepted and addressed with or without the knowledge of the prescriber, to avoid patient harm.
All discharge medication orders, discontinued by pharmacists and generated from the study wards by doctors, were included in the study, during 4 purposively selected weeks: the second week of May, first week of June, and first and fourth weeks of October 2008. A week was chosen because it included any potential errors occurring both in discharge and weekend leave medication orders. At the time of the study, junior doctors changed their rotation (within and outside the hospital) in February and August every year; hence, the authors selected 3 months in which doctors will presumably have had time to settle into the hospital’s context and e-prescribing system.
To investigate the potential predictors of PEs, a retrospective case-control study was conducted in parallel with the observational study.
Definitions
Medication Order
A medication order was defined as any prescribed medication along with its characteristics (strength, unit of measurement, frequency, dosage form, route and administration information) intended to be administered to or by a patient after discharge from hospital.
High-Risk Medication
A high-risk medication was defined as a medication that, if involved in an erroneous medication order, carried a greater risk of significant harm or death.[31] High-risk medications were compiled from the Institute for Safer Medication Practices’ high-alert medication list,[32] as well as from articles that reported on high-risk medications (figure 1).[1,31,33]
Prescribing Error (PE) Types and Severity
Dean and colleagues’[35] definition of PE was adopted: “a clinically meaningful prescribing error occurs when, as a result of a prescribing decision or prescription [ordering] process, there is an unintentional significant (a) reduction in the probability of treatment being timely and effective or (b) increase in the risk of harm when compared with generally accepted practice.” According to this definition, prescribing without taking into account the patient’s clinical status, failure to include essential information and errors in transcribing (i.e. from inpatient chart to electronic discharge prescription) are all considered PEs. However, failure to adhere to standards, such as prescribing guidelines or the drug’s product licence, was not considered a PE where these reflected accepted practice. The British National Formulary[34] (BNF) was used as a reference for the use of medicines. All errors in regular, when-required (prn) and once-only medications were included. One of the authors (DAQ) classified all PE types. One erroneous medication order might have more than one PE type. PE types in the context of e-prescribing at discharge are shown in figure 2. Severity of error was classified using the scale of Overhage and Lukes,[36] with some modifications (table I). Control medication orders were those where no PEs were identified by the pharmacists.
Instrument for characterizing pharmacists’ clinical interventions (adapted from Overhage and Lukes[36])
Types of Incidence
Six types of incidence were calculated. To calculate the incidence of PEs, all errors identified during the study weeks were divided by all medication orders made (and those orders that should have been made but were omitted in error) during the study weeks. All errors were included when more than one error existed in the same order. The incidence of patients with error was calculated by dividing the number of patients prescribed an erroneous order by all discharged patients on the day of data collection. The incidence of erroneous orders was the number of medication orders with an error divided by the total number of orders made plus those omitted in error. The incidence of omission errors (number of omission errors divided by orders made), incidence of commission errors (number of commission errors [i.e. PEs without omission errors] divided by orders made) and incidence of PEs relative to the opportunities for error (PE incidence divided by four) were also calculated. Each correctly indicated medication order was judged to have four opportunities for error (drug name, dose, frequency and formulation).
Pharmacists’ Clinical Intervention
This is defined as “any reactive (in response to an erroneous medication order) activity undertaken to suggest changes in one medication order that might involve contacting medical staff.” PI Clinical interventions were classified as those associated or not associated with PEs.
Junior Doctors
They were defined as doctors who were doing their first 2 years of postgraduate training in hospital, termed foundation years 1 and 2. Identification and Classification of Pharmacists’ Interventions
Identification and Classification of Pharmacists’ Interventions
All pharmacists’ interventions were identified and validated by several members of the research team (the authors and the previously trained 29 pharmacists working in the hospital). Validation happened when the pharmacists utilized their ‘insider’ knowledge and experience, which is part of the pharmacist’s routine clinical role, to decide initially upon the occurrence and severity of any PE recorded. Meetings among the research team members were held as soon as possible (within 1 week) after each intervention, to finalize judgements about PE occurrence and severity. One of the authors (DAQ) independently rated the severity and discussed any discrepancy with the pharmacist who made the intervention until reaching agreement. An open-ended question was posed to pharmacists as to whether they intervened independently or after having spoken to doctors. Doctors were unaware of the study in order to avoid changes in behaviour.
Severity of Errors and Impact of Pharmacists’ Interventions
When a medication order had more than one PE, the most severe error was considered in the severity, impact and CRE rating. Following the rating performed by the research team, a senior clinical pharmacist (LH), independent of the research team, retrospectively rated the severity and potential impact of PEs using a published scale.[36] The senior pharmacist was blinded as to whether interventions were pharmacist-led in order to minimize any opportunity for rating bias. Any discrepancy in rating between the senior pharmacist and the research team was resolved by discussion and agreement between LH and one of the authors (DAQ).
Computer-Related Error
Any error was subjectively classified as a CRE when it was more likely to have happened because of the presence of the e-prescribing system and would have been less likely to happen had the traditional handwritten prescribing been in place. The independent pharmacist and one of the authors (DAQ) independently judged whether any error was a CRE.
Data Analysis
Pharmacists’ Interventions
The statistical package SPSS® v.15 for Windows (SPSS Inc., Chicago, IL, USA) was used for this analysis. Nominal data were compared using the χ2 test and continuous data by the unpaired t-test; 95% confidence intervals (CI) were calculated for parametric differences. An interrater reliability analysis using the weighted kappa (k) statistic was performed to determine consistency between raters of severity, pharmacist’s impact and CREs. Values of kappa from 0.40 to 0.59 were considered moderate, 0.60 to 0.79 substantial, and 0.80 outstanding. For the open-ended question about independent pharmacists’ interventions, the conversation was transcribed verbatim, coded and grouped into emerging themes.
PE Predictors
To investigate potential PE predictors, a retrospective, case-control, 4-week study was conducted. For a minimum detectable odds ratio (OR) ≥1.2, p=0.05 and power = 0.8, a randomly selected total number of sample size required (assuming a population of 10% cases and 90% control) was 2624 medication orders, which were randomly drawn from medication orders, stratified by study week. The authors purposively selected 5% (n=30 orders per week) of the controls (i.e. non-erroneous orders on which pharmacists did not intervene) to confirm that PEs did not exist.
A priori potential predictors of PE compiled from the literature and selected based on the available information from the electronic system were used as independent variables. These were grouped into:
-
1.
Prescriber characteristics: doctor’s grade, specialty and number of discharged patients prescribed for during the day of data collection (as a surrogate for workload).
-
2.
Patient characteristics: age, sex, length of stay and number of co-prescribed drugs.
-
3.
Drug characteristics: dosage form and BNF therapeutic category.
A multivariate logistic regression was performed based on a forced entry method using Stata® 7 (Stata Corp., College Station, TX, USA). Patients were clustered by the patient ID number. ORs, significance levels and 95% CIs were calculated.
Results
Overview of the Study Data
Doctors entered 7712 electronic discharge medication orders for 1038 patients (540 females, 498 males) on the study wards. There was no statistically significant difference between the numbers of erroneous or accurate orders among the 4 study weeks; hence, the data were combined. Pharmacists entered 208 omitted medication orders; therefore, in total there were 7920 medication orders entered by doctors and pharmacists during the study period. Demographics of patients associated with one or more PEs are shown in table II.
Pharmacists’ Interventions and PEs
There were 675 pharmacists’ interventions recorded in the e-prescribing system; 11 were not associated with PEs. There were 630 erroneous medication orders, responsible for 664 PEs, for 212 patients; hence, the incidence of PEs was 8.4% (95% CI 7.8, 9.0) [table III].
British National Formulary (BNF)[34] classification of the erroneous medication orders
Erroneous Medication Orders and PEs per Patient
During the study period, pharmacists intercepted 630 erroneous medication orders in the e-prescribing system for 212 patients; hence, there were 3.0 erroneous orders per patient for all patients with error. There were 664 PEs detected for the same patients, with 3.1 PEs per patient for all patients with error.
Specialities and Therapeutic Categories of Erroneous Medication Orders
Most erroneous medication orders were prescribed on the General Medicine (139 [22.0%]), Cardiology (113 [17.9%]) and Elderly Care (101 [16.0%]) wards. Eighty-one (12.9%) erroneous orders were for medications with only one oral formulation, 428 (67.9%) had multiple oral formulations and 69 (11.0%) orders were for inhalation formulations. Table IV classifies the erroneous orders according to the BNF therapeutic categories. A closer look at the BNF sub-therapeutic categories showed that antihypertensive classes had the largest share (94 [14.9%]), followed by analgesics and antirheumatics (87 [13.8%]), single and combined inhalation bronchodilators (62 [9.8%]), and antibacterials and antifungals (39 [6.2%]). The most frequently recorded individual medications associated with an error were paracetamol (acetaminophen; 30 [4.8%]), salbutamol (albuterol; 28 [4.4%]), omeprazole (25 [4.0%]), aspirin (21 [3.3%]), codeine (18 [2.9%]), Seretide® (salmeterol/fluticasone propionate; 15 [2.4%]), senna (14 [2.2%]) and prednisolone (13 [2.1%]). Of the total prescribed items (n = 7920) during the study period, paracetamol had 9.0% (713), salbutamol 1.6% (127), omeprazole 2.6% (206), aspirin 3.6% (285), codeine 4.5% (356), Seretide® 1.4% (111), senna 2.5% (198) and prednisolone 1.5% (119).
PE Types
The ratio between commission (n = 456) and omission errors (n = 208) was 2.2:1.0. Unintentional omission, selection of drug and dosage regimen error types accounted for more than three-quarters of PEs recorded (table V).
PE Severity and Impact Ratings
Kappa statistics showed substantial agreement between raters (range 0.70–0.72). There were 18 (2.9%) serious, 481 (76.3%) significant and 131 (20.8%) minor erroneous orders. Most interventions on erroneous orders (506 [80.3%]) were rated as of significant impact. Around three-quarters (469 [74.4%]) of the corrected erroneous orders were rated as C3 (significant severity with significant impact on pharmacists) and 95 (15.1%) as D4 (minor severity with somewhat significant impact on pharmacists).
Severity of the errors appeared to differ according to the error types (table VI). There was a statistically significant difference between these error types versus their severity rating (χ2 = 388.97; df= 10; p<0.001). Only the unintentional omission, drug selection and dosage regimen error types were rated as serious. Examples of serious PEs detected are shown in table VII.
Computer-Related Errors (CREs)
There were 279 (44.3%) erroneous orders rated as CREs. Erroneous orders were rated as serious in 7 (2.5%) and significant in 183 (65.6%) of CREs detected, in comparison with 11 serious (3.1%) and 288 (82.1%) significant erroneous orders not related to the computer system. There was a statistically significant difference in severity between CREs and those not related to the computer system χ2=38.88; df<4; p<0.001), with CREs being less severe than non-CREs. Table VIII lists some examples of whether PE types were computer related (CRE) or not. Clinical examples of PEs and their interpretation are shown in table IX.
Characteristics of Pharmacists’ Interventions
Pharmacists’ interventions were performed independently (i.e. without consulting doctors) in 524 (83.2%) erroneous medication orders. The elapsed time to make interventions ranged between 0.05 and 552 hours (median 6 hours, SD 116.3). Pharmacists intervened upon 70% (441) of erroneous orders within 24 hours.
Erroneous High-Risk Medication Orders
There were 81 erroneous high-risk medication orders for 62 patients; this accounted for 12.9% of the erroneous orders (n = 630). These high-risk orders were associated with 86 PEs; in other words, 13.0% of total PEs detected (n = 664). The most frequent (top ten) high-risk medications were codeine (18 [22.2%]), morphine (7 [8.6%]), doxazosin (6 [7.4%]), amitriptyline (5 [6.2%]), citalopram (5 [6.2%]), oxycodone (4 [4.9%]), warfarin (4 [4.9%]), tramadol (4 [4.9%]), insulin (3 [3.7%]) and digoxin (3 [3.7%]). The severity of five (6.2%) medication orders was rated as serious, 68 (84.0%) significant and eight (9.8%) minor. There was a statistically significant difference in CRE occurrence between high-risk medications and non-high-risk medications (χ2 = 11.073; df=2; p=0.004), where the proportion of high-risk medications was higher in the non-CREs (16.86%) than CREs (7.89%).
Predictors of PEs
None of the sample of control orders was associated with PEs and they were judged to be valid controls. Demographics of cases and controls are shown in table X.
Table XI gives information about the contribution of the predictor variables. Only two predictors (multiple oral formulations and junior doctor) contributed significantly to the predictive ability of the model.
Circumstances Where Pharmacists Independently Changed Erroneous Medication Orders
Changes to erroneous medication orders were done independently by pharmacists if they had access to patients’ clinical data at the time of decision making, and had sufficient time to check and correct PEs.
“It depends on where you’re based, so I would usually do all my TTOs [discharge medication orders, i.e. to take out] on the ward in front of the patient. The ward round’s just gone on, so I would normally be quite up- to- date with where [the medical team are] up to.” Ph1
Pharmacists would independently intervene if they had a good relationship with the prescriber. Pharmacists noted that they would not bother doctors with trivial mistakes, which at the same time could cause problems in a patient’s treatment plan. Pharmacists also discussed some characteristics of the ‘minor’ erroneous medication orders that they would change independently. For example, if a medication was not relevant to the patient’s reason for admission or any illness they had in their admission, pharmacists would change the medication themselves. Interventions would also be done independently if changes in an ‘erroneous’ medication order did not adversely affect a patient’s blood results.
“I’ll change it independently if it’s minor and less problematic, for example, if it’s a PRN, Beconase® nasal spray they only use it in the summer, or any drug for symptomatic relief, or not relevant to their reason for admission.” Ph10
On the other hand, the majority of pharmacists claimed that wrong dosage, contraindicated therapy, starting new medication at discharge and serious health conditions were all reasons why they would contact the prescriber before they would do any clinical intervention.
“Definitely it depends on how clear I am and what’s going on. It depends on how serious and how potentially problematic the medication is. Something like aspirin, warfarin or an antihypertensive, I would not just say, oh it’s obvious. I would check it more than something like an inhaler or something topical. So it depends on the reason for admission, the indication for that drug and the drug itself.” Ph4
Discussion
This was the first study to investigate pharmacists’ interventions and PEs through a systematic computerized search followed by structured meetings held within 1 week with the pharmacists who made the clinical interventions. This method does not replace other identification methods, but could provide a technique that is relatively consistent, objective, efficient and inexpensive.[29] This study employed a ‘standard of reference’, i.e. the reports given by pharmacists making clinical interventions on erroneous medication orders. One of the authors conducted the entire data extraction and meetings, which provided consistency of data collection and investigation throughout the study. This approach was deemed appropriate, taking into account its validity, efficiency and feasibility relative to the traditional manual chart review. [37]
Study Limitations
The study has three limitations. First, generalizability of the results from a single teaching hospital in the northwest of England, from Medical and Elderly Care wards, with one version of e-prescribing system at one point in time, is limited.
Second, the incidence of clinical interventions and PEs might have been underestimated since no independent check (by, for example, an external researcher) of all doctors’ medication orders was performed; a previous study[38] showed that more than one-third of the errors were revealed by the principal investigator following an additional check.
Finally, the substantial agreement between raters could have been different had a doctor taken part in the rating. A study[1] reported that an internal medicine specialist rated the severity and impact of pharmaceutical care interventions lower than the hospital pharmacist. In addition, albeit minimal, the hindsight bias might still have had its effect to construct seemingly reasonable justifications for the raters’ conclusions. However, the problem of multiple pharmacists rating PE severity differently had minimal effect on the overall rating since one person prospectively met with the pharmacists and resolved any discrepancy.
Incidence, Types and Severity of PEs
The PE incidence in this study was at least twice as high as the PE incidence (or prevalence) in other studies. [38–41] The ‘mandatory’ documentation of the reason for any medication discontinuation in the e-prescribing system as well as the computerized data collection method might have facilitated the emergence of this high error rate. Furthermore, the discharge stage may have had more opportunities for error than the inpatient stage.[8] As with all other methods, the PE incidence calculated here could not reflect the ‘true’ overall PE rate. The incidences reflected only the recorded clinical interventions made by pharmacists. Errors detected and corrected by other healthcare professionals (e.g. doctors and nurses) were not investigated in this study, which constitute part of the overall PE rate. Moreover, errors that were not recorded in the e-prescribing system (e.g. verbal consultation by pharmacists) were not included in the study.
Whichever type of incidence is used to explain the frequency of PEs, the equation of calculation should be explicitly stated, along with consistent definitions and methods, to help researchers confidently perform comparisons and draw meaningful conclusions. The authors argue that choosing ‘opportunities for error’ as the denominator when calculating PE incidence would give a more meaningful ratio than when choosing the total number of medication orders (made plus omitted) as a denominator. In addition, having separate incidences for commission and omission errors, with a common denominator being the number of orders made in the study period, would logically relate each type of error to the total number of orders prescribed by doctors only, rather than including omitted orders prescribed by pharmacists as well.
Anton et al.[42] argued, using the number of e-prescribing system’s warning messages generated per prescription, that doctors’ prescribing improves with time as they become more experienced with the e-prescribing system. The lack of difference among PE rates between weeks in this study, however, contradicts their finding. Future reearch is required to explore the reasons why different grades of doctors make PEs in the context of an e-prescribing system both quantitatively and qualitatively.
Unintentional omission of medication orders was the largest type of PEs detected, followed by drug selection error and then dosage regimen errors. This was not consistent with UK studies conducted during the inpatient stage where dosage regimen error ranked the first type.[38,41] Collecting data about electronic, rather than paper-based, prescriptions and about discharge prescriptions only, might have caused this difference in PE types. [38,41] A recent review[26] of the evidence of the impact of e-prescribing systems on medication errors has found that the use of e-prescribing systems was associated with a 66% reduction in total PEs in adults. It showed that the rate of prescribing a wrong drug did not decrease after the introduction of an e-prescribing system; moreover, four studies of seven did not show significant changes in wrong dose prescribing. In conclusion, this shows that a considerable risk for PEs and ADEs still exists, which shows the importance of involving clinical pharmacy services in a multidisciplinary intervention strategy.
The types and frequency of intercepted medication classes in this study were consistent with that shown in a meta-analysis on pADEs.[43] Interestingly, studies have emphasized that the use of the identified medication classes has been a frequent cause of hospital admission, [44,45] or ADEs following discharge.[46] In this study, certain commonly prescribed medication classes were more likely to be associated with PEs, in particular analgesics, bronchodilators and aspirin. Therefore, these PE-associated medications (especially the high-risk medications) are good targets to improve an e-prescribing system’s decision support or doctor education about good prescribing practice.
This study used a practical, reliable and comprehensive method[36] for assessing PE severity and pharmacists’ intervention impact. The distribution of severity rating percentages in this study was closely consistent with the ratings in other studies. [3]
The availability of a medication in multiple oral formulations and prescribing by junior doctors were two expected predictors of PEs, and closely concur with another study.[47] That junior doctors’ prescribing medication orders was shown to be an independent risk factor for PEs, compared with senior doctors, is argued to imply either that medication prescribing improves with experience or that junior doctors exert less intellectual effort on (or spare less time for) prescribing at discharge. Furthermore, both predictors imply that doctors, especially the juniors, should be trained in how to write correct and complete medication orders.[48,49] Lack of prescribing training for junior doctors should be looked at as a crucial opportunity for development. Medical students both in the UK[50] and abroad[51] have reported that they feel that therapeutics teaching is not given enough time. Future research should be directed towards the incidence and causative factors of PEs committed by junior doctors; this is a recommendation of a recent systematic review that failed to reach meaningful conclusions given the wide range of designs, methods and error rates.[52]
Characteristics and Impact of Pharmacists’ Interventions
It is obvious that the number of recorded pharmacists’ clinical interventions not associated with PEs was astonishingly few (only 11), in comparison with a study[1] reporting a rate of 15.2%. Underreporting of this type of pharmacists’ intervention is attributed to the inflexibility of the e-prescribing system designed to help pharmacists capture almost all PE types but not all pharmaceutical care activities. It is also important to note that many of the typical pharmacist interventions are done during hospital admission and not at the point of discharge. One study[3] reported that only 60% of pharmacists’ interventions related to PEs. A French study[2] reported a pharmacists’ interventions rate similar to the rate in this study.
Independent interventions included all interventions independently done by the pharmacists regardless of whether they informed the doctors afterwards or not. The high proportion of these independent interventions and the short time elapsed to do these could fairly reflect how ‘competent’ the pharmacists were in checking and correcting discharge medication orders, as well as how much they were up-to-date with their patients’ clinical status at discharge. Reasons for the wide time lapse for pharmacists to intervene upon a few erroneous orders included (i) when doctors had already entered discharge medication orders for patients whose discharges were delayed because of unpredicted changes in their health status at discharge; (ii) lack of efficient communication between pharmacists and doctors, where pharmacists were sometimes not up-to-date with patients’ clinical status and medication changes happened during consultant ward rounds; and (iii) heavy workload, pressure to discharge patients and shortage of pharmacy staff.
The findings of this study contribute to the body of literature that pharmacists provide a crucial ‘safety net’ to improve the quality of hospital prescribing.[1,29,39,41,53] The independent and efficient pharmacists’ interventions reported in this study concur with the view that pharmacists are in the best position to transcribe, prescribe and change medication orders at discharge.[54–56] Given similarities in error types between inpatient and discharge stages, the latter argument can be extended to pharmacists intervening at the inpatient stage. [57,58] Strategically, the findings support the importance of developing a systematic medicines reconciliation process at hospital discharge, which is consistent with findings from other studies.[10]
Implications for Development of e-Prescribing Systems and Clinical Pharmacy Practice
The percentage of CREs in this study was higher than that reported in a UK study,[59] but closely similar to one French study.[2] Most of the CRE types identified in this study have been reported in the US and UK literature. [3,23,25] The information gathered about these errors should be used to improve the structure and facilities of the e-prescribing system. Suggested system enhancements could include the enabling of a decision-support facility to prevent ‘explicit’ (e.g. duplication of order) and more complicated (overdosage for a patient with renal impairment) errors, and the ability for the prescriber to view and prescribe medication orders throughout the patient’s journey from admission to discharge. Other examples of a system’s improvement of features could include the use of Tallman lettering,1 and showing the part of the dosage regimen and formulation at the beginning of any pre-defined order selected from the ‘look-up’ list (rather than keeping it after the drug name). Ergonomic improvement of the e-prescribing system cannot completely replace the pharmacist’s role in optimizing patient care, but it may allow pharmacists to focus on the most relevant clinical interventions.[2] A recent systematic review[60] has concluded that the evidence base reporting the effectiveness of e-prescribing to reduce PEs is not compelling.
Koppel commented, “Evaluation of CPOE [Computerized Prescriber Order Entry] systems, and of all healthcare information technology, is mostly terra incognita.”[53] Any decision to develop the existing e-prescribing system has to be evidence based; this would help estimate the harm avoided by such systems, which could be disproportional to their reduction in errors.[38] In addition, changing the clinical practice in response to e-prescribing system implementation should be simultaneously investigated as well, so pharmacists can work to complement, rather than duplicate, an e-prescribing system’s benefits. [3] Foot and Taylor[61] argue that the area that has to change most working practices is pharmacy, which should ensure the safe and effective use of the e-prescribing system within its remit. To date, published data on how e-prescribing has affected pharmacy services in the UK are limited. [62]
A multicentre, interrupted time-series study, adopting multi-method approaches, involving a range of qualitative and quantitative techniques, employing experienced study pharmacists and using cost-benefit analysis, needs to be conducted to investigate the incidence of PEs and ADEs in the context of e-prescribing systems.[63]
Conclusions
It is undeniable that PEs are common and will continue to exist, particularly in a field where complexity is the rule rather than the exception. In this study, four PEs occurred every hour in discharge prescribing on a normal workday, and one-third of the patients with PEs received high-risk medications. The pressing need for updated patient and therapeutic knowledge, the overlapping tasks of medical teams and flaws in the human-machine interface have all contributed to the emergence of PEs in hospitals. [24,25] Although challenging, pharmacists play a prominent role in efficiently documenting and preventing PEs before they reach and possibly harm the patient. There is no perfect solution for PEs. Implementing clinical pharmacy services, utilizing an e-prescribing system supported with clinical decision facility, and enhancing the awareness of the PE problem could all minimize the impact of this problem on patient safety. “Substitution of technology for people is misunderstanding of both.”[25]
References
Bosma L, Jansman F, Franken A, et al. Evaluation of pharmacist clinical interventions in a Dutch hospital setting. Pharm World Sci 2007; 30: 31–8
Estellat C, Colombet I, Vautier S, et al. Impact of pharmacy validation in a computerized physician order entry context. Int J Qual Health Care 2007; 1–9 1 Tallman lettering is the practice of writing part of a drug’s name in upper case letters to help distinguish sound-alike, look-alike drugs (e.g., predniSONE/prednisoLONE) from one another in order to avoid prescribing errors.
Donyai P, O’Grady K, Jacklin A, et al. The effects of electronic prescribing on the quality of prescribing. Br J Clin Pharmacol 2007; 1–8
Devine EB, Wilson-Norton JL, Lawless NM, et al. Characterization of prescribing errors in an internal medicine clinic. Am J Health Syst Pharm 2007; 64(10): 1062–70
Schumock GT, Guenette AJ, Keys TV, et al. Prescribing errors for patients about to be discharged from a university teaching hospital. Am JHosp Pharm 1994; 51(18): 2288–90
Franklin BD, O’Grady K, Paschalides C, et al. Providing feedback to hospital doctors about prescribing errors: a pilot study. Pharm World Sci 2007; 29(3): 213–20
Lewis PJ, Dornan T, Taylor D, et al. Prevalence, incidence and nature of prescribing errors in hospital inpatients: a systematic review. Drug Saf 2009; 32(5): 379–89
Lau HS, Florax C, Porsius AJ, et al. The completeness of medication histories in hospital medical records of patients admitted to general internal medicine wards. Br J Clin Pharmacol 2000; 49(6): 597–603
Nebeker JR, Hoffman JM, Weir CR, et al. High rates of adverse drug events in a highly computerized hospital. Arch Intern Med 2005; 165(10): 1111–6
Wong JD, Bajcar JM, Wong GG, et al. Medication reconciliation at hospital discharge: evaluating discrepancies. Ann Pharmacother 2008; 42(10): 1373–9
Poole DL, Chainakul JN, Pearson M, et al. Medication reconciliation: a necessity in promoting a safe hospital discharge. J Healthc Qual 2006; 28(3): 12–9
Santell JP. Reconciliation failures lead to medication errors. Jt Comm J Qual Patient Saf 2006; 32(4): 225–9
Vira T, Colquhoun M, Etchells E. Reconcilable differences: correcting medication errors at hospital admission and discharge. Qual Saf Health Care 2006; 15(2): 122–6
Al-Rashed SA, Wright DJ, Roebuck N, et al. The value of inpatient pharmaceutical counselling to elderly patients prior to discharge. Br J Clin Pharmacol 2002; 54(6): 657–64
Cua YM, Kripalani S. Medication use in the transition from hospital to home. Ann Acad Med Singapore 2008; 37(2): 136–41
Kerzman H, Baron-Epel O, Toren O. What do discharged patients know about their medication? Patient Educ Couns 2005; 56(3): 276–82
Makaryus AN, Friedman EA. Patients’ understanding of their treatment plans and diagnosis at discharge. Mayo Clin Proc 2005; 80(8): 991–4
Micheli P, Kossovsky MP, Gerstel E, et al. Patients’ knowledge of drug treatments after hospitalisation: the key role of information. Swiss Med Wkly 2007; 137(43-44): 614–20
Birdsey GH, Weeks GR, Bortoletto DA, et al. Pharmacistinitiated electronic discharge prescribing for cardiology patients. J Pharm Pract Res 2005; 35(4): 287–91
Hajjar ER, Hanlon JT, Sloane RJ, et al. Unnecessary drug use in frail older people at hospital discharge. J Am Geriatr Soc 2005; 53(9): 1518–23
Orme J, Shafford A, Barber N, et al. Quality of hospital prescribing [letter]. BMJ 1990; 300: 1398
Department of Health. Building a safer NHS for patients: implementing an organisation with a memory. London: The Stationery Office, 2001
Ash JS, Sittig DF, Dykstra R, et al. The unintended consequences of computerized provider order entry: findings from a mixed methods exploration. Int J Med Inform 2009; 78 Suppl. 1: S69–76
Jayawardena S, Eisdorfer J, Indulkar S, et al. Prescription errors and the impact of computerized prescription order entry system in a community-based hospital. Am J Ther 2007; 14(4): 336–40
Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA 2005; 293(10): 1197–203
Shamliyan TA, Duval S, Du J, et al. Just what the doctor ordered: review of the evidence of the impact of computerized physician order entry system on medication errors. Health Serv Res 2008; 43(1 Pt 1): 32–53
Brock TP, Franklin BD. Differences in pharmacy terminology and practice between the United Kingdom and the United States. Am J Health Syst Pharm 2007; 64(14): 1541–6
Jha AK, Kuperman GJ, Teich JM, et al. Identifying adverse drug events: development of a computer-based monitor and comparison with chart review and stimulated voluntary report. J Am Med Inform Assoc 1998; 5(3): 305–14
Koppel R, Leonard CE, Localio AR, et al. Identifying and quantifying medication errors: evaluation of rapidly discontinued medication orders submitted to a computerized physician order entry system. J Am Med Inform Assoc 2008; 15(4): 461–5
Franklin BD, Vincent C, Schachter M, et al. The incidence of prescribing errors in hospital inpatients: an overview of the research methods. Drug Saf 2005; 28(10): 891–900
‘High-alert’ medications and patient safety. Int J Qual Health Care 2001; 13(4): 339–40
Institute for Safer Medication Practices. ISMP’s list of high-alert medications [online]. Available from URL: http://www.ismp.org [Accessed 2008 Mar 13]
Barber N. Designing information technology to support prescribing decision making. Qual Saf Health Care 2004; 13(6): 450–4
British National Formulary. 56th ed. London: BMJ Group & RPS Publishing, 2008
Dean B, Barber N, Schachter M. What is a prescribing error? Qual Health Care 2000; 9(4): 232–7
Overhage JM, Lukes A. Practical, reliable, comprehensive method for characterizing pharmacists’ clinical activities. Am J Health Syst Pharm 1999; 56(23): 2444–50
Tully MP, Cantrill JA. Insights into creation and use of prescribing documentation in the hospital medical record. J Eval Clin Pract 2005; 11(5): 430–7
Franklin BD, O’Grady K, Donyai P, et al. The impact of a closed-loop electronic prescribing and administration system on prescribing errors, administration errors and staff time: a before-and-after study. Qual Saf Health Care 2007; 16(4): 279–84
Bedouch P, Charpiat B, Conort O, et al. Assessment of clinical pharmacists’ interventions in French hospitals: results of a multicenter study. Ann Pharmacother 2008; 42(7): 1095–103
Mirco A, Campos L, Falcao F, et al. Medication errors in an internal medicine department: evaluation of a computerized prescription system. Pharm World Sci 2005; 27: 351–2
Shulman R, Singer M, Goldstone J, et al. Medication errors: a prospective cohort study of hand-written and computerised physician order entry in the intensive care unit. Crit Care 2005; 9(5): R516–21
Anton C, Nightingale PG, Adu D, et al. Improving prescribing using a rule based prescribing system. Qual Saf Health Care 2004; 13(3): 186–90
Kanjanarat P, Winterstein AG, Johns TE, et al. Nature of preventable adverse drug events in hospitals: a literature review. Am J Health Syst Pharm 2003; 60(17): 1750–9
Roughead EE. The nature and extent of drug-related hospitalisations in Australia. J Qual Clin Pract 1999; 19(1): 19–22
Viktil KK, Blix HS, Reikvam A, et al. Comparison of drug-related problems in different patient groups. Ann Pharmacother 2004; 38(6): 942–8
Forster AJ, Murff HJ, Peterson JF, et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med 2003; 138(3): 161–7
Fijn R, van den Bemt PM, Chow M, et al. Hospital prescribing errors: epidemiological assessment of predictors. Br J Clin Pharmacol 2002; 53(3): 326–31
Dean B, Schachter M, Vincent C, et al. Causes of prescribing errors in hospital inpatients: a prospective study. Lancet 2002; 359(9315): 1373–8
Dean B. Learning from prescribing errors. Qual Saf Health Care 2002; 11(3): 258–60
Ellis A. Prescribing rights: are medical students properly prepared for them [letter]? BMJ 2002; 324: 1591
Wells JL, Borrie M J, Crilly R, et al. A novel clinical pharmacy experience for third-year medical students. Can J Clin Pharmacol 2002; 9(1): 7–16
Ross S, Bond C, Rothnie H, et al. What is the scale of prescribing errors committed by junior doctors? A systematic review. Br J Clin Pharmacol 2009; 67(6): 629–40
Koppel R. What do we know about medication errors made via a CPOE system versus those made via handwritten orders? Crit Care 2005; 9: 427–8
Cousins D, Luscombe D. A new model for hospital pharmacy practice. Pharm J 1996; 256: 347–51
Norris C, Thomas V, Calvert P. An audit to evaluate the acceptability of a pharmacist electronically prescribing discharge medication and providing information to GPs. Pharm J 2001; 267: 857–9
Sexton J, Brown A. Problems with medicines following hospital discharge: not always the patient’s fault. J Soc Admin Pharm 1999; 16: 199–207
Bhosle M, Sansgiry SS. Computerized physician order entry systems: is the pharmacist’s role justified? J Am Med Inform Assoc 2004; 11(2): 125–6
Williams C. Electronic prescribing can increase the efficiency of the discharge process. Hosp Pharm 2000; 7: 206–8
Mitchell D, Usher J, Gray S, et al. Evaluation and audit of a pilot of electronic prescribing and drug administration. J Inform Tech Healthcare 2004; 2(1): 19–29
Reckmann MH, Westbrook JI, Koh Y, et al. Does computerized provider order entry reduce prescribing errors for hospital inpatients? A systematic review. J Am Med Inform Assoc 2009; 16: 613–23
Foot R, Taylor L. Electronic prescribing and patient records: getting the balance right. Pharmaceutical J 2005; 274: 210–2
Mehta R, Onatade R. Experience of electronic prescribing in UK hospitals: a perspective from pharmacy staff. Pharm J 2008; 281: 79–82
Tully MP. The impact of information technology on the performance of clinical pharmacy services. J Clin Pharm Ther 2000; 25: 243–9
Acknowledgements
The authors would like to thank the pharmacists at the study hospital for their cooperation in data collection and validation.
The protocol was designed by all authors. Derar H. Abdel-Qader collected and analysed the data, and prepared the first draft of the article. All authors commented on subsequent drafts.
This study was funded by the Faculty of Medical and Human Sciences and School of Pharmacy and Pharmaceutical Sciences in the University of Manchester as part of Dr Derar Abdel-Qader’s PhD studentship. The authors have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abdel-Qader, D.H., Harper, L., Cantrill, J.A. et al. Pharmacists’ Interventions in Prescribing Errors at Hospital Discharge. Drug-Safety 33, 1027–1044 (2010). https://doi.org/10.2165/11538310-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11538310-000000000-00000