Abstract
Objectives
We determined in vitro the potency of macrolides as P-glycoprotein inhibitors and tested in hospitalised patients whether coadministration of P-glycoprotein inhibitors leads to increased serum concentrations of the P-glycoprotein substrates digoxin and digitoxin.
Methods
In vitro, the effect of macrolides on polarised P-glycoprotein-mediated digoxin transport was investigated in Caco-2 cells. In a pharmacoepidemiological study, we analysed the serum digoxin and digitoxin concentrations with and without coadministration of P-glycoprotein inhibitors in hospitalised patients.
Results
All macrolides inhibited P-glycoprotein-mediated digoxin transport, with concentrations producing 50% inhibition (IC50) values of 1.8, 4.1, 15.4, 21.8 and 22.7 μmol/L for telithromycin, clarithromycin, roxithromycin, azithromycin and erythromycin, respectively. Coadministration of P-glycoprotein inhibitors was associated with increased serum concentrations of digoxin (1.3 ± 0.6 vs 0.9 ± 0.5 ng/mL, p < 0.01). Moreover, patients receiving macrolides had higher serum concentrations of cardiac glycosides (p < 0.05).
Conclusion
Macrolides are potent inhibitors of P-glycoprotein. Drug interactions between P-glycoprotein inhibitors and substrates are likely to occur during hospitalisation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The ABCB1 (MDR1) gene encodes for the adenosine triphosphate-dependent efflux transporter P-glycoprotein. Its clinical relevance was first observed with the occurrence of multidrug resistance in cancer cells during chemotherapy.[1,2] It is now well known that the expression of P-glycoprotein in healthy tissues plays an important role in drug disposition and drug interactions.[3–5] In humans, P-glycoprotein is expressed in the apical membrane of epithelial cells in the intestine, the canalicular membrane of hepatocytes and the luminal membrane of proximal renal tubular epithelial cells, thereby modulating absorption and elimination of xenobiotics.[3–5] Moreover, it is an essential part of blood-tissue barriers, e.g. the blood-brain barrier, blood-testis barrier and placenta.[5–7] Both inhibition and induction of P-glycoprotein lead to drug interactions in humans. This is of particular clinical significance for drugs with a narrow therapeutic index, such as cardiac glycosides. For example, induction of P-glycoprotein by rifampicin (rifampin) leads to reduced plasma concentrations of orally administered digoxin, whereas P-glycoprotein inhibition by quinidine results in increased plasma concentrations of the cardiac glycoside.[8,9]
Among antibacterials, macrolides are very frequently prescribed drugs. In Germany, 52.6 million daily doses of macrolides were prescribed in 2004.[10] A broad variety of drug interactions with macrolides have been reported, which are mainly attributed to inhibition of CYP3A4.[11,12] However, there have been reports of increased serum concentrations and incidental toxicity of the P-glycoprotein substrates digoxin and digitoxin, which are not metabolised to a major extent in humans, during concomitant therapy with macrolides.[13–22] In addition, in vitro data indicate that erythromycin is a potent P-glycoprotein inhibitor.[23] Very few in vitro data are available on potential P-glycoprotein inhibition by other macrolides (e.g. roxithromycin) and ketolids such as telithromycin[24] and their relative potencies tested in the same in vitro system.
In spite of the increasingly recognised role of P-glycoprotein for drug interactions,[3–5,8,9,23,25] there is very little information as to whether P-glycoprotein-mediated drug interactions (e.g. with cardiac glycosides) are of relevance during routine care of hospitalised patients.[26] Moreover, factors influencing serum digoxin concentrations in routine patient care are still poorly understood. Recent data have indicated that in women with heart failure, digoxin serum concentrations of >1.2 ng/mL seem to be harmful.[27]
We therefore investigated the potential P-glycoprotein inhibitory effect of frequently used macrolides and the ketolid telithromycin in vitro using digoxin as a substrate on monolayers of the human colon carcinoma cell line Caco-2, which express P-glycoprotein in their apical membrane.[9,28,29] In the second part of the study, we evaluated whether digoxin and/or digitoxin serum concentrations are altered in hospitalised patients treated with macrolides or other P-glycoprotein inhibitors.
Methods
In Vitro Transport Studies in Caco-2 Cells
[3H]digoxin (19 Ci/mmol) and [3H]inulin (3.3 mg/mCi) were supplied by NEN Life Science Products (Boston, MA, USA). Unlabelled digoxin and erythromycin were purchased from Sigma Chemie (Deisenhofen, Germany). Unlabelled azithromycin, clarithromycin and roxithromycin were obtained from Chemos GmbH (Regenstauf, Germany). Unlabelled telithromycin was obtained after extraction of Ketek®Footnote 1 tablets (Sanofi-Aventis Deutschland GmbH; Bad Soden, Germany) using ethyl acetate and crystallisation from ethyl acetate/hexane (8 : 2 v/v). Purity was assayed by high-performance liquid chromatography with UV detection and found to be >99%.
Inhibition of In Vitro Drug Transport
The potential inhibition of P-glycoprotein function by macrolides and telithromycin was investigated using monolayers of P-glycoprotein-expressing Caco-2 cells (a human colon carcinoma cell line) as previously described.[9,29,30] In brief, Caco-2 cells were obtained from the American Type Culture Collection. The cells were cultured in Dulbecco’s Modified Eagle Medium supplemented with 10% heat-inactivated fetal bovine serum, L-glutamine 2 mmol/L, penicillin 100 U/mL, streptomycin 100 µg/mL, 1% sodium pyruvate and 1% nonessential amino acids at 37°C and 5% CO2. All cell culture media were obtained from Invitrogen GmbH (Karlsruhe, Germany). For transport studies, cells (passage number 43–65) were plated onto Transwell™ filters (Costar®; Corning Inc., Acton, MA, USA) and monolayers were used for experiments 7 days later. To ensure the integrity of the monolayer, the transepithelial resistance was measured after replacing the medium in each compartment by serum-free medium (Optimem™, Gibco-Invitrogen GmbH; Karlsruhe, Germany). Only wells with a resistance of ≥200Ω (≥182 Ω/cm2) after correction for the resistance obtained in control blank wells were used. For transport experiments, the medium in each compartment was then replaced with 800µL of test solution. This solution consisted of a serum-free medium with addition of tracer [3H]digoxin and 5 µmol/L of unlabelled digoxin as a P-glycoprotein substrate on the basal or apical side of the monolayer. In both compartments, the test solution also contained one of the macrolides as a putative inhibitor in concentrations of up to 500 µmol/L. For control experiments, the well known P-glycoprotein inhibitor valspodar (PSC-833; 1 µmol/L) [kindly provided by Novartis, Basel, Switzerland] was used instead of the macrolides. After 1, 2, 3 and 4 hours of incubation, the percentage of administered radioactivity appearing in the opposite compartment (basal or apical) was determined. Aliquots were analysed by liquid scintillation counting (Perkin Elmer Life Sciences GmbH; Rodgau-Jügesheim, Germany) after the addition of Ultima Gold™ (Perkin Elmer Life Sciences GmbH). All in vitro experiments were repeated at least six times. To control for the integrity of the monolayer after 4 hours and to rule out an influence of the macrolides on the integrity of the monolayer, the transport of [3H]inulin was determined in additional experiments in the presence of maximum concentrations of the putative inhibitors after 4 hours of incubation.
Data Analysis for In Vitro Experiments
The apparent permeability coefficients (Papp) from the cumulative basal-to-apical and apical-to-basal transport rates were determined according to equation 1:
where dQ/dt (mmol/sec) is the transport rate at 4 hours, C0 (mmol/cm3) is the initial substrate concentration in the donor compartment, and A (cm2) is the surface area of the monolayer (1.1 cm2). Basal-to-apical net transport was calculated after 4 hours by subtracting the apical-to-basal transport rate from the basal-to-apical transport rate. The percentage transport in inhibition experiments refers to control experiments in the absence of macrolides. The corresponding concentrations producing 50% inhibition (IC50 values) for inhibition of P-glycoprotein-mediated digoxin transport were calculated by fitting the basal-to-apical net transport at different inhibitor concentrations to a sigmoidal dose responsive regression curve (Prism 4.01 2004, GraphPad Software, Inc., San Diego, CA, USA).
Data Acquisition for Pharmacoepidemiological Study
The patients included in this study were recruited from pharmacoepidemiological study cohorts in the Department of Internal Medicine at University Hospital Erlangen-Nuremberg, the Department of Geriatric Medicine at Waldkrankenhaus Erlangen and the Department of Gastroenterology at University Hospital Regensburg, Germany. Within these cohorts, the patients’ demographic, medication and laboratory data were collected using software specifically developed for pharmacovigilance studies.[31–33]
Data Analysis for Pharmacoepidemiological Study
In these cohorts, a total of 458 patients received cardiac glycosides for treatment of heart failure or atrial fibrillation. To these patients, the following inclusion criteria were applied: (i) routine therapeutic drug monitoring (trough concentrations) for cardiac glycosides had been performed; and (ii) steady-state concentrations had been reached. All patients who met the inclusion criteria were screened for administration of P-glycoprotein inhibitors[4] or macrolides/telithromycin as included in our in vitro experiments. Patients receiving at least one of these inhibitors were included in the case groups. Patients who received no P-glycoprotein inhibitor were included in the control groups. In an initial analysis, only the first hospital stay was considered for evaluation. In an additional step, patient data from subsequent hospital stays were also included in the analysis if any of the following parameters had changed since their first hospital stay: the administered cardiac glycoside; the cardiac glycoside daily dose; or the comedication with P-glycoprotein inhibitors. The patients’ daily digoxin dosages were transferred to molar values to account for molecular weight differences between α-methyldigoxin and β-acetyldigoxin.
Statistical Analysis
In vitro data are presented as the mean ± 1 standard error of the mean. Multiple comparisons were analysed by ANOVA with a subsequent Tuckey test by using Prism 4.01 2004 (GraphPad Software, Inc.).
For the in vivo pharmacoepidemiological study, the database was screened with correlation analysis for related variables and possible covariates. The mean digoxin- and digitoxin serum values for each group were calculated on the basis of regression estimates using the general linear model in SPSS version 13 software (SPSS Inc., Chicago, IL, USA).
Serum digoxin/digitoxin values from the case and control groups were compared in a univariate analysis, taking into account the possible covariates of age, bodyweight, height, renal function (creatinine clearance determined according to the Cockcroft and Gault formula), hepatic function (AST, ALT and serum bilirubin), the daily dose of cardiac glycosides and the number of P-glycoprotein inhibitors. The data are presented as mean values ±1 standard deviation (SD) or with 95% confidence intervals (CIs). A p-value of <0.05 was required for statistical significance. In case of variance inhomogeneity, the level of significance was increased from p < 0.05 to p < 0.01.
Results
Inhibition of P-Glycoprotein by Macrolides
In Vitro Experiments
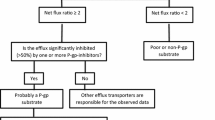
In control experiments, the directional basal-to-apical net transport of the P-glycoprotein substrate digoxin across the Caco-2 cell monolayers was confirmed. The respective Papp values (basal-to-apical 9.3 ± 2.2 × 10−6 cm/sec, apical-to-basal 2.4 ± 0.7 × 10−6 cm/sec, p < 0.001) were in good agreement with previously reported values.[13,29,34] As previously published,[13] this directional transport could be inhibited completely by valspodar (data not shown). All macrolides showed significant inhibition of P-glycoprotein-mediated digoxin transport (figure 1). The following sequence of inhibitory potency was determined: telithromycin > clarithromycin > roxithromycin > azithromycin > erythromycin, with corresponding IC50 values of 1.8 µmol/L, 4.1 µmol/L, 15.4 µmol/L, 21.8 µmol/L and 22.7 µmol/L, respectively (figure 1). The transepithelial translocation of [3H]inulin was not higher than 1%/hour in the absence and presence of azithromycin, clarithromycin, erythromycin, roxithromycin and telithromycin at the maximum tested concentrations, indicating a lack of effect of macrolides and telithromycin on the integrity of the cell monolayers.
Inhibition of P-glycoprotein-mediated digoxin net transport in Caco-2 monolayers by different concentrations of macrolides: (a) azithromycin; (b) clarithromycin; (c) erythromycin; (d) roxithromycin; and (e) telithromycin. Basal-to-apical net transport of [3H]digoxin (5 µmol/L) is presented at increasing macrolide concentrations. The basal-to-apical net transport mediated by P-glycoprotein was obtained by subtracting the apical-to-basal transport rate from the basal-to-apical transport rate. The concentrations producing 50% inhibition (IC50 values) were calculated by fitting the data to a sigmoidal dose responsive regression curve. The data are shown as the percentage of control experiments (in the absence of macrolides) and expressed as the mean ± 1 standard error of the mean from ≥6 experiments.
Influence of P-Glycoprotein Inhibitors on Serum Concentrations of Digoxin and Digitoxin
Pharmacoepidemiological Study
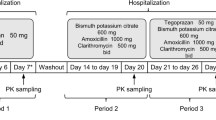
Of 458 datasets, the inclusion criteria were met by 157 patients on cardiac glycosides (80 men and 77 women). Of these 157 patients, 77 received digitoxin and 80 received digoxin. The demographic data and blood chemistry values of both patient groups are summarised in table I. As expected, patients treated with digitoxin had significantly reduced creatinine clearance compared with the digoxin group (table I). Altogether, ten different P-glycoprotein inhibitors were applied to 38 patients in the digitoxin group and 31 patients in the digoxin group, both representing the case groups (table II). On average, 1.3 and 1.5 P-glycoprotein inhibitors per patient were administered in the case groups, together with digitoxin and digoxin, respectively. A subgroup analysis of patients with serum cardiac glycoside concentrations above the therapeutic range (see table I) revealed that 33% (digitoxin) and 56% (digoxin) were additionally treated with P-glycoprotein inhibitors. In the presence of P-glycoprotein inhibitors, the odds ratio for elevated serum cardiac glycoside concentrations using digoxin instead of digitoxin was 3.48 (95% CI 0.95, 12.69). Without inhibitors, the odds ratio was <1 (0.65; 95% CI 0.21, 1.97).
Pharmacoepidemiological Study: Digitoxin
Patients receiving concomitant P-glycoprotein inhibitors had serum digitoxin concentrations similar to those of the control patients (18.9 ± 6.9 vs 18.6 ± 6.5 ng/mL) [figure 2 a]. This result remained unchanged by inclusion of values from subsequent hospital stays under changed medication and consideration of possible covariates such as hepatic function (AST, ALT and serum bilirubin) [figure 2 b].
Serum digitoxin concentrations in patients receiving P-glycoprotein inhibitors compared with controls (a) and also taking into account data from subsequent hospital stays under changed medication (b). The dots in the P-glycoprotein inhibitor group correspond to data from single patients receiving macrolides [n = 3 in (a) and n = 4 in (b)]. The central line in each box represents the median value, the lower and upper lines represent the 25th and 75th percentiles, respectively, and the whisker represents the 10th and 90th percentiles.
Pharmacoepidemiological Study: Digoxin
Because the daily digoxin dose and the patients’ mean creatinine clearance values differed between the case group and the control group, these variables were included as covariates in the univariate analysis of variance. Patients receiving concomitant P-glycoprotein inhibitors had higher serum digoxin concentrations than those not receiving them. The result was confirmed by adding covariates such as creatinine clearance and the daily digoxin dose (1.3 ± 0.6 vs 0.9 ± 0.5 ng/mL, p < 0.01) [figure 3 a]. Addition of patient data from subsequent hospital stays did not affect the observed difference (p = 0.01) [figure 3 b].
Elevated serum digoxin concentrations in patients receiving P-glycoprotein inhibitors compared with controls (a) and also taking into account data from subsequent hospital stays under changed medication (b). The dots in the P-glycoprotein inhibitor group correspond to data from single patients receiving macrolides [n = 7 in (a) and n = 8 in (b)]. The central line in each box represents the median value, the lower and upper lines represent the 25th and 75th percentiles, respectively, and the whisker represents the 10th and 90th percentiles. * p < 0.01 vs controls.
Pharmacoepidemiological Study: Macrolides
Data analysis of normalised cardiac glycoside serum concentrations (percentage values based on group means) revealed that patients receiving concomitant macrolides (erythromycin in six patients, clarithromycin in six patients) had higher serum cardiac glycoside concentrations than control patients receiving no P-glycoprotein inhibitor (Moses rank test p < 0.05) [figure 4 a]. In a further analysis, this effect was significant for the digoxin subgroup only (serum digoxin concentration control vs macrolide 100.0 ± 52.9% vs 175.0 ± 100.1%, Moses rank test p < 0.01) [figure 4 b].
(a) Serum cardiac glycoside concentrations in patients receiving macrolides compared with controls. Pooled data from all patients are shown (normalised to the mean values of each control group; the data are shown as the mean percentage ± SD). (b) Serum digoxin and digitoxin plasma concentrations in patients receiving macrolides compared with controls treated with digoxin or digitoxin only. The data are normalised to the mean values of each control group. The effect of macrolides on cardiac glycoside serum levels was significant in the digoxin group. * p < 0.05, ** p < 0.01 vs controls.
Discussion
Cardiac glycosides play an important role in the treatment of cardiovascular diseases such as heart failure or tachyarrhythmia. Because of their narrow therapeutic range, it is essential to understand factors determining interindividual differences in serum concentrations of cardiac glycosides. For example, recent data have indicated that women with heart failure and high serum digoxin concentrations were at increased risk of death.[27,35]
In this study, we observed the P-glycoprotein inhibitory effect of four commonly used macrolides and telithromycin in vitro using monolayers of P-glycoprotein-expressing Caco-2 cells. We found that all compounds inhibited P-glycoprotein-mediated digoxin transport, with IC50 values of 1.8–22.7 µmol/L. It is very likely that these concentrations are reached at the apical membrane of enterocytes, where P-glycoprotein is an important part of the barrier against entry of xenobiotics.
In our pharmacoepidemiological study of patients from routine clinical management, we showed that coadministration of P-glycoprotein inhibitors was associated with increased serum concentrations of digoxin, whereas no significant effect of P-glycoprotein inhibitors on serum concentrations of digitoxin was detected. Our findings on digoxin are consistent with those of a previous retrospective study[26] in which the possible influence of P-glycoprotein inhibitors on serum digoxin concentrations, but not on digitoxin concentrations, was assessed in comparison with controls in a parallel-group design. In line with our data, the investigators demonstrated that serum concentrations of digoxin were increased in the case group in comparison with controls, using a univariate and multivariate approach.[26] In accordance with our in vitro data, we were also able to show that concomitant administration of the macrolides clarithromycin and erythromycin was associated with significantly increased cardiac glycoside serum concentrations in comparison with controls who did not receive macrolides.
Our in vitro data are in line with previous studies of erythromycin, clarithromycin and roxithromycin.[17,23,24] Pachot et al.[24] showed qualitatively that 100 µmol/L (but not 1 µmol/L) of roxithromycin and telithromycin significantly inhibited basal-to-apical verapamil translocation across Caco-2 monolayers. Unfortunately, no IC50 values were determined in this study.[24] The IC50 values for P-glycoprotein inhibition obtained in our study were close to the therapeutic serum concentrations of the investigated compounds in humans. Since the highest inhibitor concentrations are reached in the gut lumen, it is likely that inhibition of intestinal P-glycoprotein plays the major role in the observed drug interactions. This is in line, for example, with the increased bioavailability of digoxin when coadministered with clarithromycin compared with the moderate effect on digoxin renal clearance.[17,19,20] In addition, there have been a number of case reports of interactions of macrolides (erythromycin or clarithromycin) and digoxin, where P-glycoprotein inhibition is likely to be one important underlying mechanism.[14,17,36–39]
We observed increased cardiac glycoside serum concentrations in patients receiving macrolides. Interestingly, the patient with the highest serum digoxin concentration during administration of the P-glycoprotein inhibitor clarithromycin (2.9 ng/mL [figure 3 b], which is in the toxic range), had had a previous hospital stay without any coadministration of a P-glycoprotein inhibitor. During that previous hospital stay, the patient’s serum digoxin concentrations had been in the therapeutic range (0.8 ng/mL). These data indicate that cardiac glycosides serum concentrations need to be carefully monitored in the clinical setting if these macrolides are coadministered.
There are several lines of evidence from in vivo studies for a major role of P-glycoprotein in digoxin disposition in humans. First, following intravenous application to healthy subjects, about 11% of the digoxin dose was found in the gut lumen, demonstrating the secretory function of intestinal cells.[25] Second, this efflux transport could be inhibited by luminally administered P-glycoprotein inhibitors.[25] Increased bioavailability of digoxin was observed when it was coadministered orally with quinidine, a potent P-glycoprotein inhibitor.[40] Third, reduced biliary clearance was observed when digoxin and quinidine were administered simultaneously.[41] Fourth, animal studies and studies in humans also showed reduced renal clearance of digoxin when quinidine was coadministered.[40,42] In addition, in vitro and in vivo data have indicated a potential role of P-glycoprotein in digitoxin disposition in humans.[13,43,44]
In our pharmacoepidemiological study, we found increased serum digoxin concentrations but no change in digitoxin serum concentrations compared with the respective control groups. The latter finding was unexpected since no obvious differences for both P-glycoprotein substrates have been reported from in vitro experiments.[13] One possible explanation is the different pharmacokinetic properties of both cardiac glycosides. Whereas digitoxin has nearly maximal oral bioavailability (90%) in humans, the lower bioavailability of digoxin (60–80%) could lead to a more pronounced increase in serum digoxin concentrations if P-glycoprotein inhibitors are coadministered.[45,46] This indicates that the effect of P-glycoprotein inhibition on digitoxin serum concentrations will be smaller than with digoxin.
The present study may have underestimated the effect of digitalis drug interactions because of other confounders in the hospital setting (e.g. underlying diseases, partial noncompliance, comedications not being mentioned to the physician, e.g. St John’s wort). On the other hand, clinicians need information about drug interactions that reflect ‘real life’ in the hospital, e.g. studying drug interactions in steady-state conditions. We therefore believe that the present study contributes to this knowledge.
Conclusion
By use of a combined in vitro and in vivo approach, we have provided some insight into determinants of cardiac glycoside serum concentrations. First, a direct in vitro comparison of four frequently used macrolides and telithromycin as P-glycoprotein inhibitors was conducted. Second, the relevance of P-glycoprotein inhibition to routine hospital care was shown, since P-glycoprotein inhibitors increased serum digoxin concentrations. Finally, in accordance with the in vitro data, patients receiving macrolides had significantly increased serum concentrations of cardiac glycosides.
In view of recent data showing that serum digoxin concentrations of >1.2 ng/mL seem to be harmful in women with heart failure,[27] particular attention should be given to transporter-mediated drug-drug interactions in the clinical setting.
Notes
The use of trade names is for product identification purposes only and does not imply endorsement.
References
Juliano RL, Ling V. A surface glycoprotein modulating drug permeability in Chinese hamster ovary cell mutants. Biochim Biophys Acta 1976 Nov; 455(1): 152–62
Ford JM, Hait WN. Pharmacology of drugs that alter multidrug resistance in cancer. Pharmacol Rev 1990 Sep; 42(3): 155–99
Mizuno N, Niwa T, Yotsumoto Y, et al. Impact of drug transporter studies on drug discovery and development. Pharmacol Rev 2003 Sep; 55(3): 425–61
Marzolini C, Paus E, Buclin T, et al. Polymorphisms in human MDR1 (P-glycoprotein): recent advances and clinical relevance. Clin Pharmacol Ther 2004 Jan; 75(1): 13–33
Fromm MF. Importance of P-glycoprotein at blood-tissue barriers. Trends Pharmacol Sci 2004 Aug; 25(8): 423–9
Fromm MF. P-glycoprotein: a defense mechanism limiting oral bioavailability and CNS accumulation of drugs. Int J Clin Pharmacol Ther 2000 Feb; 38(2): 69–74
Fricker G, Miller DS. Modulation of drug transporters at the blood-brain barrier. Pharmacology 2004 Apr; 70(4): 169–76
Greiner B, Eichelbaum M, Fritz P, et al. The role of intestinal P-glycoprotein in the interaction of digoxin and rifampin. J Clin Invest 1999 Jul; 104(2): 147–53
Fromm MF, Kim RB, Stein CM, et al. Inhibition of P-glycoprotein-mediated drug transport: a unifying mechanism to explain the interaction between digoxin and quinidine. Circulation 1999 Feb; 99(4): 552–7
Schwabe U, Paffrath D. Arzneiverordnungs-Report 2005: Aktuelle Daten, Kosten, Trends und Kommentare. Berlin: Springer Verlag, 2005
Ito K, Ogihara K, Kanamitsu S, et al. Prediction of the in vivo interaction between midazolam and macrolides based on in vitro studies using human liver microsomes. Drug Metab Dispos 2003 Jul; 31(7): 945–54
Polasek TM, Miners JO. Quantitative prediction of macrolide drug-drug interaction potential from in vitro studies using testosterone as the human cytochrome P4503A substrate. Eur J Clin Pharmacol 2006 Mar; 62(3): 203–8
Pauli-Magnus C, Mürdter T, Godel A, et al. P-glycoprotein-mediated transport of digitoxin, alpha-methyldigoxin and beta-acetyldigoxin. Naunyn Schmiedebergs Arch Pharmacol 2001 Mar; 363(3): 337–43
Morton MR, Cooper JW. Erythromycin-induced digoxin toxicity. DICP 1989 Sep; 23(9): 668–70
Corallo CE, Rogers IR. Roxithromycin-induced digoxin toxicity. Med J Aust 1996 Oct; 165(8): 433–4
Thalhammer F, Hollenstein UM, Locker GJ, et al. Azithromycin-related toxic effects of digitoxin. Br J Clin Pharmacol 1998 Jan; 45(1): 91–2
Wakasugi H, Yano I, Ito T, et al. Effect of clarithromycin on renal excretion of digoxin: interaction with P-glycoprotein. Clin Pharmacol Ther 1998 Jul; 64(1): 123–8
Aventis Pharmaceuticals. Ketek™ (telithromycin): briefing document for the FDA Anti-Infective Drug Products Advisory Committee meeting, March 2001 [online]. Available from URL: http://www.fda.gov/ohrms/dockets/ac/01/briefing/3746b_01_aventis.pdf [Accessed 2007 Sep 21]
Zapater P, Reus S, Tello A, et al. A prospective study of the clarithromycin-digoxin interaction in elderly patients. J Antimicrob Chemother 2002 Oct; 50(4): 601–6
Rengelshausen J, Goggelmann C, Burhenne J, et al. Contribution of increased oral bioavailability and reduced nonglomerular renal clearance of digoxin to the digoxin-clarithromycin interaction. Br J Clin Pharmacol 2003 Jul; 56(1): 32–8
Stahlmann R, Fuhr R. Azithromycin. Arzneimitteltherapie 2004 Apr; 22(4): 110–8
Nenciu LM, Laberge P, Thirion DJ. Telithromycin-induced digoxin toxicity and electrocardiographic changes. Pharmacotherapy 2006 Jun; 26(6): 872–6
Kim RB, Wandel C, Leake B, et al. Interrelationship between substrates and inhibitors of human CYP3A and P-glycoprotein. Pharm Res 1999 Mar; 16(3): 408–14
Pachot JI, Botham RP, Haegele KD, et al. Experimental estimation of the role of P-glycoprotein in the pharmacokinetic behaviour of telithromycin, a novel ketolide, in comparison with roxithromycin and other macrolides using the Caco-2 cell model. J Pharm Pharm Sci 2003 Jan-Apr; 6(1): 1–12
Drescher S, Glaeser H, Mürdter T, et al. P-glycoprotein-mediated intestinal and biliary digoxin transport in humans. Clin Pharmacol Ther 2003 Mar; 73(3): 223–31
Englund G, Hallberg P, Artursson P, et al. Association between the number of coadministered P-glycoprotein inhibitors and serum digoxin levels in patients on therapeutic drug monitoring. BMC Med 2004 Apr; 2: 8
Adams Jr KF, Patterson JH, Gattis WA, et al. Relationship of serum digoxin concentration to mortality and morbidity in women in the Digitalis Investigation Group trial: a retrospective analysis. J Am Coll Cardiol 2005 Aug; 46(3): 497–504
Yamashita S, Tanaka Y, Endoh Y, et al. Analysis of drug permeation across Caco-2 monolayer: implication for predicting in vivo drug absorption. Pharm Res 1997 Apr; 14(4): 486–91
Bachmakov I, Rekersbrink S, Hofmann U, et al. Characterisation of (R/S)-propafenone and its metabolites as substrates and inhibitors of P-glycoprotein. Naunyn Schmiedebergs Arch Pharmacol 2005 Mar; 371(3): 195–201
Kim RB, Fromm MF, Wandel C, et al. The drug transporter P-glycoprotein limits oral absorption and brain entry of HIV-1 protease inhibitors. J Clin Invest 1998 Jan; 101(2): 289–94
Egger T, Dormann H, Ahne G, et al. Identification of adverse drug reactions in geriatric inpatients using a computerised drug database. Drugs Aging 2003; 20(10): 769–76
Dormann H, Criegee-Rieck M, Neubert A, et al. Implementation of a computer-assisted monitoring system for the detection of adverse drug reactions in gastroenterology. Aliment Pharmacol Ther 2004 Feb; 19(3): 303–9
Reisig M. Implementierung und Evaluation eines computergestützten Systems zur Optimierung der individuellen Arzneimitteltherapie [dissertation]. Erlangen: Friedrich-Alexander-Universität Erlangen-Nürnberg, 2006
Kivistö KT, Zukunft J, Hofmann U, et al. Characterisation of cerivastatin as a P-glycoprotein substrate: studies in P-glyco-protein-expressing cell monolayers and mdr1a/b knock-out mice. Naunyn Schmiedebergs Arch Pharmacol 2004 Aug; 370(2): 124–30
Rathore SS, Curtis JP, Wang Y, et al. Association of serum digoxin concentration and outcomes in patients with heart failure. JAMA 2003 Feb; 289(7): 871–8
Lindenbaum J, Rund DG, Butler Jr VP, et al. Inactivation of digoxin by the gut flora: reversal by antibiotic therapy. N Engl J Med 1981 Oct; 305(14): 789–94
Midoneck SR, Etingin OR. Clarithromycin-related toxic effects of digoxin. N Engl J Med 1995 Nov; 333(22): 1505
Nawarskas JJ, McCarthy DM, Spinler SA. Digoxin toxicity secondary to clarithromycin therapy. Ann Pharmacother 1997 Jul-Aug; 31(7–8): 864–6
Laberge P, Martineau P. Clarithromycin-induced digoxin intoxication. Ann Pharmacother 1997 Sep; 31(9): 999–1002
Pedersen KE, Christiansen BD, Klitgaard NA, et al. Effect of quinidine on digoxin bioavailability. Eur J Clin Pharmacol 1983; 24(1): 41–7
Angelin B, Arvidsson A, Dahlqvist R, et al. Quinidine reduces biliary clearance of digoxin in man. Eur J Clin Invest 1987 Jun; 17(3): 262–5
Koren G, Klein J, De Lannoy IA, et al. Cyclosporin and quinidine inhibition of renal digoxin excretion: evidence for luminal secretion of digoxin. Am J Physiol 1992 Oct; 263(4): F613–22
Sphakianaki E, Tsouderos I, Morali A, et al. Interactions between digitoxin and some antiarrhythmic drugs. Methods Find Exp Clin Pharmacol 1992 Jun; 14(5): 355–60
Laer S, Scholz H, Buschmann I, et al. Digitoxin intoxication during concomitant use of amiodarone. Eur J Clin Pharmacol 1998 Mar; 54(1): 95–6
Smith TW. Pharmacokinetics, bioavailability and serum levels of cardiac glycosides. J Am Coll Cardiol 1985 May; 5 (5 Suppl. A): 43A–50A
Francke DE. Bioavailability of digoxin. Ann Pharmacother 2006 Jun; 40(6): 1185
Acknowledgements
Drs Sonja Eberl and Bertold Renner contributed equally to the study. The authors thank Mrs B. Endress for excellent technical assistance and Novartis for providing the PSC-833. This work was supported by grant numbers Fr1298/2–4 and K02120/1–3 from the Deutsche Forschungsgemeinschaft (Bonn, Germany). The authors have no other conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Eberl, S., Renner, B., Neubert, A. et al. Role of P-Glycoprotein Inhibition for Drug Interactions. Clin Pharmacokinet 46, 1039–1049 (2007). https://doi.org/10.2165/00003088-200746120-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003088-200746120-00004