Abstract
Ciclosporin is a potent immunomodulator that acts selectively and locally when administered at the ocular surface. 0.05% ciclosporin ophthalmic emulsion has recently been approved by the US FDA for treatment of keratoconjunctivitis sicca (KCS) [dry-eye disease].
After topical application, ciclosporin accumulates at the ocular surface and cornea, achieving concentrations (≥0.236 μg/g) that are sufficient for immunomodulation. Very little drug penetrates through the ocular surface to intraocular tissues. Ciclosporin is not metabolised in rabbit or dog eyes and may not be prone to metabolism in human eyes. Cultured human corneal endothelial and stromal cells exposed to ciclosporin in vitro exhibited no adverse effects and only minor effects on DNA synthesis. No ocular or systemic toxicity was seen with long-term ocular administration of ciclosporin at concentrations up to 0.4%, given as many as six times daily for 6 months in rabbits and 1 year in dogs. Systemic blood ciclosporin concentration after ocular administration was extremely low or undetectable in rabbits, dogs and humans, obviating concerns about systemic toxicity. In 12-week and 1-year clinical safety studies in dry-eye patients, the most common adverse event associated with the ophthalmic use of ciclosporin emulsion was ocular burning. No serious drug-related adverse events occurred.
These data from in vitro, nonclinical and clinical studies indicate effective topical delivery of ciclosporin to desired target tissues along with a favourable safety profile, making 0.05% ciclosporin ophthalmic emulsion a promising treatment for KCS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Ciclosporin is a potent immunomodulator that has been used to treat various immunological disorders for more than two decades.[1] The drug was first introduced for prevention of solid organ graft rejection in 1983.[2] In addition to its applications for immunosuppression after transplantation and for treatment of rheumatoid arthritis and severe psoriasis, systemically administered ciclosporin at dosages from 2 to 15 mg/kg/day has been found to relieve many ocular disorders such as uveitis, Behçet’s disease and bird shot retinochoroiditis.[3–8] Common adverse effects associated with systemic administration of ciclosporin, including elevated serum creatinine, hypertension and renal dysfunction, are reversed upon reduction of the ciclosporin dosage.[4] Such adverse effects limit systemic ciclosporin use to the treatment of intraocular disorders unlikely to respond to topically administered therapies.
For ocular surface disorders, delivery of ciclosporin directly to the eye provides efficacy and safety advantages. Treatment by topical administration achieves high ciclosporin concentrations in surface tissues and precludes toxicity associated with high systemic levels of ciclosporin. Ophthalmic application of ciclosporin has been used for corneal allografts,[9] vernal keratoconjunctivitis,[10] keratoconjunctivitis sicca (KCS) [dry-eye disease],[11] immune-mediated keratitis,[12] necrotising scleritis[13] and herpetic stromal keratitis.[14] 0.05% ciclosporin ophthalmic emulsion has been evaluated for treatment of KCS in several large clinical trials.[15,16]
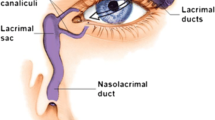
Dry-eye patients exhibit chronic inflammation at the ocular surface and in the lacrimal gland.[11,17] Immunohistochemical studies have demonstrated accumulation of CD4 (T-helper) cells within these tissues.[18,19] Ciclosporin specifically inhibits the activation of T-helper cells in the ocular surface tissues by blocking the production of interleukin-2, a key cytokine for immune-mediated inflammation.[20] Topical ophthalmic ciclosporin has been shown to reduce lacrimal gland lymphocytic infiltrates and improve tear production in dry-eye patients with or without Sjögren’s syndrome[21–24] and in dogs with dry eye.[25–28]
In 1995, the US FDA approved 0.2% ciclosporin ophthalmic ointment (Optimmune®; Schering-Plough, Union, NJ, USA)Footnote 1 for the treatment of canine KCS. Various vehicles have been tested for ocular penetration in rabbits and in humans, including castor oil,[29] aqueous cyclodextrin,[30] collagen shields,[31] nanocapsules,[32] nanoparticles[33] and emulsions.[34] Recently, the FDA approved Restasis™ 0.05% ophthalmic ciclosporin emulsion (Allergan, Irvine, CA, USA) for treatment of KCS in humans. It is the first commercially available therapy that acts on the inflammation underlying KCS.
This review explores ocular pharmacokinetics and safety studies of ciclosporin, as well as drug bioavailability in formulations tested during development of 0.05% ciclosporin emulsion.
1. Physicochemical Properties and Ophthalmic Dosage Forms
Ciclosporin is a neutral, hydrophobic, cyclic undecapeptide[35] (figure 1) with a molecular weight of 1202.6 daltons. Given its physicochemical properties, ciclosporin presents a challenge in developing an ophthalmic formulation of adequate drug concentration to provide stability, reliable drug delivery and acceptable vehicle safety. Topical drug absorption is a function of formulation, drug concentration and vehicle drug solubility. The poor water solubility of ciclosporin should preclude aqueous solution formulations for any clinically useful dosage strength, but ciclosporin suspensions in balanced salt solution,[36] in aqueous cyclodextrin solution[30] and in polyisohexylcyanoacrylate nanocapsules dispersed in an isotonic and neutral aqueous vehicle are under investigation.[37,38] Many ophthalmic ciclosporin dosage forms have been prepared in castor, corn, olive and peanut oils. However, epithelial keratitis has been associated with the use of these oil vehicles.[36,39] While ciclosporin formulated in a corn oil ointment helped relieve symptoms of KCS patients, it was also associated with early burning, redness and itching.[22]
To improve delivery of ciclosporin to ocular tissues, an emulsion formulation in castor oil was developed that produces sustained ciclosporin concentrations sufficient for immunomodulation in external ocular tissues. Using this emulsion formulation, ciclosporin concentrations as low as 0.05% effectively treated symptoms of dry-eye disease.[15,16] Topical administration of the castor oil-water emulsion results in extremely low systemic ciclosporin concentrations while maintaining acceptable patient comfort. The castor oil-water emulsion formulation used for Restasis™ also includes glycerin, polysorbate 80 and sodium hydroxide to adjust the pH.[40] Upon instillation directly into the eyes, ciclosporin partitions from the oil droplets into ocular surface tissues (see section 3.1). The ocular retention time (ORT) for this emulsion vehicle is approximately 2 hours,[41] which exceeds that observed for saline and viscous solution formulations (in the range of minutes).[42]
2. Bioanalytical Methodology
Treatment by topical administration of ciclosporin avoids toxicity associated with high systemic levels of ciclosporin. Because topical administration of ciclosporin results in extremely low blood concentrations (section 3.1), highly sensitive and selective detection methods are required. Many bioanalytical methods have been developed to assay ciclosporin in human blood.[16,43–48] Among these methods, radioimmunoassay (RIA) and fluorescence polarisation immunoassay (FPIA) provide rapid means for determining ciclosporin concentrations in biological fluids; however, both methods generally tend to overestimate ciclosporin concentration because of cross-reactivity with its many metabolites. High pressure liquid chromatography (HPLC) appears to be more selective than RIA and FPIA. None of these methods, however, are very sensitive; the lower limits of quantitation (LLOQ) for RIA, FPIA and HPLC were 62.5, 50 and 20 µg/L, respectively.[45] Several more sensitive liquid chromatography-mass spectrometry (LC-MS/MS) methods have been developed for the assay of ciclosporin in human blood, providing LLOQ in the range of 0.5–10 µg/L.[43,44,46]
An even more sensitive LC-MS/MS method has been developed for the determination of ciclosporin concentrations in human and dog blood.[16] A similar assay was used for rabbit blood. An organic extract of each blood sample was characterised by separation on a reverse-phase HPLC column coupled to a mass spectrometer. Protonated molecules of ciclosporin (m/z 1203) and geclosporin (m/z 1217), the internal standard, were collisionally dissociated; product ions at m/z 425 were monitored. Standard curves for human and dog assays were linear over the concentration range of 0.1–5 µg/L. Interday precision (percentage relative standard deviation) based on day-to-day evaluation of quality control samples of human or dog blood was <14%. Interday accuracies for the human blood and dog blood assays were 102.6–113.4% and 94.6–108.3%, respectively. The LLOQ was 0.1 µg/L, providing greater sensitivity than HPLC, RIA, FPIA or earlier LC-MS/MS methods.
3. Pharmacokinetics of Ophthalmic Ciclosporin
3.1 Ocular Absorption and Distribution
3.1.1 Animals
Ocular absorption and tissue distribution of ciclosporin after ophthalmic administration have been studied extensively in rabbits and dogs.[29,38,41,49–56] Results of these studies are consistent in two respects: high ciclosporin bioavailability is observed for ocular surface tissues, and drug penetration into intraocular tissues is extremely poor (table I and table II). After topical instillation, ciclosporin readily leaves the tear film and partitions into the conjunctiva, cornea and accessory lacrimal glands, achieving high concentrations. Cyclosporin concentrations in the conjunctiva, cornea and lacrimal gland of rabbits increased as the ciclosporin strength in the castor oil-water emulsion increased from 0.05% to 0.2% (table I). In general, these concentrations of ciclosporin in ocular tissues were observed 20 minutes to 1 hour after dose instillation, indicating that ciclosporin was rapidly absorbed into rabbit and dog eyes.[57]
The corneal epithelium is the most significant drug reservoir for topically applied ciclosporin in rabbits.[29] The corneal stroma, however, is mainly composed of water and is an effective barrier against penetration of ciclosporin from the castor oil-water emulsion, resulting in sustained high concentrations at the ocular surface and low concentrations in intraocular tissues (table II).
The absorption, efficacy and potential toxicity of a drug can each increase with repeated administration. Ratios in various ocular tissues of the maximum concentration (Cmax) values after multiple ocular doses to those after single ocular doses were determined to estimate the extent of ciclosporin accumulation after repeated administration of a castor oil-water emulsion formulation.[41] These ratios showed variable accumulation of ciclosporin in different ocular tissues of dogs and rabbits. In dogs, ciclosporin accumulated slightly in the conjunctiva (multiple-dose/single-dose ratio 1.4), moderately in the lacrimal gland (ratio 2.4), and to a greater extent in the cornea (ratio 5.8). In rabbits, ciclosporin accumulated moderately in the cornea (ratio 3.9) and significantly in the lacrimal gland (ratio 9.2). The relative accumulation of ciclosporin in various tissues was similar in rabbits and dogs; the difference seen in the accumulation ratios for the lacrimal gland was attributed to anatomical differences between the two species.[41] Work by Kaswan et al.[25,26,49] showed that the dog is better than the rabbit for modelling ciclosporin penetration and efficacy in humans.
Drug vehicle retention time is a major factor affecting the extent of a drug’s accumulation. Studies were conducted in the left eyes of beagle dogs to evaluate the ORT of the ciclosporin castor oil-water emulsion formulations and corresponding vehicles.[41] The castor oil content of the emulsion was elevated for formulations containing greater ciclosporin concentrations. The mean ORT after instillation increased proportionately with increasing ciclosporin concentration (and increasing castor oil content). For example, 0.05% ciclosporin had an ORT of 1.75 hours, whereas 0.2% ciclosporin had an ORT of 3.1 hours. Similarly, the vehicle for 0.05% ciclosporin had an ORT of 2 hours and the vehicle for 2% ciclosporin had an ORT of 2.75 hours. The long ORTs may have contributed to the prolonged absorption of ciclosporin into ocular surface tissues. In clinical terms, the emulsion vehicle may reduce evaporation of the limited natural tears produced by patients with dry-eye disease, thereby providing additional benefits to these patients.
The terminal half-life of ciclosporin in ocular tissues after ocular administration was long,[41] approximately 40 hours in rabbit corneas and 20–30 hours in the conjunctivae of rabbits and dogs. Such prolonged retention of ciclosporin, together with the favourable drug partitioning into the ocular surface tissues discussed earlier in this section, promotes prolonged ciclosporin efficacy in the ocular surface tissues associated with dry-eye disease.
3.1.2 Humans
More studies of ciclosporin concentrations in ocular tissue and blood have been performed for laboratory animals (section 3.1.1) than for humans; in addition, the results from the few clinical trials are much more variable. After topical application of ciclosporin (0.5% in olive oil), an extremely steep concentration gradient (over two orders of magnitude) formed across the human cornea button; ciclosporin concentrations of 1.252, 0.161 and 0.007 ng/mm2 accumulated in the epithelium, stroma and endothelium, respectively.[59] Low aqueous humour concentrations in clinical studies showed that intraocular penetration of ophthalmic ciclosporin was low (mean values <100 µg/L) [table III]. These results are consistent with observations in laboratory animal eyes (table I).
Ciclosporin concentrations in human cornea and conjunctiva after instillation of 0.05% ciclosporin emulsion are not available, but may be extrapolated from tissue concentration data in rabbits and dogs treated with 0.05% ciclosporin emulsion. Human[61] and dog[55] corneal concentrations were similar (3840 ng/g vs 3700 ng/g) after ocular instillation of a 0.5% aqueous solution of ciclosporin every 15 minutes for 1 hour before keratoplasty. When albino rabbits received an identical dosage regimen and formulation, the mean corneal concentration was approximately 9400 ng/g.[55] These data indicate that when rabbits, dogs and humans are subjected to the same ciclosporin ophthalmic regimen, human corneal concentrations are comparable to those in dogs and 40% of those in rabbits. Therefore, based on a steady-state corneal Cmax value of 1550 ng/g during 0.05% ciclosporin emulsion treatment twice daily to rabbits,[54] the human corneal Cmax value should be 620 ng/g. The steady-state Cmax value in dog cornea[41] (452 ng/g) comes close to that value.
Choice of vehicle can affect the drug’s availability. In the study where 0.5% ciclosporin was administered in aqueous solution,[61] the mean human corneal ciclosporin concentration was approximately 3700 ng/g. Topical instillation of five to ten drops of 2% ciclosporin solution in olive oil yielded a mean human cornea ciclosporin concentration of only 236 ng/g.[65] This low corneal concentration occurred despite the greater drug concentration, and despite the initiation of treatment 1 day before keratoplasty, as opposed to 1 hour before keratoplasty for the 0.5% ciclosporin in aqueous solution. Olive oil is clearly a less favourable vehicle for delivery of ciclosporin than castor oil.
3.2 Ocular Metabolism
Although extensive metabolism of ciclosporin occurs in the livers of humans and laboratory animals,[66] ciclosporin is not metabolised in rabbit eyes[29,41] or in dog eyes.[57]
On the basis of these observations, ocular metabolism of ciclosporin is not expected in humans. In one study, hydroxylated ciclosporin metabolites were detected in the aqueous humour of patients who received one to two drops of 2% ciclosporin prior to cataract surgery.[60] Ciclosporin is mainly metabolised by hepatic cytochrome P450 (CYP) 3A isoenzymes[67] whose ocular metabolic activities are 1000–5000 times lower than those found in hepatic microsomes. These data, together with observations that constitutive CYP drug metabolism activities in rabbit, dog, monkey and human eyes are qualitatively similar,[68] suggest that little or no ocular metabolism of ciclosporin occurs in humans. Thus, drug interactions due to metabolic mechanisms are not expected from ophthalmic ciclosporin treatment.
3.3 Ocular and Systemic Cyclosporin Concentrations in Humans
Ocular ciclosporin concentrations observed after ophthalmic ciclosporin application are much lower than the systemic tissue ciclosporin concentrations required for procedures such as organ transplantation. In patients with (n = 8) and without (n = 9) cellular rejection after orthotopic liver transplantation, a statistically significant difference occurred in hepatic ciclosporin concentrations (1879 ± 998 vs 3493 ± 936 ng/g; p < 0.01), suggesting a threshold concentration for immunosuppression.[69] Similar observations were reported for kidney,[70] ileum[71] and colon.[69,72] Patients whose systemic treatment with ciclosporin resulted in successful immunosuppression had mean tissue concentrations ranging from 3000 to 10 000 ng/g (figure 2). These concentrations are 8- to 20-fold greater than the ciclosporin concentrations in ocular surface tissues (estimated to be 450–620 ng/g, extrapolated from dog and rabbit data) anticipated from topical application of ophthalmic 0.05% ciclosporin emulsion in dry-eye patients. When administered topically, 0.05% ciclosporin castor oil-water emulsion has been shown to alleviate symptoms of KCS.[15,16]
Comparative human tissue ciclosporin concentrations. Concentrations in colon, ileum, kidney and liver are from immunosuppressive treatment by oral or intravenous administration of ciclosporin,[69–71] whereas the concentration in cornea/conjunctiva represents ocular administration of 0.05% ciclosporin in castor oil emulsion. 1 Ciclosporin concentration in cornea and conjunctiva is predicted from comparable data sets in rabbit, dog and human.
4. Ocular Safety of Ciclosporin
4.1 In Vitro Studies
Ophthalmic administration of ciclosporin is a possible way to avoid adverse effects associated with systemic administration, such as elevated serum creatinine, hypertension and renal dysfunction.[73] To evaluate whether ophthalmic administration of ciclosporin is safe, ciclosporin toxicity was tested on cultured human corneal endothelial monolayer from a 9-month-old donor. These cells showed signs of proliferation, elongation and mitosis, with normal nuclei and no vacuolisation of the cell cytoplasm. After treatment of cells by addition of up to 1000 µg/L ciclosporin to the culture medium for up to 7 days, no degenerative vacuoles appeared in the cytoplasm. The cells maintained normal morphology and showed mitotic cell divisions similar to those of untreated control cells.[74] Additionally, no adverse effects occurred in corneal stroma cell cultures exposed to higher concentrations of ciclosporin, from 100 to 250 µg/mL;[75] however, DNA synthesis in cultured epithelial cells was minimally decreased (10–15%) under these conditions.
4.2 Animal Studies
4.2.1 Topical Administration
The ocular safety of ciclosporin ophthalmic castor oil-water emulsions was evaluated by long-term ocular studies in rabbits and beagle dogs.[76] Ciclosporin ophthalmic formulations did not produce any ocular toxicity at concentrations up to 0.4% administered as many as six times daily for up to 6 months in rabbits and for up to 1 year in dogs; also, there were no ciclosporin-related histological changes in the eye.
Dogs with spontaneous KCS have a high incidence of ocular surface infection. When KCS dogs were treated with 2% ciclosporin twice daily for up to 1 year, there were no opportunistic corneal infections,[77] further supporting the safety of ocular use of ciclosporin.
4.2.2 Systemic Administration
Long-term oral toxicity studies of ciclosporin have been conducted in mice, rats and dogs. In three mouse and rat studies where ciclosporin was given orally, there were no macroscopic or microscopic eye findings, nor was there any evidence of toxicity-related pre-neoplastic or neoplastic events in the eye. At the same time, the dosages yielded serum and tissue concentrations sufficient for drug efficacy. Oral ciclosporin administration produced serum ciclosporin levels in the immunosuppressive range, up to 200 µg/L in mice[78] and up to 120–350 µg/L in rats.[79] In a similar 104-week study of oral administration in rats,[80] corneal ciclosporin concentrations ranged from 200 to700 ng/g for a 2 mg/kg/day group and from 500 to 900 ng/g for an 8 mg/kg/day group; corresponding conjunctival ciclosporin concentrations ranged from 700 to 2000 ng/g and from 1500 to 3000 ng/g.
In several long-term canine studies, oral ciclosporin dosages resulted in high concentrations in plasma and in tissues, but no ocular toxicity. Dogs given ciclosporin orally had plasma ciclosporin concentrations up to 5242 µg/L after 52 weeks.[79] In a similar study, dogs had corneal ciclosporin concentrations of 335 µg/L for a 15 mg/kg/day group and 2123 µg/L for a 45 mg/kg/day group, with corresponding conjunctival ciclosporin concentrations of 1296 and 4616 µg/L. Corresponding lacrimal gland ciclosporin concentrations were 13 028 and 9871 µg/L.[80] No ocular toxicity was observed in these canine studies, supporting the long-term ocular safety of ciclosporin.
4.3 Oral Administration in Humans
Many clinical trials have evaluated oral ciclosporin treatment of humans for ocular inflammation and immunological disorders (table IV). From 1984 to 1996, more than 550 patients used oral ciclosporin for periods of up to 44 months for treatment and up to 8 years of continuous follow-up, with only a handful of adverse events requiring the discontinuation of treatment. Of these, not one was related to the eye: four cases involved nephrotoxicity, three systemic hypertension, three nausea/malaise, and one gingivitis.
Among these studies, three were randomised, double-blind clinical trials. In a 1-year comparative, prospective trial of 56 patients with endogenous uveitis (excluding Behçet’s disease), patients received either ciclosporin 10 mg/kg/day (initial dosage) or prednisolone.[3] Although the ciclosporin group complained of more adverse effects, no complaints were related to the eyes and all were resolved with dose reduction.
In a second trial, 27 patients received either ciclosporin (10 mg/kg/day initially, with tapering over 1 year) plus prednisone, or placebo plus prednisone.[81] The ciclosporin group initially performed better than the placebo group, but the positive effect diminished as the dosage was reduced. The investigators concluded that ciclosporin was effective and may be considered in the treatment of uveitis. All adverse effects were systemic in nature and no ocular adverse effects were reported.
In a comparative trial of ciclosporin versus colchicine followed by an open-label extension, 96 patients with Behçet’s disease received either ciclosporin 10 mg/kg/day or colchicine 1 mg/day and were followed up for 16 weeks.[6] Weekly assessments included visual acuity, ocular manifestations (by slit-lamp microscopy, tonometry and funduscopy), systemic symptoms and the frequency of ocular attack. Ciclosporin produced improvement in 91% of patients with minimal adverse effects, whereas only 33% of colchicine-treated patients improved. The most serious adverse effect was renal dysfunction.
Results from other studies including uncontrolled prospective trials, retrospective chart reviews, and case studies (table IV) were generally consistent with those from the three randomised, double-blind studies.[3,6,81]
5. Systemic Drug Exposure and Safety after Topical Administration
5.1 Animals
Systemic drug exposure and safety after administration of ophthalmic ciclosporin castor oil-water emulsion were evaluated in rabbits and in beagle dogs.[76] Ciclosporin ophthalmic formulations at concentrations up to 0.4% did not produce any systemic toxicity when administered as often as six times daily for up to 6 months in rabbits and for up to 1 year in dogs. There were no ciclosporin-related histological changes in any organs or tissues. After administration of a 0.4% ciclosporin ophthalmic formulation, mean steady-state Cmax values of blood ciclosporin were 1.36 µg/L and 0.65 µg/L in rabbits and dogs, respectively. For comparison, oral administration to animals yielded plasma concentrations of ciclosporin ranging from 200 to 5000 µg/L (see section 4.2.2), approximately 200–5000 times the plasma ciclosporin concentrations after topical administration. Thus, systemic ciclosporin concentrations in rabbits and dogs after ocular administration of ophthalmic ciclosporin formulations are minimal in comparison with those after oral administration.
5.2 Humans
The extent of systemic ciclosporin exposure in humans after topical administration was evaluated in clinical studies in which patients received either 0.5% or 2% ciclosporin, in castor, olive or peanut oil (table III).[59,62,64,65] Ciclosporin could be detected in patients’ blood in only one[62] clinical study, and in that study the concentration was very low (4.7 µg/L).
Two clinical studies were conducted to evaluate the safety and systemic drug exposure of the ciclosporin castor oil-water emulsion formulation.[57,87] In these studies, the most common adverse event was ocular burning, and no serious adverse events were considered to be related to ciclosporin.
In the first clinical study, 162 dry-eye patients received placebo or ophthalmic 0.05%, 0.1%, 0.2% or 0.4% ciclosporin emulsion twice daily for 12 weeks.[57] Blood samples taken after 1, 4 and 12 weeks of treatment revealed that mean blood ciclosporin concentrations were below the LLOQ (0.1 µg/L) in all samples from the 0.05% and 0.1% treatment groups at all sampling times. The highest blood ciclosporin concentration measured in any patient from the 0.05% and 0.1% treatment groups was 0.102 µg/L. The highest blood ciclosporin concentration measured in any treatment group was 0.158 µg/L, from a patient who received 0.4% ciclosporin emulsion.[57]
The second clinical study involved ophthalmic treatment of dry-eye patients with the same ciclosporin concentrations in the same vehicle.[87] Predose blood samples were collected after 1 month of treatment from 113 dry-eye patients, after 6 months of treatment from 94 patients, and from 82 patients after 6–12 months of treatment. Serial blood samples were also taken during one 12-hour dosing interval from 26 patients after 9–12 months of treatment, to characterise blood ciclosporin concentration fluctuations within a single dosing interval at steady state and to quantitate Cmax. Out of 224 trough blood samples collected and 208 serial blood samples, only ten contained quantifiable ciclosporin (LLOQ 0.1 µg/L). All ten samples were from the 0.1% ciclosporin treatment group; the highest value was 0.299 µg/L. No quantifiable ciclosporin was detected in the blood of any patient receiving ophthalmic 0.05% ciclosporin emulsion in both eyes twice daily for up to 1 year.[87]
One drop of 0.05% ciclosporin emulsion in both eyes twice daily results in a total daily exposure of 0.057mg. By contrast, the daily oral ciclosporin dose for treatment of severe psoriasis recommended by the package insert of Neoral® (Novartis Pharmaceuticals Corp., East Hanover, NJ, USA) [2.5 mg/kg/day or about 190mg total for a 76kg patient][73] is 3000-fold greater. These doses result in mean steady-state blood Cmax and trough values of ciclosporin of 655 and 74.9 µg/L, respectively.[73] Similar amounts of ciclosporin, 2–3 mg/kg/day or 150–230 mg/day for a 76kg patient, are employed for systemic maintenance administration to treat intraocular inflammatory conditions such as uveitis.[4] Ciclosporin administration for transplant patients receiving systemic immunosuppressive therapy is designed to achieve trough blood ciclosporin concentrations of 20–100 µg/L. Consistent with the fact that daily topical doses are several thousand times less than daily oral doses, blood ciclosporin concentrations in humans after ocular instillation of ciclosporin emulsion (ranging from 0.10 to 0.299 µg/L) are orders of magnitude less than after oral administration.
5.3 Implications for Adverse Effects
Systemic exposure to ciclosporin after ocular administration of the ciclosporin castor oil-water ophthalmic formulation is minimal in humans, rabbits and dogs (sections 5.1 and 5.2). Therefore, the risk of nephrotoxicity and hypertension (hallmarks of systemic adverse effects associated with systemic ciclosporin treatment) is minimal for ophthalmic ciclosporin administration. The ocular safety of ciclosporin ophthalmic formulations has also been documented in human, rabbit and dog studies, obviating concerns about ciclosporin-related ocular infections.
6. Conclusion
Twice-daily instillation of 0.05% ciclosporin castor oil-water emulsion effectively delivers ciclosporin to surface ocular tissues at concentrations sufficient for immunomodulation. By contrast, topically administered ciclosporin penetrates intraocular tissues poorly, and twice-daily instillation of 0.05% ciclosporin emulsion results in plasma ciclosporin concentrations <0.1 µg/L, orders of magnitude below those found during systemic immunosuppressive therapies. In accordance with the low ciclosporin concentrations found in blood and in tissues other than those at the ocular surface, no systemic adverse effects were associated with topical ophthalmic ciclosporin treatment; nor were there any ocular adverse effects except for some mild, transient ocular discomfort. Because of its favourable safety profile and effective delivery of ciclosporin to affected target tissues, the 0.05% ciclosporin castor oil-water formulation appears to be a promising treatment for dry-eye disease.
Notes
The use of trade names is for product identification purposes only and does not imply endorsement.
References
Faulds D, Goa KL, Benfield P. Cyclosporin: a review of its pharmacodynamic and pharmacokinetic properties, and therapeutic use in immunoregulatory disorders. Drugs 1993; 45: 953–1040
DeBakey ME. Cyclosporin A: a new era in organ transplantation. Compr Ther 1984; 10: 7–15
Nussenblatt RB, Palestine AG, Chan CC, et al. Randomized, double-masked study of cyclosporine compared to prednisolone in the treatment of endogenous uveitis. Am J Ophthalmol 1991; 112: 138–46
Dick AD, Azim M, Forrester JV. Immunosuppressive therapy for chronic uveitis: optimising therapy with steroids and cyclosporin A. Br J Ophthalmol 1997; 81: 1107–12
Ozdal PC, Ortac S, Taskintuna I, et al. Long-term therapy with low dose cyclosporin A in ocular Behcet’s disease. Doc Ophthalmol 2002; 105: 301–12
Masuda K, Nakajima A, Urayama A, et al. Double-masked trial of cyclosporin versus colchicine and long-term open study of cyclosporin in Behcet’s disease. Lancet 1989; I: 1093–6
Le Hoang P, Girard B, Deray G, et al. Cyclosporine in the treatment of birdshot retinochoroidopathy. Transplant Proc 1988; 20: 128–30
Binder AI, Graham EM, Sanders MD, et al. Cyclosporin A in the treatment of severe Behcet’s uveitis. Br J Rheumatol 1987; 26: 285–91
Oh C, Apel AJ, Saville BA, et al. Local efficacy of cyclosporine in corneal transplant therapy. Curr Eye Res 1994; 13: 337–43
Ben Ezra D, Matamoros N, Cohen E. Treatment of severe vernal keratoconjunctivitis with cyclosporine A eyedrops. Transplant Proc 1988; 20: 644–9
Calonge M. The treatment of dry eye. Surv Ophthalmol 2001; 45 Suppl. 2: S227–39
Kiang E, Tesavibul N, Yee R, et al. The use of topical cyclosporin A in ocular graft-versus-host-disease. Bone Marrow Transplant 1998; 22: 147–51
Diaz-Valle D, Benitez del Castillo JM, Castillo A, et al. Immunologic and clinical evaluation of postsurgical necrotizing sclerocorneal ulceration. Cornea 1998; 17: 371–5
Gunduz K, Ozdemir O. Topical cyclosporin as an adjunct to topical acyclovir treatment in herpetic stromal keratitis. Ophthalmic Res 1997; 29: 405–8
Sall K, Stevenson OD, Mundorf TK, et al. Two multicenter, randomized studies of the efficacy and safety of cyclosporine ophthalmic emulsion in moderate to severe dry eye disease. CsA Phase 3 Study Group. Ophthalmology 2000; 107: 631–9
Stevenson D, Tauber J, Reis BL. Efficacy and safety of cyclosporin A ophthalmic emulsion in the treatment of moderate-to-severe dry eye disease: a dose-ranging, randomized trial. The Cyclosporin A Phase 2 Study Group. Ophthalmology 2000; 107: 967–74
Stern ME, Geo J, Siemasko KF, et al. Role of the lacrimal gland functional unit in the pathophysiology of dry eye. Exp Eye Res 2004; 78: 409–16
Pepose JS, Akata RF, Pflugfelder SC, et al. Mononuclear cell phenotypes and immunoglobulin gene rearrangements in lacrimal gland biopsies from patients with Sjogren’s syndrome. Ophthalmology 1990; 97: 1599–605
Pflugfelder SC, Wilhelmus KR, Osato MS, et al. The autoimmune nature of aqueous tear deficiency. Ophthalmology 1986; 93: 1513–7
Borel JF, Baumann G, Chapman I, et al. In vivo pharmacological effects of ciclosporin and some analogues. Adv Pharmacol 1996; 35: 115–246
Drosos AA, Skopouli FN, Costopoulos JS, et al. Cyclosporin A (CyA) in primary Sjogren’s syndrome: a double blind study. Ann Rheum Dis 1986; 45: 732–5
Laibovitz RA, Solch S, Andriano K, et al. Pilot trial of cyclosporine 1% ophthalmic ointment in the treatment of keratoconjunctivitis sicca. Cornea 1993; 12: 315–23
Power WJ, Mullaney P, Farrell M, et al. Effect of topical cyclosporin A on conjunctival T cells in patients with secondary Sjogren’s syndrome. Cornea 1993; 12: 507–11
Fox RI, Tornwall J, Maruyama T, et al. Evolving concepts of diagnosis, pathogenesis, and therapy of Sjogren’s syndrome. Curr Opin Rheumatol 1998; 10: 446–56
Kaswan RL, Salisbury MA, Ward DA. Spontaneous canine keratoconjunctivitis sicca: a useful model for human keratoconjunctivitis sicca: treatment with cyclosporine eye drops. Arch Ophthalmol 1989; 107: 1210–6
Kaswan RL, Salisbury MA. A new perspective on canine keratoconjunctivitis sicca: treatment with ophthalmic cyclosporine. Vet Clin North Am Small Anim Pract 1990; 20: 583–613
Morgan RV, Abrams KL. Topical administration of cyclosporine for treatment of keratoconjunctivitis sicca in dogs. J Am Vet Med Assoc 1991; 199: 1043–6
Olivero DK, Davidson MG, English RV, et al. Clinical evaluation of 1% cyclosporine for topical treatment of keratoconjunctivitis sicca in dogs. J Am Vet Med Assoc 1991; 199: 1039–42
Wiederholt M, Kossendrup D, Schulz W, et al. Pharmacokinetic of topical cyclosporin A in the rabbit eye. Invest Ophthalmol Vis Sci 1986; 27: 519–24
Kanai A, Alba RM, Takano T, et al. The effect on the cornea of alpha cyclodextrin vehicle for cyclosporin eye drops. Transplant Proc 1989; 21: 3150–32
Reidy JJ, Gebhardt BM, Kaufman HE. The collagen shield: a new vehicle for delivery of cyclosporin A to the eye. Cornea 1990; 9: 196–9
Calvo P, Sanchez A, Martinez J, et al. Polyester nanocapsules as new topical ocular delivery systems for cyclosporin A. Pharm Res 1996; 13: 311–5
De Campos AM, Sanchez A, Alonso MJ. Chitosan nanoparticles: a new vehicle for the improvement of the delivery of drugs to the ocular surface: application to cyclosporin A. Int J Pharm 2001; 224: 159–68
Gebhardt BM, Kaufman HE. Collagen as a delivery system for hydrophobic drugs: studies with cyclosporine. J Ocul Pharmacol Ther 1995; 11: 319–27
Borel JF. CsA: historical perspectives. Transplant Proc 1983; 15: 2219–29
Secchi AG, Tognon MS, Leonardi A. Topical use of cyclosporine in the treatment of vernal keratoconjunctivitis. Am J Ophthalmol 1990; 110: 641–5
Bonduelle S, Foucher C, Leroux JC, et al. Association of cyclosporin to isohexylcyanoacrylate nanospheres and subsequent release in human plasma in vitro. J Microencapsul 1992; 9: 173–82
Bonduelle S, Carrier M, Pimienta C, et al. Tissue concentration of nanoencapsulated radio-labelled cyclosporin following peroral delivery in mice or ophthalmic application to rabbits. Eur J Pharm Biopharm 1996; 42: 313–9
Belin MW, Bouchard CS, Frantz S, et al. Topical cyclosporine in high-risk corneal transplants. Ophthalmology 1989; 96: 1144–50
Restasis™ prescribing information. Irvine (CA): Allergan Inc., 2003
Acheampong AA, Shackleton M, Tang-Liu D, et al. Distribution of cyclosporin A in ocular tissues after topical administration to albino rabbits and beagle dogs. Curr Eye Res 1999; 18: 91–103
Snibson GR, Greaves JL, Soper ND, et al. Precorneal residence times of sodium hyaluronate solutions studied by quantitative gamma scintigraphy. Eye 1990; 4(Pt 4): 594–602
Bethem R, Lehman J, Woolley P, et al. Quantitative analysis of cyclosporin A in human whole blood by LC-API/MS/MS. Pharm Res 1999; 14: S–698
Kirchner GI, Vidal C, Winkler M, et al. LC/ESI-MS allows simultaneous and specific quantification of SDZ RAD and cyclosporine, including groups of their metabolites in human blood. Ther Drug Monit 1999; 21: 116–22
Schroeder TJ, Brunson ME, Pesce AJ, et al. A comparison of the clinical utility of the radioimmunoassay, high-performance liquid chromatography, and TDx cyclosporine assays in outpatient renal transplant recipients. Transplantation 1989; 47: 262–6
Simpson J, Zhang Q, Ozaeta P, et al. A specific method for the measurement of cyclosporin A in human whole blood by liquid chromatography-tandem mass spectrometry. Ther Drug Monit 1998; 20: 294–300
Steimer W. Performance and specificity of monoclonal immunoassays for cyclosporine monitoring: how specific is specific? Clin Chem 1999; 45: 371–81
Zucchelli GC, Pilo A, Chiesa MR, et al. Progress report of an external quality assessment scheme for cyclosporine assay. Ther Drug Monit 1996; 18: 273–9
Kaswan RL. Intraocular penetration of topically applied cyclosporine. Transplant Proc 1988; 20: 650–5
Mosteller MW, Gebhardt BM, Hamilton AM, et al. Penetration of topical cyclosporine into the rabbit cornea, aqueous humor, and serum. Arch Ophthalmol 1985; 103: 101–2
Bellot JL, Alio JL, Ruiz Moreno JM, et al. Corneal concentration and systemic absorption of cyclosporin-A following its topical application in the rabbit eye. Ophthalmic Res 1992; 24: 351–6
Ben Ezra D, Maftzir G. Ocular penetration of cyclosporin A: the rabbit eye. Invest Ophthalmol Vis Sci 1990; 31: 1362–6
Foets B, Missotten L, Vanderveeren P, et al. Prolonged survival of allogeneic corneal grafts in rabbits treated with topically applied cyclosporin A: systemic absorption and local immunosuppressive effect. Br J Ophthalmol 1985; 69: 600–3
Study report PK-98-074. Ocular cyclosporine distribution during 91/2 days of dosing of 0.05% and 0.1% 3H-cyclosporin A emulsion to albino rabbit eyes. Irvine (CA): Allergan, 1998. (Data on file)
Study report PK-99-073. Cornea, conjunctiva and aqueous humor concentrations in rabbits and dogs dosed every 15 minutes four times with an aqueous formulation of 0.5% 3H-cyclosporine. Irvine (CA): Allergan, 1999. (Data on file)
Study report PK-98-016. Ocular absorption and disposition in beagle dogs following multiple ocular doses of 0.2% 3H-cyclosporine emulsion. Irvine (CA): Allergan, 1996. (Data on file)
Acheampong AA, Shackleton M, Lam S, et al. Cyclosporine distribution into the conjunctiva, cornea, lacrimal gland, and systemic blood following topical dosing of cyclosporine to rabbit, dog, and human eyes. Adv Exp Med Biol 1998; 438: 1001–4
Study report PK-96-011. Dose proportionality of ocular tissue 3H-cyclosporine concentrations after a single dose administration of 0.05%, 0.2% and 0.4% cyclosporine emulsions into rabbit eyes. Irvine (CA): Allergan, 1996. (Data on file)
Theng J, Zhiou L, Tan D, et al. Distribution of cyclosporine A in the cornea after topical or oral administration. J Ocular Pharmacol Ther 2002; 18: 83–8
Althaus C, Dagres E, Reinhard T, et al. Cyclosporin-A and its metabolites in the anterior chamber after topical and systemic application as determined with high-performance liquid chromatography-electrospray mass spectrometry. Ger J Ophthalmol 1996; 5: 189–94
Perry HD, Donnenfeld ED, Acheampong A, et al. Topical cyclosporine A in the management of postkeratoplasty glaucoma and corticosteroid-induced ocular hypertension (CIOH) and the penetration of topical 0.5% cyclosporine A into the cornea and anterior chamber. CLAO J 1998; 24: 159–65
Pfau B, Kruse FE, Rohrschneider K, et al. Comparison between local and systemic administration of cyclosporin A on the effective level in conjunctiva, aqueous humor and serum [in German]. Ophthalmologe 1995; 92: 833–9
Chipont E, Diaz-Llopis M, Tomas S, et al. Collagen shields and intraocular penetration of cyclosporin. Arch Soc Esp Oftalmol 1995; 69: 251–7
Diaz-Llopis M, Menezo JL. Penetration of 2% cyclosporin eyedrops into human aqueous humour. Br J Ophthalmol 1989; 73: 600–3
Minguez E, Tiestos MT, Cristobal JA, et al. Intraocular absorption of cyclosporin A eyedrops [in French]. J Fr Ophtalmol 1992; 15: 263–7
Vickers AE, Fischer V, Connors S, et al. Cyclosporin A metabolism in human liver, kidney, and intestine slices: comparison to rat and dog slices and human cell lines. Drug Metab Dispos 1992; 20: 802–9
Combalbert J, Fabre I, Fabre G, et al. Metabolism of cyclosporin A: IV. Purification and identification of the rifampicin-inducible human liver cytochrome P-450 (cyclosporin A oxidase) as a product of P450IIIA gene subfamily. Drug Metab Dispos 1989; 17: 197–207
Madhu C, Dinh D, Babusis D, et al. Expression of cytochrome P450 isoenzymes in dog and human eye. Proceedings of the 9th Annual North American ISSX Meeting; 1999 Oct 24–28; Nashville. Bethesda (MD): ISSX 1999; 15: 162
Sandborn WJ, Lawson GM, Krom RA, et al. Hepatic allograft cyclosporine concentration is independent of the route of cyclosporine administration and correlates with the occurrence of early cellular rejection. Hepatology 1992; 15: 1086–91
Hanas E, Tufveson G, Lindgren PG, et al. Concentration of cyclosporin-A and its metabolites in transplanted human kidney tissue during rejection and stable graft function. Clin Transplant 1991; 5: 107–11
Sandborn WJ, Tremaine WJ, Lawson GM. Clinical response does not correlate with intestinal or blood cyclosporine concentrations in patients with Crohn’s disease treated with highdose oral cyclosporine. Am J Gastroenterol 1996; 91: 37–43
Sandborn WJ, Tremaine WJ, Schroeder KW, et al. Cyclosporine enemas for treatment-resistant, mildly to moderately active, left-sided ulcerative colitis. Am J Gastroenterol 1993; 88: 640–5
Physician’s desk reference. Montvale (NJ): Medical Economics, 2002: 2388-91
Singh G, Lindstrom RL, Doughman DJ. Cyclosporin A on human corneal endothelium. Cornea 1984; 3: 272–7
Ben Ezra D, Antebe I, Maftzir G. Differential effect of cyclosporin A on lymphocyte and keratocyte proliferation [abstract]. Invest Ophthalmol Vis Sci 1987; 28: 42
Angelov O, Wiese A, Yuan Y, et al. Preclinical safety studies of cyclosporine ophthalmic emulsion. Adv Exp Med Biol 1998; 438: 991–5
Salisbury MA, Kaswan RL, Brown J. Effect of topical cyclosporine on the recovery of micro-organisms from dogs with KCS [abstract]. Invest Ophthalmol Vis Sci 1994; 35: 1693
Ryffel B. The carcinogenicity of ciclosporin. Toxicology 1992; 73: 1–22
Donatsch P, Ryffel B. Pharmacokinetics of cyclosporine in toxicological studies. Transplant Proc 1986; 6: 71–6
Study report PK-00-013. Cyclosporine A concentrations in the eyes of rats and dogs dosed orally with cyclosporin A for 5 days. Irvine (CA): Allergan, 2000. (Data on file)
de Vries J, Baarsma GS, Zaal MJ, et al. Cyclosporin in the treatment of severe chronic idiopathic uveitis. Br J Ophthalmol 1990; 74: 344–9
Cohen E, Raz J, Maftzir G, et al. Low-dose cyclosporin A in uveitis. Ocul Immunol Inflamm 1993; 1: 195–201
Towler HM, Lightman SL, Forrester JV. Low-dose cyclosporin therapy of ocular inflammation: preliminary report of a long-term follow-up study. J Autoimmun 1992; 5 Suppl. A: 259–64
Towler HM, Whiting PH, Forrester JV. Combination low dose cyclosporin A and steroid therapy in chronic intraocular inflammation. Eye 1990; 4(Pt 3): 514–20
Towler HM, Cliffe AM, Whiting PH, et al. Low dose cyclosporin A therapy in chronic posterior uveitis. Eye 1989; 3(Pt 3): 282–7
Nussenblatt RB, Palestine AG, Chan CC. Cyclosporine therapy for uveitis: long-term followup. J Ocul Pharmacol 1985; 1: 369–82
Small DS, Acheampong A, Reis B, et al. Blood concentrations of cyclosporin a during long-term treatment with cyclosporin a ophthalmic emulsions in patients with moderate to severe dry eye disease. J Ocul Pharmacol Ther 2002; 18: 411–8
Acknowledgements
The authors are employees of Allergan Inc., manufacturer of Restasis™. This article is a scientific review of published literature.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tang-Liu, D.DS., Acheampong, A. Ocular Pharmacokinetics and Safety of Ciclosporin, a Novel Topical Treatment for Dry Eye. Clin Pharmacokinet 44, 247–261 (2005). https://doi.org/10.2165/00003088-200544030-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003088-200544030-00003