Abstract
Objective
To determine whether food intake influences the pharmacokinetics of a new, once daily, extended release (ER) capsule formulation of tolterodine in healthy volunteers, and to compare its bioavailability with that of the existing immediate release (IR) tablet.
Design
Open, randomised, 3-way crossover trial.
Participants
17 healthy volunteers (3 females, 14 males) aged between 19 and 50 years. With the exception of 1 male volunteer, all participants were classified as extensive metabolisers by cytochrome P450 2D6 genotyping.
Methods
Volunteers received single oral doses of tolterodine L-tartrate ER 8mg (2 × 4mg capsules) on an empty stomach or with a standardised high-fat breakfast. Reference therapy comprised tolterodine L-tartrate IR 4mg (2 × 2mg tablets), administered in the fasting state. Serum concentrations of tolterodine, its active 5-hydroxymethyl metabolite (5-HM) and the active moiety (sum of unbound tolterodine + 5-HM) were measured for up to 72 hours post-dose. Safety end-points were also determined.
Results
No effect of food on the bioavailability of tolterodine ER capsules was apparent and there was no sign of dose-dumping with meals. The geometric mean fed: fasting ratio of area under the serum concentration-time curve to infinity (AUC∞) of the active moiety, for all volunteers combined, was 0.95 (90% confidence interval 0.88 to 1.03). Equivalence with respect to AUC∞ (dose-corrected) was also found for the ER capsule compared with the IR tablet, although uncorrected maximum serum concentrations were around 50% lower despite the fact that the capsule dose was twice as high. Seven volunteers reported adverse events, predominantly headache. No volunteer reported dry mouth. Overall, there were no safety concerns.
Conclusions
The new ER formulation of tolterodine shows no pharmacokinetic interaction with food. On the basis of these results, patients with overactive bladder may, therefore, be advised to take the drug without regard to the timing of meals, maximising convenience during therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Tolterodine is the first antimuscarinic agent developed specifically for the treatment of patients with overactive bladder, a common and distressing medical condition characterised by symptoms of increased urinary frequency and urgency, with or without urge incontinence.[1,2] Numerous studies confirm the clinical efficacy and favourable tolerability of tolterodine in the treatment of patients with overactive bladder (for a review see Guay[3]). Moreover, in comparative studies, tolterodine 2mg twice daily has proved therapeutically equivalent to oxybutynin 5mg three times daily, but with superior tolerability.[4–6] This profile is attributed to the bladder selectivity of tolterodine observed in preclinical studies (for review see Nilvebrant[7]).
The pharmacokinetic profile of the current immediate release (IR) tablet formulation of tolterodine (Detrol™, Detrusitol®)[8] is characterised by rapid and virtually complete absorption after oral administration,[9] followed by high first-pass metabolism. Two major hepatic metabolic pathways have been identified: oxidation [mediated by cytochrome P450 (CYP) 2D6] and N-dealkylation (mediated by CYP3A).[10,11] The 5-hydroxymethyl metabolite (5-HM), produced by the CYP2D6 pathway, has a similar pharmacological profile to tolterodine with equivalent antimuscarinic potency in vitro.[12] However, since CYP2D6 is subject to genetic polymorphism,[13] individuals vary in the extent to which they are able to metabolise tolterodine. The majority utilises the CYP2D6 pathway (‘extensive metabolisers’), whereas the minor proportion (7% of Caucasians[14]) that lacks the CYP2D6 enzyme (‘poor metabolisers’) instead metabolise tolterodine via the CYP3A pathway to N-dealkylated tolterodine.[15] The half-life of tolterodine in extensive metabolisers is 2 to 3 hours with an absolute bioavailability of about 26%, compared with 8 to 12 hours and 91%, respectively, in poor metabolisers.[10] Higher serum concentrations of tolterodine are therefore observed in poor metabolisers, but 5-HM is virtually undetectable.
Even though the extensive and poor metaboliser pharmacokinetic profiles are different, exposure to the active moiety (sum of unbound tolterodine + 5-HM) is comparable regardless of metabolic phenotype. This is because tolterodine binds extensively to serum proteins [mainly α1-acid glycoprotein (AGP)] with an unbound fraction of 3.7%.[16] 5-HM, however, has an unbound fraction of 36%,[16] resulting in significantly higher concentrations of unbound 5-HM compared with tolterodine in extensive metabolisers.[10] Thus, the pharmacological effect is attributed to unbound tolterodine in poor metabolisers whereas in extensive metabolisers it is derived from the sum of unbound tolterodine and 5-HM, with the latter constituting the majority of the active moiety.[10] As exposure to the pharmacologically active moiety (i.e. unbound tolterodine in poor metabolisers; unbound tolterodine + 5-HM in extensive metabolisers) is similar irrespective of metabolic phenotype,[17] the same dosage can be used in all patients.
It is well established that food can affect the bioavailability of drugs.[18] In the case of the IR formulation of tolterodine, a previous study found increased serum tolterodine concentrations in the presence of food, although no clinically relevant effects on exposure to the active moiety were apparent.[19] The objective of this study was to assess the effect of food, by estimating the fed : fasting ratios for area under the serum concentration-time curve (AUC) and maximum observed serum concentrations (Cmax) of the active moiety, after the single dose oral administration of a new extended release (ER) capsule formulation of tolterodine for once daily treatment of patients with overactive bladder. A secondary objective was to evaluate bioavailability (with regard to the active moiety) of the ER capsule relative to the existing IR tablet formulation under fasting conditions, as part of an overall pharmacokinetic assessment of the new formulation. Safety and tolerability of the ER capsule formulation of tolterodine were also determined.
Subjects and Methods
On the basis of an assumed intra-individual coefficient of variation for AUC of 10% for the reference treatment (tolterodine IR), and that the true bioavailability for the test treatment (tolterodine ER) is 90%, it was estimated that a minimum of 16 participants would be required to show equivalence for tolterodine ER under fed and fasting conditions (α = 5%, 80% power).[20]
Study Design
This was a randomised, open, 3-way crossover study in 17 healthy volunteers (3 females, 14 males) aged between 19 and 50 years. All volunteers were in good health, as judged by their medical history and clinical, haematological and biochemical findings, with a body mass index of 18 to 29 kg/m2. Female volunteers, if premenopausal, were required to be using an adequate contraceptive method prior to and throughout the study. The use of oral hormonal contraceptives was permitted, given the lack of interaction between tolterodine and such agents.[21] Use of other concomitant medication was not permitted, except at the discretion of the investigator. Written informed consent was obtained from all volunteers before study commencement, the protocol having been approved by a local institutional review board. The study was performed in accordance with the latest revisions to the Declaration of Helsinki.
After completing a pretrial screening visit (at which blood samples were collected for CYP2D6 genotyping according to a modified technique of Dahl et al.[22]), volunteers were randomly assigned to 1 of 3 treatment sequences: a single dose of tolterodine ER 8mg (2 × 4mg capsules), under fed and fasting conditions, or tolterodine IR 4mg (2 × 2mg tablets) under fasting conditions. A 7-day washout period separated each administration. All doses of tolterodine were given orally (at between 08.00 and 09.00), under supervision of study personnel to ensure compliance, and are expressed as the L-tartrate salt. During the fed treatment period, volunteers took study medication immediately after consumption of a standardised high-fat breakfast [4255kJ (1017 kcal); 53% fat, 34% carbohydrate, 13% protein], which had to be eaten within 30 minutes. For the fasting treatment periods, volunteers fasted from 22.00 on the evening prior to administration and had lunch 4 hours after drug administration. All meals given during the volunteers’ stay at the clinic were standardised in terms of composition and timing of ingestion. Water was permitted ad libitum from 2 hours post-dose in each of the 3 treatment periods, and caffeine-containing beverages were allowed from 4 hours post-dose. The consumption of alcohol was not permitted from 48 hours prior to, and throughout, each treatment period. Volunteers were housed at the study clinic from the morning of administration until completion of blood sampling.
Venous blood samples were collected pre-dose and up to 72 hours post-dose to quantify tolterodine and 5-HM concentrations in serum. Timing of sampling varied according to formulation: ER capsule, at 0.5, 1, 2, 3, 4, 6, 9, 12, 18, 24, 30, 36, 42, 48, 54 and 60 hours after administration of tolterodine; IR tablets, at 0.25, 0.5, 0.75, 1, 1.5, 2, 3, 4, 6, 9, 12, 16, 20 and 24 hours after administration of tolterodine.
In poor metabolisers, with a longer half-life of tolterodine, further blood samples were drawn at 66 and 72 hours after administration of tolterodine ER, whereas additional samples at 32, 40, 48, 56, 64 and 72 hours post-dose were drawn following administration of the IR formulation. All blood samples (7ml) were collected into evacuated collection tubes without additives and allowed to coagulate for 45 minutes to 1 hour. Serum was subsequently separated by centrifugation, and samples stored frozen at −20°C until analysis.
Serum concentrations of tolterodine and 5-HM were determined using gas chromatography-mass spectrometry, as described in Palmér et al.[23] The accuracy and precision of the method were continuously determined during the study by the analysis of quality control samples. The interassay precision, expressed as the coefficient of variation, varied between 2.1 and 6.9% and the accuracy, expressed as the mean recovery of the theoretical quality control concentrations, varied between 98.6 and 101% for all analytes over the concentration range tested.
Adverse events were assessed by spontaneous reports and investigator observations throughout the study. The onset and intensity (mild, moderate or severe) of adverse events after drug administration were recorded as part of the investigator assessment of possible causality. Laboratory safety parameters (clinical chemistry and haematology) were assessed prior to and at the end of the study and screened for trends.
Pharmacokinetic Calculations
Pharmacokinetic calculations were performed by noncompartmental analysis using WinNonlin (Pharsight Corporation, Mountain View, California, USA). The following pharmacokinetic parameters of tolterodine and 5-HM were determined from the serum concentration-time profiles: AUC from time zero to infinity (AUC∞), Cmax, time to Cmax (tmax), minimum serum concentration at the end of the dosage interval (Cmin; i.e. 24 hours post-dose for the ER capsule and 12 hours post-dose for the IR tablet), and terminal half-life (t1/2z). Standard methods were adopted for the calculation of these parameters.[24]
Pharmacokinetic parameters were also calculated for the active moiety. The unbound fractions (fu) of tolterodine and 5-HM were calculated for each volunteer using the individual concentration of AGP (Pt) in pre-dose samples, and respective affinity constants (Ka) of tolterodine and 5-HM to AGP, using the following relationship:
The affinities of tolterodine and 5-HM for AGP were assumed to be 2.1 × 106 L/mol and 13 × 106 L/mol, respectively.[16] The AUC∞ of the active moiety was subsequently calculated as:
The corresponding calculation was also performed for Cmax, where Cmax,unbound was determined after calculation of unbound serum concentrations of tolterodine and 5-HM.
For the ER formulation, relative bioavailability (Frel) under fed versus fasting conditions and versus the IR tablet formulation (fasting) was estimated from AUC∞ ratios for the active moiety. Similar calculations were performed for AUC∞ of tolterodine and 5-HM. In the comparison of AUC∞ between ER and IR formulations, a correction was made for differences in dose, i.e. Frel = AUC∞,capsule/(AUC∞,tablet × 2). No such correction was made for comparison of Cmax ratios, which were also calculated for the active moiety, tolterodine and 5-HM.
Statistical Analysis
An analysis of variance (ANOVA) model was used for the statistical analysis of the log-transformed AUC∞ and Cmax data for tolterodine, 5-HM and the active moiety. The sources of variation, included as factors in the model, were participant, period and formulation. No carry-over effect was included in the model. From the ANOVA, geometric means of the fed : fasting ratio for the ER capsule, with the corresponding 90% confidence interval, were calculated. Similar calculations were performed for determination of Frel for ER capsule versus IR tablet under fasting conditions. Equivalence in AUC∞ values under fed and fasting conditions was assumed if the confidence interval was completely contained within 0.80 to 1.25, and for Cmax within 0.70 to 1.43. Descriptive statistics were calculated for other pharmacokinetic parameters.
Results
A total of 17 volunteers entered and completed the study; baseline demographics are shown in table I. Most volunteers were Caucasian (n = 14); the remainder were either Black (n = 2) or Oriental (n = 1). With the exception of 1 male volunteer, all volunteers were classified as extensive metabolisers by CYP2D6 genotyping. There were no protocol violations; all participants were therefore included in the analyses of pharmacokinetic variables and safety. Two volunteers received concomitant medication during the study, for the relief of cold symptoms and headache, respectively. No effect on the study findings was assumed.
Pharmacokinetic Findings
Median pharmacokinetics for tolterodine ER capsules and IR tablets are summarised for the active moiety in table II. Values for Frel confirmed equivalence in the fed and fasting state (table III). Similarly, the 90% confidence interval for the Cmax ratio was well within the required limits for equivalence (table III).
Median (range) pharmacokinetic parameters of the active moietya following single dose administration of either a new extended release (ER) capsule formulation of tolterodine, under fed and fasting conditions, or immediate release (IR) tolterodine tablets under fasting conditions, to 17 healthy volunteers
Geometric mean (90% confidence interval) ratios for pharmacokinetic parameters of the active moiety,a tolterodine and its active 5-hydroxymethyl metabolite.Values represent the ratios for the extended release (ER) capsule 8mg in the fed versus fasting state and relative to the immediate release (IR) tablet 4mg in the fasting state
Correcting for difference in dose, Frel values were consistent with equivalence (with respect to AUC∞) between the ER and IR formulations when administered in the fasting state (table III). Relative to the IR tablet, however, absolute Cmax values were reduced by about 50% for the ER capsule even though twice the dose was administered, whereas Cmin values were nearly 2-fold higher (table II).
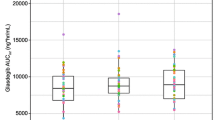
Median serum concentration-time profiles for tolterodine and 5-HM in the 16 extensive metabolisers, following administration of tolterodine ER capsules in the fed and fasting state, are shown in figure 1. Overall, the profiles were consistent with prolonged release of the drug over the entire 24-hour interval, and there was no indication of dose dumping with food. A summary of median pharmacokinetics for extensive metabolisers is provided in table IV. For both tolterodine and 5-HM, comparison between the 2 formulations administered in the fasting state showed lower median Cmax values and longer times to Cmax for the ER formulation (see figure 1), whereas t1/2z was increased. Median Cmin values were around 2- to 4-fold higher for the ER compared with the IR formulation.
Median serum concentration-time profiles of tolterodine and its active 5-hydroxymethyl metabolite (5-HM) in 16 extensive metabolisers following an 8mg single oral dose of an extended release (ER) capsule formulation of tolterodine (given as 2 × 4mg capsules) under fed and fasting conditions. For comparative purposes, the median serum concentration-time profiles for a 4mg single oral dose of conventional immediate release (IR) tablets of tolterodine (given as 2 × 2mg tablets) under fasting conditions is also shown.
Median (range) pharmacokinetic parameters of tolterodine and its active 5-hydroxymethyl metabolite in 16 extensive metabolisers following single dose administration of either a new extended release (ER) capsule formulation of tolterodine, under fed and fasting conditions, or immediate release (IR) tolterodine tablets under fasting conditions
Tolterodine pharmacokinetics in the 1 poor metaboliser were consistent with previous observations for this genotype, i.e. tolterodine concentrations were around 5- to 10-fold higher than in extensive metabolisers [Cmax values for this volunteer following administration of the ER (8mg) and IR (4mg) formulations were 39 nmol/L (ER fed), 30 nmol/L (ER fasting) and 118 nmol/L (IR), respectively] whereas 5-HM was undetectable. No food effect was apparent for this volunteer, consistent with the findings for extensive metabolisers.
Safety and Tolerability
All participants were included in the safety evaluation. Overall, 7 (41%) reported a total of 14 adverse events, all of which were of mild to moderate intensity and generally not deemed to be drug-related. The most common adverse event was headache. There were no reports of dry mouth, and no serious adverse events were reported. Overall, the incidence of adverse events for tolterodine ER in the fed and fasting states was similar (4 and 3 volunteers, respectively).
There were no trends towards clinically significant changes in laboratory safety parameters between screening and study completion.
Discussion
For any new drug formulation it is important to determine the level of interaction with food, as this can have a marked effect on drug bioavailability. Such studies are particularly relevant for ER formulations, as the presence of food can lead to the phenomenon of dose-dumping, which may have consequences for drug efficacy and safety. Moreover, the findings of such studies can have important implications for patients and disease management in general, as the requirement to take a medication 1 to 2 hours before a meal (because of a known interaction with food) can potentially lead to compliance problems. For a drug formulation aimed at the once daily treatment of patients with overactive bladder, a chronic condition that requires long term therapy to maintain symptom relief, the demonstration of no interaction with food would therefore allow patients to take the drug without regard to meals. In turn, convenience is maximised, which helps towards ensuring high levels of patient compliance and therefore good disease management.
The present study was therefore designed to evaluate the effect of food on the bioavailability of a new ER capsule formulation of tolterodine. For comparative purposes, volunteers also received a single oral dose of the existing IR formulation of tolterodine under fasting conditions. The administered doses of tolterodine (8mg ER; 4mg IR) were twice those normally given in routine clinical practice (i.e. 2mg twice daily)[8] in order to obtain adequate serum drug concentrations, especially in the terminal phase after administration of the ER formulation, for more accurate determination of AUC∞. Given that the pharmacokinetics of tolterodine IR exhibit dose proportionality in the range of 1 to 4mg,[25] and that Cmax values after 8mg ER did not exceed those after 4mg IR, backwards extrapolation of the present study findings to dosages relevant to clinical practice is justified.
Overall, the ER capsule showed the desired pharmacokinetic profile for once daily administration — prolonged release of the drug over the 24-hour interval. No effect of food on the bioavailability of tolterodine ER capsules was apparent, as shown by the AUC∞ and Cmax ratios for the active moiety (which approached unity). The absence of an effect of food on tolterodine ER pharmacokinetics contrasts with a previous food interaction study with the existing IR formulation.[19] In that study, a 50% increase in tolterodine concentrations was observed in the presence of food, with no change in 5-HM pharmacokinetics. However, the interaction was not deemed to be clinically relevant, as exposure to the activity moiety was unchanged. This is explained by the fact that unbound 5-HM constitutes the majority of the active moiety (in extensive metabolisers), such that changes in unbound tolterodine do not influence the sum. The increase in tolterodine concentrations when tolterodine IR is given with food may be attributable to physiological alterations induced by food, most probably the inhibition of the intrinsic ability of the liver to metabolise this highly extracted drug.[26] The hormonal response to feeding may explain this phenomenon.[27] However, the ER formulation does not show any notable differences in pharmacokinetic profile in the presence and absence of food, which can probably be explained by the slower and sustained release of tolterodine from this formulation coupled with the transient nature of the food effect. Similar findings have been observed for an ER formulation of the β-adrenoreceptor antagonist propranolol, in which no interaction with food was noted[28] although earlier studies with the conventional formulation had described reduction of first-pass hepatic metabolism by food.[29]
Pharmacokinetic findings for tolterodine, 5-HM and the active moiety were subject to pronounced inter-individual variability under both fed and fasting conditions in the present study. Such variability, however, is in accordance with previous pharmacokinetic studies with tolterodine.[9,10] In their study, for example, Brynne et al.[10] reported tolterodine Cmax values in the range of 1.9 to 43 nmol/L among extensive metabolisers, and 71 to 212 nmol/L in poor metabolisers, after treatment with tolterodine IR 4mg twice daily in healthy volunteers. Pronounced inter-individual variability in tolterodine, 5-HM and active moiety pharmacokinetics was therefore anticipated, and is unlikely to have affected the overall study findings.
Comparison of the pharmacokinetic profiles of the ER and IR formulations, administered at 8 and 4mg, respectively, shows major differences. For example, median t1/2z values for tolterodine ER were longer than those for the IR tablet, which can be explained by slow, continuous release of the drug from the new formulation. The most notable finding was that Cmax values were about 50% lower for tolterodine ER capsules compared with the conventional IR tablet formulation, despite the fact that the administered dose was twice as high. On the basis of dose proportionality, this difference in Cmax can also be expected at the regular therapeutic doses of 4mg (ER) and 2mg (IR), respectively. The implication of such findings is that, by decreasing the peaks in serum concentrations of tolterodine and 5-HM (and therefore also the active moiety) associated with the twice daily administration of the current IR tablet, the ER formulation may be associated with improved tolerability. This has been confirmed in a recent double-blind, randomised, placebo-controlled trial of tolterodine ER 4mg once daily in 1529 patients with overactive bladder, in which the frequency of dry mouth was 23% lower (p < 0.05) relative to tolterodine IR administered at 2mg twice daily.[30]
Another interesting pharmacokinetic finding for the ER formulation was that Cmin values for the active moiety were around 2-fold higher than those observed for the conventional tablet formulation. Thus, with multiple doses and the attainment of steady state, higher Cmin values would be expected. This has indeed been shown to occur in a repeat-dose study of tolterodine ER 4mg once daily in healthy volunteers.[31] Higher Cmin values appear to result in significantly improved efficacy for tolterodine ER 4mg once daily relative to the existing IR 2mg twice daily formulation, as observed in a recent comparative study of the 2 formulations in patients with overactive bladder.[30]
This study focused predominantly on extensive metabolisers, as only 1 poor metaboliser was enrolled. Pharmacokinetic findings for the latter individual were consistent with previous observations.[10,17] Thus, following administration of the IR tablet in the fasting state at a dose of 4mg, peak tolterodine concentrations (118 nmol/L) were comparable with the median Cmax observed in ‘poor metaboliser’ overactive bladder patients treated with tolterodine IR 4mg in dose-ranging studies [43 µg/L (132 nmol/L)].[17] Although the Cmax was around 10-fold higher compared with the median value for extensive metabolisers, exposure to the active moiety (in terms of AUC∞) in the poor metaboliser was within the range of exposure observed for those with the extensive metaboliser genotype. As for the latter group, no food effect was apparent for the ER formulation in the poor metaboliser. This was anticipated, as there is no reason to believe that conditions in the gastrointestinal tract would differ according to genotype.
Conclusion
Food intake has no effect on the bioavailability of tolterodine ER capsules, and there is no indication of dose-dumping when the drug is administered after a high-fat meal. The pharmacokinetic profile of this formulation is consistent with sustained release of the drug over a 24-hour period, thereby permitting once daily administration. Therefore, on the basis of these results, patients with overactive bladder may be advised to take the new ER formulation of tolterodine without regard to the timing of meals, maximising convenience and so improving compliance with long term therapy for this chronic condition.
References
Jackson S. The patient with overactive bladder: symptoms and quality of life issues. Urology 1997; 50(6A Suppl.): 18–22
Wein AJ, Rovner ES. The overactive bladder: an overview for primary care health providers. Int J Fertil 1999; 44: 56–66
Guay DRP. Tolterodine, a new antimuscarinic drug for treatment of bladder overactivity. Pharmacotherapy 1999; 19: 267–80
Appell RA. Clinical efficacy and safety of tolterodine in the treatment of overactive bladder: a pooled analysis. Urology 1997; 50(6A Suppl.): 90–6
Abrams P, Freeman R, Anderström C, et al. Tolterodine, a new antimuscarinic agent: as effective but better tolerated than oxybutynin in patients with an overactive bladder. Br J Urol 1998; 81: 801–10
Drutz H, Appell RA, Gleason D, et al. Clinical efficacy and safety of tolterodine compared to oxybutynin and placebo in patients with overactive bladder. Int Urogynecol J Pelvic Floor Dysfunct 1999; 10: 283–9
Nilvebrant L. The mechanism of action of tolterodine. Rev Contemp Pharmacother 2000; 11: 13–27
Physicians’ desk reference®. 54th ed. Montvale (NJ): Medical Economics Co. Inc., 2000: 2439–41
Brynne N, Stahl MMS, Hallén B, et al. Pharmacokinetics and pharmacodynamics of tolterodine in man: a new drug for the treatment of urinary bladder overactivity. Int J Clin Pharmacol Ther 1997; 35: 287–95
Brynne N, Dalén P, Alván G, et al. Influence of CYP2D6 polymorphism on the pharmacokinetics and pharmacodynamics of tolterodine. Clin Pharmacol Ther 1998; 63: 529–39
Postlind H, Danielson A, Lindgren A, et al. Tolterodine, a new muscarinic receptor antagonist, is metabolized by cytochromes P450 2D6 and 3A in human liver microsomes. Drug Metab Dispos 1998; 26: 289–93
Nilvebrant L, Gillberg P-G, Sparf B. Antimuscarinic potency and bladder selectivity of PNU-200577, a major metabolite of tolterodine. Pharmacol Toxicol 1997; 81: 169–72
Mahgoub A, Idle JR, Dring LG, et al. Polymorphic hydroxylation of debrisoquine in man. Lancet 1977; II: 584–6
Alván G, Bechtel P, Iselius L, et al. Hydroxylation polymorphisms of debrisoquine and mephenytoin in European populations. Eur J Clin Pharmacol 1990; 39: 533–7
Brynne N, Forslund C, Hallén B, et al. Ketoconazole inhibits the metabolism of tolterodine in subjects with deficient CYP2D6 activity. Br J Clin Pharmacol 1999; 48: 564–72
Påhlman I, Gozzi P. Serum protein binding of tolterodine and its major metabolites in humans and several animal species. Biopharm Drug Dispos 1999; 20: 91–9
Larsson G, Hallén B, Nilvebrant L. Tolterodine in the treatment of overactive bladder: analysis of the pooled phase II efficacy and safety data. Urology 1999; 53: 990–8
Welling PG. Interactions affecting drug absorption. Clin Pharmacokinet 1984; 9: 404–34
Olsson B, Brynne N, Johansson C, et al. Food increases the bioavailability of tolterodine but not effective exposure. J Clin Pharmacol 2001; 41: 1–7
Chow S-C, Liu J-P. Design and analysis of bioavailability and bioequivalence studies. New York (NY): Marcel Dekker, 1992
Pharmacia Corporation. Influence of tolterodine on the pharmacokinetics of Neovletta®, an oral contraceptive. An open, randomized, multiple-dose cross-over study in healthy volunteers [Document no. 9600483]. Stockholm: Pharmacia Corp. (Data on file)
Dahl ML, Johansson I, Palmertz MP, et al. Analysis of the CYP2D6 gene in relation to debrisoquin and desipramine hydroxylation in a Swedish population. Clin Pharmacol Ther 1992; 51: 12–7
Palmér L, Andersson L, Andersson T, et al. Determination of tolterodine and the 5-hydroxymethyl metabolite in plasma, serum and urine using gas chromatography-mass spectrometry. J Pharm Biomed Analysis 1997; 16: 155–65
Rowland M, Tozer TN. Clinical pharmacokinetics: concepts and applications. 3rd ed. Philadelphia (PA): Williams & Wilkins, 1995
Pharmacia Corporation. Dose proportionality of tolterodine. An open, randomized, single-dose cross-over study in healthy volunteers [Document no. 9600247]. Stockholm: Pharmacia Corp. (Data on file)
Tam YK. Individual variation in first-pass metabolism. Clin Pharmacokinet 1993; 25: 300–28
Semple HA, Tam YK, Coutts RT. A computer simulation of the food effect: transient changes in hepatic blood flow and Michaelis-Menten parameters as mediators of hepatic first pass metabolism and bioavailability of Propranolol. Biopharm Drug Dispos 1990; 11: 61–76
Byrne AJ, NcNeil JJ, Harrison PM, et al. Stable oral availability of sustained release Propranolol when co-administered with hydralazine or food: evidence implicating substrate delivery rate as a determinant of presystemic drug interactions. Br J Clin Pharmacol 1984; 17 Suppl. 1: 45S–50S
McLean AJ, Isbister C, Bobik A, et al. Reduction of first-pass hepatic clearance of Propranolol by food. Clin Pharmacol Ther 1981; 30: 31–4
Van Kerrebroeck P, Kreder K, Jonas U, et al. Tolterodine oncedaily: superior efficacy and tolerability in the treatment of the overactive bladder. Urology. In press
Olsson B, Szamosi J. Multiple dose pharmacokinetics of a new once daily, extended-release tolterodine formulation versus immediate release tolterodine. Clin Pharmacokinet. In press
Acknowledgements
This study was sponsored by Pharmacia Corporation. The authors wish to thank Nkechi Azie, Joy Wisser and Sharyn Cugnetti at the Pharmacia Clinical Research Unit, Kalamazoo, Michigan, USA, for the clinical conduct of the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Olsson, B., Szamosi, J. Food Does Not Influence the Pharmacokinetics of a New Extended Release Formulation of Tolterodine for Once Daily Treatment of Patients with Overactive Bladder. Clin Pharmacokinet 40, 135–143 (2001). https://doi.org/10.2165/00003088-200140020-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003088-200140020-00005