Abstract
Background: HMG-CoA reductase inhibitors, more commonly called statins, are widely used in the pharmacological management of hyperlipidaemias. The most common adverse drug reactions (ADRs) of statins are muscular. Other reported ADRs of statins along with other lipid-lowering drugs, namely fibrates, include erectile dysfunction (ED). The relationship between ED and exposure to statins has not clearly been established even though a number of significant case reports have associated ED with exposure to statins.
Objective: To investigate the association between exposure to statins and the occurrence of ED on the French Pharmacovigilance System Database.
Methods: Within the French Pharmacovigilance System Database, the case/ non-case method was used to measure the disproportionality of combination between a statin and ED. Cases are defined as those reports corresponding to the ADR of interest (i.e. ED) and non-cases are all reports of ADRs other than that being studied. The study period was from 1 January 1985 to 31 December 2006, limited to males aged 13–80 years. We estimated the association between ED and statins by calculating a reporting odds ratio (ROR) of exposure to each drug, with its 95% confidence interval (CI).
Results: Among the total of spontaneous reports selected (110 685), exposure to statins was identified in 4471 cases (4%), of which 51 reports (1.1%) concerned ED, whereas 431 (0.4%) cases of ED were found in the 106 214 reports without exposure to statins (p< 0.0001). The mean delay of onset of ED after starting statins, known for 19 cases, was 62 days (median 29 days). In 56.9% of cases, recovery occurred after withdrawal of statin, and rechallenge was positive in five cases.
The association was statistically significant for all statins (adjusted ROR [aROR] = 2.4; 95% CI 1.8, 3.3), simvastatin (aROR = 2.6; 1.6, 4.1), atorvastatin (aROR=3.4; 2.1, 5.4) and rosuvastatin (aROR = 7.1; 2.6, 19.4) [p < 0.001 for all] but not for pravastatin and fluvastatin. We did not find any relationship between the occurrence of ED and the daily dose or the duration of exposure to statins (data not shown). Assessment of the association between drugs other than statins known to be at risk of ED confirmed a significant association for finasteride (aROR= 14.5; 95% CI 8.3, 25.4), fibrates (aROR=3.6; 2.6, 5.1), b-adrenergic receptor antagonists (aROR=1.5; 1.01, 2.1) and tricyclic antidepressants (aROR = 2.0; 1.2, 3.4) [all p<0.05].
Conclusion: Despite some methodological limitations, the present study suggests that statins may induce or worsen ED in accordance with other data. Further pharmacoepidemiological studies are necessary to confirm this conclusion and to improve the precision of the prevalence and/or the risk factors of this ADR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
HMG-CoA reductase inhibitors, more commonly called statins, are widely used in the pharmacological management of hypercholesterolaemias and combined hyperlipidaemias.[1] Long-term studies have provided evidence of significant reductions of cardiovascular morbidity and mortality in patients exposed to some statins.[2,3] The most common adverse drug reactions (ADRs) of statins are muscular, such as rhabdomyolysis, myalgia or even dermatopoly-myositis.[1,4] Other reported ADRs of statins along with other lipid-lowering drugs, namely fibrates, include erectile dysfunction (ED).[5–9] A review of case series from the Spanish and French drug-monitoring systems identified a total of 75 cases reported spontaneously for various statins, with a positive rechallenge in five cases.[10] Therefore a case/non-case study was undertaken using the French Pharmacovigilance System Database to further investigate the association between exposure to statins and the occurrence of ED.
Methods
Data Collections
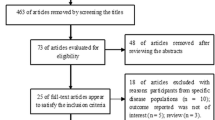
We used the French Pharmacovigilance System Database, which includes all ADRs reported to the French Regional Pharmacovigilance Centers since 1985. The reporting of ADRs has been compulsory in France since 1984. According to the law, physicians and pharmacists must report ’serious’ or ’unexpected’ ADRs to their regional pharmacovigilance centre (a total of 31 centres in France) to be registered in the national database. All reports are included in the database regardless of causality and seriousness level.[11] ADRs were coded according to the MedDRA (Medical Dictionary for Regulatory Activities) classifications. [12] For this study, the terms ‘impotence’, ‘erectile dysfunction’ or ‘dyserection’ were used. All statins marketed in France during the study period (pravastatin, simvastatin, fluvastatin, atorvastatin and rosuvastatin) were selected; cerivastatin was excluded because of its short period of marketing.
Case/Non-Case Method
The case/non-case method measures the disproportionality of combination between a drug and a particular ADR in a pharmacovigilance database. Many papers and regulatory agencies (e.g. UK Medicines Control Agency, WHO Drug Monitoring Center) have described different approaches to disproportionality for signal detection in spontaneous reporting. [13–15] Cases are defined as those reports corresponding to the ADR of interest (i.e. ED) and non-cases are all reports of ADRs other than that being studied. Exposure is considered as the presence in a report of the drug of interest (i.e. statins), whether or not it is suspected of causing the ADR. The method allows comparison of exposure to drug(s) of interest with all other drugs combined in the database and calculation of an ADR reporting odds ratio (ROR) or adjusted ROR (aROR) and its 95% confidence interval (CI).[16]
The study period was from 1 January 1985 to 31 December 2006. We applied the case/non-case method, comparing cases of ED with other cases of ADRs reported in the database regarding exposure to statins. Considering the characteristic of the ADR (ED), research on the French Pharmacovigilance System Database was limited to males aged 13–80 years. Moreover, the following data were collected from each report if available: age, body mass index, medical history (hypertension, cardiovascular disease, diabetes mellitus, other endocrinal diseases, depression, neuropathy and neurological impairment, alcoholism, smoking), delay of onset of ED after initiation of statin, outcome if statin was stopped and all other drug administration known to induce ED (ACE inhibitors, β-adrenergic receptor antagonists [β-blockers], fibrates, finasteride, centrally-acting antihypertensive agents, tricyclic antidepressants, antipsychotics) .[1]
Statistical Analysis
Data were analysed using STATA software, version 9.1 (Stata Corp LP, College Station, TX, USA). We estimated the association between ED and statins by calculating crude and adjusted RORs for statin exposure with the 95% CI. Other drugs well known to induce ED, as listed in the previous section, were used as positive controls to test the ability of the method to identify or recognize the association. For analysis of statininduced ED, we used two backward stepwise logistic regressions to calculate aROR. We ran a first regression model including all statins, which enabled evaluation of the association with the pharmacological class of statins. The second one aimed to analyse the association with each statin; other variables included in these models were clinical risk factors (such as arterial hypertension, cardiovascular diseases, diabetes) and drugs well known to induce ED. Because some patients could be exposed to more than one statin before the occurrence of the event (change of statins), we ran a single regression with one separate variable for each statin. The level of statistical significance was p<0.05.
Results
During the period of study, a total of 110 685 spontaneous reports were collected in the French Pharmacovigilance System Database for males aged from 13 to 80 years, of which 482 (0.43%) concerned drug-induced ED. Table I shows demographic characteristics and medical conditions as possible risk factors for ED of the patients with ED (cases) or without ED (non-cases). The frequency of arterial hypertension is significantly higher in patients with ED than those without ED.
Exposure to Statins
Among the 110 685 spontaneous reports selected from the database, 4471 (4%) involved the use of a statin. Of these 4471 reports involving a statin, 51 (1.1%) concerned ED. Furthermore, 431 (0.4%) cases of ED were identified in the 106214 reports not involving exposure to statins (p<0.0001). The mean delay of onset of ED after starting statins, known for 19 cases (37%), was 62 days (median 29; range 0–100 days): ED occurred in 25% of patients within 9 days and in 75% within 75 days after starting statins. In 56.9% of cases, recovery occurred after withdrawal of statin, and rechallenge was positive in five cases.
Table II illustrates the ROR and aROR for the occurrence of ED, for any statin and for each one separately; the association was statistically significant for any statin (aROR = 2.4 [95% CI 1.8, 3.3]), simvastatin (aROR = 2.6 [1.6, 4.1]), atorvastatin (aROR = 3.4 [2.1, 5.4]) and rosuvastatin (7.1 [2.6, 19.4]) [all p<0.001] but not for pravastatin or fluvastatin. We did not find any relationship between the occurrence of ED and the daily dose or the duration of exposure to statins (data not shown).
Assessment of the association between drugs other than statins known to induce ED confirmed a significant association for finasteride (aROR= 14.5 [95% CI 8.3,25.4]; p < 0.001), fibrates (aROR = 3.6 [2.6, 5.1]; p < 0.001), β-blockers (aROR =1.5 [1.01, 2.1]; p = 0.04) and tricyclic antidepressants (aROR = 2.0 [1.2, 3.4]; p = 0.009) [table III].
Regarding the risk of ED when statins are associated with other cardiovascular drugs known to induce this adverse effect (synergic action), we tested statins with three classes of cardiovascular drugs (b-blockers, fibrates, angiotensin II receptor antagonists). No significant difference was found between patients exposed to statins alone and those exposed to statins associated with β-blockers, fibrates or angiotensin II receptor antagonists (crude ROR was 0.7 [95% CI 0.2,1.6] for statins + β-blockers, 0 [0, 4.3] for statins + fibrates and 1.0 [0.6, 2.7] for statins + angiotensin II receptor antagonists).
Discussion
The relationship between ED and exposure to statins has not clearly been established even though a number of case reports have associated ED with statin exposure.[10,17–19] Approximately 50 spontaneous reports of statin-induced ED have also been collected by regulatory agencies (the Australian Adverse Drug Reaction Advisory Committee or UK Committee on Safety of Medicines).[19,20] Other data suggest the potential effect of atorvastatin to improve the responsiveness to sildenafil in men with ED via an increase in vascular sensitivity to sildenafil through nitrous oxide-mediated pathways.[21,22] Many factors may explain the difficulty in assessing the relationship between exposure to statin and ED: (i) ED is commonly associated with atherosclerosis of the penile vasculature;[23] (ii) over 50% of men attending routine cardiovascular disease clinics have some degree of ED prior to introduction of a statin;[24] (iii) many drugs used for the underlying risk factors of atherosclerosis (e.g. β-blockers, thiazide diuretics or ACE inhibitors) are established risk factors for ED.[25] Moreover, ED remains an under-reported ADR because patients often do not complain spontaneously about ED and doctors usually do not question them about sexual functioning.
According to the French Pharmacovigilance System Database, a significant association was found for exposure to statins and ED; 1.1% of spontaneous reporting involving statins concerned ED (51 of 4471) compared with 0.4% of cases of ED reported with drugs other than statins (431 of 106214). The analysis of each statin separately shows a significant association for simvastatin, atorvastatin and rosuvastatin. For fluvastatin, the association cannot be ruled out owing to the low number of cases (only two), since this drug remains rarely prescribed in France. On the contrary, for pravastatin, present results confirm our previous data suggesting that the risk of ED may be lower with pravastatin (reporting rate of 2.5 per 1 000000 male patient-years).[10]
Concerning the method used in this study, some limitations should be underlined. The collection of data was based on spontaneous reporting and therefore was limited by under-reporting, which could be more important for some particular ADRs, such as ED. Another limiting factor could be incomplete information for cases (medical history of patients, chronology of drug intake and outcome of ADR) that may be particularly important in ED, which is often multifactorial. A significant association was found for arterial hypertension, known as a risk factor for ED, but not for diabetes, with a significantly lower prevalence of diabetes in cases compared with non-cases. This is a surprising result, since diabetes is associated with hyperlipidaemias. Furthermore, the data of our previous analysis of the prevalence of diabetes and drug use on the French Pharmacovigilance System Database suggested a prevalence of 2.7%, very close to the prevalence of diabetes estimated in the French Health Insurance system claims database. [26] In our study, the selection of cases and non-cases was limited to male sex, which could perhaps explain the difference of results.
Regarding drugs involved in ED in the French Pharmacovigilance System Database, the results confirm a significant association for some drugs well known to lead to ED, such as finasteride (with a high ROR), β-blockers, fibrates or tricyclic antidepressants.[1] These results allow us to validate the present case/non-case approach using the French Pharmacovigilance System Database and identify a signal. This is in accordance with several other studies performed using the case/ non-case methodology in the French Pharmacovigilance System Database, suggesting its usefulness to detect a signal concerning drug safety in the context of real life.[27,28] Nevertheless, the ROR found for antipsychotics (aROR = 0.5 [95% CI 0.3, 0.96]) could be explained by difficulties in assessing the relationship between ED and psychotropic drugs because of the influence of psychiatric disorders on erectile function.[29]
ED was also reported with other lipid-regulating drugs such as fibrates.[19] Several hypotheses were suggested to explain this rare ADR. First, the decrease in cholesterol levels could affect testosterone synthesis and libido.[30] In vitro assays have shown that a high dosage of simvas-tatin could block synthesis of cholesterol by inhibition of the enzyme converting dehydroepiandrosterone o testosterone.[31] A moderate but significant decrease of free testosterone was found in eight patients treated with simvastatin for poly genic hypercholesterolaemia.[32] In addition, in familial hypercholesterolaemia, the low-density lipoprotein receptor is dysfunctional, which makes the Leydig cells more dependent on ‘de novo’ synthesis of cholesterol; moreover, statins were found in small quantities in the testes, where they could inhibit this de novo synthesis of cholesterol.[33] Another postulated mechanism was the lipophilicity of statin; simvastatin is highly lipophilic and hence could act centrally or induce peripheral neuropathy in the penile nerves. The results of our study show that the risk of ED may be lower with pravastatin, which is less lipophilic than other statins.[10] However, rosuvastatin, which has similar lipophilicity to pravastatin, was significantly associated with ED. As suggested by other authors, no relationship was found between dose or relative lipophilicity of the statins and the extent of ED.[34]
Taking into account the extensive use of lipid-regulating drugs, ED appears to be a rare ADR, although a high rate of under-reporting could be a bias for estimation of the prevalence. It could be a specific effect of statins that occurs in some patients with susceptibility, as suggested by some authors.[33] Exposure to statins could also be associated with worsening ED in patients with severe endothelial dysfunction due to established cardiovascular risk factors. [34]
Conclusion
Overall, despite some limitations, the present study suggests the association of exposure to statins with ED in accordance with other data cited above. It is interesting to note that the topic of a possible association between sexual disturbances and statins is being currently discussed at the European Medicine Agency. Further pharmaco-epidemiological studies (case-control studies) are necessary to confirm this conclusion and to improve the precision of the prevalence and/or the risk factors of this ADR.
References
Sweetman SC, editor. Martindale: the extra pharmacopoeia. 34th ed. London: Pharmaceutical Press, 2005
Walley T, Folino-Gallo P, Schwabe U, et al. Variations and increase in use of statins across Europe: data from administrative databases. EuroMedStat Group. BMJ 2004; 328: 385–6
Scandinavian Simvastatin Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Study (4S). Lancet 1994; 344: 1383–9
Vasconcelos OM, Campbell WW. Dermatomyositis-like syndrome and HMG-CoA reductase inhibitor (statin) intake. Muscle Nerve 2004; 30: 803–7
Halkin A, Lossos IS, Mevaorach D. HMG-CoA reductase inhibitor-induced impotence [letter]. Ann Pharmacother 1996; 30: 192
Schneider J, Kaffarnik H. Impotence in patients treated with clofibrate. Atherosclerosis 1975; 21: 455–7
Pizzarro S, Bargay J, D’Agosto P. Gemfibrozil-induced impotence [letter]. Lancet 1990; 336: 1135
Bharani A. Sexual dysfunction after gemfibrozil [letter]. BMJ 1992; 305: 693
Figueras A, Castel JM, Laporte JR, et al. Gemfibrozil-induced impotence [letter]. Ann Pharmacother 1993; 27: 982
Caraval A, Macias D, Sainz M, et al. HMG CoA Reductase inhibitors and impotence: two case series from the Spanish and French drug monitoring systems. Drug Saf 2006; 2: 143–9
Moore N, Noblet C, Kreft-Jais C, et al. French pharmaco-vigilance database system: examples of utilisation. Therapie 1995; 50: 557–62
Brown EG, Wood L, Wood S. The medical dictionary for regulatory authorities. Drug Saf 1999; 2: 109–17
Moore N, Thiessard F, Begaud B. The history of disproportionality measures (reporting odds ratio, proportional reporting rates) in spontaneous reporting of adverse drug reactions. Pharmacoepidemiol Drug Saf 2005; 14: 285–6
Evans SJ, Waller PC, Davis S. Use of proportional reporting ratios (PRRs) for signal generation from spontaneous adverse drug reaction reports. Pharmacoepidemiol Drug Saf 2001; 10: 483–6
Bate A, Lindquist M, Edwards IR, et al. Bayesian neural network method for adverse drug reaction signal generation. Eur J Clin Pharmacol 1998; 54: 315–21
van Puijenbroek EP, Bate A, Leufkens HGM, et al. A comparison of measures of disproportionality for signal detection in spontaneous reporting systems for adverse drug reactions. Pharmacoepidemiol Drug Saf 2002; 11: 3–10
Jackson G. Simvastatin and impotence. BMJ 1997; 315: 31
Boyd IW. HMG-CoA reductase inhibitor-induced impotence [letter]. Ann Pharmacother 1996; 30: 1199
Rizvi K, Hampson JP, Harvey JN. Do lipid-lowering drugs cause erectile dysfunction? A systematic review. Fam Prac 2002; 19: 95–8
Adverse Drug Reactions Advisory Committee. Simvastatin and adverse endocrine effects in men. Aust Adverse Drug React Bull 1995; 14: 10
Hermann HC, Levine LA, Macaluso J, et al. Can atorvastatin improve the response to sildenafil in men with erectile dysfunction not initially responsive to sildenafil? Hypothesis and pilot trial results. J Sex Med 2006; 2: 303–8
Bank AJ, Kelly AS, Kaiser DR, et al. The effects of quinapril and atorvastatin on the responsiveness to sildenafil in men with erectile dysfunction. Vasc Med 2006; 4: 251–7
Solomon H, Man JW, Jackson G. Erectile dysfunction and the cardiovascular patient: endothelial dysfunction is the common denominator. Heart 2003; 89: 251–3
Bruckert E, Giral P, Heshmati HM, et al. Men treated with hypolipidaemic drugs complain more frequently of erectile dysfunction. J Clin Pharm Ther 1996; 21: 89–94
Lewis RW. Epidemiology of erectile dysfunction. Urol Clin North Am 2001; 28: 209–16, vii
Berthet S, Grolleau S, Brefel-Courbon C, et al. Prevalence of diabetes in France and drug use: study based on the French Pharmacovigilance Database. Therapie 2007; 6: 483–8
Moore N, Kreft-Jais C, Haramburu F, et al. Reports of hypoglycaemia associated with the use of ACE inhibitors and other drugs: a case/non-case study in the French Pharmacovigilance System Database. Br J Clin Pharmacol 1997; 44: 513–8
Lugardon S, Lapeyre-Mestre M, Montastruc JL. Upper gastrointestinal adverse drug reactions and cyclo-oxygenase-2 inhibitors (rofecoxib and celecoxib): a case/non-case study from the French Pharmacovigilance Database. Eur J Clin Pharmacol 2004; 9: 673–7
Kaminetsky J. Epidemiology and pathophysiology of male sexual dysfunction. Int J Impot Res 2008; 20 Suppl. 1: S3–10
de Graaf L, Brouwers AH, Diemont WL. Is decreased libido associated with the use of HMG-CoA-reductase inhibitors? Br J Clin Pharmacol 2004; 3: 326–8
Smals AG, Weusten JJ, Benraad TJ, et al. The HMG-CoA reductase inhibitor simvastatin suppresses human testicular testosterone synthesis in vitro by a selective inhibitory effect on 17-ketosteroid-oxidoreductase enzyme activity. Steroid Biochem Mol Biol 1991; 38: 465–8
Azzarito C, Boiardi L, Vergoni W, et al. Testicular function in hypercholesterolemic male patients during prolonged simvastatin treatment. Horm Metab Res 1996; 28: 193–8
Jay RH, Sturley RH, Stirling C, et al. Effects of pravastatin and cholestyramine on gonadal and adrenal steroid production in familial hypercholesterolaemia. Br J Clin Pharmacol 1991; 32: 417–22
Solomon H, Samarasinghe YP, Feher MD, et al. Erectile dysfunction and statin treatment in high cardiovascular risk patients. Int J Clin Pract 2006; 60: 141–5
Acknowledgements
We are grateful for the helpful comments and assistance of Ms Jessica Yeung Shut-Yee, University of Texas Health Science Center, MD Anderson Cancer Center, Houston, TX, USA, who reviewed the draft versions of the manuscript. ## No funding was received for the preparation of this study. The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Do, C., Huyghe, E., Lapeyre-Mestre, M. et al. Statins and Erectile Dysfunction. Drug-Safety 32, 591–597 (2009). https://doi.org/10.2165/00002018-200932070-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200932070-00005