Abstract
Introduction: Monitoring was required for the introduction of non-chlorofluorocarbon (CFC) propellants in metered dose inhalers (MDIs) to ensure that there were no unexpected adverse events due to the new products. A postmarketing surveillance study has been conducted to evaluate the introduction of the MDI Seretide Evohaler™ (hydrofluoroalkane-134a inhaler containing salmeterol and fluticasone propionate).
Objectives: To summarise the modified prescription-event monitoring (PEM) study conducted to evaluate the introduction of Seretide Evohaler™ and discuss the relevance of this type of study towards pharmacovigilance risk-management planning.
Methods: Modified PEM methodology was used to examine the introduction of Seretide Evohaler™ into general practice in England. Patients were identified from the first National Health Service prescriptions dispensed in England for Seretide Evohaler™. One postal questionnaire was sent to the prescribing doctor, requesting demographic information, severity of the indication, concomitant medication for this condition, smoking history, event data 3 months prior to and 3 months after the first prescription for Seretide Evohaler™ and also reason for stopping if it had been stopped. Pregnancies, deaths and selected events were followed up. Incidence density ratios were calculated to compare event rates 3 months prior to and 3 months after the introduction of Seretide Evohaler™. A matched cohort analysis examined oral corticosteroid use and hospital admissions between the pre-and post-exposure periods.
Results: The cohort comprised 13 464 patients prescribed Seretide Evohaler™, with a response rate of 62%. There was no significant difference in the length of courses of oral corticosteroid use when the pre-and post-exposure periods were compared. A matched cohort analysis showed there was no increase in the use of oral corticosteroids (relative risk [RR] 0.95; 95% CI 0.90, 0.99) or hospital admissions in the post-exposure period (RR 0.87; 95% CI 0.73, 1.04). When the number of patients with events were compared for the periods 3 months before and 3 months after exposure, fewer events were reported in the post-exposure period. There were 64 patients who experienced adverse events within an hour of using Seretide Evohaler™, including one report of paradoxical bronchospasm and one of myocardial infarction with fatal outcome that were both assessed as possibly related to treatment.
Discussion: The results of the study suggest that the introduction of Seretide Evohaler™ was generally well tolerated. The modified methodology has allowed a comparison of the event rates before and after the introduction of this CFC-free inhaler into general practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The phasing out of chlorofluorocarbon (CFC)-containing products to protect the environment as a result of the Montreal protocol[1] has led to the reformulation of pressurised metered dose inhalers (MDIs) with new propellants, including the hydro-fluoroalkane (HFA)-134a.[2–5] Preclinical toxicological tests and clinical studies established HFA-134a as a safe alternative to CFCs.[2–5] However, these studies are limited by the small number of patients evaluated, and it was unknown whether the introduction of HFA-134a-containing products could result in unexpected safety hazards.[6]
To ensure the safe introduction of these products into the market, the European Commission made specific recommendations for studying the safety of these products postmarketing.[6] The European Medicines Agency (EMEA) also produced specific guidelines for the conduct of postmarketing surveillance studies for MDIs.[7] These recommendations provide a good example for using pharmacoepidemiological studies for risk-management planning and predated the International Conference on Harmonisation (ICH) E2E guidelines for pharmacovigilance planning, which provide guidance on producing the safety specification and the pharmacovigilance plan.[8]
The Drug Safety Research Unit (DSRU) conducted a modified prescription-event monitoring (PEM) study on Seretide Evohaler™Footnote 1in response to a regulatory request to the manufacturers. Seretide Evohaler™ is a combination product containing the corticosteroid fluticasone propionate and the long-acting β-adrenoceptor agonist salmeterol, with the propellant HFA-134a. Standard PEM methodology was modified to enable the examination of events that occurred 3 months pre-exposure and 3 months post-exposure to Seretide Evohaler™. PEM is well suited for examining the introduction of Seretide Evohaler™ because patients are identified from dispensed prescriptions and represent ‘real world’ use of these products in general practice in England.[9] In particular, using this methodology would allow an examination of the effects in children and other populations with limited information from clinical trials, e.g. off-label use.
The safety profiles of fluticasone propionate and salmeterol are well established, as the products have been on the market in other formulations for a number of years. A dry-powder inhaler, Seretide Accuhaler™, was launched prior to Seretide Evohaler™ in 1999.[10] Commonly reported adverse events associated with fluticasone propionate include hoarseness and candidiasis,[11] and those related to salmeterol include headache, tremor, palpitations and muscle cramps.[12] A mixture of these symptoms has been reported in patients treated with the combination product.[11,13,14] As with all inhalation products, paradoxical bronchospasm has been reported to occur very rarely.[13] Corticosteroids, including fluticasone propionate, have been associated with adrenal suppression and caution is particularly urged at higher doses.[15,16] The increased risk of asthma-related deaths, particularly in African Americans, found in the SMART (Salmeterol Multicenter Asthma Research Trial) study,[17] as led to labelled warnings in the summary of product characteristics (SmPC).[12,18]
The efficacy of salmeterol/fluticasone propionate-MDIs containing HFA-134a has been demonstrated in clinical trials.[19,20] Although these studies showed that the safety profile of the product was equivalent to other formulations, it was necessary to ensure that this translated into clinical practice. The objectives of this paper are to summarise the modified PEM study conducted to evaluate the introduction of Seretide Evohaler™ and discuss the relevance of this type of study towards pharmacovigilance risk-management planning.
Methods
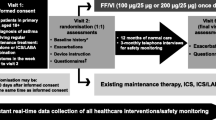
The PEM study for Seretide Evohaler™ was conducted using a modified methodology. The technique of PEM has been described elsewhere.[9] The main difference from standard PEM studies was that the questionnaires were designed to gather information on the pre-and post-exposure periods to allow a comparison of 3 months before and 3 months after the patient started the medication under investigation. PEM is a non-interventional cohort technique in which patients are identified from dispensed National Health Service (NHS) prescriptions written by general practitioners (GPs) in England. Information on prescriptions was supplied in confidence by the Prescription Pricing Division (PPD) of the NHS Business Services Authority (formerly the Prescription Pricing Authority). Dispensed prescriptions for all strengths of Seretide Evohaler™ were used to identify patients who were issued the CFC-free inhaler between June 2000 and April 2001.
Questionnaires were posted to the prescribing doctor approximately 6 months after the DSRU was notified of the first prescription for an individual patient. Only one questionnaire was sent per patient, and the study cohorts were formed from those patients for whom the GP had returned a questionnaire containing relevant information. The questionnaires requested information on the patient’s age, the indication and its severity, smoking history, the date and duration of courses of oral corticosteroids (if needed) over the 6-month period, concomitant respiratory medication, spacer use, reasons for stopping if the inhaler had been stopped, suspected adverse drug reactions (ADRs), and events 3 months prior to and 3 months following the first prescription for the study drug. GPs were also asked to report any events that occurred within an hour of taking the study medication to try and identify any events associated with the new product. The term ‘event’ in this modified PEM study was defined as including any new diagnosis, any reason for referral to a consultant or admission to hospital, any unexpected deterioration (or improvement) in their chest disease or a concurrent illness, any suspected drug reaction, any alteration of clinical importance in laboratory values or any other complaint that was considered of sufficient importance to enter the patient’s notes.
Patients were eligible for inclusion into the study if the GP indicated that patients had used the medication and were registered at the practice. If patients had a start date prior to the launch of the product in the UK, they were excluded unless there was information to confirm earlier use of the product. Where there was any discrepancy between the start date given by the GP and PPD, the latter was used. All events reported on the questionnaires were coded onto the computer using the DSRU dictionary, which is arranged hierarchically by system-organ class.
Reasons for stopping treatment and suspected ADRs were reviewed in detail. Where further information on selected events was required, additional questionnaires were sent to the prescribing GP. Further information was also sought on the outcome of pregnancies, and deaths where the date or cause was not specified.
Causality assessments were conducted for events for which follow-up information was available or if sufficient information had been provided on the green form. The DRSU conducts causality assessments using a similar system as the WHO, with the following four assessment categories: ‘probable’, ‘possible’, ‘unlikely’ and ‘not assessable’. When causality assessments were made between the study medication and a particular event, the following factors were taken into account: the time to onset, past medical history, concurrent illnesses, concomitant medications, whether the event was a reason for stopping and if so whether it resolved, the effect of rechallenge if taken again, pharmacological plausibility, or whether the GP specified an alternative cause.[21] Assessments were made by the senior research fellow and medically trained research fellows, with the director of the DSRU arbitrating any differences.
To enable the detection of differences in event rates of a minimum 2/1000 (baseline 1/1000 and on treatment 3/1000) with power of 80%, at a significance level of 99%, we needed to include at least 12 634 users of Seretide Evohaler™. The aim of the study was to try and include 66% on 25μg/125μg and 25μg/250μg Seretide Evohaler™ and 33% on lower strength 25μg/50μg Seretide Evohaler™.Footnote 2
Incidence densities (IDs) were calculated for a given time period for all events during treatment for patients for whom either the date of stopping the drug was known or who continued to take it until the end of the 3-month exposure period. IDs were calculated for all events that occurred in the first month after starting treatment (ID1), for the second and third months after starting treatment (ID2–3), for the overall treatment period (IDT), and for the 3-month baseline period (IDB). Results are presented as ID per 1000 patient-months of treatment. The difference between the proportion of patients with events (and 95% CIs) in the pre-and post-exposure periods was calculated using STATA (StataCorp, College Station, TX, USA). Additionally, a matched-cohort analysis was conducted to compare the use of oral corticosteroids and hospital admissions between the pre-and post-exposure periods. To compare event rates pre-and post-exposure, crude incidence density ratios (IDRs) with 95% CIs were calculated using a Poisson rate model using StatXact 5 (Cytel Software Corporation, Cambridge, MA, USA). IDRs were calculated for ID1/IDB, ID2–3/IDB, and IDT/IDB.
This study was conducted in accordance with the International Guidelines for Biomedical Research prepared by the Council for International Organizations of Medical Sciences (CIOMS) in collaboration with the WHO.[22] PEM also complies with the Guidelines on the Practice of Ethics Committees in Medical Research Involving Human Subjects, as issued by the Royal College of Physicians for records based research.[23] At the time of the study, PEM was listed in the Multicentre Research Ethics Committee guidelines for researchers (Appendix C) as a method of enquiry and survey conducted in the interest of the public that does not need reference to an ethics committee. The DSRU is now included in the ‘Frequently Asked Questions’ section of the General Medical Council booklet, ‘Confidentiality: Protecting and Providing Information’, as “a professional organisation that monitors the safety of medicines to which doctors should provide relevant information from patients’ records wherever possible.”[24]
Results
Total Cohort
Questionnaires were sent to 25 432 patients; 15 756 (62.0%) were returned of which 13 464 were valid (see table I for cohort information). Females accounted for 52.2% of the cohort, and 44.3% were male. At the time of marketing, Seretide Evohaler™ was only recommended for children aged ≥12 years, and 826 patients (6.1 % of cohort) were younger than this age. However, the product information has been updated since to recommend the use of the lowest strength in children aged ≥4 years.[18]
Asthma is the only licensed indication and it was the only and primary indication for use in 11 242 (83.5%) of patients. Chronic obstructive pulmonary disease (COPD) was given as a primary indication or for part of the indication for 1864 (13.8%) patients. Details of the dose prescribed stratified by the severity of disease are provided in table II; of the patients graded as severe, 56% were using the highest strength (25μg/250μg). A total of 397 adults graded as severe were given the lowest strength (25μg/50μg); however, according to the SmPC, these adults should have been given the highest dose.[13] During the entire study period, there were 681 patients reported to have used Seretide Accuhaler™, for 412 patients this was specified to be prior to starting Seretide Evohaler™.
The use of oral corticosteroids is a marker for deterioration in asthma control; therefore, it was important to determine whether there was any alteration in oral corticosteroid use after the introduction of Seretide Evohaler™. During the entire study period, 27.9% of the cohort required one or more courses of oral corticosteroids. The highest proportion of patients requiring oral corticosteroids were those graded as severe 48.4% (1231 patients), compared with 12.4% (197 patients) with mild disease and 24.8% (2299 patients) with moderate disease. The relative risk (RR) for oral corticosteroid use tended towards there being no difference between the pre-and post-exposure periods with increasing severity of disease (see table III). Patients with mild disease (RR 0.83; 95% CI 0.66, 1.04) showed the largest difference towards there being more use of oral corticosteroids in the pre-exposure period, and for patients with moderate disease (RR 0.90; 95% CI 0.84, 0.96), this difference was significant. In patients with severe disease (RR 1.05; 95% CI 0.97, 1.13), no difference was observed between the pre-and post-exposure periods. When the pre-and post-exposure periods were compared, there was no difference in the length of courses of oral corticosteroids (Pearson chi-squared [χ2] test with 2 degrees of freedom, p = 0.649). For hospital admissions, no obvious differences were found for the rates pre-and post-exposure, regardless of severity.
After exposure to Seretide Evohaler™, there were 3854 (28.6% of cohort) patients who regularly used a spacer; however, for 25.3% of the cohort spacer use was either not known or not specified. Of those for whom severity was known, increased spacer use was found with increasing severity of disease; mild 22.0% (349 of 1584 patients), moderate 27.6% (2550 of 9253 patients) and severe 36.8% (938 of 2546 patients).
Within 3 months, 1654 patients (12.3% of cohort) had stopped Seretide Evohaler™, and for 290 of these patients no reason for stopping was specified. For the remaining 1364 patients, there were 1462 reasons for stopping. The most common reasons for stopping were not effective (279 patients; 2.1% cohort), patient request (268; 2.0%), condition improved (165; 1.2%) and non-compliance (96; 0.7%). There was one report of paradoxical bronchospasm within an hour of using Seretide Evohaler™ given as a reason for stopping; however, the patient was subsequently restarted and there were no recurrences.
Adverse events
There were 33 events reported as suspected ADRs in 30 patients (0.2% of cohort). Eight of the suspected ADRs were reported to have occurred within an hour of using Seretide Evohaler™, one each of: headache, chest pain, palpitations, cough, breathlessness, increased shortness of breath/ wheeze in an asthmatic, choking and faintness, and stiffness and tingling with paraesthesia of fingers. The remaining events were also consistent with the known adverse-effect profile of Seretide Evohaler™ and included: muscle cramps, headache, palpitations, hoarseness, sore mouth and oral candiasis.[13]
The ten most commonly reported adverse events, with IDs and IDRs are shown in table IV. When the first month of exposure (ID1) was compared with prior exposure (IDB), ‘asthma worse’, cough, COPD, and ‘asthma/wheezing’ were all reported less frequently in the first month of exposure than in the 3 months before starting Seretide Evohaler™. These events as well as lower respiratory tract infections, dyspnoea and ‘non-surgical admissions’ were all reported less frequently during the entire treatment (IDT) period compared with prior to starting treatment (IDB). The adverse events reported to have occurred significantly more frequently in the first month and the first 3 months after exposure were: intolerance (ID1/IDB 39.59 [95% CI 9.91, 344.2], IDT/IDB 23.69 [95% CI 6.19, 201.6]); palpitation (ID1/IDB 2.47 [95% CI 1.22, 4.91], IDT/IDB 1.96 [95% CI 1.12, 3.50]); cramp (ID1/IDB 2.24 [95% CI 1.04, 4.72], IDT/IDB 1.88 [95% CI 1.05, 3.50]); and malaise/lassitude (ID1/IDB 1.84 [95% CI 1.12, 2.98], IDT/IDB 1.49 [95% CI 1.02, 2.21]).
The proportion of patients for whom at least one event was reported in the pre-exposure period (37.5%) was significantly greater than the post-exposure period (35.0%), with a difference of 2.5% (95% CI 1.37, 3.70). When these were analysed further to examine the effect of severity, for mildly (difference 3.9%; 95% CI 0.65, 7.13) and moderately severe disease (difference 2.6%; 95% CI 1.16, 3.94) there were more patients with events in the pre-exposure period. However, for patients with severe disease, there was no difference in the number of patients with events in the pre-and post-exposure periods (difference 1.6%; 95% CI —1.20, 4.34).
Information on events that occurred within an hour of use was requested to identify any events that may be associated with the product. There were 64 patients (0.5%) who had one or more events within an hour of using Seretide Evohaler™. Of these patients, 39 were followed up for further information, no replies were received for 12 patients and for four patients a blank questionnaire was returned. Table V lists those that were assessed as causally related to Seretide Evohaler™.
Details are provided on those cases thought to be particularly relevant to examining the safety of the new product. A case of ‘paradoxical bronchospasm’ was reported to have occurred within an hour of using Seretide Evohaler™ and assessed as possibly related to treatment; it is also described in the reasons for stopping section. Another patient was reported to have ‘bronchospasm’, which was followed up; however, no further information was received. Three cases involving choking were all assessed as possibly related to Seretide Evohaler™. One of these was reported as a choking sensation with a swollen uvula, and another as a choking sensation with faintness; however, on follow-up, the GPs did not confirm whether it had occurred within an hour for both of these cases. The condition was said to have resolved after stopping for two of the cases, and the outcome after stopping was not stated for the case of choking sensation with faintness. A patient experienced dyspnoea and was reported to be breathless after using Seretide Evohaler™ on the first 2 days of treatment; the condition resolved once it was stopped. There was a report of violent cough after using Seretide Evohaler™, the patient continued taking Seretide Evohaler™ but it made his wheezing worse and the drug was stopped. There was also a report of myocardial infarction with fatal outcome, which is described in the deaths section.
In addition to the events that occurred within an hour of taking Seretide Evohaler™, there were another 38 patients with events assessed as possibly related to Seretide Evohaler™. Other respiratory events were: deterioration in asthma; two reports of cough (with one of these queried by the GP as an allergic response to Seretide Evohaler™ propellant); and two patients experienced dyspnoea a week after starting Seretide Evohaler™. There was also a case of haemoptysis; although the GP thought it may also involve bleeding gums.
One case of allergy was assessed as possibly related to Seretide Evohaler™; it was described as puffy itchy eyes and occurred approximately 1 month after starting Seretide Evohaler™ in the winter.
In addition to the case described under deaths, there were two patients with myocardial infarctions assessed as possibly related to Seretide Evohaler™. In addition to the three patients who had palpitations within an hour of using Seretide Evohaler™, there were seven other patients with this event assessed as possibly related; palpitations is listed on the SmPC.[13] There were two reports involving atrial fibrillation, three of chest pain, one of left ventricular failure and one of angina that were assessed as possibly related to Seretide Evohaler™. Of these events, atrial fibrillation is listed on the SmPC.[13]
Other event terms that have not already been described, with cases assessed as possibly or probably related to Seretide Evohaler™ and not listed on the SmPC (excluding indication related events) are: ‘skin thinning’; burning sensation of the chest; numbness and tingling; dizziness; diplopia; sore watering eyes; blepharitis and rosacea; abdominal pain; diarrhoea and vomiting with visual disturbance; heartburn and chest pain (which occurred with headache). The remaining events assessed as possibly or probably related were consistent with the known safety profile of Seretide Evohaler™.[13,14,18]
Pregnancies
There were 59 pregnancies reported in the 3 months pre-and 3 months post-exposure to Seretide Evohaler™. Of these pregnancies, 41 were known to have been exposed to Seretide Evohaler™; 26 patients were initially exposed in the first trimester, six during the second trimester; eight during the third trimester, and with the remaining case it was not clear whether the patient was exposed during the first or second trimesters.
The outcomes of these pregnancies were known for 38 patients; there were 30 live births, four spontaneous abortions, one missed abortion and three elective terminations of pregnancy. Of the 15 pregnancies exposed during the first trimester with a known outcome of live birth, 12 were born at term and for the remaining three it was unknown. One baby born at term after an emergency caesarean section died at 13 days; the child was diagnosed with non-ketotic hyperglycaemia. One baby, whose length of gestation was not known, had systolic murmurs and a small ventricular septal defect but this had closed by 4 weeks. Another baby had three apnoeic attacks, which were thought to be secondary to ‘liquor aspiration’. A scan suggested a hydatiform mole for pregnancy that ended in missed abortion. The baby for whom it was unclear whether exposure had occurred during the first or second trimester was born with a small anterior fontalle following an emergency caesarean section and inhaled meconium but was reported to be otherwise well. A baby exposed initially during the second trimester had undescended right testes.
Deaths
There were 52 deaths reported in the 3-month post-exposure period, and for 39 of these patients it was known that they were taking Seretide Evohaler™ at the time of death, 2 were not taking Seretide Evohaler™ and for 11 it was not known. The cause of death was ascertained for 38 patients; 18 died from cardiovascular causes, 11 from respiratory causes, 8 from cancer and 1 from pancreatitis. None of the respiratory deaths were attributed to asthma; however, six patients died from COPD; the indication was COPD for three patients, asthma for two patients and one had asthma/COPD. With the exception of patients with cystic fibrosis the patients who died from respiratory causes were all >60 years (range 63–84 years).
An elderly patient (>65 years old) died from a myocardial infarction within an hour of using Seretide Evohaler™. The patient had no history of chest pain but was dyspnoeic and had smoked for several years but stopped about 1 month before the patient died. It was not known whether there was a family history of ischaemic heart disease. The DSRU assessed the association of this death with Seretide Evohaler™ as ‘possible’.
Use in Children
At the time the modified PEM study was conducted, Seretide Evohaler™ was not licensed for use in children aged ≤11 years.[13] However, it is now licensed for children aged ≥4 years at the lowest strength (25μg/50μg).[18] Of the 826 patients (6.13% of cohort) who were aged ≤11 years, 308 patients (37.3%) and 117 patients (14.2%) were prescribed the 25μg/125μg and 25μg/250μg strengths, respectively. The remaining patients were prescribed the lowest strength (25μg/50μg). Where it was specified, spacer use was required for 512 (62.0%) of the 826 children after exposure to Seretide Evohaler™. Only one child was reported to have an event within an hour of taking Seretide Evohaler™ and this was cough; however, no further information was obtained from follow-up. No events in this age group were reported as suspected ADRs, nor were there any deaths reported in children.
Use in Patients with Chronic Obstructive Pulmonary Disease
COPD represents off-label use of Seretide Evohaler™,[13] and there were 1864 patients (13.8% of cohort) who had COPD as an indication. COPD was the primary indication for 1440 patients (10.7%). There were 819 patients (43.9%) prescribed the highest strength of 25μg/250μg, 585 patients (31.4%) prescribed 25μg/125μg and 460 (24.7%) prescribed the lowest strength of 25μg/ 50μg. One or more courses of oral corticosteroids were required by 695 patients (37.3% of patients with COPD), which is higher than the proportion observed for the total cohort. A similar trend was observed to the whole cohort with increasing oral corticosteroid use being associated with increased severity of disease (18.4% mild patients, 31.5% moderate, 47.6% severe). There was no difference between the length of courses of oral corticosteroids (χ2 test with 2 degrees of freedom p = 0.883) when stratified between the pre-(567 courses) and post-(557 courses) exposure periods.
There were 246 patients (1.8%) with COPD as an indication who were reported to have stopped Seretide Evohaler™. There were seven patients (0.4%) who had an event reported within 1 hour of using Seretide Evohaler™, these were: dyspnoea, cough, palpitations, giddiness, asthma improved, wheeze worse/wheezing worse and increased shortness of breath/wheeze. There were eight reports of suspected ADRs in this group: one report of muscle cramps, two of palpitations, four events related to breathing worse and/or wheezing and a report of adverse effects on drug.
Discussion
This paper has summarised the results from a modified PEM study to examine the introduction of the CFC-free product, Seretide Evohaler™, into general practice in England. The study demonstrated that Seretide Evohaler™ was generally well tolerated.
The study has fulfilled the EMEA guidelines for conducting postmarketing surveillance studies for MDIs with CFC-free propellants (table VI).[7] As table VI demonstrates, the advantages of the modified PEM methodology were: the patients were identified from dispensed prescriptions, data were collected for the 3 months pre-and post-exposure and the information collected exceeded the minimum requirements. The study also allowed the identification of potential ADRs not attributed to the drug by the GPs since they were requested to provide event data irrespective of whether they thought these were related to the drug. Furthermore, the patients included in this cohort are likely to be representative of those who would be prescribed the drug in everyday clinical practice. They are therefore likely to represent a wide range of ages and include more patients with concurrent diseases or using concomitant medications than the highly selected patients found in clinical trials.
An important methodological aspect of this study is that it included a comparison (3 months before and after exposure to Seretide Evohaler™), which is an important development in the PEM method. A potential problem with changing/starting treatments is that patients may not respond as well to the new product and therefore have an exacerbation of asthma. When the pre-and post-exposure periods were compared there were fewer patients with events reported in the post-exposure period. When stratified by severity, this difference was maintained for those with mild and moderate disease, but no difference was observed for severe disease. The matched cohort analysis showed there was no increase in oral corticosteroid use or hospital admissions in the post-exposure period.
Only 62% of Seretide Evohaler™ questionnaires that were posted were returned, which may conceal biases if the patients of GPs who returned the questionnaires differed in some way to patients of GPs who did not. Nevertheless, the response rates are greater than the estimated rates of spontaneous reporting[25,26] and from GP surveys in general.[27] Another possible source of bias is incomplete or imprecise completion of original or follow-up questionnaires. Under-reporting including under-reporting of serious or fatal events was possible. While patients who had used Seretide Accuhaler™ were identified, there was not enough information to allow a detailed analysis of this subset of patients, in particular there was no information on dose. However, the focus of the study was to examine the safety of the propellant irrespective of whether patients were new-users or had switched from a pre-existing formulation.
Asthma is recognised to have seasonal variation in exacerbations of disease,[28] and a limitation of the current study is that although attempts were made to identify patients with prescriptions throughout the year, most of the patients had prescriptions issued between August 2000 and January 2001. Although we recognise that the indication-related events may have seasonal variation, the main focus of this study was to identify any previously unrecognised safety concerns. It is noteworthy that there were fewer respiratory events (asthma worse, cough, COPD, dyspnoea, asthma/wheezing and lower respiratory tract infections) when the post-exposure period was compared with the pre-exposure period, and with the timing of exposure an increase may have been expected. Asthma is itself variable and, while we recognise that a longer observation period may have been needed to fully evaluate the variability of the disease and acute exacerbations of asthma, it was beyond the scope of this study because our objective was to investigate the short-term effects of the introduction of Seretide Evohaler™.
The study was successful in including >12 634 patients, including information on off-label use in children and patients with COPD. The data demonstrate that Seretide Evohaler™ appeared to be generally well tolerated in these populations. There were three strengths of inhaler available and it was hoped to get an even proportion of patients on each of the strengths; however, this was not possible because of differences in prescribing. There was selective posting of questionnaires to patients on 25μg/50μg Seretide Evohaler™ to try and achieve similar proportions to the patients initially prescribed the 25μg/ 125μg and 25μg/250μg strengths.
It was apparent that a number of patients with different forms of severity of the disease may have been receiving inappropriate doses; for example, a number of patients with severe disease were using the lowest strength of Seretide Evohaler™. It did also appear that a number of children were using higher than recommended strengths of inhaler, which is of concern given the effects of high-dose corticosteroids on adrenal suppression.[15,16,29–31] A specific warning on the use of high-dose fluticasone propionate in children was also issued by the Medicines and Healthcare products Regulatory Agency.[32] During the study, there were no reports of adrenal suppression or growth retardation; however, the duration of observation in our study was too short to detect such events. Another concern is that if children had switched from Seretide Accuhaler™ to an equivalent strength Seretide Evohaler™, they may have an increased delivery of the drugs to the lungs and therefore be exposed to a higher dose of the medication. Since dry-powder inhalers are reliant on the airflow produced by the patient, the optimum results of these inhalers cannot always be achieved by all asthmatic patients, in particular children.[33] However, no information was available on the strength of Seretide Accuhaler™ used.
The IDR analysis highlighted that ‘asthma worse’ and ‘asthma/wheezing’ were reported more frequently in the pre-exposure period than in the first month of exposure. This may in part be due to an exacerbation of the patients’ respiratory condition being the reason for prescribing the drug; ‘asthma improved’ was reported more frequently in the post-exposure period compared with the 3 months prior. Intolerance was reported more significantly in the first month and the total post-exposure period compared with the pre-exposure period, which may have occurred because some patients had used other respiratory medications for a long time prior to starting Seretide Evohaler™. Other adverse events reported more significantly in the first month and the whole post-exposure period were palpitation and cramp, which may be due to salmeterol;[12,14] ‘malaise/lassitude’ was also reported. The IDRs have not been adjusted for possible confounders such as severity of disease, smoking history, season or age.
It was important to identify whether there were any cases of paradoxical bronchospasm and determine whether there was a trend for these being associated with using Seretide Evohaler™. There was one case reported to have occurred within an hour of using Seretide Evohaler™ that was assessed as possibly related to treatment; however, when the drug was restarted it did not reoccur. It must be noted that there may be under-reporting of an event such as paradoxical bronchospasm. In particular, determining whether an event occurred within an hour of use requires this timing to have been reported by the patient and for this to be sufficiently documented in the patient’s medical record (or for it to be remembered by the GP).
Other reports related to paradoxical bronchospasm that occurred within an hour of treatment included three patients who experienced choking, a report of wheezing and another of breathlessness. A report of fatal myocardial infarction that occurred within an hour of using Seretide Evohaler™ was assessed as possibly related to treatment. There was also a report of an allergic reaction that was assessed as causally related to Seretide Evohaler™. A number of other events were also reported to have occurred within an hour of using Seretide Evohaler™, and eight of these were reported as ADRs. However, these events of concern only affected a small number of patients.
The results of this PEM study are consistent with other clinical studies that have demonstrated the safety of products delivered by the propellant HFA-134a.[19,20,34–37] However these studies were conducted on a small number of patients, whereas the PEM study had information on >13 000 patients. The majority of adverse events identified in this study are consistent with the known adverse effect profiles of corticosteroids and long-acting β-agonists.[14] However, a number of events assessed as causally-related to treatment were not listed on the SmPC.[13,18]
The pregnancy outcomes were similar in proportion to those found for other respiratory medications studied by PEM,[38] and a survey of the population.[39] There have been recent concerns about asthma related deaths in patients taking salmeterol;[17] in this PEM study no deaths were attributed to asthma. However, the cause of a number of deaths did remain unspecified.
The study was done as a result of a regulatory request to the manufacturer and provides an example of pharmacovigilance risk management. International guidelines were implemented specifically for transfer to CFC-free MDIs because it was recognised that there could potentially be a public health problem when new propellants were introduced to a large population over a short period of time.[6] The concept of these guidelines provide an example of pharmacovigilance planning, which has now been introduced formally as part of the ICH E2E guidelines, which were published in 2004.[8] The ICH E2E guidelines introduce the concepts that at the time of marketing, products have a pharmacovigilance specification and a pharmacovigilance plan.[40,41] The pharmacovigilance specification contains details about the known and unknown aspects of safety as well as the populations studied; and the pharmacovigilance plan describes the routine pharmacovigilance procedures and an action plan to address any safety issues or missing information as ,needed.[40,41] These can be seen as steps towards a more systematic approach to safety assessments in the postmarketing phase, as well as trying to anticipate and prepare for any potential safety issues.[42] While this modified PEM study predated the ICH E2E guidelines, it was conducted to identify any untoward effects of the new product when used in clinical practice. If at any stage during the conduct of the study any serious concerns regarding drug safety were identified, the DSRU would have informed the drug manufacturer.
Conclusion
The introduction of Seretide Evohaler™ was generally well tolerated when used in general practice in England. However, a small number of individuals experienced events of concern that were assessed as causally related to Seretide Evohaler™. This study provides a useful example of pharmacovigilance planning to examine the introduction of a new propellant and the use of an observational study (a modified PEM study) to monitor the safety of the new product as part of a risk management plan. Information was also provided on the off-label use of Seretide Evohaler™ in children and patients with COPD.
Notes
1The use of trade names is for product identification purposes only and does not imply endorsement.
2Doses are stated as salmeterol/fluticasone propionate.
References
The Montreal protocol on substances that deplete the ozone layer. 2000 [online]. Available from URL: http://www.unep.org/ozone/Montreal-Protocol/Montreal-Protocol2000.shtml [Accessed 2006 Aug 23]
Ibiapina CC, Cruz AA, Camargos PA. Hydrofluoroalkane as a propellant for pressurized metered-dose inhalers: history, pulmonary deposition, pharmacokinetics, efficacy and safety [in Portuguese]. J Pediatr (Rio J) 2004; 80(6): 441–6
Leach CL. The CFC to HFA transition and its impact on pulmonary drug development. Respir Care 2005; 50(9): 1201–8
Gates BJ, Neumiller JJ. CFC Phaseout and Adances in Oral Inhalers. Advances in Pharmacy 2005; 3(2): 131–142, 155
Zeidler M, Corren J. Hydrofluoroalkane formulations of inhaled corticosteroids for the treatment of asthma. Treat Respir Med 2004; 3(1): 35–44
European Commission. European Community strategy for the phaseout of CFCs in metered dose inhalers, 1998 [online]. Available from URL: http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=CELEX:51998DC0603:EN:HTML [Accessed 2006 Aug 23]
European Agency for the Evaluation of Medicinal Products. Guideline for PMS studies for metered dose inhalers with new propellants. CPMP/180/95. 1995 [online]. Available from URL: http://www.emea.eu.int/pdfs/human/qwp/018095en.pdf [Accessed 2006 Sep 1]
International Conference on Harmonisation of Technical Requirements for Registration of Medicinal Products for Human Use. Pharmacovigilance planning E2E. 2004 [online]. Available from URL: http://www.ich.org [Accessed 2006 Aug 23]
Shakir SAW. Prescription-event monitoring. In: Strom BL, editor. Pharmacoepidemiology. 4th ed. Chichester, UK: John Wiley & Sons Ltd, 2005: 203–16
Allen & Hanburys. Seretide Accuhaler, summary of product characteristics. 2005
Allen & Hanburys. Flixotide Evohaler, summary of product characteristics. 2000
Allen & Hanburys. Serevent Evohaler, summary of product characteristics. 2006
Allen & Hanburys. Seretide Evohaler, summary of product characteristics. 2000
Reynolds NA, Lyseng-Williamson KA, Wiseman LR. Inhaled salmeterol/fluticasone propionate: a review of its use in asthma. Drugs 2005; 65(12): 1715–34
Macdessi JS, Randell TL, Donaghue KC, et al. Adrenal crises in children treated with high-dose inhaled corticosteroids for asthma. Med J Aust 2003; 178(5): 214–6
Todd GR, Acerini CL, Ross-Russell R, et al. Survey of adrenal crisis associated with inhaled corticosteroids in the United Kingdom. Arch Dis Child 2002; 87(6): 457–61
Nelson HS, Weiss ST, Bleecker ER, et al. The Salmeterol Multicenter Asthma Research Trial: a comparison of usual pharmacotherapy for asthma or usual pharmacotherapy plus salmeterol. Chest 2006; 129(1): 15–26
Allen & Hanburys. Seretide Evohaler, summary of product characteristics. 2005
Bateman ED, Silins V, Bogolubov M. Clinical equivalence of salmeterol/fluticasone propionate in combination (50/100 microg twice daily) when administered via a chlorofluorocarbonfree metered dose inhaler or dry powder inhaler to patients with mild-to-moderate asthma. Respir Med 2001; 95(2): 136–46
van Noord JA, Lill T, Carillo Diaz T, et al. Clinical equivalence of a salmeterol/fluticasone proprionate combination product (50/500ug) delivered via a chlorofluorocarbon-free metered-dose inhaler with the Diskus™ in patients with moderate to severe asthma. Clin Drug Invest 2001; 21(4): 243–56
Shakir SAW. Causality and correlation in pharmacovigilance. In: Talbot J, Waller P, editors. Stephens’ detection of new adverse drug reactions. 5th ed. Chichester: John Wiley & Sons Ltd, 2003: 329–43
CIOMS/WHO. International ethical guidelines for biomedical research involving human subjects. Geneva: CIOMS/WHO, 2002
Royal College of Physicians of London. Guidelines on the practice of ethical research involving human subjects. London: Royal College of Physicians of London, 1996
General Medical Council. Confidentiality: protecting and providing information. Frequently asked questions Q7. London: General Medical Council, 2004: 9
Heeley E, Riley J, Layton D, et al. Prescription-event monitoring and reporting of adverse drug reactions. Lancet 2001; 358: 1872–3
Martin RM, Kapoor KV, Wilton LV, et al. Underreporting of suspected adverse drug reactions to newly marketed (“black triangle”) drugs in general practice: observational study. BMJ 1998; 317(7151): 119–20
Templeton L, Deehan A, Taylor C, et al. Surveying general practitioners: does a low response rate matter? Br J General Pract 1997; 47: 91–4
Fleming DM, Cross KW, Sunderland R, et al. Comparison of the seasonal patterns of asthma identified in general practitioner episodes, hospital admissions, and deaths. Thorax 2000; 55: 662–5
Wong JY, Zacharin MR, Hocking N, et al. Growth and adrenal suppression in asthmatic children on moderate to high doses of fluticasone propionate. J Paediatr Child Health 2002; 38(1): 59–62
Sim D, Griffiths A, Armstrong D, et al. Adrenal suppression from high-dose inhaled fluticasone propionate in children with asthma. Eur Respir J 2003; 21(4): 633–6
Visser MJ, van der Veer E, Ma DS, et al. Side-effects of fluticasone in asthmatic children: no effects after dose reduction. Eur Respir J 2004; 24(3): 420–5
CSM/MCA. Current problems in pharmacovigilance. 2001; 27: 10
Atkins PJ. Dry powder inhalers an overview. Respir Care 2005; 50(10): 1304–12
Nathan RA, Rooklin A, Schoaf L, et al. Efficacy and tolerability of fluticasone propionate/salmeterol administered twice daily via hydrofluoroalkane 134a metered-dose inhaler in adolescent and adult patients with persistent asthma: a randomized, double-blind, placebo-controlled, 12-week study. Clin Ther 2006; 28(1): 73–85 695
Nelson HS, Wolfe JD, Gross G, et al. Efficacy and safety of fluticasone propionate 44 microg/salmeterol 21 microg administered in a hydrofluoroalkane metered-dose inhaler as an initial asthma maintenance treatment. Ann Allergy Asthma Immunol 2003; 91(3): 263–9
Pearlman DS, Peden D, Condemi JJ, et al. Efficacy and safety of fluticasone propionate/salmeterol HFA 134A MDI in patients with mild-to-moderate persistent asthma. J Asthma 2004; 41(8): 797–806
You-Ning L, Humphries M, Du X, et al. Efficacy and safety of salmeterol/fluticasone propionate delivered via a hydrofluoroalkane metered dose inhaler in Chinese patients with moderate asthma poorly controlled with inhaled corticosteroids. Int J Clin Pract 2005; 59(7): 754–9
Wilton LV, Pearce G, Mann RD. The use of newly marketed drugs in children and adolescents prescribed in general practice. Pharmacoepidemiol Drug Saf 1999; 8 Suppl. 1: S37–45
Maconochie N, Doyle P, Prior S. The National Women’s Health Study: assembly and description of a population-based reproductive cohort. BMC Public Health 2004; 4: 35
Bahri P, Tsintis P. Pharmacovigilance-related topics at the level of the International Conference on Harmonisation (ICH). Pharmacoepidemiol Drug Saf 2005; 14(6): 377–87
Tsintis P, La ME. CIOMS and ICH initiatives in pharmacovigilance and risk management: overview and implications. Drug Saf 2004; 27(8): 509–17
Waller PC, Evans SJ. A model for the future conduct of pharmacovigilance. Pharmacoepidemiol Drug Saf 2003; 12(1): 17–29
Acknowledgements
The Drug Safety Research Unit (DSRU) is an independent charity (No. 327206) that works in association with the University of Portsmouth, Portsmouth, UK. It receives unconditional donations from pharmaceutical companies. The companies have no control over the conduct or the publication of the studies conducted by the DSRU. The DSRU has received such funds from GlaxoSmithKline.
Dr Shakir used to be an employee of GlaxoSmithKline. The other authors have no conflicts of interest that are directly relevant to the content of this study.
We would like to thank all the staff at the DSRU who contributed to the study. We thank the general practitioners who have participated in this study, without whose general support prescription-event monitoring would not be possible. We also thank the Prescription Pricing Division of the National Health Service Business Services Authority for their important participation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Perrio, M.J., Wilton, L.V. & Shakir, S.A.W. A Modified Prescription-Event Monitoring Study to Assess the Introduction of Seretide Evohaler™ in England. Drug-Safety 30, 681–695 (2007). https://doi.org/10.2165/00002018-200730080-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200730080-00005