Abstract
Background: It has been shown that the abrupt cessation of treatment with β-adrenoceptor antagonists (β-blockers) increases the risk of myocardial infarction in patients with hypertension. As β-blockers differ in their pharmacokinetic and pharmacodynamic properties, this risk of discontinuation might also differ between subgroups of β-blockers.
Objective: To determine whether discontinuation of β-blockers is associated with an increased risk of myocardial infarction in elderly patients and whether the effects of recent cessation differs between subgroups of β-blockers, categorised according to their selectivity, lipophilic profile and intrinsic sympathomimetic activity (ISA).
Design: A cohort study in users of β-blockers within the Rotterdam Study, which was a prospective population-based follow-up study of 7983 individuals aged ≥55 years.
Patients: We identified 2588 individuals who had been treated with a β-blocker for at least 30 days at any time during the study period of 1 January 1991 to 1 January 2002. In this group, 148 subjects developed incident myocardial infarction.
Methods: Detailed information on the medication use and clinical characteristics of all patients were collected from the files of pharmacies, general practices and hospitals. Myocardial infarction was diagnosed on the basis of internationally accepted criteria and verified by a cardiologist. The duration of β-blocker use was calculated from computerised pharmacy records on the basis of the number of dispensed tablets or capsules and the prescribed daily number.
For every individual, on the index date (date of myocardial infarction in cases, the same date in controls [defined as any patient who had not experienced a myocardial infarction up to that timepoint]) the usage of β-blockers was determined and classified as either current or as past use. Past use was classified into three different periods: cessation of β-blockers less than 30 days; between 30 and 180 days; and more than 180 days before the index date. The risk of myocardial infarction in the three periods of cessation of exposure were analysed using a Cox proportional hazards model that included potential confounders and cardiac comedication. These analyses were performed for the whole group and for subgroups of β-blockers.
Results: Discontinuation of any β-blocker was not associated with an increased risk of myocardial infarction compared with current use of a β-blocker. Analyses within subgroups showed that discontinuation of selective β-blockers was associated with an increased risk of myocardial infarction compared with current use of any β-blocker within the first 30 days (relative risk [RR] 2.70; 95% CI 1.06, 6.89) and also between 30 and 180 days after discontinuation (RR 2.44; 95% CI 1.07, 5.59). No increased risk was demonstrated in the other β-blocker subgroups.
Conclusion: Overall, discontinuation of β-blockers was not associated with an increased risk of myocardial infarction. However, when analysed by β-blocker subgroup, cessation of selective β-blockers was associated with an increased risk of myocardial infarction during the first 180 days after discontinuation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Withdrawal syndromes after discontinuation of β-adrenoceptor blockers (β-blockers) in patients with angina pectoris have been recognised for approximately 20 years.[1–3] In patients treated for hypertension, only mild and transient withdrawal syndromes, such as tachycardia and anxiety, have been described.[4] In 1990, it was suggested that abrupt cessation of β-blockers in patients who were treated for high blood pressure was associated with an increased risk of myocardial infarction and chest pain during a 30-day period of after discontinuation.[5] Potential mechanisms that were suggested for this increased risk were an increase in β-adrenergic receptors available for binding by circulating catecholamines, sudden loss of the control of hypertension, an increase in the adhesiveness or aggregation of platelets, and asymptomatic progression of coronary heart disease during treatment.[5] The increased risk due to recent discontinuation of therapy was associated with particular β-blockers, i.e. atenolol, propranolol, metoprolol and nadolol, which differ in their selectivity for β1 receptors and their lipophilicity, but that are all without intrinsic sympathomimetic activity (ISA). In this study, analyses were not adjusted for current use of cardiac co-medication. Comedication, however, could have confounded the results because current use of calcium channel blockers is associated with an increased risk of myocardial infarction.[6]
Therefore, we studied whether the discontinuation of β-blockers was associated with an increased risk of myocardial infarction in elderly patients during the subsequent 30 days when adjusted for use of cardiac co-medication, and whether the risk differed between β-blockers categorised according to their selectivity, lipophilic profile and presence of ISA.
Methods
Study Population
The Rotterdam Study was started in 1990 as a population-based prospective follow-up study. All 10 275 residents aged ≥55 years in the suburb of Ommoord in Rotterdam were invited to participate, of whom 7983 (78%) subjects gave written informed consent. The baseline measurements took place between 1990 and 1993. The design of this population-based study has been described elsewhere.[7] The baseline examination included an interview on demographics, current health status, medical history, family history of disease, smoking habits, and current use of medication. During a physical examination, blood pressure, weight and height were measured, and blood was drawn for determination of total cholesterol and high-density lipoprotein cholesterol levels. Once patients entered the Rotterdam Study, they were continuously monitored for myocardial infarction by automated linkage with the files from general practitioners. Pharmacy records were available for 99% of all patients as of 1 January 1991.
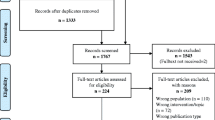
Design
Within the Rotterdam Study, we performed a nested case-control analysis in persons who were current or past users of β-blockers. Hereto, we first selected a cohort of all subjects who had used a β-blocker for at least 30 days during the study period between 1 January 1991 and 1 January 2002. These 30 days were considered the minimum period required to study the effect of withdrawal syndromes after discontinuation. Hence, every user of a β-blocker for at least 30 days was followed until the occurrence of incident myocardial infarction, death, or the end of the study period. According to these inclusion criteria, all included patients were either current or past users of a β-blocker. We only included those patients who had filled any prescription at the community pharmacy within the 90 days prior to the index dates in the cohort.
Case and Control Definition
Within the resulting cohort of 2588 individuals, we studied incident cases of fatal or non-fatal myocardial infarction during the study period. Such an event occurred in 148 patients. The date of myocardial infarction was taken to be the index date. All subjects within the cohort who had not had a myocardial infarction at the index date served as controls. Cases were compared with all controls who were alive and eligible at the index date. When myocardial infarction was reported, additional information was obtained from the medical records of the general practitioner and by scrutinising information from hospital discharge records in instances where patients were admitted or referred. Information on each possible event was gained by review of hospital discharge reports and letters from medical specialists, and classified as definite or possible myocardial infarction. Only definite events were included as cases in the analyses. Two research physicians independently coded events according to the International Classification of Diseases (ICD-10). A medical expert in cardiovascular disease also reviewed all coded events for final classification.[8] In subgroup analyses for the different categories of β-blockers, controls were matched to cases from within the specific category of β-blocker.
Exposure Definition
Pharmacy records were used to calculate periods of drug use, dividing the total number of dispensed tablets by the prescribed daily number according to pharmacy records. In cases of overlap of prescriptions, we considered use as one continuous period of exposure. A maximum delay of 7 days between the end of a prescription for a certain β-blocker and the filling of a new one for the same drug at the pharmacy was accepted as being continuous use. In an earlier study, we demonstrated that these pharmacy records are a very reliable proxy for actual medication use.[9] We computed mutually exclusive categories of current use and past use. In the analyses, we further divided past use into three mutually exclusive categories: (i) discontinuation of β-blockers <30 days before the index date; (ii) discontinuation 30–180 days before the index date; and (iii) discontinuation >180 days before the index date. Hence, all cases and controls were included who had used β-blockers for at least 30 days and were either currently using them at the index date, or who had discontinued them before that date.
Analyses were performed for all β-blockers, as well as for certain subgroups: selective β-blockers, nonselective β-blockers, lipophilic β-blockers, hydrophilic β-blockers, β-blockers with ISA and β-blockers without ISA (table I). β-Blockers were classified into these subgroups according to information in the literature.[10,11] We allocated the qualifications ‘no ISA’, ‘hydrophilic’ and ‘nonselective’ when we did not find any mention in the literature for the presence of ISA, lipophilicity or cardioselectivity at any dosage.
Covariables
As potential confounders, we considered age, gender, and comorbid heart failure (as described in an earlier publication)[12] estimated at the index date. Because discontinuation and current use of β-blockers may be associated with the initiation of therapy with other antihypertensive drugs, we also adjusted for current use of other antihypertensive drugs, such as diuretics, calcium channel blockers, ACE inhibitors and angiotensin II type 1 receptor antagonists and miscellaneous antihypertensives, at the index date. We further adjusted for the prevalences of asthma or chronic obstructive lung disease (defined on the basis of use of antiasthmatic drugs or inhaled corticosteroids preceding or at the index date), and for the baseline values for body mass index (BMI) in kg/m2, history of myocardial infarction, smoking history and status, hypertension (defined as blood pressure >160/95mm Hg) and a history of diabetes mellitus or use of antidiabetic agents on the index date.
Statistical Analyses
In the analyses, we included current use and the three categories of past use of β-blockers as time-dependent covariables in a multivariable Cox proportional hazards model. In this way, the risks of myocardial infarction during the three categories of past use were compared with the risk of myocardial infarction during current use of β-blockers. Risk estimates were adjusted for all of the covariables mentioned above, and separately in a model where we included only covariables that caused a change in the point estimate of at least 10%. In the subgroup analyses of the β-blockers, we adjusted for current use of any of the other categories, because discontinuation of one subtype might have been followed by the use of a β-blocker from another subgroup. All analyses were performed with SPSS version 11.0 (Chicago, IL, USA) and SAS (Statistical Analyses System) version 8, Cary, NC, USA.
Results
Table I shows which β-blockers were used during the study period, and for each individual product gives the number of prescriptions and the pharmacological characteristics. As shown in table II, cases were significantly older (72 vs 69 years) and more likely to be male compared with controls. Cases more often had a history of myocardial infarction and diabetes mellitus than controls. There were no significant differences between cases and controls regarding the BMI, rates of hypertension or smoking status.
When comparing the risk of cessation of β-blockers as a whole group versus current use, no increased risk was found at any time after cessation. Adjustment for covariables did not alter the results (table III). Analyses for effects of cessation within the subgroups of β-blockers showed an increased risk of myocardial infarction for certain time periods after discontinuation compared with current use for selective β-blockers, β-blockers with ISA and lipophilic β-blockers. Discontinuation of selective β-blockers was associated with an increased risk of myocardial infarction compared with current use of β-blockers during the first 30 days (relative risk [RR] = 2.70, 95% CI 1.06, 6.89) as well from day 30 to day 180 after discontinuation (RR = 2.44, 95% CI 1.07, 5.59). Cessation of β-blockers with ISA led to an approximately 4-fold increased risk of myocardial infarction during the first 30 days of cessation and a more than 2-fold increased risk for discontinuation from 30 to 180 days, but these increases were not significant (RR = 4.05, 95% CI 0.97, 16.9 and RR = 2.5, 95% CI 0.61, 10.3, respectively). Discontinuation of lipophilic β-blockers was associated with a nonsignificantly increased risk during the first two time periods (<30 days: RR = 1.90, 95% CI 0.72, 5.00; 30–180 days: RR = 1.91, 95% CI 0.87, 4.23).
For all β-blockers, discontinuation >180 days before the index date was found to be associated with a significant decrease in the risk of myocardial infarction compared with current β-blocker use (RR = 0.59, 95% CI 0.38, 0.91); a similar result was seen for this time period for nonselective β-blockers (RR = 0.49, 95% CI 0.26, 0.90).
Discussion
In this study, we did not find an increased risk of myocardial infarction after the cessation of β-blockers. Therefore, we were not able to reproduce the increased transient 4-fold risk of incident coronary heart disease within the first 30 days of discontinuing β-blockers that was found in an earlier study by other investigators.[5] This was not altered when adjusting for covariables and current use of other antihypertensive drugs. The different results may be explained by the fact that in the study of Psaty et al.,[5] patients were younger (30–79 years) and were treated for hypertension. In our study, in which patients were aged >55 years, we had information about the indication for β-blockers at baseline but not during follow-up. Thus, we adjusted for hypertension and myocardial infarction at baseline. In the earlier study, patients with prior myocardial infarction were excluded. Our study compared past use of β-blockers with current use, whereas the earlier study used a reference group consisting of users of any antihypertensive medication. Finally, our outcome was definite myocardial infarction, whereas the study by Psaty et al. also included unstable angina as an outcome. A recent study has shown markedly increased odds ratios for mortality after perioperative discontinuation of β-blockers.[13] Another recent study described that withdrawal was associated with even worse survival than no β-blocker therapy.[14] However, the patients in this study had undergone vascular surgery and belonged to a selected population with a high risk of coronary artery disease and perioperative mortality, which is quite different to our population. We tried to focus on community-dwelling patients by including only those patients who had filled any prescription for any drug at the community pharmacy within the 90 days prior to the index date.
In subgroup analyses, we found a 4-fold increased risk of myocardial infarction associated with the discontinuation of β-blockers that had ISA compared with current use of β-blockers during the first 30 days following treatment cessation, which was borderline significant; however, after adjusting for all co-variables, the risk increase was no longer significant. This lack of significance might be due to the small numbers of patients using β-blockers of this category. However, an increased risk of myocardial infarction after discontinuation of β-blockers because of ISA is counterintuitive and not in line with results from other studies.[5,15] The increased risk of myocardial infarction following discontinuation of β-blockers that was found in an earlier study[5] was attributed to four β-blockers, all without ISA (propranolol, nadolol, atenolol and metoprolol). Moreover, in a trial of β-blockers with ISA, no increase in the risk of myocardial infarction occurred after sudden withdrawal.[15]
In our study population, atenolol (which is selective and hydrophilic) and metoprolol (selective and lipophilic) were used the most frequently used agents. This is in line with the guidelines of the General Dutch Practitioners,[16] which, until recently, recommended the selective β-blockers metoprolol and atenolol as equal first-choice treatments for hypertension. In November 2004, meta-analyses suggested that lipophilic β-blockers might be superior to their hydrophilic counterparts in the treatment of hypertension, because they better penetrate into the CNS and therefore have a greater ability to prevent ventricular fibrillation.[17] If it is true that the selective and lipophilic qualities of β-blockers are valuable in prevention of myocardial infarction, abrupt cessation of β-blockers with this quality should be more harmful than discontinuing hydrophilic or nonselective β-blockers. For selective β-blockers, we found a significantly increased risk of myocardial infarction in the first 30 days following discontinuation and also an increased risk for the period 30–180 days after discontinuation. The risk associated with cessation of lipophilic β-blockers was also increased during the first 30 and 30–180 days after discontinuation, but to a lesser extent than for the selective β-blockers, and the increase was not significant. The number of users within this category was smaller than for the category of selective β-blockers, but was considerably higher than for the subgroup receiving β-blockers with ISA (table III).
Our result of a persistent increased risk for myocardial infarction in the period 30–180 days after cessation of a selective β-blocker was unexpected because withdrawal symptoms caused by rebound phenomena, a supersensitivity response or an increase in platelet aggregation are thought to develop soon after the abrupt discontinuation of β-blockers. If this is not a chance finding, the most plausible explanation for the increased risk during the 180 days after ceasing selective β-blocker therapy seems to be a nonsymptomatic worsening of the underlying disease during treatment that becomes apparent after its cessation. This theory was confirmed when we repeated all analyses in only those patients who had used β-blockers for at least 180 days prior to the index date. This did not markedly change our results; however, the increased risk associated with discontinuation of selective β-blockers within 30 days of the index date compared with current use no longer remaining significant. However, for cessation between 30 and 180 days prior to the index date the increase in the risk of myocardial infarction was greater in the patients with a longer period of exposure to selective β-blockers than in those with shorter preceding use (RR = 2.73, 95% CI 1.12, 6.63). Also unexpected was the decreased risk of myocardial infarction in patients who had discontinued treatment with any β-blocker >180 days prior to the index date compared with current use. The decreased risk for across all β-blockers was mostly accounted for by the nonselective and hydrophilic subgroups of β-blockers. In these groups, confounding by indication might have contributed to the result, as β-blockers with these qualities may be chosen for patients with different characteristics who are possibly healthier[18] and at lower risk of myocardial infarction p ]Potential limitations of every observational study are selection bias, information bias and confounding. Selection bias is unlikely because of the population-based design and because cases and controls were derived from the same study population. In this follow-up study, data on disease and drug use were gathered prospectively and by people who were unaware of the research hypothesis, so information bias was excluded. We cannot exclude, however, some random misclassification of exposure. Although we had complete access to pharmacy records, we had only limited information about the actual use of β-blockers. In particular, we do not know whether the β-blockers were discontinued abruptly. When discontinuing a β-blocker, it is advised that the dosage be tapered over 1–2 weeks.[19] Thus, it is possible that many patients did not stop their β-blockers abruptly, but took a longer period to finish the last prescription. Because cases and controls had both received β-blockers, confounding by indication seems less probable in the comparisons involving all β-blockers. Even if there was a relatively large proportion of patients who used these drugs because of coronary heart disease rather than hypertension, any confounding by indication would explain an increased risk of myocardial infarction during use instead of after cessation.
In conclusion, we did not find an overall association between the discontinuation of β-blockers and an increased risk of myocardial infarction, but we did find an increased risk of myocardial infarction within 6 months of stopping selective β-blocker therapy compared with current use of β-blockers. Although this study does not facilitate conclusions about potential mechanisms, it is unlikely that this risk increase in the 6 months following discontinuation is explained by rebound phenomena, supersensitivity or an increase in platelet aggregation. As a harmful effect of withdrawal may be an indication of capability in the prevention of myocardial infarction,[5] that we only found an increased risk associated with cessation within the subgroup of selective β-blockers may suggest that β1 selectivity is the most important characteristic of β-blockers for preventing myocardial infarction. Whatever the mechanism, it remains advisable to discourage abrupt withdrawal of β-blockers.
Conclusion
Overall, discontinuation of β-blockers in the elderly was not associated with an increased risk of myocardial infarction. For selective β-blockers, however, cessation was associated with an increased risk of myocardial infarction during the first 180 days after discontinuation. This might be due to nonsymptomatic worsening of the underlying disease during treatment becoming visible after discontinuation of β-blockers.
References
Prichard BNC, Waiden RJ. The syndrome associated with the withdrawal of β-adrenergic receptor blocking drugs. Br J Clin Pharmacol 1982; 13: 337–43
Rangno RE, Langlois S. Comparison of withdrawal phenomena after propranolol, metoprolol and pindolol. Br J Clin Pharmacol 1982; 13: 345–51
Frishman WH. β-Adrenergic blocker withdrawal. Am J Cardiol 1987; 59(13): 26F-32F
Hart GR, Anderson RJ. Withdrawal syndromes and the cessation of antihypertensive therapy. Arch Intern Med. 1981; 141: 1125–7
Psaty BM, Koepsell TD, Wagner EH, et al. The relative risk of incident coronary heart disease associated with recently stopping the use of β-blockers. JAMA 1990; 263: 1653–7
Psaty BM, Heckbert SR, Koepsell TD, et al. The risk of myocardial infarction associated with antihypertensive drug therapies. JAMA 1995; 247: 620–5
Hofman A, Grobbee DE, de Jong PT, et al. Determinants of disease and disability in the elderly: the Rotterdam Elderly Study. Eur J Epidemiol 1991; 7: 403–22
Bots ML, Hoes AW, Koudstaal PJ, et al. Common carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam Study. Circulation 1997; 96: 1432–7
Sjahid SI, Van der Linden PD, Stricker BHCh. The agreement between the pharmacy medication history and patient interview for cardiovascular drugs: the Rotterdam elderly study. Br J Clin Pharmacol 1998; 45: 591–5
Hardman JG, Limbird LE, editors. Goodman and Gilman’s the pharmacological basis of therapeutics. 10th ed. San Diego (CA): McGraw-Hill, 2005
Sweetman SC, editor. Martindale: the complete drug reference. 34th ed. London (UK): Pharmaceutical Press, 2005
Bleumink GS, Knetsch AM, Sturkenboom MCJM, et al. Quantifying the heart failure epidemic: prevalence, incidence rate, lifetime risk, sand prognosis of heart failure — the Rotterdam study. Eur Heart J 2004; 25: 1614–9
Shammash JB, Trost JC, Gold JM, et al. Perioperative β-blocker withdrawal and mortality in vascular surgical patients. Am Heart J 2001; 141: 148–52
Hoeks SE, Scholte op Reimer WJM, van Urk H, et al. Increase of 1 -year mortality after perioperative beta-blocker withdrawal in endovascular and vascular surgery patients [online]. Eur J Vasc Endovasc Surg 2007 Jan; 33(1): 13–9
Bolli P, Buhler FR, Raeder EA. Lack of beta-adrenoreceptor hypersensitivity after abrupt withdrawal of long-term therapy with oxprenolol. Circulation 1981; 64: 1130–4
NHG Standaard Hypertensie until december 2005 [online]. Available from URL: http://nhg.artsennet.nl/content/resources/AMGATE_6059_l04_TICH_L230443008 [Accessed 2007 May 9]
Carlberg B, Samjuelsson O, Lindholm LH. Atenolol in hypertension: is it a wise choice? Lancet 2004; 364: 1684–9
Farmacotherapeutisch Kompas. College voor zorgverzekeringen: Amstelveen, 2005
Informatorium Medicamentorum. Wetenschappelijk Instituut Nederlandse Apothekers, Den Haag, 2005
Acknowledgements
No sources of funding were used to assist in the preparation of this study. The authors have no conflicts of interest that are directly relevant to the contents of this study. We gratefully acknowledge the valuable comments of Professor Bruce Psaty while preparing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Teichert, M., de Smet, P.A.G.M., Hofman, A. et al. Discontinuation of β-Blockers and the Risk of Myocardial Infarction in the Elderly. Drug-Safety 30, 541–549 (2007). https://doi.org/10.2165/00002018-200730060-00008
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200730060-00008