Abstract
The periodic safety update report for marketed drugs (PSUR) was designed to be a stand-alone document that allows a periodic but comprehensive assessment of the worldwide safety data of a marketed drug or biological product. The PSUR can be an important source for the identification of new safety signals, a means of determining changes in the benefit-risk profile, an effective means of risk communication to regulatory authorities and an indicator for the need for risk management initiatives, as well as a tracking mechanism monitoring the effectiveness of such initiatives. For these reasons, the PSUR can be an important pharmacovigilance tool.
Numerous steps are involved in the PSUR process including: intake of adverse drug reaction information, case processing, data retrieval, data analysis, and medical review and risk assessment. These processes are heavily reliant on the availability of adequate resources. An overarching principle throughout the PSUR process is the need for a proactive approach in order to identify the critical steps in the process and to have a clear understanding of the consequences of any critical ‘mis-step’. With this information comes appropriate planning, building quality into each step of the PSUR process and monitoring performance will maximise the likelihood of generating a quality report. Any failure of a key PSUR process will have the opposite effect — a poor quality report that will give little insight into emerging safety signals or provide misleading information that can adversely affect public health. A pragmatic approach that will avoid or minimise these pitfalls includes the following: adequate resource planning, training, development of ‘scripts’ designed to maximise the capture of key information for medically important reactions, standardised and harmonised Medical Dictionary for Regulatory Activities (MedDRA) coding procedures, pre-specified search criteria for data retrieval, ongoing medical review, and metrics to evaluate the effectiveness and efficiencies of these processes.
With these quality measures in place, the utility of the PSUR as an effective pharmacovigilance tool is enhanced.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The periodic safety update report for marketed drugs (PSUR) was designed to be a stand-alone document that allows a periodic but comprehensive and integrated assessment of the worldwide safety data of a marketed drug or biological product. The safety information contained within the PSUR comes from a variety of different sources, e.g. spontaneous reports from different countries, the literature, clinical trials, registries, regulatory adverse drug reaction (ADR) databases and important animal findings. The PSUR can be an important source for the identification of new safety signals, a means of determining changes in the benefit-risk profile, an effective means of risk communication to regulatory authorities, an indicator for the need for risk management initiatives as well as a tracking mechanism for monitoring the effectiveness of such initiatives. For these reasons the PSUR can be an important pharmacovigilance tool.
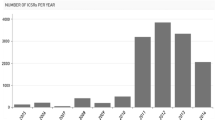
The concept for the PSUR evolved from the Council for International Organizations of Medical Sciences (CIOMS) Working Group II report.[1] This initiative formed the basis for the International Conference on Harmonisation (ICH) Guidance for Industry, ‘E2C Clinical Safety Data Management: Periodic Safety Update Reports for Marketed Drugs’.[2] After its adoption, practical considerations regarding the content and preparation of the report were addressed in the CIOMS Working Group V report, ‘Current Challenges in Pharmacovigilance: Pragmatic Approaches’.[3] Many of the recommendations in this report formed the basis of an addendum to the E2C Guidance.[4] The PSUR has been adopted in a number of European countries and Japan, and is gaining worldwide acceptance[3] including a proposal that the PSUR replace the current periodic report used in the US,[5] and therefore is emerging as a global standard.
The rationale for the PSUR and the content and format of the report, have been set forth in the documents referenced above.[1–4] Definitions relevant to the PSUR and the table of contents of the report are shown in table I and table II, respectively.[2,4] Although the intent of the PSUR initiative is to have a standard PSUR format and content, individual countries may require additional information (e.g. ADRs reported by consumers). The PSUR is designed to contain information reported or confirmed by a healthcare professional; however, regulatory agencies in some countries, including the US, require consumer reports; this is accommodated by including consumer information in an appendix to the PSUR.[5]
Numerous steps are involved in the preparation of the PSUR, and the focus of this review will be on the PSUR process.
1. Pitfalls of the Periodic Safety Update Report for Marketed Drugs Process
The PSUR process includes the following: intake of ADR information, case processing, data retrieval, data analysis and medical review and risk assessment. This process is heavily reliant on the availability of adequate resources. An overarching principle throughout the PSUR process is the need for a proactive approach to identify the critical steps in the process and a clear understanding of the consequences of any critical ‘mis-step’. With this information appropriate planning, building quality into each step of the PSUR process, and monitoring performance will maximise the likelihood of generating a quality report. Any failure of a key step in the PSUR process will have the opposite effect — a poor quality report that will give little insight into emerging safety signals or provide misleading information which can adversely affect public health.
1.1 Resources
The resources required by a company to prepare the PSUR are dependent on a number of factors. These include: the size of the company, the number of marketed products, when these products were approved, the number of countries where these medical products are marketed, the volume of ADRs and the complexity of the medical condition for which the medical product is indicated. Therefore the resources needed for a newly approved drug that is marketed in many countries, for example to treat AIDS, will be considerably greater than the resources needed to prepare a PSUR for a 15-year-old topical formulation which is only approved in a few countries worldwide for the treatment of athletes foot. Competition for the same resources for other projects covering the same timeframe must also be considered. Resources outside a product safety department are also needed, i.e. the marketing department typically has to provide sales/prescriptions data so exposure estimates can be determined; the regulatory department needs to provide information regarding the status of worldwide approval and any regulatory action undertaken anywhere in the world; and clinical research needs to provide any important safety issues emerging from ongoing clinical trials.
There is also a trend globally toward more rigorous regulations governing product safety, e.g. the European Union (EU) Trial Directive[6] which goes into effect May, 2004 and the US-proposed regulations regarding safety reporting requirements for human drugs and biological products.[5] If the US-proposed regulations get passed as currently written, the annual volume of expedited reports will significantly increase, and considerably more follow-up will be required. Even though the EU directive covers clinical trials and not spontaneous postmarketing ADRs, depending on the size and the organisation of a product safety department, the same individuals may have responsibility for both clinical and postmarketing expedited and periodic ADR reporting. It is therefore anticipated that these new regulations will significantly increase the resource requirements of product safety departments. Additionally, those regulatory authorities which have not as yet accepted the concept of the international birth date (IBD) and the recommended periodicity of the PSURs which is based on the IBD, often request information outside the interval period of the PSUR resulting in further expenditure of resources. For these reasons, resources needed to prepare the PSUR may be significantly underestimated.
1.2 Intake of Adverse Drug Reaction (ADR) Information
The individual case safety report (ICSR) is the ‘basic safety unit’ of the PSUR and serves as the building blocks from which the required line listings and summary tabulations of the report originate. A quality PSUR is predicated on the quality of the information contained within the document and therefore is highly dependent on the quality of information in the ICSR. In the draft ‘Concept Paper: Risk Assessment of Observational Data: Good Pharmacovigilance Practices and Pharmacoepidemiologic Assessment’,[7] the characteristics of a ‘good case report’ (whether a spontaneous report or a case reported in the literature) are described and are summarised in table III.
The prevalence of the lack of quality of information in the ICSR has long been identified and discussed, but still remains a universal problem. The intake of ADR information is therefore a critical step of the PSUR process and is where the quality and clinical ‘weight’ of the information is determined. In general, the major source of the ICSR is from spontaneous reports, where the information is usually reported directly to a company representative. Ideally, the company representative should be a healthcare professional who has the necessary clinical experience and background to ensure that as much relevant information as possible is collected. This should not be a passive process, where the company healthcare professional merely takes ‘dictation’ from the reporter, but rather an interactive communication between both parties. The reporter must be actively questioned to ensure the reported information received by the company is clearly understood and is adequate for a proper case assessment to be done. For those countries that accept ADR reports from consumers, it is especially important that the company healthcare professionals understand what the consumer means when describing the adverse event using non-medical terminology. A case where the ADR is described as ‘thick throat’ (see section 2.4) provides little clinical understanding of the ADR. Importantly, when possible, diagnoses reported by consumers should be medically confirmed.
Not obtaining important clinical information from the reporter may well be due to the limited time the reporter gives the company healthcare professional to capture the ADR information. But the inability to obtain a quality case is often due to inadequately trained individuals handling the calls. Training deficiencies typically include: incomplete understanding of the pharmacology, biological activity or mechanism of action of the marketed product; insufficient knowledge regarding common coexistent diseases and concomitant medication use of the patient population who takes the marketed product; and lack of technical knowledge, e.g. Medical Dictionary for Regulatory Activities (MedDRA) terminology.
1.3 Case Processing
Once the information is taken from the reporter, the case is entered into a safety database, a narrative of the case is prepared and a MedDRA term is assigned for the ADRs described in the case. Assignment of seriousness, and ‘labelledness’ for postmarketed events (causality is assumed for postmarketing spontaneous ADRs)[8] determine whether or not the event needs to be processed as an expedited report. If the ADR reported is found in the product information for a given country, the event is considered ‘labelled’, if not, the ADR is classified as ‘unlabelled’. ‘Labelledness’ is therefore country-specific and not uniform across countries. For the PSUR, ‘listedness’ must be determined. An event is ‘listed’ or ‘unlisted’ if the ADR is found, or not found, respectively, in the company core safety information (CCSI). Unlike ‘labelledness’, ‘listedness’ is uniform across all countries.
Inconsistencies regarding case classification, i.e. serious/non-serious, labelled/unlabelled, and selection of MedDRA terms, arise during case processing. Cases with outcomes of death, hospitalisation or prolonged hospitalisations, and congenital anomalies more easily fit the definition of ‘serious’.[8] However, medically important outcomes, and outcomes due to disability usually require more medical interpretation and clinical judgement which can result in more inconsistencies in the determination of the ‘seriousness’ of a case. Inconsistencies among medical reviewers have been well documented.[3,9] A cumulative tabulation across all intervals of the PSUR is required for serious, unlisted ADRs; if a serious case is misclassified it will not be part of the cumulative tabulation and will not be located in the line listings dealing with serious ADRs thereby increasing the chance that the event may be overlooked and/or under-assessed during medical review.
Case classification inconsistencies increase with the number of individuals responsible for processing cases. Likewise, if cases are processed locally, (i.e. at an affiliate rather than centrally [global headquarters]) the likelihood of inconsistencies increases further.
Manual coding in MedDRA can result in inconsistent results and are subject to the same factors that influence case misclassification (i.e. the number of individuals responsible for MedDRA coding, and whether coding occurs centrally or locally). MedDRA’s granularity is also a contributing factor in coding inconsistencies due to the number of MedDRA terms that can be chosen for any given verbatim term.
The totality of these inconsistencies during the case handling process for large volume PSURs may have a considerable impact on the accuracy of the PSUR and weaken the ability to identify new signals or do a proper evaluation.
Mention must also be given to narrative writing, which is an integral part of the ICSR and the case handling process. A summary of all relevant information in narrative format provides a medical reviewer with better insight and understanding of the reported reaction. Choosing the relevant information is not always straightforward and is dependent on clinical knowledge, experience and judgement. Including a medical history of bunion repair in the narrative of a subject with acute liver failure adds no understanding of the case and can be potentially distracting. Furthermore, case information provided by the reporter may at times be inconsistent with the given diagnosis. In such situations, the company should provide an alternative diagnosis and the justification for this difference in the narrative,[3] again underscoring the need for clinical experience and sound medical judgement.
1.4 Data Retrieval
Data retrieval from the data lock point (DLP) and generation of line listings and summary tabulations are typically the most rate-limiting and time-consuming steps for high volume PSURs, usually taking far longer than originally planned. Delay at this step will compress the time required to complete other critical parts of the report, i.e. sections 1.6 and 1.9, ‘presentation of individual case histories’, and ‘overall safety evaluation’, respectively. Without this information, a proper medical review and risk assessment can be severely hampered.
To ensure better accuracy and consistency, data retrieval is usually performed by data managers or programmers rather than by medical writers or medical reviewers. However, based on personal observation, it is not unusual for the data output, e.g. number of cases retrieved, to be different depending on who is retrieving the data, and what database search criteria are used. Duplicate cases are often found in the database that if not identified could result in misleading findings. Moreover, ‘homegrown’ systems, rather than commercially developed databases, built before the evolution of the PSUR, may not have the design features that more easily and reliably retrieve data needed for report preparation.
1.5 ADR Analysis
The limitations of postmarketing data are well known and include the inability to precisely determine the incidence of ADRs due to under-reporting, difficulty in calculating exposure, and reporting biases.[10–15] It would be ideal if signal detection and signal validation could be done automatically, and for these reasons, data mining methods as a means for signal detection have stimulated a lot of interest. Statistical algorithms such as the Multi-Item Gamma Poisson Shrinker (MGPS) method,[16] Bayesian Confidence Propagation Neural Network (BCPNN),[17] and Proportional Reporting Ratios (PRR),[18] automatically generate safety signals, from large ADR databases, without relying on incidences, and are emerging as useful tools in signal detection. However, channelling and over representation of some classes of drugs, resulting in skewing the proportion of certain ADRs in a database, are but a few of the biases and limitations that exist in using such methods. Data mining methods for signal detection while useful, supplement but do not replace the traditional method of medical review.
1.6 Medical Review and Risk Assessment
The strength of the PSUR’s utility as a pharmacovigilance tool resides in sections 1.6 and 1.9 of the document, which force the marketing authorisation holder (MAH) to take a critical look at its data. Section 1.6 provides the reviewer by virtue of line listings, summary tabulations and review of individual cases of interest, a comprehensive look at the data to determine whether the pattern of ADRs collected during the reporting interval has changed, and whether medically important events previously unlisted, but with an apparent strong causal relationship to the marketed product, have emerged. Section 1.9 requires the integration of information from section 1.6 as well as all other relevant safety sources, e.g. new animal toxicology data or the results of a drug-drug interaction study, to determine whether the risk for the marketed product has changed and whether changes to the product label have to be made or other risk management initiatives have to be implemented. One of the major strengths of the PSUR is the ability to review aggregate data. If a medical product is marketed in numerous countries, an adverse reaction of interest found across many countries rather than isolated countries, provides greater clinical weight to the finding. The ability to look at all adverse reactions in listings and tabulations can also strengthen the identification of a signal and the potential aetiology of the signal. This is especially relevant with MedDRA utilisation. Because of MedDRA’s granularity verbatim terms may be coded to medically similar but different MedDRA preferred terms. For these reasons ADRs across different system organ classes must also be reviewed. For example, if a number of cases of ‘syncope’ were identified other MedDRA preferred terms should also be evaluated, e.g. ‘loss of consciousness’, ‘dizziness’, ‘hypotension’, ‘orthostatic hypotension’, ‘blood pressure decreased’, ‘bradycardia’, ‘heart rate decreased’, etc. A listing of all the ADRs that were reported for a given subject can potentially provide an insight into the possible aetiology of the event, e.g. a subject who experienced syncope and was also found to have bradycardia. These medical assessments rely on clinical experience and good clinical judgement. Medical review, however, as discussed above, is dependent on the availability of line listings, summary tabulations and access to cases of interest and this in turn is dependent on the data retrieval process. Since data retrieval is often fraught with delays, as already mentioned, this results in shortened review times. Other measures, as discussed in section 2, must be put into place to ensure that the time needed for medical review and risk assessment is not compromised.
Thorough medical review and risk assessment implies the availability of adequate numbers of well trained healthcare professionals, i.e. a paediatrician new to the pharmaceutical industry who is responsible for assessing the risk associated with a drug for Alzheimer’s disease, will undoubtedly need training on the marketed product and the target patient population, to best be able to identify emerging safety signals and do proper risk assessment.
2. Pragmatic Solutions
By understanding the pitfalls in the PSUR process described above pragmatic solutions to avoid or minimise such problems can and should be undertaken.
2.1 Resource Planning
Over a given period of time, e.g. 12 months, the MAH should know the number of PSURs due in that year, including the DLPs and submission dates of these reports. An estimate of the volume and complexity of cases should also be factored in. The complexity of cases can be anticipated by the condition for which the drug is being prescribed and the likely co-existent diseases of the patient population who will be receiving the drug. Therefore, the cases reported for a drug used in the treatment of sepsis are likely to be more complex than the cases reported for a topical drug used for the treatment of hair loss. Other roles and responsibilities of the personnel assigned to the PSUR process as well as the skill sets of these individuals should also be known. Based on this information, potential conflicts due to competing projects, or identification of individuals lacking the necessary expertise, can be predetermined. If there are too few resources available, the MAH has several options, e.g. re-assigning tasks, re-prioritising other projects, hiring more people, providing training or out-source the work. Communicating expectations, deliverables and dates of completion with individuals within and outside the product safety department, e.g. marketing, must also be done regularly. There should also be a contingency plan in place if unanticipated work, such as a response to an unexpected regulatory query, arises.
2.2 Development of Scripts for Medically Important Conditions
From the point of contact, it is important to maximise communication between the reporter and the company’s healthcare professional ensuring that adequate case information is obtained. Initiatives must therefore be implemented to ensure that key information of medically important cases is obtained in the limited time that the company’s healthcare professional may have with the reporter. ‘Scripts’ to proactively extract key information from the reporter should be developed and those responsible for the intake of ADR information should be thoroughly trained on these scripts. Examples of some medically important ADRs[5] are summarised in table IV. The WHO Critical Term list provides an even more extensive list of such ADRs.[19] A script dealing with ‘liver necrosis’ should guide the company’s healthcare professional to ask specific questions, such as liver function test results especially alanine aminotransferase and bilirubin levels (where clinically significant increases in both these parameters are associated with a 10–15% risk of death),[20] the basis of the diagnosis (e.g. viral serologies, needle biopsy), the use of paracetamol (acetaminophen) and alcohol, and exposure to other hepatotoxins. This information will help immeasurably in the review and assessment of such cases. Scripts should also be developed for any other ADRs that are judged to be medically important. An added benefit of the utilisation of scripts is that higher quality information obtained at initial point of contact is likely to result in fewer requests for follow-up information, which will result in lessened work burden.
2.3 Training
Adequately trained resources are an integral part of the PSUR process and should take into account the educational background, and roles and responsibilities of the staff. Three broad areas of training include product training, clinical training and MedDRA training. Product training is needed to fully understand a product’s pharmacology or biological activity, mechanism of action and the known risks associated with its use. This core information gives the healthcare professional the necessary foundation to ask the appropriate questions when a reporter calls. In addition to this, the healthcare professional must also be clinically grounded and understand the characteristics of the targeted patient population likely to take the medical product with respect to underlying co-existent diseases and concomitant medications. This too will maximise communication between reporter and company healthcare professional. Product and clinical training are also required for case classification, narrative writing, coding of ADRs, medical review and risk assessment as well as the actual writing of the PSUR. Training in the methods of case assessment, including the determination of seriousness, causality and expectedness as recommended by, for example, the CIOMS V Working Group,[3] Benichou,[21] and Venulet et al.,[22] will provide a more objective, consistent, and medically grounded approach.
MedDRA training is required to ensure a full understanding of the dictionary, its hierarchy, and the implications of its granularity. MedDRA is further discussed below.
2.4 Standardised and Harmonised Medical Dictionary for Regulatory Activities Coding
The quality of the verbatim term drives the coding process. A high quality verbatim term is likely to auto-encode whereas a poor quality term is more likely to require manual assignment of a MedDRA term, which as discussed before increases the potential for inconsistencies. Therefore the goal should be to achieve a large percentage of auto-encoded terms. The company’s healthcare professionals should also undergo MedDRA training even if these individuals are not responsible for coding, since this will reinforce the importance of obtaining a quality verbatim term. Such training should result in the avoidance of terms such as ‘thick throat’, which is medically meaningless. Trying to ‘guess’ the appropriate meaning of such a term can lead to disparate results ranging from nonserious if the term represented ‘pharyngitis’, to serious and life-threatening if the term represented ‘laryngeal oedema’.
To ensure coding consistency for global companies where it is likely that cases will be entered remotely worldwide into the MAH’s central database, harmonised and standardised coding procedures are required. It is therefore important that a ‘global’ coding convention document be created, maintained and revised as needed. This document can include the ‘Points to Consider’ developed by the Maintenance and Support Services Organisation (MSSO) for MedDRA [23] but should also include other conventions. An example of a coding convention, would be the establishment of the ‘rule’ that states that for any surgical procedure, the ADR that led to the surgery will be coded rather than the procedure itself, i.e. ‘gallstones’ rather than ‘cholecystectomy’. Another convention may address the handling of confusing terms, i.e. any time ‘cervical pain’ is reported, the reporter should be queried to specify whether the pain is in the neck or related to the cervix. The company healthcare professional responsible for intake of ADR information, even if not involved in coding per se, should at least be aware of these coding issues so they can be handled at the point of contact rather than retrospectively. Standardised procedures to add verbatim terms to the glossary/synonym lists must also be in place. All these measures will better ensure consistent output whether a term is coded in France, Brazil or Canada.
2.5 Prespecified Search Criteria
Prespecified search criteria for data retrieval should be developed, utilised and documented. This will ensure consistent and reproducible data retrieval. Documented search criteria will also aid in better use of data management and programming resources since a search that originated by one programmer would then be able to be duplicated by another, providing better utilisation of resources.
2.6 Ongoing Medical Review
As discussed earlier, sections 1.6 and 1.9 of the PSUR typically are the most time intensive sections to prepare. Selection of individual and series of cases for review and discussion, and the distillation of all the safety information included in the evaluation process, require expert medical judgement and experience. This process cannot be rushed. As already emphasised above, the time needed to prepare PSURs often takes longer than originally planned. If safety review is not initiated before the DLP, it is possible that there will simply be too little time to do a careful medical review and risk assessment. For these reasons, regardless of when a PSUR report needs to be submitted, companies should commit to reviewing their data on an ongoing basis.
Cases are often inconsistently classified and according to the PSUR guidance,[2] cumulative summary tabulations across reporting intervals are only required for serious unlisted ADRs. However, in situations where a case was misclassified as nonserious, this case would not be part of the cumulative summary tabulation. Furthermore, incidences of spontaneous postmarketing ADRs cannot be reliably calculated because of the inability to accurately determine the numerator and denominator.[10,11,14] For these reasons, a simple tabulation (table V) of ADRs regardless of seriousness or listedness may be an aid in helping the medical reviewer focus on what could be an emerging signal. In the example shown in the table, hepatic failure and syncope may alert the reviewer to investigate these cases in greater detail. In this example, if syncope was sometimes classified as serious and other times as nonserious the emerging pattern as displayed in table V could be overlooked. It should however be emphasised that such a table should not be used in exclusion of other available signal detection methodologies. Furthermore, a table like this should be used in only a qualitative way, i.e. as a tool for the medical reviewer to assist in the identification of an unusual pattern that deserves a closer look.
To further enhance the medical review process, the establishment of an in-house Safety Review Committee (SRC) is recommended. The medical reviewer responsible for a given medical product may become too close to the data and lose objectivity. Furthermore, a medical reviewer may miss a signal. An in-house SRC that would meet on a regular basis, e.g. quarterly, composed of senior experienced individuals not directly involved in the safety evaluation of the medical product to review medical products new to the market, would provide an opportunity for a fresh look at the data, and access to broader medical expertise during the evaluation process. Such proactive approaches to ongoing medical review will increase the likelihood of safety signal identification and ensure more accurate risk assessment.
2.7 Metrics
It is important to continually re-examine existing processes to ensure that they remain effective and efficient. Metrics are also important to evaluate ‘corrective actions’, to ensure such actions are having the intended effect. An example of such a metric would be looking at the number of avoidable ADRs that were due to a newly identified drug-drug interaction. Risk management initiatives to address this finding could include a label change, physician notification and patient education. The results of these risk management initiatives should be reflected in subsequent PSURs. If the number of drug-drug interactions reports were not decreasing or stabilising, this would have to be critically reviewed to determine the cause. If the cause was determined to be legitimate and not due to artificial influences such as stimulated reporting from unethical competitor sales representatives, the risk-management initiatives would have to be modified or replaced. Other examples of PSUR metrics are summarised in table VI. Ongoing metrics will help to identify and fix problems before they become unwieldy or evolve into crises.
3. Conclusion
A proactive approach with quality built into each step of the PSUR process, will generate a report that will serve as an invaluable pharmacovigilance tool and an effective means of risk communication to regulatory authorities. Ongoing metrics will identify any weakness in the process so that corrective action can be undertaken. PSUR metrics can also serve to monitor the effectiveness of risk-management initiatives.
References
Council for International Organizations of Medical Sciences (CIOMS). International Working Group I. International reporting of periodic drug-safety update summaries. CIOMS, Geneva, Switzerland 1990
Clinical safety data management: periodic safety update reports for marketed drugs E2C. ICH Expert Working Group, November 1996. Available from URL: http://www.ich.org/MediaServer.jser?.@_ID=477&@_MODE=GLB [Accessed 2004 Jan 20]
Council for International Organizations of Medical Sciences (CIOMS). International Working Group V. Current challenges in pharmacovigilance: pragmatic approaches. CIOMS, Geneva, Switzerland 2001
Addendum to ICH E2C Clinical safety data management periodic safety update reports for marketed drugs. ICH Expert Working Group, February 2003. Available from URL: http://www.ich.org/MediaServer.jser?.@_ID=478&@_MODE=GLB [Accessed 2004 Jan 20]
Department of Health and Humans Services, the US Food and Drug Administration. Proposed safety regulations March 2004 [online]. Available from URL: http://www.fda.gov/OHRMS/DOCKETS/98fr/03-5204.pdf [Accessed 2004 Jan 20]
Directive 2001/20/EC of the European Parliament and the Council, 4 April 2001. Available from URL: http://www.europa.eu.int/eur-lex/pri/en/oj/dat/2001/l_121/l_12120010501en00340044.pdf [Accessed 2004 Jan 20]
Concept Paper. Risk assessment of observational data: good pharmacovigilance practices and pharmacoepidemiologic assessment (draft) March 2003. Available from URL: http://www.fda.gov/cder/meeting/groupIIIfinal.pdf [Accessed 2004 Jan 20]
ICH Working Group. Post-approval safety data management: definitions and standards for expedited reporting E2D. November 2003. Available from URL: http://www.ich.org/MediaServer.jser?.@_ID=631&@_MODE=GLB [Accessed 2004 Jan 20]
Koch-Weser J, Sidel VW, Sweet RH, et al. Factors determining physician reporting of adverse drug reactions: comparison of 2000 spontaneous reports with surveillance studies at the Massachusetts General Hospital. N Engl J Med 1969 Jan; 280(1): 20–6
Strom BL, Tugwell P. Pharmacoepidemiology: current status, prospects, and problems. Ann Intern Med 1990; 113: 179–81
Scott HD, Rosenblaum SE, Waters WJ, et al. Rhode Island physicians’ recognition and reporting of adverse drug reactions. R I Med J 1987; 70: 311–6
Sachs RM, Bortnichak EA. An evaluation of spontaneous adverse drug reaction monitoring systems. Am J Med 1986; 81Suppl. 5B: 49–55
Weber JP. Epidemiology of adverse drug reactions to nonsteroidal anti-inflammatory drugs. In: Rainsford KD, Velo GP, editors. Advances in inflammatory research. Vol. 6. New York: Raven Press, 1984: 1–7
Begaud B, Moride Y, Tibert-Bitter P, et al. False-positives in spontaneous reporting: should we worry about them? Br J Clin Pharmacol 1994; 38: 401–4
Serradell J, Bjornson DC, Hartzema AG. Drug utilization study methodologies: national and international perspectives. Drug Intell Clin Pharm 1987; 21: 994–01
Szarfman A, Machado SG, O’Neill RT. Use of screening algorithms and computer systems to efficiently signal higher than expected combinations of drugs and events in the US FDA’s spontaneous reports database. Drug Saf 2002; 25(6): 381–92
Lindquist M, Stahl M, Bate A, et al. A retrospective evaluation of a data mining approach to aid finding new adverse drug reaction signals in WHO international database. Drug Saf 2002; 23(6): 533–42
Evans SJW, Waller PC, Davis S. Use of proportional reporting ratios (PRRs) for signal generation from spontaneous adverse drug reaction reports. Pharmcoepidemiol Drug Saf 2001 Oct-Nov; 10(6): 483–6
World Health Organization (WHO) Adverse Reaction Terminology: critical term list. WHO Collaborating Center for International Drug Monitoring, Uppsala, Sweden. Available from URL: http://www.who-umc.org [Accessed 2004 Mar 22]
FDA Working Group CDER-PhRMA-AASLD Conference 2000, Clinical White Paper, November 2000 Available from URL: http://www.fda.gov/cder/livertox/clinical.pdf [Accessed 2004 Jan 20]
Benichou C, editor. Adverse drug reactions: a practical guide to diagnosis and management. Chichester, England: John Wiley & Sons Ltd, 1994
Venulet J, Ciucci A, Berneker GC. Standardized assessment of drug-adverse reaction associations: rationale and experience. Int J Clin Pharmacol Ther 1980; 18(9): 381–8
MedDRA® term selection: points to consider, November 2003. Available from URL: http://www.meddramsso.com/New-Web2003/Docs/ptc_3.2_final.pdf [Accessed 2004 Jan 20]
Acknowledgements
The author acknowledges that he received no funding to assist in the preparation of this manuscript and no conflicts of interest exist with respect to the contents of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Klepper, M.J. The Periodic Safety Update Report as a Pharmacovigilance Tool. Drug-Safety 27, 569–578 (2004). https://doi.org/10.2165/00002018-200427080-00008
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200427080-00008