Abstract
Introduction: Toxic epidermal necrolysis (TEN) is a life-threatening adverse drug reaction (ADR) that is primarily the result of drug exposure (incidence 0.4–1.3 per million person-years). Life-threatening ADRs such as TEN should be reported to ADR monitoring programmes, which collect reports for suspected ADRs and alert the public and medical practitioners to new drug hazards. In Canada, reports are made to the Canadian Adverse Drug Reaction Monitoring Program (CADRMP).
Objective: To examine the extent of under-reporting for TEN in Canada.
Design: A retrospective case series design was used to collect all TEN cases for the period January 1995 to December 2000.
Methods: The CADRMP and 22 burn centres across Canada were contacted for all TEN patients treated during the specified time period.
Patient Groups Studied: The study population consisted of patients admitted to burn treatment sites across Canada, patient cases reported to the CADRMP and patient cases recorded by the Canadian Institute for Health Information (CIHI) hospital discharge summaries as the International Classification of Diseases Version 9 Clinical Modification (ICD-9-CM) code 695.1.
Results: Twenty-five TEN cases (six fatal) were reported to CADRMP from January 1995 to December 2000. During this period, 14 (63.6%) burn treatment sites reported admission of 250 TEN cases. Hospital discharge summaries using the ICD-9-CM code 695.1 indicated that 4349 cases were admitted to hospital during this time period and it was estimated that 15.5% (n = 674) of these cases were TEN. Using the burn facility data as the denominator, 10% (25 of 250) of TEN cases were reported to CADRMP. Using CIHI data as a denominator, only 4% (25 of 674) of TEN cases were reported to CADRMP.
Conclusions: There is serious under-reporting of TEN. Lack of reporting of life-threatening ADRs can compromise population safety. There is a need to increase awareness of ADR reporting programmes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Spontaneous voluntary reporting is the most common method used in pharmacovigilance and is used to generate signals on rare, serious or life-threatening adverse events. Under-reporting is the major limitation associated with this system of reporting.
Toxic epidermal necrolysis (TEN) is a life-threatening adverse drug reaction (ADR) that is almost exclusively the result of drug exposure.[1] The incidence for TEN ranges from 0.4–1.3 per million person-years.[1–3] Mortality is estimated at 32%.[4] Poor prognostic indicators include extent of necrolysis, increased age of patient and elevated serum urea levels.[5–7] Current classification schemes recognise Stevens-Johnson syndrome (SJS) as a milder form of TEN.[8] When there is extensive skin detachment, poor prognosis and mortality in the range of 30–40%, the condition is usually called TEN.[7]
The hallmark of TEN is the widespread detachment of epidermis (‘necrolysis’) following drug exposure.[9,10] Exfoliation occurs with sheets of full-thickness necrotic epidermis sloughing off in what resembles a partial thickness burn over 30% or more of the body surface area.[8–11] Mucous membrane involvement is present in nearly all patients and may affect the mouth (93%), genital areas (63%) and eyes (78%).[7,9,10] TEN becomes a multisystem disease after the skin integrity is lost due to microbial invasion and onset of a systemic inflammatory response. Patients with TEN are typically treated in burn units because their clinical and surgical management is very similar to that of burn patients.[9,10,12,13]
More than 100 drugs have been implicated as causes of TEN and SJS.[7,14] A recent case-control study reported substantially increased risks associated with antibacterial sulfonamides, anticonvulsants and NSAIDs.[15] In that study, 14 drugs were responsible for more than 80% of TEN and 50% of SJS cases.
Life threatening ADRs such as TEN should be reported to ADR monitoring programmes. Case reports of suspected ADRs are an important means of alerting healthcare professionals, regulatory authorities, manufacturers and the public to new drug hazards. In Canada, the Canadian Adverse Drug Reaction Monitoring Program (CADRMP) is a spontaneous voluntary ADR reporting programme that is governed by the Adverse Reaction and Medication Error Assessment Division, Bureau of Licensed Product Assessment, Therapeutic Products Directorate, Health Products and Food Branch of Health Canada (1965–present). All reports of suspected ADRs are welcomed by the CADRMP because they contribute to information that will assist in determining the strength of a signal of an association between a drug and an adverse event. The CADRMP particularly encourages ADR reports for recently marketed drugs, unexpected reactions irrespective of severity, and all serious reactions even if the reaction has already been labelled. Causality or proof that a drug has caused an undesirable patient effect is not a requirement for reporting. The purpose of this spontaneous reporting system is to identify and describe adverse events as they occur after drug exposure and disseminate the information to healthcare professionals.
Under-reporting is a major limitation of voluntary spontaneous reporting programmes.[16] It is estimated that only 1–30% of ADRs are reported.[17] If ADRs are not reported, the detection of signals identifying possible drug associations will not occur. Not reporting or delays in reporting may lead to a delay in signal detection where suspect drug reactions reported earlier may have prevented future ADRs.
We hypothesise that there is under-reporting of TEN. The objective of this study was to examine the extent of under-reporting of TEN cases across Canada.
Study Design
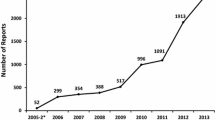
A retrospective case series study design was used. The study examined TEN/SJS cases from January 1995 to December 2000. Case selection included: (i) all cases reported to the CADRMP; (ii) all cases admitted to burn treatment sites across Canada; and (iii) all cases recorded by the Canadian Institute for Health Information (CIHI) hospital discharge summaries as the International Classification of Diseases Version 9 Clinical Modification (ICD-9-CM) code 695.1. This code is a multi-diagnostic code that codes for TEN, SJS and erythema multiforme exudativa (EM). Given the multi-diagnostic nature of the code, it was important to determine the proportion of TEN, SJS and EM cases. To do this, the total number of cases of TEN, SJS and EM reported to the CADRMP was requested. A total of 161 cases were found (15.5% TEN, 48.4% SJS, 45.3% EM). The value of 15.5% was used to determine the number of TEN cases in the CIHI discharge abstract database. Figure 1 shows the breakdown of cases from CIHI with ≥1 diagnosis.
Methods
The CADRMP, the 22 burn centres across Canada and CIHI were contacted by the investigators who requested all TEN patients treated during the specified time period. All Canadian burn treatment sites were contacted via telephone and a fax was sent to make a request for the number of TEN cases admitted to hospital between January 1995 and December 2000. Reminder telephone calls were made after an extended period (2 months, 6 months) of non-response. Up to three contact attempts were made. Information requested included the number of cases, age, gender, outcome (survival/death), incident date and length of hospitalisation. No identifying patient information was collected.
Descriptive statistics (mean, percent) were used to characterise the data from the three data sources. Cases from the Canadian burn care facilities were matched with cases from the CADRMP using various identifying markers such as age, gender and location. Two investigators were used to match data. CIHI data were used to verify the number of cases in Canada. SPSS 10.0 was used to analyse the data set. As this was a database study, we did not have access to patient identifiers. This study was approved by the Sunnybrook and Women’s College Health Sciences Centre Research Ethics Board.
All TEN cases reported to the CADRMP, all TEN cases admitted to burn treatment sites across Canada, and all cases of TEN/SJS discharged from Canadian hospitals as reported by CIHI contributed to the study patient population.
Canadian Adverse Drug Reaction Monitoring Program (CADRMP)
The following information was extracted from each case reported from the CADRMP: gender, age, suspected drug, profession of reporter, location of report, suspect drug(s), concomitant drug(s), treatment drug(s), outcome, any causality information including onset of reaction, other symptoms and laboratory test abnormalities.
Canadian Burn Treatment Facilities
A list of all Canadian burn care facilities was obtained from the Canadian Burn Care Network, the American Burn Association and the Ross Tilley Burn Centre in Toronto. There are a total of 22 (16 adult; six paediatric) burn treatment centres in Canada. These sites are part of the Canadian Burn Care Network.
Canadian Institute for Health Information (CIHI)
The number of cases per province per year between January 1995 and December 2000 was collected from the CIHI. CIHI is an independent, pan-Canadian, non-profit organisation working to improve the health of Canadians and the healthcare system by providing quality, reliable and timely health information, such as all cases with the ‘Most Responsible Diagnosis’ code of 695.1 by province from 1995–2000 collected from the hospital discharge abstract data (DAD) summaries. The code 695.1 is a multi-diagnostic code that represents TEN, SJS and EM and the ‘Most Responsible Diagnosis’ is considered the primary diagnosis for why a patient is hospitalised. It should be noted that Manitoba only submits 60% of their acute care data to the CIHI discharge abstract database. Quebec does not submit data to the CIHI discharge abstract database.[18]
Results
CADRMP
The investigators were informed that 25 TEN cases (six fatal) were reported to CADRMP. Reports came from across Canada: Ontario (20%), Quebec (12%), Alberta (12%), Nova Scotia (12%), Saskatchewan (4%), British Columbia (4%), and New-foundland (4%). Location information was not available in 32% of the cases. Drugs suspected of causing TEN included antibiotics, anticonvulsants and a number of other medications (table I). Nineteen of the 25 cases were coded as TEN only, whereas two cases (8%) were TEN/SJS, three (12%) were TEN/EM and one (4%) was TEN/EM/SJS.
Canadian Burn Treatment Facilities
Table II shows that 14 (63.6%) burn treatment units responded to the request for TEN cases. 250 cases were admitted to 12 burn treatment units from January 1995 to December 2000. Two centres reported no cases within the specified time period.
CIHI
CIHI data showed that there were 4349 cases discharged from hospital with a ‘Most-Responsible Diagnosis’ ICD-9-CM code of 695.1 between 1995 and 2000. In the hospital discharge summaries, the highest number of cases recorded with code 695.1 as the ‘Most Responsible Diagnosis’ was contributed by Ontario (n = 1585; table III). This was followed by Quebec (n = 935) and Alberta (n = 593). The total number of cases (4349) was multiplied by the proportion of TEN cases extracted from the CADRMP (i.e. 15.5%). Using this estimate, the number of TEN patients admitted to hospital across Canada would be 674 (4349 × 0.155). This number may also be an under-estimation, given the fact that Manitoba and Quebec did not have complete data sets and that provinces with <5 cases were not reported by Statistics Canada.
Unique Cases
In order to examine the extent of overlap in the reporting of ADRs, an examination of CADRMP cases and Canadian Burn Unit cases was undertaken. Results showed a possibility of three matched cases between the two databases. The remaining cases did not have corresponding matches with respect to age, gender, outcomes, location and date. Consequently, there were at least 272 (250 burn treatment facility cases and 25 CADRMP cases, with three possible matches) unique cases of TEN in Canada over a 5-year time frame.
Calculation of Reporting Rate
If one used the burn facility data as the denominator, 10% (25/250) of TEN cases were reported to the CADRMP. Using CIHI data as a denominator, only 4% (25/674) of TEN cases were reported to the CADRMP.
Discussion
Case reports of suspected ADRs are an important means of alerting physicians, regulatory authorities, manufacturers and the public to possible drug hazards. Spontaneous reporting systems, such as the CADRMP, do not definitively establish a relationship between an adverse effect and drug exposure. Such data is best used for generating hypotheses for further study. When cases are not reported, signals are not detected. Also, when cases are not reported, risk factors may not be detected.
This analysis highlights that there is serious under-reporting of a very visible and recognisable drug-related adverse event. Other serious and life-threatening conditions such as aplastic anaemia, agranulocytosis or liver failure may not be as immediately apparent in their association to drug exposure. Consequently, detection and reporting may be more difficult.
The CADRMP received approximately 8566 spontaneous reports in 2002.[20] The US FDA received 159 504 evaluable adverse drug experiences in 1996.[21] Ninety-one percent of those reports were sent via the manufacturer. Fifty-seven point six percent of the cases were reported by healthcare professionals and 41.2% by consumers. Given the population size and the volume of pharmaceutical products (billions of dollars) sold, the small number of cases reported clearly highlights the serious nature of under-reporting in pharmacosurveillance programmes.
Spontaneous reporting schemes are a systematised attempt to collect case reports of suspected ADRs.[22] Spontaneous, voluntary reporting of ADRs is the most widely used method to detect ADRs after drugs have been marketed. A number of national and international reporting and monitoring programmes to collect case reports of ADRs have been established including the CADRMP, WHO and FDA MedWatch Program. Other case population surveillance schemes, such as the Euronet project[23] and the registry of severe cutaneous adverse reactions in Germany[24] have been established to evaluate the risk of severe adverse events or severe cutaneous adverse reactions.
The goal of post-marketing spontaneous reporting studies is to identify trends and signals of ADRs. Spontaneous reports play a major role in the identification of new drug hazards, especially when the reaction cannot be predicted or when the incidence rate is low. A signal is defined as the detection of early warning signs.[25] Spontaneous reports may also form the basis for identifying risk factors associated with certain ADRs. Reports to ADR programmes generally start immediately after a new drug is marketed and continue indefinitely throughout the life of the drug and programme. Reports may also be submitted prior to marketing if the product is available through the special access program.
Based on the results of this analysis, there is severe under-reporting of TEN to the CADRMP. Burn facilities across Canada reported more than a 10-fold difference in the number of TEN cases reported from only 64% of the burn treatment units when compared with the number reported to the CADRMP. The number of cases reported to CIHI’s discharge abstract database exceeds the estimated incidence rate of 1 per 1 million.[2,24]
We suspect that there is more under-reporting of TEN in Canada than revealed in this analysis. We hypothesise that it is likely that more TEN cases were admitted to the burn care facilities that did not respond to our requests for cases. Moreover, some TEN patients may not have been treated in burn units. TEN patients could also be admitted to a medical ward, dermatological ward or intensive care unit. Availability and accessibility may play a role in admission to burn facilities. For this analysis, we focused only on burn units because they are specialised facilities and are limited in number. A search of all Canadian hospitals with medical, dermatological and intensive care wards would not have been logistically possible given the number of contacts necessary, the retrospective nature of the study design and the variable nature of staffing. Here, CIHI data was used to approximate the number of admissions for TEN with the caveat that diagnosis with an ICD-9-CM code may have introduced some uncertainty. There was also uncertainty around the CADRMP cases with cases being labelled as TEN, TEN/SJS, TEN/EM and TEN/EM/SJS. This ambiguity may hinder the signal detection process. Despite the ability to collect the numerator, the exposure or denominator in the equation needed to determine the incidence of the event are not obtainable with a spontaneous pharmacovigilance system.
Alternatively, there may have been over-reporting of TEN. Data from CIHI provided an overwhelming number of cases (n = 4349). This large number may be due in part to the multi-diagnostic 695.1 code for TEN. Consequently, only a small proportion of cases admitted to the hospitals may have been considered TEN cases. The number of unique cases reported here may decrease in number as the quality of patient information improves.
It is important to note that information on the number of cases from CIHI was not reported when there were five of fewer cases in that year. Consequently, a minimum of one case per year or as many as five cases per year could have been discharged. A range of the number of possible cases was presented.
Under-reporting is not unique to Canada. Other countries and organisations with spontaneous reporting programmes have also commented on the gravity of under-reporting.[16,26] Under-reporting can also be evaluated within the context of the clinical trial. Ioannidis and Lau found that safety reporting in clinical trials was inadequate and often neglected.[27]
Other examples of under-reporting of ADRs exist. Inman[28] noted that only 5 of 44 cases of fatal aplastic anaemia due to phenylbutazone and oxybutazone were reported spontaneously to the UK Yellow Card system. Another study found that <1% of suspected serious ADRs are reported directly to the FDA.[29] Alvarez-Requejo and colleagues[30] quantified the extent of and the factors contributing to under-reporting in a general practice population in Spain. Researchers compared the reports received by a regional pharmacovigilance centre to those collected by a short and intensive survey in a randomised sample of general practitioners. An under-reporting coefficient was calculated as the ‘ratio between the number of effects actually observed by physicians and those spontaneously reported to the pharmacovigilance system’.[30] Results showed that the rate of ADR under-reporting was considerable. The rate of under-reporting was lower for newly marketed drugs and for unlabelled effects. Moride and colleagues[31] examined a random sample of 100 general practitioners practising in the region of the Bordeaux Pharmacovigilance Centre in France. Physicians were asked to report drug related-adverse events over a 3-day non-consecutive period. Results were then compared with those received by the regional pharmacovigilance centre. Results showed that under-reporting was lowest for serious, unlabelled effects and newly marketed drugs.
Reasons for not reporting ADRs are complex. Lack of knowledge about the existence of the national ADR monitoring programme, lack of ADR recognition, lack of clarity about the definition of an ADR, lack of report forms, lack of contact information for reporting agency, lack of clarity about how to report, lack of time needed to report, bias, and fear of liability have all been cited as reasons for underreporting.[32–34]
It is important to note that even when cases are reported to ADR programmes, the information submitted may be incomplete.[35] ADR submission forms prompt the reporter to enter case-specific information such as outcome, description of reaction, relevant tests/laboratory data, patient history, medication information, dechallenge (discontinuation of medication) and rechallenge (patients receive same medication again). This information may not be reported because the variables are unavailable to the reporter at the time of reporting. Such data is crucial in the determination of an association between drug exposure and ADR. Other limitations include the following: (i) incidence and scope of the ADR cannot be estimated because the number of adverse drug events actually occurring and the number of events actually reported may not be the same; (ii) the type of information that can be collected and entered into a national database is limited by programme time and resource restraints; (iii) there is often a significant delay of signal generation; and (iv) causality assessment may not be done on a regular basis at the CADRMP.[35]
For serious ADRs, such as TEN, more comprehensive information including laboratory and diagnostic findings, treatments, genetics and outcomes specific to TEN may be required to determine causality.
Possible limitations of this investigation include the multi-diagnostic nature of the ICD-9-CM code, the retrospective study design, quality of the reports, denominator, causality assessments and absence of data from some regions. The retrospective nature of the analysis may be affected by recall bias. A prospective study design would improve the accuracy of the number of cases. Diagnosis of TEN may be variable. Matching cases was difficult due to the incomplete nature of the ADR reports. Cases from some burn treatment centre respondents were provided in an ICD-9-CM diagnosis format. In this format it was unclear which patients were diagnosed with TEN, SJS or EM. Most importantly, there are some limitations with the denominator obtained. As the burn unit data only represented 64% of the facilities across Canada, it is possible that the proportion derived would result in an inflation of the ratio or a decreased estimate of under-reporting. The CIHI data is not specific for the diagnosis of TEN, so there will be over estimation of the denominator resulting in a higher estimate of under-reporting. The CADRMP may represent a more severe group of the ICD patients as they were reported. Causality assessment information was not collected because the CADRMP did not conduct formal and systematic causality assessments on this patient group and CIHI did not collect information on ‘causative’ agents. Data from burn centres was lacking from several areas and provinces across the country where there was a high incidence of TEN according to CIHI data. This lack of information may skew the study outcomes. This study assumed that all cases in burn units were diagnosed as TEN. It is possible that some of these cases may have been SJS or EM. Access to medical records would have provided information for the differential diagnosis of TEN.
Despite the study limitations, the message regarding the extent of under-reporting is clear. There were at least 272 unique cases of TEN over a 6-year time-period across Canada between 1995 and 2000. Given the population of Canada (n = 30 750 087),[36] it was estimated that the incidence of TEN was at least 1 per 100 000. This was a conservative estimate for incidence as we did not collect cases from all burn care facilities or those cases admitted to other hospital units (i.e. dermatology, intensive care units). There may be as few as four (CADRMP: 25 cases in 6 years or approximately four per year); 45 (272 unique cases from CADRMP plus burn unit in 6 years); or 112 (CIHI: 674 for 6 years or 112 per 1 year) cases of TEN per year in Canada. The incidence could vary between 1 in 10 million and 1 in 250 000 persons per year.
Conclusions
There is serious under-reporting of adverse drug events on a global scale. Lack of reporting of serious and life-threatening adverse events can compromise population safety. Understanding adverse events is important in the determination of rational therapeutics and is fundamental in ensuring the safer use of medications. The studied example highlights the need for increasing awareness of the existence of the voluntary reporting systems. Recognition of the importance of reporting may improve the number of cases sent to voluntary reporting agencies. The establishment of ADR registries, active surveillance or electronic voluntary adverse event reporting programs to collect and evaluate serious life-threatening cases may aid in the signal detection process.
References
Roujeau J, Guillaume J, Fabre J, et al. Toxic epidermal necrolysis (Lyell syndrome): incidence and drug etiology in France, 1981-1985. Arch Dermatol 1990; 126: 37–42
Schopf E, Stuhmer A, Rzany B, et al. Toxic epidermal necrolysis and Steven’s Johnson syndrome: an epidemiologic study from West Germany. Arch Dermatol 1991; 127: 839–42
Chan H, Stern R, Arndt K, et al. The incidence of erythema multiforme, Stevens-Johnson syndrome and toxic epidermal necrolysis: a population-based study with particular reference to reactions caused by drugs among outpatients. Arch Dermatol 1990; 126: 43–7
Palmieri T, Greenhalgh D, Saffle J, et al. A multicentre review of toxic epidermal necrolysis treated in US burn centres at the end of the twentieth century. J Burn Care Rehabil 2002; 23: 87–96
Revuz J, Penso D, Roujeau J, et al. Toxic epidermal necrolysis: clinical findings and prognosis factors in 87 patients. Arch Dermatol 1987; 123: 1160–5
Heimach D, Engrav L, Marvin J, et al. Toxic epidermal necrolysis: a step forward in treatment. JAMA 1987; 257: 2171–5
Roujeau J, Stern R. Severe cutaneous reactions to drugs. N Engl J Med 1994; 331: 1272–83
Eisen E, Fish J, Shear N. Management of drug-induced toxic epidermal necrolysis. J Cutan Med Surg 2000; 4(2): 96–102
Becker D. Toxic epidermal necrolysis. Lancet 1998; 351: 1417–20
Schwartz R. Toxic epidermal necrolysis. Cutis 1997; 59: 123–7
Chang D, Shear N. Cutaneous reactions to anticonvulsants. Semin Neurol 1992; 12: 329–37
Halebian P, Madden M, Finkelstein J, et al. Improved burn centre survival of patients with toxic epidermal necrolysis managed without corticosteroids. Ann Surg 1986; 204: 503–12
Avakian R, Flowers F, Araujo O, et al. Toxic epidermal necrolysis: a review. J Am Acad Dermatol 1991; 25: 69–79
Stern R, Chan H. Usefulness of case report literature in determining drugs responsible for toxic epidermal necrolysis. J Am Acad Dermatol 1989; 21: 317–22
Roujeau J, Kelly J, Naldi L, et al. Medication use and risk of Stevens-Johnson syndrome or toxic epidermal necrolysis. N Engl J Med 1995; 333: 1600–7
MEDWATCH. The clinical impact of adverse event reporting. Washington, DC: Department of Health and Human Services, 1996
Naranjo C, Busto U. Adverse drug reactions. In: Kalant H, Roschlau W, editors. Principles in medical pharmacology. 5th ed. Toronto: BC Decker, 1989: 658–65
Canadian Institute for Health Information (CIHI) [online]. Available from URL: http://www.cihi.ca [Accessed 2004 Apr]
Statistics Canada, Population Estimates [online]. Available from URL: http://www.statcan [Accessed 2004 Apr 21]. ca/Daily/English/00 0926, 2000
Health Canada. Canadian adverse drug reaction newsletter. Ottawa (ON): Therapeutic Products Programme, 2003
US FDA Annual Adverse Drug Experiences Report 1996 [online]. Available from URL: http://www.fda.gov/medwatch/articles.htm [Accessed 2004 Apr]
Venning G. Identification of adverse reactions to new drugs III: altering process and early warning. BMJ 1983; 286: 458–60
Capella D, Laporte J, Vidal X, et al. European network for the case-population surveillance of rare disease (Euronet): a prospective feasibility study. Eur J Clin Pharmacol 1998; 53: 299–302
Mockenhaupt M, Schopf E. Epidemiology of drug-induced severe skin reactions. Semin Cutan Med Surg 1996; 15(4): 236–43
Meyboom R, Egberts A, Edwards I, et al. Principles of signal detection on Pharmacovigilance. Drug Saf 1997; 16(6): 355–65
Olsson S. The role of the WHO programme on international drug monitoring in coordinating world-wide drug safety efforts. Drug Saf 1998; 19(1): 1–10
Ionnidis J, Lau J. Completeness of safety reporting in randomized trials: an evaluation of 7 medical areas. JAMA 2001; 285: 437–43
Inman W. Study of fatal bone marrow depression with special reference to phenylbutazone and oxybutazone. BMJ 1977; 1: 1500–5
Scott H, Rosenbaum S, Waters W, et al. Rhode Island physician’s recognition and reporting of adverse drug reactions. R I Med J 1987; 70: 311–6
Alvarez-Requejo A, Carvajal A, Begaud B, et al. Under-reporting of adverse drug reactions: estimate based on a spontaneous reporting scheme and a sentinel system. Eur J Clin Pharm 1998; 54: 483–8
Moride Y, Haramburu F, Requejo A, et al. Under-reporting of adverse drug reactions in general practice. Br J Clin Pharmacol 1997; 43: 177–81
Belton K. Attitude survey of adverse drug-reaction reporting by healthcare professionals across the European Union. Eur J Clin Pharm 1997; 52(6): 423–7
LaCalamita S. Top 10 reasons for not reporting adverse drug reactions. Hosp Pharm 1995; 30(3): 245–6
Colodny L, Spillane J. Toward increased reporting of adverse drug reactions. Hosp Pharm 1999; 34(10): 1179–85
Mittmann N, Liu BA, Iskedjian M, et al. Drug-related deaths in Canada (1984-1994). Pharmacoepidemiol Drug Saf 1997; 6: 157–68
Statistics Canada Population, 2000 [online]. Available from URL: http://www.statcan [Accessed 2004 Apr 21]
Acknowledgements
No funding was used to assist in the preparation of this manuscript and there are no potential sources of conflict that are directly relevant to the contents of this manuscript.
The authors would like to thank the burn facilities that responded to the request for toxic epidermal necrolysis (TEN) cases. We would like to thank the Canadian Institute for Health Information (CIHI) for providing information on the Canadian profile of TEN. The authors would like to thank the Canadian Adverse Drug Reaction Monitoring Program (CADRMP) for the list of reported TEN cases. The opinions expressed in this paper do not reflect those of Health Canada.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Mittmann, N., Knowles, S.R., Gomez, M. et al. Evaluation of the Extent of Under-Reporting of Serious Adverse Drug Reactions. Drug-Safety 27, 477–487 (2004). https://doi.org/10.2165/00002018-200427070-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200427070-00004