Abstract
Objective: To establish the frequency with which anxiolytic and sedative drugs result in fatal poisonings and to examine longitudinal changes in poisoning deaths.
Method: The number of fatal poisonings between 1983 and 1999 in England, Scotland and Wales due to a single anxiolytic or sedative drug was obtained from the Department of Health in the UK. This was divided by the number of prescriptions for these drugs in England and Scotland to derive a fatal toxicity index (FTI) of deaths per million prescriptions.
Results: Chloral hydrate, clomethiazole, barbiturates, and related sedatives had much higher FTIs than benzodiazepines, buspirone, zolpidem and zopiclone. There has been a substantial reduction in the annual number of deaths from sedative drug poisoning between 1983 and 1999. This has been due to a sustained reduction in prescriptions for high toxicity drugs and more recently a major reduction in temazepam deaths that coincided with the withdrawal of gelatin capsule formulations.
Conclusion: Deaths would be expected to be further reduced if there were reduced prescriptions of high toxicity drugs — and the continuing need for short-acting barbiturates, clomethiazole and chloral hydrate should be questioned.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anxiolytic and sedative drugs are among the most common drugs leading to fatal poisoning.[1,2] Any comparison of these drugs in terms of their fatal toxicity must be done using coronial data (or information from the procurator fiscal system in Scotland) as most of these deaths occur out-of-hospital. To facilitate comparisons previous authors have calculated fatal toxicity indices (FTI).[3,4] The number of fatal poisonings is divided by measures of drug usage to give a FTI of deaths per million prescriptions or deaths per million patient-years. Despite many limitations of FTIs,[5] such estimates of the relative toxicity in overdose of drugs are the best means we have of comparing fatal toxicity in human overdose. Two previous studies have examined the fatal toxicity of some of these drugs in the UK.[4,6] Neither examined toxicity due to a number of non-benzodiazepine non-barbiturate drugs or examined longitudinal trends. The aim of this paper is to establish the frequency with which anxiolytic and sedative drugs resulted in fatal poisoning and to look for longitudinal changes in the FTI.
Methods
We examined the fatal toxicity of anxiolytic and sedative drugs for the years 1983–1999. The number of deaths in England, Wales and Scotland due to acute poisoning by a single drug alone with or without alcohol co-ingestion was obtained from the Office for National Statistics[7] (England, Wales) and the General Registrar’s Office (Scotland). Fatal poisonings due to multiple drugs (about 30–40% of the total) are excluded. The number of prescriptions for England and Scotland, as supplied by their Departments of Health for these years, was used as a measure of relative drug usage.
There have been some changes in data collection over time. The English prescription data from 1983–1990 are based on fees and on a sample of 1 in 200 prescriptions dispensed by community pharmacists and appliance contractors only. The data from 1991–1999 are based on items and cover all prescriptions dispensed by community pharmacists, appliance contractors, dispensing doctors and prescriptions submitted by prescribing doctors for items personally administered. There have also been some changes in practices for coding for poisoning deaths. This has involved changing to automated methods in 1996 and the inclusion of 304.x codes (from the International Classification of Diseases, 9th and 10th revisions) [poisoning due to drug dependence] in Scottish poisoning deaths from 1993.[8]
For each drug, we calculated a FTI expressed as deaths per million prescriptions. This was calculated by dividing the number of deaths attributed to an overdose of the drug in England, Scotland and Wales over these years by the total number of prescriptions for the drug (in England and Scotland alone) for the years 1983–1999. No data on prescriptions are available for Wales before 1994 and we did not include any of their data in this longitudinal study. Welsh data has not been included in most previous FTIs including those performed on this class of drugs.[3–6] In a previous study on antidepressants, Welsh prescriptions only accounted for between 5 and 7% of the annual total of UK prescriptions.[9]
Ninety-five percent CIs were calculated by assuming the prescriptions (i.e. the denominator of the FTI) were fixed and that the deaths followed a Poisson distribution. The 95% CI limits were obtained for the deaths from exact CIs for a Poisson distribution.[10] These limits were divided by the prescription count to obtain the lower and upper confidence limits for the FTI.
Results
The results are presented in table I and table II with the drugs listed within their class in descending order of the FTI. The overall results were as follows: 1458 deaths associated with sedative benzodiazepines and a total of 198 026 000 prescriptions, giving a mean FTI of 7.4 (95% CI 7.0–7.7); 818 deaths associated with barbiturates and a total of 5 594 000, giving a mean FTI of 146.2 (95% CI 136–156); and 387 deaths associated with benzodiazepine anxiolytics and a total of 130 493 000 prescriptions, giving a mean FTI of 3.0 (95% CI2.7–3.3).
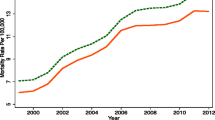
Longitudinal changes in prescriptions and deaths are shown in figure 1. As can be seen, there has been a nearly 4-fold decline in the total number of deaths. In trying to explain this result we have divided the drugs into those with a high FTI (>30: barbiturates, chloral hydrate and betaine, clomethiazole) and those with a low FTI. There was a marked decline in deaths due to high toxicity drugs between 1983–1992 with only small further reductions since. In contrast, low toxicity drugs had a fairly constant number of deaths except for a sudden drop in 1995 (figure 1). We can see the effect in more detail by looking at the two main drug classes in these groups (benzodiazepines and barbiturates). The reduction in deaths due to barbiturates directly followed reduced prescriptions, with no substantial change over time in the FTI (deaths per million prescriptions) [figure 2]. Similar results were seen with the other high toxicity drugs (data not shown). In contrast, the marked reduction in deaths due to low FTI drugs in 1995 was due to reduced benzodiazepine deaths but was not associated with any significant reduction in prescriptions (figure 2). Further examination of the data revealed that this reduction was largely due to reduced temazepam deaths from 1995 onwards (figure 3). In 1994, temazepam accounted for the majority of benzodiazepine deaths. The reduction appeared to coincide with a major reduction in prescribing of temazepam gelatin capsule preparations prior to their complete removal from the National Health Service (NHS) and rescheduling in January 1996. Earlier reductions in non-temazepam benzodiazepine deaths partially reflect the removal of flurazepam and flunitrazepam (the two with the highest FTIs) from the market in 1986. There was an increase in temazepam prescriptions and deaths at the same time (figure 3).
The utility of using FTIs for postmarketing surveillance for sedatives is demonstrated by showing a cumulative FTI and CI in figure 4. It can be seen that the safety in overdose of zopiclone, the first drug of a new sedative class, was established as being of the same order as the benzodiazepines after about a million prescriptions (and only four deaths) within a few years of marketing. At this time the FTI was 5.5 (95% CI 1.5–14). The FTI based on the full ten million prescriptions and 23 deaths was within this CI but it took 10 years to show that zopiclone may in fact have a slightly lower FTI than some more commonly prescribed benzodiazepine sleeping tablets (see also table I).
Discussion
The calculated FTIs confirm previous observations for benzodiazepines and barbiturates.[4,6] It is for other sedative and anxiolytic drugs that the most interesting results are observed. Thus, the very high FTIs for clomethiazole and the chloral hydrate/chloral betaine sedatives have not been previously noted. Chloral hydrate is known to be a very potent sedative with a low therapeutic index, particularly in patients with cardiac disease.[11] The high FTI for clomethiazole, similar to that observed for barbiturates, must also raise concerns about the continuing use of this drug. The dramatic effect of removing temazepam gelatin capsules (figure 3) suggests that even for ‘low toxicity’ drugs there may be scope for improvement in sedative drug overdose mortality if they are being deliberately abused. The very low FTIs for some newer drugs such as zopiclone, zolpidem and buspirone are reassuring and support the use of FTIs for post-marketing surveillance of overdose toxicity.
We have concluded that these FTIs largely reflect the inherent toxicity of these drugs. However, it is not possible from the coronial data to exclude the possibilities that drugs are more frequently taken, or are prescribed for or taken in overdose by an at-risk group. There are a number of characteristics of the patients for whom these drugs have been prescribed which might influence the choice of drug and also alter their risk of poisoning or their risk of death if poisoned. These would include age, gender, other medical conditions, whether the drugs were prescribed for drug dependence, psychiatric illness or other indications and whether some drugs were given specifically to counteract suicidal behaviour. These drugs are disproportionately used in suicide attempts[1] and some specific drug groups and individual drugs are recommended in books and on the Internet for suicide by active euthanasia lobby groups.[12,13] The perceived risk of overdose with each drug has the potential to confound the relationship with fatal toxicity. For example, if prescription of barbiturates is avoided in those deemed to be at risk of suicide, this would tend to reduce differences in the FTI. However, if people wishing to commit suicide were aware of the toxicity of barbiturates in overdose from publicly available sources, they may preferentially seek barbiturates for overdose.[13] Also, particular drugs are used in the treatment of drug or alcohol addiction (e.g. clomethiazole) or are abused (e.g. temazepam gelatin capsules).[14,15] Alcohol potentiates the sedative effects of these drugs and these patients also have a disproportionately higher risk of suicide or accidental poisoning, both of which may increase the FTI for these drugs.[16,17] However, both diazepam and clomethiazole are used in alcohol withdrawal, but the FTI of diazepam was still 30-fold lower than that of clomethiazole. This suggests substitution of diazepam for clomethiazole in the treatment of alcohol withdrawal may lead to further reduction in fatal poisonings. Most fatal toxicity studies including ours have used prescriptions rather than a measure of the number of people using the drug. Previously we found only minor differences in the rank order when we have compared these figures with FTIs calculated as deaths per million years of use in the UK for these and other groups of drugs.[5,18] Unfortunately, permission to publish the drug usage data has not been provided and this analysis can not be presented in this paper.
A couple of further limitations apply to observations of longitudinal trends. As noted in the methods section there have been small changes in coding of deaths over this time and there may have been other gradual changes that might have occurred that would change the data used to record the FTI. For example, the size of prescriptions might have changed, or influencing the attribution of death to a single drug by the coroner there may have been improvements in analytical techniques which detected more co-ingestions. There have also been changes in the overall rates of suicide, at least partly attributed to changing methods of suicide and birth cohort effects.[19,20] It is unclear what impact this might have on the indexes, although despite considerable yearly fluctuations there are no large differences between the overall barbiturate FTI at the beginning and end of the study period and the only change in the overall benzodiazepine FTI is explained on other grounds (figure 2). However, small differences between data from the beginning and end of this time frame (for example, the relative toxicity of benzodiazepines that were removed from the market in the 1980s compared with the newer agents such as zolpidem and zopiclone) should probably be interpreted conservatively.
It is unlikely that any of the potential confounders considered above could explain 10-fold differences within drug classes and even larger differences across all these drugs. These differences in fatal toxicity have also been supported by studies comparing the relative clinical toxicity of these drugs and by studies that include coronial data from other countries.[1,12,21] So, using such data, how should we assess the safety of both new and old drugs used as sedatives or anxiolytics? It is all too common for the safety in overdose of new drugs to be proclaimed on the basis of benign outcomes in a selected group of hospital admissions. However, even the most lethal sedatives rarely require more than supportive therapy after admission to hospital,[11] and the vast majority of lethal overdoses do not present to medical attention.[22] The contrast between the in-hospital course of benzodiazepine poisonings and the observation that temazepam was the sixth most common single cause of fatal poisoning in the UK further emphasises this point.[2,21] Although there is evidence that the coroner’s recording of cause of death may frequently be incomplete or inaccurate from a toxicological perspective,[23] it is probably the best means available for assessing the toxicity in overdose after a drug has been marketed. As can be seen with the data on zopiclone, this can be established within a few years of marketing (figure 4).
For a number of older drugs, data about their toxicity in overdose is available from a number of sources.[1–3,6,21] The FTI calculated in this study make it even more difficult to justify continuing prescription of short acting barbiturates and related sedatives such as meprobamate and glutethimide. These older sedatives are also taken more frequently in overdose than most other drugs, have greater toxicity in animal studies and clinical series and are also frequently abused.[1] Equally effective and safer drugs, such as the benzodiazepines, zopiclone and zolpidem, can be substituted for all indications. Most of the same criticisms can be made of the chloral group of sedatives and clomethiazole. These drugs would probably not be granted a marketing licence if developed now, but remain available only due to their ‘grandfather’ status. Their availability should be restricted as far as possible to reduce fatal poisonings. It is apparent from the experience with temazepam gelatin capsules that further scheduling changes may be necessary to further decrease deaths selectively abused. A number of voluntary less restrictive measures such as warnings and educational initiatives conducted through the early 1990s[24–26] were superficially successful in decreasing prescriptions of the gelatin capsules. However, it was only rescheduling that appears to have been successful in significantly reducing temazepam deaths (figure 3). A ban on clomethiazole, short acting barbiturates and chloral hydrate and betaine might be expected to nearly halve the current (greatly reduced) rate of deaths due to sedative drug poisoning in the UK (figure 1). Other countries that have been slower to adopt restrictions and still have larger problems with poisoning with barbiturates[27] and abuse of temazepam gelatin capsules[28] may have even more to gain.
References
Buckley NA, Whyte IM, Dawson AH, et al. Correlations between prescriptions and drugs taken in self-poisoning: implications for prescribers and drug regulation. Med J Aust 1995; 162(4): 194–7
Crome P. The toxicity of drugs used for suicide. Acta Psychiatr Scand Suppl 1993; 371: 33–7
King LA, Moffat AC. Hypnotics and sedatives: an index of fatal toxicity. Lancet 1981; I(8216): 387–8
Serfaty M, Masterton G. Fatal poisonings attributed to benzodiazepines in Britain during the 1980s. Br J Psychiatry 1993; 163: 386–93
Buckley NA, McManus PR. Can the fatal toxicity of antidepressant drugs be predicted with pharmacological and toxicological data? Drug Saf 1998; 18(5): 369–81
King LA, Moffat AC. A possible index of fatal drug toxicity in humans. Med Sci Law 1983; 23(3): 193–8
Office of National Statistics. Deaths from poisoning by solid or liquid substances: accidental, suicidal and undetermined whether accidentally taken or purposely inflicted, 1983–1999. London: HMSO, 2001
Jackson GWL. Drug-related deaths in Scotland in 2000 [online]. Available from URL: http://www.gro-scotland.gov.uk/grosweb/grosweb.nsf/pages/00ddeaths [Accessed 2002 Dec 12]
Buckley NA, McManus PR. Fatal toxicity of serotoninergic and other antidepressant drugs: analysis of United Kingdom mortality data. BMJ 2002; 325: 1332–3
Lentner C. Geigy scientific tables. Vol. 2. Introduction to statistics: statistical tables. Mathematical formulae. 8th ed. Basle: Ciba Geigy Ltd, 1984
Ellenhorn MJ. Medical toxicology: diagnosis and treatment of human poisoning. 2nd ed. Baltimore (MD): Williams & Wilkins, 1998
Michel K, Waeber V, Valach L, et al. A comparison of the drugs taken in fatal and nonfatal self-poisoning. Acta Psychiatr Scand 1994; 90(3): 184–9
Marzuk PM, Tardiff K, Leon AC. Increase in fatal suicidal poisonings and suffocations in the year Final Exit was published: a national study. Am J Psychiatry 1994; 151(12): 1813–4
Naik P, Lawton J. Pharmacological management of alcohol withdrawal. Br J Hosp Med 1993; 50(5): 265–9
Robertson JR, Roberts JJ, Black H, et al. Management of drug abuse. Lancet 1987; II(8553): 284–5
Ekeberg O, Ellingsen O, Jacobsen D. Mortality and causes of death in a 10-year follow-up of patients treated for self-poisonings in Oslo. Suicide Life Threat Behav 1994; 24(4): 398–405
Madden JS. Alcohol and depression. Br J Hosp Med 1993; 50(5): 261–4
Buckley NA, McManus PR. The fatal toxicity index (FTI) of anxiolytic and sedative drugs in the UK (1983-1999) [abstract]. J Toxicol Clin Toxicol 2002; 40(3): 344
Gunnell D, Middleton N, Whitley E, et al. Influence of cohort effects on patterns of suicide in England and Wales, 1950-1999. Br J Psychiatry 2003; 182: 164–70
Gunnell D, Wehner H, Frankel S. Sex differences in suicide trends in England and Wales. Lancet 1999; 353(9152): 556–7
Buckley NA, Dawson AH, Whyte IM, et al. Relative toxicity of benzodiazepines in overdose. BMJ 1995; 310(6974): 219–21
Buckley NA, Whyte IM, Dawson AH, et al. Self-poisoning in Newcastle, 1987-1992. Med J Aust 1995; 162(4): 190–3
Dwyer PS, Jones IF. Fatal self-poisoning in the UK and the paracetamol/dextropropoxyphene combination. Hum Toxicol 1984; 3Suppl.: 145S–74S
Crompton B. Misuse of benzodiazepines: voluntary ban on prescribing is effective. BMJ 1994; 308(6945): 1709
Innes CF, Cotter JC, Davies P, et al. Misuse of temazepam. BMJ 1992; 305(6857): 832–3
Grahame-Smith DG. Misuse of temazepam [letter]. BMJ 1991; 302(6786): 1210
Hatzitolios AI, Sion ML, Eleftheriadis NP, et al. Parasuicidal poisoning treated in a Greek medical ward: epidemiology and clinical experience. Hum Exp Toxicol 2001; 20(12): 611–7
Feeney GF, Gibbs HH. Digit loss following misuse of temazepam. Med J Aust 2002; 176(8): 380
Acknowledgements
We would like to thank Zoe Uren of the Office for National Statistics, Graham Jackson of the General Register Office for Scotland, Bill Gold of ISD, Primary Care Information Unit, Scotland, and Andy Savva of the Statistics Division of the Department of Health, England for supplying the data on which this analysis is based.
The authors have no conflicts of interest directly relevant to the content of this study. No sources of funding were used to assist in the preparation of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Buckley, N.A., McManus, P.R. Changes in Fatalities Due to Overdose of Anxiolytic and Sedative Drugs in the UK (1983–1999). Drug-Safety 27, 135–141 (2004). https://doi.org/10.2165/00002018-200427020-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200427020-00004