Abstract
We and others have reported that Rho-kinase plays an important role in the pathogenesis of heart ischemia/reperfusion (I/R) injury. Studies have also demonstrated that the activation of Rho-kinase is reversed in ischemic preconditioning (IPC). However, the mechanisms by which Rho-kinase is increased in I/R and reversed in IPC are not thoroughly understood. In female Wistar rats, we created I/R by ligating the left anterior-descending branch of the coronary artery (LAD) for 30 min and releasing the ligature for 180 min. IPC rats underwent IPC (two cycles of 5-min ligation of the LAD and 5-min reflow) before I/R. IPC caused a significant increase in extracellular signal-regulated kinase (ERK)1/2 activity and reduced Rho-kinase activity and cardiomyocyte apoptosis (P < 0.05 versus I/R). Administration of PD98059, an inhibitor of ERK-mitogen-activated protein kinase (MAPK), increased cardiomyocyte apoptosis, Caspase-3 activity and myocardial infarction size (P < 0.05 versus IPC). Western-blot analysis showed that administration of PD98059 increased Rho-kinase activity. Treatment with fasudil, an inhibitor of Rho-kinase, reversed cell apoptosis caused by treatment with PD98059 in IPC. In addition, ROCK1 (Rho-kinase 1) may be the major Rho-kinase isoform that is opposed by ERK-MAPK signaling in IPC. These results indicate that ERK-MAPK signaling is required in IPC to oppose Rho-kinase activity in cardiomyocyte apoptosis in vivo.
Similar content being viewed by others
Introduction
In the prototypical mechanism of RhoA GTPase signaling, various environmental cues, acting through G-protein-coupled receptors or receptor-dependent and -independent tyrosine kinases, activate guanine-nucleotide exchange factors, which induce exchange of guouosine diphosphate (GDP) for GTP binding and translocation of GTP-RhoA to the plasma membrane. Upon translocation to the plasma membrane, GTP-RhoA activates one or more of its effectors, including the ubiquitously expressed Rho-kinase. Rho-kinase plays crucial roles in various cellular functions, and mediates cellular events such as changes in cell morphology, cell motility, focal adhesions and cytokinesis (1,2). The myosin-phosphatase target subunit (MYPT-1) is the major effector of Rho-kinase. To date, two iso-forms of Rho-kinase have been cloned, Rho-kinase 1 (ROCK1) and ROCK2. Both isoforms are about 160 kD, with 92% homology at the kinase domain (3). Accumulating evidence demonstrates that Rho-kinase plays important roles in many major cardiovascular diseases such as hypertension, heart failure, myocardial infarction and atherosclerosis. Results of recent animal studies suggest that inhibition of Rho-kinase protects the heart against ischemia/reperfusion (I/R) injury (4). We demonstrated recently that the inhibition of Rho-kinase reduces cell apoptosis in I/R in vivo via suppression of the translocation of JNK (c-Jun NH2-terminal kinase)-mediated apoptosisinducing factor (5).
Ischemic preconditioning (IPC) has been exploited as a powerful endogenous form of cardioprotection. IPC was first discovered by Murry and associates (6), who demonstrated that a brief period of repetitive cardiac I/R exerts a protective effect against subsequent lethal periods of ischemia. IPC was found to similarly reduce cytosolic and mitochondrial Ca2+ overloading, to augment postischemic functional recovery and to decrease infarct size (7). In addition, IPC is known to decrease cardiomyocyte apoptosis during reperfusion. Previous studies have demonstrated that IPC causes a substantial decrease of Rho-kinase activation during sustained ischemia and reduces infarct size (8). In this study, we also observed that the activation of Rho-kinase induced by I/R was significantly attenuated by IPC. However, little is known about the mechanisms by which Rho-kinase activity is increased in I/R and decreased in IPC. Therefore, the aim of this study was to elucidate the mechanism of decreased Rho-kinase activity in IPC.
Materials and Methods
All procedures were performed in conformity with the Institutional Animal Care and Use Committee and National Institutes of Health guidelines.
Myocardial I/R and IPC
Female Wistar rats (body weight 250–300 g, from Shandong University, Shandong Province, China) were maintained under conditions of standard lighting (alternating 12-h light/dark cycles), temperature (22°C ± 0.5°C) and humidity (60% ± 10%) for at least 1 wk before the experiments. The rats were anesthetized with sodium pentobarbital (50 mg/kg intraperitoneally). The trachea was cannulated with a PE-90 catheter, and artificial respiration was provided by a respirator with an FiO2 (fraction of inspired oxygen) of 0.80, a frequency of 100 strokes/min and a tidal volume of 0.8 to 1.2 mL to maintain normal PO2 (partial pressure of oxygen), PCO2 (partial pressure of carbon dioxide) and pH. A left lateral thoracotomy was made in the fourth intercostal space; the skin, muscles and ribs were retracted; and the pericardial sac was removed. The left-anterior branch of the descending coronary artery (LAD) was occluded by ligation with a 4–0 silk suture. The LAD ligation was performed by using an easily opened knot set on a PE50 silicon tube lying over the LAD. After 30 min of ischemia, the ligation was loosened and reperfusion occurred. Rats were killed at 180 min of reperfusion. The sham control animals were subjected to the entire surgical procedure and the silk suture was passed beneath the coronary artery, but the LAD was not ligated.
IPC was introduced by two cycles of 5 min of ischemia followed by 5 min of reperfusion. The rats were then subjected to 30 min of LAD occlusion followed by 180 min of reperfusion similar to that performed in the I/R rats.
Experimental Groups
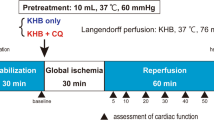
The experimental groups we studied (Figure 1) were as follows:
The IR group (control group; n = 12) underwent 30-min ischemia and 180-min reperfusion.
The IPC group (n = 12) underwent two cycles of 5-min ischemia followed by 5-min reperfusion before sustained ischemia.
The IPC + PD98059 group (n = 12) underwent two cycles of 5-min ischemia followed by 5-min reperfusion before sustained ischemia plus administration of PD98059, an inhibitor of extracellular signal-regulated kinase (ERK)1/2 (9). PD98059 was dissolved in 100 µL dimethylsulfoxide (DMSO), and 0.3 mg/kg was administered intravenously between the onset and two brief periods of ischemia.
The IPC + fasudil group (n = 12) underwent two cycles of 5-min ischemia followed by 5-min reperfusion before sustained ischemia plus administration of fasudil, an inhibitor of Rho-kinase, (10 mg/kg intravenously) (10).
The IPC + PD98059 + fasudil group (n = 12) underwent two cycles of 5-min ischemia followed by 5-min reperfusion before sustained ischemia plus administration of PD98059 and fasudil.
The IPC + DMSO group (n = 12) underwent two cycles of 5-min ischemia followed by 5-min reperfusion before sustained ischemia plus administration of 100 µL DMSO.
Determination of Myocardial Infarct Size
At the end of reperfusion, the LAD coronary artery was reoccluded and Evans blue dye solution (3 mL, 2% wt/vol) was injected into the left ventricle to enable us to identify ischemic (area at risk [AAR], unstained) and nonischemic myocardium (area not at risk, stained blue). Then the hearts were harvested and rinsed in normal saline. The atria, right ventricle and great vessels were removed. The tissues were semifreezed for 30 min in a −20°C freezer so they could be sliced more easily. After that, the left ventricle was surgically isolated and cut into slices (1-mm thick). The AAR was separated from the area not at risk and then incubated with nitro-blue tetrazolium (1% wt/vol, 15 min at 37°C), which enabled us to distinguish between ischemic and infarcted tissue. After we evaluated the entire surface area, we designated segments with blue staining as viable and those without staining as nonviable (infarcted). Finally, the AAR and infarct size were calculated after the respective tissue samples were weighed, and the infarct size was expressed as the percentage of the AAR (11).
Terminal Deoxynucleotidyl Transferase-Mediated dUTP Nick-End Labeling
To evaluate apoptotic activity, we used the terminal deoxynucleotidyl transferase-mediated dUTP nick-end labeling (TUNEL) technique. Each section was deparaffinized and rehydrated with serial changes of xylene and ethanol. Proteinase K (20 mg/L) was applied to the section for 30 min to produce optimal proteolysis. The endogenous peroxidase was inhibited with 3% hydrogen peroxide for 10 min. A commercial apoptosis detection kit (Roche, Mannheim, Germany) was used. The TdT reaction was carried out for 1 h at 37°C in a humidified chamber, and then 3,3′-diaminobenzidine tetrahydrochloride chromogen was applied. Hematoxylin was used as a counterstain. TUNEL-positive cells were determined by random counting of 10 fields of the section and were expressed as a percentage of normal nuclei (12).
Immunohistochemical Staining for Phospho-ERK1/2
The 5-µm-thick, formalin-fixed, paraffinembedded sections were cut, deparaffinized and then rehydrated with graded alcohol and xylene. Endogenous peroxidase was blocked by using 3% hydrogen peroxide for 10 min, followed by a brief wash in Tris buffer (pH 7.2). Sections were boiled in citrate buffer (pH 6.0) with microwaves at 92°C–98°C for 10 min to retrieve the antigen. After blocking of nonspecific binding with 5% bovine serum albumin, the slides were incubated with primary antibody overnight at 4°C (antimouse phospho-ERK1/2 1:100; Santa Cruz Biochemicals, Santa Cruz, CA, USA). Sections were thoroughly washed in phosphate-buffered saline (PBS) and incubated with a peroxidase-conjugated polymer that carried antibodies to mouse (1:200) immunoglobulin for 30 min. After being rinsed with PBS, the sections were exposed for 5–10 min to 3,3′-diaminobenzidine tetrahydrochloride. The slides were rinsed in water and counterstained with hematoxylin and eosin. We used sections that were incubated with PBS instead of the primary antiserum as the negative controls. The sections were examined by using light microscopy and analyzed with a computer-assisted color-image analysis system (Image-ProPlus 5.0, Media Cybernetics, Bethesda, MD, USA).
Western Blot
Nuclear and cytoplasmic fractions were extracted by using a kit from Bipec Biopharma (Cambridge, MA, USA) according to the manufacturer’s instructions. Membrane fractions were extracted by using the kit from Keygen Biotech (Nanjing, China) according to the manufacturer’s instructions. Equal amounts of protein (50 µg) were fractionated on 10% sodium dodecyl sulfate-polyacrylamide gels in running buffer (25 mmol/L Tris, 192 mmol/L glycine, 0.1% [wt/vol] sodium dodecyl sulfate, pH 8.3) at 90 V and then electroblotted to nitrocellulose membranes. Membranes were blocked at room temperature with 5% nonfat milk in Tris-buffered saline (25 mmol/L Tris, 137 mmol/L NaCl, and 2.7 mmol/L KCl) containing 0.05% Tween-20 and then incubated overnight at 4°C with the following primary antibodies: β-actin (Santa Cruz Biochemicals; dilutions, 1:1000; molecular weight of β-actin, 43 kD), rabbit monoclonal antirat cleaved Caspase-3 antibody (Cell Signaling, Danvers, MA, USA; dilutions, 1:1000; molecular weight 17 or 19 kD), rabbit polyclonal antirat phospho-MYPT-1 (Thr850) antibody (Millipore, Billerica, MA, USA; dilutions: 1:1500; molecular weight 80 kD), rabbit polyclonal MYPT-1 antibody (bioWORLD, Dublin, Ohio, USA; dilutions, 1:500; molecular weight 130 kD), rabbit polyclonal p-MYPT-1 antibody (bioWORLD; dilutions, 1:500; molecular weight 130 kD), rabbit polyclonal RhoA antibody (bioWORLD; dilutions, 1:500; molecular weight 23 kD), rabbit monoclonal antirat ROCK1 antibody (Abcam, Cambridge, UK; dilutions, 1:1000; molecular weight 158 kD), goat polyclonal ROCK2 antibody (Santa Cruz Biochemicals; dilutions, 1:1000; molecular weight 160 kD) mouse monoclonal antirat phospho-ERK1/2 antibody (Santa Cruz Biochemicals; dilutions, 1:1000; molecular weight 42 or 44 kD). Then the membranes were washed three times in Tween-20 and incubated with the corresponding secondary antibody (Santa Cruz Biochemicals; dilutions, 1:10000) conjugated to horseradish peroxidase at room temperature. Immunoreactive bands were visualized with the SuperSignal West Pico enhanced chemoluminescence kit (Piece, Rockford, IL, USA) according to the manufacturer’s instructions. Band intensities were quantified by using a densitometer analysis system (Quantity One, Bio-Rad, Hercules, CA, USA).
Real-time Quantitative Reverse-Transcription Polymerase Chain Reaction for ROCK1
Total RNA was isolated from frozen rat left-ventricular tissue with Trizol reagent (Invitrogen, Carlsbad, CA, USA) (13). The concentration of total RNA was quantified by spectrophotometry (Beckman, Fullerton, CA, USA) and reverse transcribed with the use of a Moloney murine leukemia virus reverse transcriptase system (Fermentas, Sankt Leon-Rot, Germany) and oligo(dT). The sequences of the real-time polymerase chain reaction (PCR) primers were designed by using Primer Premier 5 (Premier Biosoft, Palo Alto, CA, USA) and synthesized by BioAsia (Shanghai, China). Real-time PCR was performed with an ABI PRISM 7500 sequence-detection system (Applied Biosystems, Foster City, CA, USA) by using an SYBR reverse transcription-PCR (RT-PCR) kit (Toyobo, Osaka, Japan). Expression level of ROCK1 was determined by threshold cycle number (Ct) and, by use of the ΔΔCt method, was normalized against the internal standard gene β-actin and compared relative to the control.
The primer sequences used were: ROCK1 (78 bp), forward: 5′-TTT CGG ATT CAA CTA GTG TTG C-3′, reverse: 5′-TGC AGG CAG AAC CAA CTG-3′; β-actin (254 bp), forward: 5′-AGA CCT TCA ACA CCC CAG-3′, reverse: 5′-CAC GAT TTC CCT CTC AGC-3′.
Statistics
Values were expressed as means ± SD. Statistical analysis of the results was carried out by one-way analysis of the variance followed by the Newman-Keuls test. Significance was defined at P < 0.05.
Results
Effect of IPC on Cardiomyocyte Apoptosis, Caspase-3 Cleavage and Infarct Size
TUNEL-positive cells are shown in Figure 2. TUNEL-positive cells were expressed as a percentage of normal nuclei. The percentage of TUNEL-positive cells was 33.87% ± 1.57% in the I/R group. The TUNEL-positive cells were significantly reduced to 17.29% ± 0.84% in the IPC group (P < 0.05 versus I/R group). Activation of Caspase-3 is a hallmark of apoptotic cell death, and Caspase-3 cleavage is indicative of its activation. As determined by Western blot analysis (Figure 3), IPC resulted in a 65% reduction in the amount of Caspase-3 cleavage (P < 0.05 versus I/R group). Caspase-3 activity attenuated in the IPC group. As shown in Figure 4, the infarct size of the heart was 60.53% ± 4.08% in I/R group. In IPC, the myocardial infarct size was 29.16% ± 1.08% (P < 0.05 versus I/R group). These values showed no significant differences between the IPC and IPC + DMSO groups.
Representative photomicrographs of ventricular tissue stained for TUNEL for DNA breaks. A, I/R group; B, IPC group; C, IPC + PD98059 group; D, IPC + fasudil group; E, IPC + PD98059 + fasudil group; F, IPC + DMSO group. In the I/R group we observed a large number of TUNEL-positive cells. The percentage of TUNEL-positive cells of the IPC group was significantly reduced compared with the I/R group (*P < 0.05). After administration of PD98059, the percentage of TUNEL-positive cells was significantly increased (#P < 0.05 versus IPC group). And in the IPC + PD98059 + fasudil group, TUNEL-positive cells were significantly reduced (**P < 0.05 versus the IPC + PD98059 group).
Western blot analysis of cleaved Caspase-3 in rat hearts of different groups (I/R, IPC, IPC + PD98059, IPC + fasudil, IPC + PD98059 + fasudil, IPC + DMSO). The amount of cleaved Caspase-3 attenuated in the IPC group (*P < 0.05 versus I/R). After administration of PD98059, the amount of cleaved Caspase-3 significantly increased (#P < 0.05 versus the IPC group). And in the IPC + PD98059 + fasudil group, the amount of cleaved Caspase-3 was significantly reduced (**P < 0.05 versus the IPC + PD98059 group).
Changes in myocardial infarct size of the different groups (I/R, IPC, IPC + PD98059, IPC + fasudil, IPC + PD98059 + fasudil, IPC + DMSO) in rat hearts. The myocardial infarct sizes were similar between the IPC and IPC + DMSO groups. A significant reduction in myocardial infarct size was observed in the IPC (*P < 0.05 versus the I/R group). After administration of PD98059, the myocardial infarct size was increased (#P < 0.05 versus IPC group). And in the IPC + PD98059 + fasudil group, the infarct size was reduced (**P < 0.05 versus the IPC + PD98059 group).
Effect of IPC on Activity of ERK1/2
Representative pictures of phospho-ERK1/2 expression in the myocardium of different groups of rats were shown in Figure 5. Phospho-ERK1/2 expression increased clearly in the heart in the IPC group. Western blot analysis for the phosphorylation of ERK1/2 also served to determine the activity of ERK1/2 in the IPC group. As shown in Figure 6, IPC resulted in an immediate increase in ERK1/2 phosphorylation. The increase in the phosphorylation of ERK1/2 was about 1.7-fold (P < 0.05 versus the I/R group).
Western blot analysis of phospho-MYPT-1, ROCK1 and phospho-ERK1/2 in rat hearts of different groups (I/R, IPC, IPC + PD98059, IPC + fasudil, IPC + PD98059 + fasudil, IPC + DMSO). The amount of phospho-ERK1/2 increased in the IPC group (*P < 0.05 versus I/R), whereas the amount of phospho-MYPT-1 and ROCK1 attenuated in the IPC group (*P < 0.05 versus I/R). After administration of PD98059, the amount of phospho-MYPT-1 and ROCK1 significantly increased (#P < 0.05 versus the IPC group). The molecular weight for phospho-MYPT1 (Millipore) was 80 kDa.
Effect of IPC on Activity of RhoA, ROCK1, ROCK2 and Rho-Kinase
RhoA protein was determined by immunoblotting of cytosolic and membrane fractions. In all groups, RhoA protein was detected in both cytosolic and membrane fractions. An enhanced RhoA translocation to the membrane was detected in the I/R rat model. But no difference was observed between the I/R and IPC groups (Figure 7A). ROCK1 and ROCK2 were also determined by Western blot analysis. As shown in Figure 7B, ROCK1 was increased in the I/R group and attenuated in the IPC group. ROCK2 increased in the I/R group, but there were no significant differences between the I/R and IPC groups. RT-PCR was also used to evaluate ROCK1 activity. As shown in Figure 8, a significant increase in mRNA expression of ROCK1 was detected in the I/R group, and the expression was decreased by IPC. We assessed Rho-kinase activity by examining phosphorylation of MYPT-1, a well-established Rho-kinase-specific substrate. As shown in Figure 6, IPC resulted in a 48% reduction in MYPT-1 phosphorylation and a 54% reduction in ROCK1 (P < 0.05 versus I/R group).
Western blot analysis of RhoA, ROCK1 and ROCK2 in rat hearts of different groups (sham, I/R, IPC, IPC + PD98059). (A) RhoA expression in the membrane fraction was significantly higher in the I/R group than in the sham group. But the amounts of RhoA in membrane fractions were similar between the I/R and IPC groups. (B) The amount of ROCK1 increased in the I/R group and attenuated in the IPC group. The amount of ROCK2 increased in the I/R group, but the amounts of ROCK2 were similar between the I/R and IPC groups.
Inhibition of ERK1/2 Increased Cardiomyocyte Apoptosis, Caspase-3 Activity and Infarct Size during IPC
As shown in Figure 2, the TUNEL-positive cells were significantly increased with administration of PD98059 (29.83% ± 0.7%) in the IPC + PD98059 group (P < 0.05 versus IPC group). As shown in Figure 3, after administration of PD98059, cleaved Caspase-3 significantly increased. The increase in the amount of cleaved Caspase-3 was about 2.1-fold (P < 0.05 versus IPC group). As shown in Figure 4, administration of PD98059 caused a significant increase of myocardial infarct size. The infarct size of the heart was 44.88% ± 0.7% in the IPC + PD98059 group (P < 0.05 versus IPC group).
ERK1/2 Opposed Rho-Kinase during IPC
As shown in Figures 6 and 9, ERK1/2 was strongly activated and Rho-kinase activity decreased in IPC. Inhibition of ERK1/2 in IPC could lead to upregulation of MYPT-1 phosphorylation and the amount of ROCK1. Inhibition of ERK1/2 in IPC also could lead to upregulation of ROCK1 mRNA (Figure 8). In the IPC + fasudil group, phospho-ERK1/2 expression was similar to that in the IPC group. In the IPC + PD98059 group, phospho-ERK1/2 expression significantly decreased. And phospho-ERK1/2 expression was not recovered in the IPC + PD98059 + fasudil group.
Western blot analysis of MYPT-1 phosphorylation in rat hearts of different groups (sham, I/R, IPC, IPC + PD98059, IPC + fasudil, IPC + PD98059 + fasudil, IPC + DMSO). **P < 0.05 versus sham; *P < 0.05 versus I/R group; #P < 0.05 versus IPC group. The molecular weight for p-MYPT1 (bioWORLD) is 130 kDa.
Inhibition of Rho-Kinase Rescued the Effect of Inhibition of ERK1/2 on Apoptosis
To test the hypothesis that ERK1/2 acts to inhibit Rho-kinase in IPC, we examined whether the effect of inhibition of ERK1/2 could be rescued by inhibition of Rho-kinase. As shown in Figure 2, fasudil treatment reversed cell apoptosis caused by treatment with PD98059 in IPC. The number of TUNEL-positive cells was 23.3% ± 0.67% in the IPC + PD98059 + fasudil group. The amount of cleaved Caspase-3 was also significantly reduced in the IPC + PD98059 + fasudil group (Figure 3). Fasudil resulted in a 22% reduction in cardiomyocyte apoptosis and a 30% reduction in cleaved Caspase-3 in the IPC + PD98059 + fasudil group (P < 0.05 versus the IPC + PD98059 group). In addition, as shown in Figure 4, the infarct size of the heart was 39.44% ± 0.92% in the IPC + PD98059 + fasudil group. The combination of PD98059 and fasudil also resulted in a 12% reduction in myocardial infarct size (P < 0.05 versus the IPC + PD98059 group).
Discussion
The results of this study provided the experimental evidence that ERK-MAPK signaling opposed Rho-kinase to decrease cardiomyocyte apoptosis in IPC. We report for the first time that IPC induces the reduction of Rho-kinase activity via the activation of ERK-MAPK signaling in vivo.
Recent studies have shown that Rho-kinase is involved in the clearance of apoptotic cells through regulation of the actin cytoskeleton (14,15). Rho-kinase is recognized as a major regulator of the morphological events that occur during the execution phase of apoptosis, including cell contraction, dynamic membrane blebbing, nuclear disintegration and fragmentation of apoptotic cells into apoptotic bodies. Previous studies have demonstrated that I/R upregulates expression of RhoA in ischemic myocardium and subsequently increases Rho-kinase activity (4). The Rho-kinase inhibitor significantly inhibits the activation of Rho-kinase after I/R and reduces infarct size and the amount of cell apoptosis (5). In this study we found that both RhoA translocation and Rho-kinase activity increased in the myocardium following I/R, but only the activation of Rho-kinase was reversed in IPC. In the present study, we assessed the activity of Rho-kinase by examining phosphorylation of MYPT-1. IPC resulted in a 48.3% decrease in the amount of phospho-MYPT-1, indicating that the activation of Rho-kinase was reduced in the myocardium following IPC. We demonstrated that IPC produced an attenuation of myocardial infarction and cardiomyocyte apoptosis. In this study we also used the TUNEL assay to examine apoptotic myocardial cells. The percentage of TUNEL-positive cardiomyocytes after 30-min ischemia and 180-min reperfusion was 33.87% ± 1.57%; these data are similar to the data reported previously for rat hearts subjected to I/R (5,16). IPC resulted in a 49% reduction in apoptotic cardiomyocytes. In addition, Caspase-3 activation also attenuated in IPC group. These results suggest that Rho-kinase activity and cardiomyocyte apoptosis are reduced by IPC.
We attempted to elucidate the mechanism of the reduction of Rho-kinase activity in IPC. Rho-kinase activity can be regulated by several distinct mechanisms, such as the Rho/Rho-kinase pathway (17) and the Caspase-3/Rho-kinase pathway (18). Other negative regulators have been found bind to and inhibit Rho-kinase activity. Recent evidence indicates that there is selective cross-talk between Ras and Rho signaling pathways (19–21). Ras is a small GTP-binding protein that functions as a molecular switch and as a link between membrane tyrosine-kinase receptors and the downstream signal-transduction machinery. Ras-Raf-MEK-ERK1/2 is the prototypic MAP kinase cascade. Results of previous studies have shown that inhibition of ERK-MAPK signaling in cancer cells can lead to upregulation of Rho-kinase activity (22). ERK-MAPK signaling was found to oppose Rho-kinase to promote endothelial cell survival (23). We focused on investigating the role of ERK-MAPK in Rho-kinase activity in IPC.
The ERK-MAPK was first described in 1990 as a serine/threonine protein kinase that was tyrosine phosphorylated by various extracellular signals including insulin and nerve growth factor (24). ERK1/2, a prototypic member of the MAPK family, is the best candidate among the protein kinases that determine the specificity of cellular responses—including cell proliferation, cell differentiation and cell survival—and are activated by a large variety of extracellular agents (25). In cultured cardiomyocytes, peptide growth factors and other MAPK-inducing agents provide protective effects against serum starvation, hypoxia and reoxygenation-induced injuries. Inhibition of MEK or ERK activity with pharmacological reagents diminishes these protective effects (26,27). In vivo, MEK transgenic hearts are protected from I/R injury and cardiomyocyte apoptosis (28). In contrast, inhibition of Raf-1 by the expression of a dominant-negative mutant or cardiac-specific knockout promotes cardiomyocyte apoptosis and decompensated heart failure (29,30). Yue et al. have demonstrated that inhibition of ERK enhances ischemia/reoxygenation-induced apoptosis and exaggerates reperfusion injury (31). But the role of ERK1/2 as a potential mediator of protection in the setting of IPC has been controversial, with the majority of studies supporting its role in IPC (32), because several studies have failed to demonstrate a role for ERK1/2 in IPC (33). By use of immunohistochemical analysis and Western blot, we demonstrated that ERK-MAPK was strongly activated in IPC. Cardiomyocyte apoptosis was also significantly reduced in IPC. Inhibition of ERK-MAPK in IPC led to increased Rho-kinase activity and cardiomyocyte apoptosis. ERK1/2 activation has not been examined directly in this setting; its activation would be expected to reduce cell death through several different antiapoptotic mechanisms (34). We investigated the effect of ERK1/2 on cardiomyocyte apoptosis and myocardial infarct size following Rho-kinase activation. The effects of inhibition of ERK-MAPK could be rescued by inhibition of Rho-kinase in vivo. Inhibition of Rho-kinase reversed cardiomyocyte apoptosis and the size of infarcts caused by inhibition of ERK-MAPK in IPC. The combination of PD98059 and fasudil restored protection, as reflected by decreased cardiomyocyte apoptosis (22%) and infarct size (12%) (P < 0.05 versus the IPC + PD98059 group). The infarct size did not decrease as significantly as cardiomyocyte apoptosis. These data show that cardioprotection of Rho-kinase inhibition is mediated by antiapoptosis more than decreased infarct size after inhibition of ERK-MAPK. These results indicate that ERK-MAPK signaling is required in IPC to oppose the effect of Rho-kinase signaling on cell apoptosis.
Previous studies have demonstrated that sustained ERK-MAPK signaling might downregulate ROCK1 (19). In this study, we also examined ROCK1 and ROCK2 with Western blot analysis. We showed that ROCK1 and ROCK2 both increased in I/R, but only ROCK1 expression was downregulated in IPC. Inhibition of ERK-MAPK in IPC also leads to increased ROCK1 expression. Thus, ROCK1 may be the major Rho-kinase that is opposed by ERK-MAPK signaling in IPC.
In our study, inhibition of ERK1/2 and Rho-kinase partly reduced cell apoptosis, and ERK1/2 expression was not recovered. ERK-MAPK signaling leads to downregulation of Rho-kinase, but not RhoA, activity (19). I/R upregulated expression of RhoA in ischemic myocardium and subsequently increased Rho-kinase activity (4).
Overpression of RhoA in I/R might not be changed by preconditioning. Because RhoA is the main upstream activator of Rho-kinase, ERK-MAPK signaling partly decreased Rho-kinase activity. Thus cell apoptosis was reduced when fasudil was used in the IPC + PD98059 group. These data show that in IPC, Rho-kinase inhibition is mediated, at least in part, via ERK-MAPK signaling. Next we will study the cross-talk between ERK-MAPK signaling and thoroughly investigate Rho/Rho-kinase signaling in I/R and IPC.
In summary, we have demonstrated that Rho-kinase activity and cardiomyocyte apoptosis were reduced in IPC in vivo. Our results also indicated that ERK-MAPK activity increased in IPC, and inhibition of ERK-MAPK led to increased Rho-kinase activity and cardiomyocyte apoptosis. These results establish the relationship between ERK-MAPK and Rho-kinase, demonstrating that ERK-MAPK signaling is required in IPC to oppose the effect of Rho-kinase signaling on cell apoptosis in vivo. The elucidation of this process may lead to new treatment possibilities for patients suffering coronary heart diseases.
Disclosure
The authors declare that they have no competing interests as defined by Molecular Medicine, or other interests that might be perceived to influence the results and discussion reported in this paper.
References
Amano M, et al. (1997) Formation of actin stress fibers and focal adhesions enhanced by Rho-kinase. Science. 275:1308–11.
Yasui Y, et al. (1998) Roles of Rho-associated kinase in cytokinesis; mutations in Rho-associated kinase phosphorylation sites impair cytokinetic segregation of glial filaments. J. Cell Biol. 143:1249–58.
Loirand G, Guerin P, Pacaud P. (2006) Rho kinases in cardiovascular physiology and pathophysiology. Circ. Res. 98:322–34.
Bao W, et al. (2004) Inhibition of Rho-kinase protects the heart against ischemia/reperfusion injury. Cardiovasc. Res. 61:548–58.
Zhang J, et al. (2009) Inhibition of the activity of Rho-kinase reduces cardiomyocyte apoptosis in heart ischemia/reperfusion via suppressing JNK-mediated AIF translocation. Clin. Chim. Acta. 401:76–80.
Murry CE, Jennings RB, Reimer KA. (1986) Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium. Circulation. 74:1124–36.
An J, Varadarajan SG, Novalija E, Stowe DF. (2001) Ischemic and anesthetic preconditioning reduces cytosolic [Ca2+] and improves Ca(2+) responses in intact hearts. Am. J. Physiol. Heart Circ. Physiol. 281: H1508–23.
Sanada S, et al. (2004) Protein kinase A as another mediator of ischemic preconditioning independent of protein kinase C. Circulation. 110:51–7.
Alessi DR, Cuenda A, Cohen P, Dudley DT, Saltiel AR. (1995) PD 098059 is a specific inhibitor of the activation of mitogen-activated protein kinase kinase in vitro and in vivo. J. Biol. Chem. 270:27489–94.
Demiryurek S, et al. (2005) Effects of fasudil, a Rho-kinase inhibitor, on myocardial preconditioning in anesthetized rats. Eur. J. Pharmacol. 527:129–40.
Ji ES, Yue H, Wu YM, He RR. (2004) Effects of phytoestrogen genistein on myocardial ischemia/reperfusion injury and apoptosis in rabbits. Acta Pharmacol. Sin. 25:306–12.
Mohanty I, Arya DS, Gupta SK. (2006) Effect of Curcuma longa and Ocimum sanctum on myocardial apoptosis in experimentally induced myocardial ischemic-reperfusion injury. BMC Complement. Altern. Med. 6:3.
Chomczynski P. (1993) A reagent for the singlestep simultaneous isolation of RNA, DNA and proteins from cell and tissue samples. Biotechniques. 15:532–4, 536–7.
Erwig LP, et al. (2006) Differential regulation of phagosome maturation in macrophages and dendritic cells mediated by Rho GTPases and ezrinradixin-moesin (ERM) proteins. Proc. Natl. Acad. Sci. U. S. A. 103:12825–30.
Tosello-Trampont AC, Nakada-Tsukui K, Ravichandran KS. (2003) Engulfment of apoptotic cells is negatively regulated by Rho-mediated signaling. J. Biol. Chem. 278:49911–19.
Song ZF, et al. (2008) Inhibition of the activity of poly (ADP-ribose) polymerase reduces heart ischaemia/reperfusion injury via suppressing JNK-mediated AIF translocation. J. Cell Mol. Med. 12:1220–8.
Matsui T, et al. (1996) Rho-associated kinase, a novel serine/threonine kinase, as a putative target for small GTP binding protein Rho. EMBO J. 15:2208–16.
Coleman ML, et al. (2001) Membrane blebbing during apoptosis results from caspase-mediated activation of ROCK I. Nat. Cell Biol. 3:339–45.
Sahai E, Olson MF, Marshall CJ. (2001) Cross-talk between Ras and Rho signalling pathways in transformation favours proliferation and increased motility. EMBO J. 20:755–66.
Piazzolla D, Meissl K, Kucerova L, Rubiolo C, Baccarini M. (2005) Raf-1 sets the threshold of Fas sensitivity by modulating Rok-alpha signaling. J. Cell Biol. 171:1013–22.
Manapov F, Muller P, Rychly J. (2005) Translocation of p21(Cip1/WAF1) from the nucleus to the cytoplasm correlates with pancreatic myofibroblast to fibroblast cell conversion. Gut. 54:814–22.
Vial E, Sahai E, Marshall CJ. (2003) ERK-MAPK signaling coordinately regulates activity of Rac1 and RhoA for tumor cell motility. Cancer Cell. 4:67–79.
Mavria G, et al. (2006) ERK-MAPK signaling opposes Rho-kinase to promote endothelial cell survival and sprouting during angiogenesis. Cancer Cell. 9:33–44.
Boulton TG, et al. (1990) An insulin-stimulated protein kinase similar to yeast kinases involved in cell cycle control. Science. 249:64–7.
Torii S, Nakayama K, Yamamoto T, Nishida E. (2004) Regulatory mechanisms and function of ERK MAP kinases. J. Biochem. 136:557–61.
Sugden PH, Clerk A. (2006) Oxidative stress and growth-regulating intracellular signaling pathways in cardiac myocytes. Antioxid. Redox. Signal. 8:2111–24.
Bueno OF, Molkentin JD. (2002) Involvement of extracellular signal-regulated kinases 1/2 in cardiac hypertrophy and cell death. Circ. Res. 91:776–81.
Lips DJ, et al. (2004) MEK1-ERK2 signaling pathway protects myocardium from ischemic injury in vivo. Circulation. 109:1938–41.
Harris IS, et al. (2004) Raf-1 kinase is required for cardiac hypertrophy and cardiomyocyte survival in response to pressure overload. Circulation. 110:718–23.
Yamaguchi O, et al. (2004) Cardiac-specific disruption of the c-raf-1 gene induces cardiac dysfunction and apoptosis. J. Clin. Invest. 114:937–43.
Yue TL, et al. (2000) Inhibition of extracellular signal-regulated kinase enhances ischemia/reoxygenation-induced apoptosis in cultured cardiac myocytes and exaggerates reperfusion injury in isolated perfused heart. Circ. Res. 86:692–9.
Hausenloy DJ, Tsang A, Mocanu MM, Yellon DM. (2005) Ischemic preconditioning protects by activating prosurvival kinases at reperfusion. Am. J. Physiol. Heart Circ. Physiol. 288:H971–6.
Mocanu MM, Bell RM, Yellon DM. (2002) PI3 kinase and not p42/p44 appears to be implicated in the protection conferred by ischemic preconditioning. J. Mol. Cell. Cardiol. 34:661–8.
Hausenloy DJ, Yellon DM. (2004) New directions for protecting the heart against ischaemiareperfusion injury: targeting the Reperfusion Injury Salvage Kinase (RISK)-pathway. Cardiovasc. Res. 61:448–60.
Acknowledgments
This work was supported by the National High-tech Research and Development Program of China Grant 2006AA02A406. We thank R. Wang, J-B Feng, C-X Liu, X-P Wang and H Jiang for their excellent technical help.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Juan-Zhang, Bian, HJ., Li, XX. et al. ERK-MAPK Signaling Opposes Rho-Kinase to Reduce Cardiomyocyte Apoptosis in Heart Ischemic Preconditioning. Mol Med 16, 307–315 (2010). https://doi.org/10.2119/molmed.2009.00121
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.2119/molmed.2009.00121