Abstract
Background and Objective
According to the Barcelona Clinic Liver Cancer (BCLC) algorithm, tumor burden and liver function, but not tumor biology, are the key factors in determining tumor staging and treatment modality, and evaluating treatment prognosis. The serum α‐fetoprotein (AFP) level is an important characteristic of hepatocellular carcinoma (HCC) biology, and we aimed to evaluate its prognostic value for patients undergoing liver resection of early-stage HCC.
Methods
Patients who underwent curative liver resection for early-stage HCC were identified from a multi‐institutional database. Patients were divided into three groups according to preoperative AFP levels: low (< 400 ng/mL), high (400–999 ng/mL), and extremely-high (≥ 1000 ng/mL) AFP groups. Overall survival (OS) and recurrence rates were compared among these three groups.
Results
Among 1284 patients, 720 (56.1%), 262 (20.4%), and 302 (23.5%) patients had preoperative low, high, and extremely-high AFP levels, respectively. The cumulative 5-year OS and recurrence rates were 71.3 and 38.9% among patients in the low AFP group, 66.3 and 48.5% in the high AFP group, and 45.7 and 67.2% in the extremely-high AFP group, respectively (both p < 0.001). Multivariate Cox regression analysis identified both high and extremely-high AFP levels to be independent risk factors of OS (hazard ratio [HR] 1.275 and 1.978, 95% confidence interval [CI] 1.004–1.620 and 1.588–2.464, respectively; p = 0.047 and p < 0.001, respectively) and recurrence (HR 1.290 and 2.050, 95% CI 1.047–1.588 and 1.692–2.484, respectively; p = 0.017 and p < 0.001, respectively).
Conclusions
This study demonstrated the important prognostic value of preoperative AFP levels among patients undergoing resection for early-stage HCC. Incorporating AFP to prognostic estimation of the BCLC algorithm can help guide individualized risk stratification and identify neoadjuvant/adjuvant treatment necessity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hepatocellular carcinoma (HCC) is a major global health concern, representing the sixth most common cancer and the third leading cause of cancer-related deaths worldwide.1 It is prevalent in Southeast Asia and Africa, and particularly in China.2,3,4 Early detection and appropriate treatment modalities are crucial for improving survival prognosis in HCC patients.5,6 The Barcelona Clinic Liver Cancer (BCLC) algorithm is a widely accepted staging system that guides treatment decisions for HCC.7 It was developed based on a comprehensive analysis of several prognostic variables, including tumor burden, liver function, and patient performance status. The BCLC system classifies HCC patients into five stages (0, A, B, C, and D) and recommends specific treatment strategies for each stage. For patients with early-stage HCC (BCLC stage 0/A), surgical resection, liver transplantation, and local ablation therapies are the main curative treatment options.7,8,9 Despite its widespread use and clinical utility, the BCLC algorithm has some potential limitations. One drawback is the lack of consideration for tumor biology, which can significantly impact patient long-term prognosis.7 Tumor biology refers to the unique molecular and cellular characteristics of a tumor, including its growth rate, invasiveness, and potential to metastasize. These factors can vary significantly between individual tumors and may influence treatment response and long-term prognosis. Therefore, incorporating tumor biology into the HCC staging system could enhance its predictive accuracy and help guide individualized risk stratification and identify treatment decisions, including necessary neoadjuvant/adjuvant therapy for patients undergoing curative treatment but at high risk of recurrence.
α-Fetoprotein (AFP) is a glycoprotein that is produced in high amounts during fetal development.10,11 It is thought to be involved in cell proliferation, angiogenesis, and immune evasion of HCC, and has been observed to be elevated in HCC.12,13,14 As a result, AFP has been widely studied as a potential biomarker for HCC diagnosis, prognosis, and treatment response monitoring.15 Several studies have demonstrated that high preoperative AFP levels are associated with worse clinicopathologic features, increased tumor recurrence, and shorter long-term survival after curative treatments.16,17,18,19,20,21,22,23,24,25,26,27,28 However, most of these studies were carried out at a single center, had a limited sample size, performed only univariate survival analyses, or included a heterogeneous mix of early-, intermediate-, and advanced-stage HCC patients.16,17,18,19,20,21,22,23,24,25,26,27,28 Thus far, there has been limited evidence on the prognostic role of AFP, specifically among patients with early-stage HCC (BCLC stage 0/A), who are the most suitable candidates for curative liver resection.
We hypothesized that high preoperative serum AFP levels would be independently associated with poorer survival and increased recurrence rates after curative liver resection for early-stage HCC (BCLC stage 0/A). To achieve these objectives, we conducted a retrospective analysis of a large-scale, multicenter database, and stratified patients into different groups based on their preoperative serum AFP levels, and compared their cumulative survival and recurrence rates. The results of this study could have significant implications for surgical decision making and prognostic evaluation, and lead to better clinical outcomes for patients with early-stage HCC.
Methods
Study Design and Patient Population
This study was a multicenter, retrospective cohort analysis designed to evaluate the prognostic value of preoperative serum AFP levels in patients undergoing liver resection for early-stage HCC (BCLC stage 0/A). Patients who underwent curative open liver resection for BCLC stage 0/A HCC between January 2010 and December 2019 were identified from a multicenter database that included data from 10 participating hospitals in China (General Surgery Center, First Hospital of Jilin University, Changchun, Jilin, China; Eastern Hepatobiliary Surgery Hospital, Second Military Medical University [Navy Medical University], Shanghai, China; Ziyang First People’s Hospital, Ziyang, Sichuan, China; Mengchao Hepatobiliary Hospital, Fujian Medical University, Fujian, China; Affiliated Hospital of Nantong University, Nantong, Jiangsu, China; First Affiliated Hospital of Shandong First Medical University and Shandong Provincial Qianfoshan Hospital, Jinan, Shandong, China; Pu’er People’s Hospital, Pu’er, Yunnan, China; Fuyang People’s Hospital, Fuyang, Anhui, China; Pingxiang Mining Group General Hospital, Jiangxi, China; First Affiliated Hospital of Harbin Medical University, Harbin, Heilongjiang, China). The study was performed in accordance with the Declaration of Helsinki and the Ethical Guidelines for Clinical Studies for the enrolled centers. Due to the retrospective nature of this study, informed consent was waived by the Institutional Review Board of the First Hospital of Jilin University (No. 2022-553). Consent for the relevant procedures and the use of data for research purposes was obtained from all patients prior to treatment.
Inclusion and Exclusion Criteria
Patients were included in the study if they met the following criteria: (1) pathologically confirmed diagnosis of HCC; (2) BCLC stage 0/A HCC; (3) underwent curative liver resection with negative surgical margins (R0 resection); and (4) had available preoperative serum AFP levels that were measured within 2 weeks before surgery. Patients were excluded from the study if they had any of the following: (1) under 18 years of age; (2) had recurrent HCC; (3) had combined HCC-cholangiocarcinoma; (4) received any preoperative treatment for HCC, such as portal vein embolization, transarterial chemoembolization (TACE), local ablation, or systemic therapy; (5) postoperative early death within 90 days after surgery; (6) lost to follow-up within 6 months after surgery; or (7) missing data on important prognostic variables.
Data Collection
Potential risk factors that were related to long-term survival and recurrence after liver resection of HCC were classified relative to the patient, tumor, and operation. Patient-related factors included sex, age, American Society of Anesthesiologists (ASA) score, a positive hepatitis B virus (HBV) and hepatitis C virus (HCV) status, presence of liver cirrhosis or portal hypertension, and Child–Pugh grade. Tumor-related factors included preoperative serum AFP levels, tumor size, tumor number, satellite nodules, microscopic vascular invasion (MVI), tumor encapsulation, and tumor differentiation, while operation-related factors included intraoperative blood transfusion, intraoperative blood loss, extent of hepatectomy (minor or major), type of resection (anatomical or non-anatomical), and width of the resection margin (narrow [< 1.0 cm] or wide [≥ 1.0 cm]). Cirrhosis was diagnosed on histopathological examination. Portal hypertension was defined as the presence of splenomegaly with esophageal varicosities; tumor differentiation was defined according to the Modified Edmondson Criteria;29 minor hepatectomy was defined as the removal of fewer than three Couinaud segments; major hepatectomy was defined as the removal of three or more segments;30 and anatomical resection was defined by the Brisbane 2000 system, whereas non-anatomical resection included limited or wedge resections.30
Preoperative serum AFP levels were categorized into three groups based on previously established cut-off values: low (< 400 ng/mL), high (400–999 ng/mL), and extremely-high (≥ 1000 ng/mL). These cut-off values were chosen based on their clinical relevance and their association with oncological prognosis after liver resection or liver transplantation for HCC in previous studies.21,22,24,25,26,31
Follow-Up
Patients were regularly followed-up at each participating hospital following a relatively unified postoperative surveillance strategy for postoperative recurrence. Each participating hospital had established its own prospectively collected database for collecting information and conducting patient follow-up and re-evaluation. The follow-up algorithm consisted of clinical examination, laboratory tests, and imaging studies (such as contrast-enhanced computed tomography [CT] or magnetic resonance imaging [MRI]) to monitor for disease recurrence at 2-monthly intervals for the first 6 months, 3-monthly intervals for the next 1½ years, and then once every 6 months thereafter. Enhanced CT or MRI, hepatic angiography, bone scan, or positron emission tomography were performed when recurrence or distant metastasis was suspected. Tumor recurrence was defined as a new appearance of intra- or extrahepatic tumor nodule(s) with radiological characteristics as for diagnosis of the primary tumor, with or without a rise in the serum AFP level. Appropriate treatment for recurrence was carried out using repeat liver resection, liver transplantation, local ablation, TACE, radiotherapy, systemic therapy, or palliative care.
Outcome Endpoints
The outcome endpoints of this study were overall survival (OS) and recurrence. OS was defined as the time from the date of surgery to the date of death from any cause or the last follow-up, while time to recurrence was defined as the time from the date of surgery to the date of first documented tumor recurrence or the last follow-up without recurrence. Patients who were lost to follow-up or died without recurrence were censored at the date of their last follow-up.
Statistical Analysis
Continuous variables were presented as mean ± standard deviation (SD) or median with interquartile range (IQR), depending on their distribution, whereas categorical variables were presented as frequencies and percentages. The baseline characteristics of the three AFP groups (low, high, and extremely high) were compared using the analysis of variance (ANOVA) test for continuous variables and the Chi-square or Fisher's exact tests for categorical variables, as appropriate. Cumulative OS and recurrence analyses were performed using the Kaplan–Meier method, and the log-rank test was used to compare OS and recurrence curves among the three AFP groups. Variables with a p value < 0.10 in the univariate analysis were included in the multivariate Cox proportional hazards regression models to determine the independent risk factors for OS and recurrence. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated for each variable in the models. The proportional hazards assumption was tested using Schoenfeld residuals, and no significant violations were detected. Subgroup analyses were performed to assess the prognostic value of serum AFP levels in different patient subgroups. Interaction tests were conducted to determine whether the effect of preoperative serum AFP levels on OS and recurrence differed significantly among the subgroups. All statistical analyses were performed using SPSS statistical software (version 26.0; IBM Corporation, Armonk, NY, USA). Two-sided p-values < 0.05 were considered statistically significant.
Results
Patient Characteristics
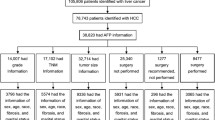
A total of 1284 patients who underwent curative liver resection for early-stage HCC (BCLC stage 0/A) between January 2010 and December 2019 were included in the analytic cohort (electronic supplementary material [ESM] eFig. 1); 1128 (87.9%) patients were male and 156 (12.1%) were female, with a median age of 52 years. HBV positivity was observed in 82.6% of patients, while HCV positivity was found in 8.7% of patients. Liver cirrhosis and portal hypertension were present in 76.7 and 23.0% of patients, respectively. The median tumor size was 4.0 cm (IQR 2.7–6.0 cm) and the majority of patients had a single tumor (95.5%). Most patients had a preoperative low AFP level (< 400 ng/mL; n = 720, 56.1%), while 262 (20.4%) and 302 (23.5%) patients were included in the high AFP (400–999 ng/mL) and extremely-high AFP (≥ 1000 ng/mL) groups, respectively.
The clinical characteristics and operative variables of the patients stratified by preoperative serum AFP levels are shown in Table 1. Significant differences were observed among the three AFP groups in terms of age, tumor size, tumor number, presence of MVI, presence of satellite nodules, presence of incomplete tumor encapsulation, intraoperative blood loss, presence of intraoperative blood transfusion, extent of hepatectomy, and resection margin (all p < 0.05). Patients with higher AFP levels were more likely to be female, have larger and multiple tumors, MVI, satellite nodules, incomplete tumor encapsulation, more intraoperative blood loss, intraoperative blood transfusion, major hepatectomy, and a narrow resection margin.
Long-Term Outcomes
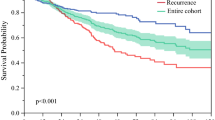
With a median follow-up of 52.3 months (IQR 33.7–66.2), 660/1284 (51.4%) patients developed recurrence and 543 (42.3%) patients died. In the entire cohort, the cumulative 1-, 3-, and 5-year OS rates were 91.4, 76.6, and 66.9%, respectively, while the cumulative 1-, 3-, and 5-year recurrence rates were 23.8, 40.5, and 47.5%, respectively (ESM eFig. 2).
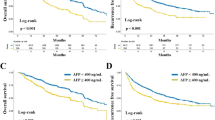
The long-term outcomes of patients stratified by preoperative serum AFP levels are shown in Table 2. The cumulative 1-, 3-, and 5-year OS rates of the low, high, and extremely-high AFP groups were 94.6, 83.7, and 71.3%; 90.1, 73.5, and 66.3%; and 85.0, 61.2, and 45.7%, respectively (among the three groups, p < 0.001) (Fig. 1). The 1-, 3-, and 5-year recurrence rates of the low, high, and extremely-high AFP groups were 18.7, 31.9, and 38.9; 27.1, 40.5%, and 48.5; and 33.1, 61.3, and 67.2%, respectively (among the three groups, p < 0.001) (Fig. 2).
Subgroup Analyses
To further explore the prognostic value of preoperative serum AFP levels in different patient subgroups, we performed subgroup analyses stratified by various clinical characteristics. The results of univariate analysis stratified by preoperative serum AFP levels among these subgroup analyses are presented in Fig. 3 (for OS and recurrence). In general, the prognostic value of serum AFP levels was consistent across the different subgroups, with high and extremely-high AFP levels being associated with poorer OS and increased recurrence in most of the subgroups. Interaction tests revealed no significant interactions between serum AFP levels and the examined subgroups, suggesting that the effect of serum AFP levels on OS and recurrence did not differ significantly among the subgroups.
Univariate and Multivariate Analyses for Risk Factors of Overall Survival and Recurrence
The results of the univariate and multivariate Cox proportional hazards regression analyses for OS and recurrence are shown in Tables 3 and 4, respectively. In the univariate analysis, factors significantly associated with poorer OS included high AFP levels (HR 1.370, 95% CI 1.100–1.708; p = 0.005), extremely-high AFP levels (HR 2.192, 95% CI 1.804–2.663; p < 0.001), liver cirrhosis, Child–Pugh grade B, tumor size > 5.0 cm, multiple tumors, MVI, satellite nodules, incomplete tumor encapsulation, poorly differentiated tumors, intraoperative blood loss > 400 mL, intraoperative blood transfusion, major hepatectomy, and narrow resection margin (all p < 0.05). In the multivariate analysis, both high (HR 1.275, 95% CI 1.004–1.620; p = 0.047) and extremely-high (HR 1.978, 95% CI 1.588–2.464; p < 0.001) AFP levels remained independent risk factors for poorer OS, after adjusting for other significant variables. Other independent prognostic factors for OS included liver cirrhosis, tumor size > 5.0 cm, MVI, incomplete tumor encapsulation, intraoperative blood transfusion, and narrow resection margin (all p < 0.05).
The univariate analysis for risk factors of recurrence revealed that high AFP levels (HR 1.369, 95% CI 1.121–1.671; p = 0.002), extremely-high AFP levels (HR 1.472, 95% CI 1.347–1.609; p < 0.001), age > 60 years, positive HBV, liver cirrhosis, portal hypertension, Child–Pugh grade B, tumor size > 5.0 cm, multiple tumors, MVI, satellite nodules, incomplete tumor encapsulation, poorly differentiated tumors, intraoperative blood loss > 400 mL, intraoperative blood transfusion, major hepatectomy, non-anatomical resection, and narrow resection margin were significantly associated with poorer RFS (all p < 0.05). In the multivariate analysis, both high (HR 1.290, 95% CI 1.047–1.588; p = 0.017) and extremely-high (HR 2.050, 95% CI 1.692–2.484; p < 0.001) AFP levels were identified as independent risk factors for increased recurrence, after adjusting for other significant variables. Other independent prognostic factors for recurrence included liver cirrhosis, tumor size > 5.0 cm, multiple tumors, MVI, incomplete tumor encapsulation, intraoperative blood transfusion, and narrow resection margin (all p < 0.05).
Discussion
The BCLC algorithm, which is widely used for staging and guiding treatment decisions in HCC, primarily focuses on tumor burden, liver function, and patient performance status. However, it does not consider the unique characteristics of tumor biology, which can significantly impact treatment response and long-term outcomes. Incorporating tumor biology into the staging system is crucial for accurate risk stratification and treatment selection, especially for early-stage HCC patients who are potential candidates for curative treatments such as liver resection. In this large, multicenter, observational study, the prognostic value of AFP levels in patients undergoing liver resection for early-stage HCC has been in-deep investigated. Our findings demonstrate that preoperative high (400–999 ng/mL) and extremely-high (≥ 1000 ng/mL) AFP levels are independent risk factors for poorer OS and increased recurrence rates after curative liver resection for early-stage HCC. This suggests that preoperative serum AFP levels could serve as a valuable prognostic marker for patients with early-stage HCC undergoing liver resection. In the subgroup analyses, we found that the prognostic value of preoperative serum AFP levels was consistent across various patient subgroups, indicating that the association between AFP levels and patient outcomes is robust and is not influenced by other clinical characteristics. Therefore, preoperative serum AFP levels could potentially be used as a stratification factor in future clinical trials or in the development of individualized treatment strategies for patients with early-stage HCC.
As depicted in Table 1, patients with higher preoperative AFP levels were more likely to have larger tumor size, multiple tumors, MVI, satellite nodules, incomplete tumor encapsulation, and other adverse clinicopathologic features. These findings suggest that elevated AFP levels are associated with aggressive tumor biology and increased tumor invasiveness. Our results are consistent with previous studies that have shown an association between high AFP levels and poor clinicopathologic features in HCC patients. Importantly, our study demonstrates that high and extremely-high AFP levels are independent prognostic factors for both OS and recurrence after curative liver resection. Patients with extremely-high AFP levels (≥ 1000 ng/mL) had significantly lower 5-year OS rates (45.7%) and higher recurrence rates (67.2%) compared with those with low AFP levels (< 400 ng/mL) [both p < 0.001]. These findings highlight the importance of considering preoperative AFP levels as an additional criterion for risk stratification and treatment decision making in early-stage HCC patients.
In the context of our study, the incorporation of AFP levels into the BCLC staging system could enhance its predictive accuracy and help guide individualized risk stratification and treatment decisions, including the selection of neoadjuvant/adjuvant therapies for patients at high risk of recurrence. AFP levels could serve as a complementary biomarker to assess tumor biology and predict treatment response, allowing for more personalized treatment approaches. This integration of biomarkers into the clinical decision-making process holds promise for improving patient outcomes and optimizing treatment strategies in early-stage HCC. Furthermore, our study emphasizes the importance of conducting further research to explore the underlying molecular mechanisms linking elevated AFP levels to aggressive tumor behavior and poor prognosis in HCC. Understanding the biological pathways involved in AFP-mediated tumor growth, angiogenesis, and immune evasion could lead to the development of novel therapeutic targets and strategies for HCC management. Additionally, investigating the potential interactions between AFP and other molecular markers, such as genetic mutations or gene expression profiles, may provide deeper insights into the complex biology of HCC and help identify novel therapeutic targets.
As some previous studies mentioned, an AFP cut-off of 200 ng/mL is a significant threshold to predict tumor recurrence or survival after hepatic resection or liver transplantation of HCC.21,24,25,32 In fact, we have performed an additional prognostic analysis between patients with preoperative AFP < 200 ng/mL and patients with preoperative AFP of 200–400 ng/mL (ESM eFig. 3). Unfortunately, no significant differences in OS and recurrence were found between these two groups. Meanwhile, significant differences were found in the present study when the AFP cut-off values were used by two other more commonly used cut-off values, i.e., 400 and 1000 ng/mL.22,26,31,33,34,35
The decision to categorize patients into these three groups was driven by a desire to capture the diverse range of AFP levels found in HCC patients and to understand how these levels might differentially impact prognoses. This granularity was crucial, as it revealed a clear dose–response relationship: as AFP levels increased, survival times decreased and recurrence rates increased. This approach, although uncommon in the current literature, was both statistically sound and clinically relevant. It underscored the potential value of AFP not just as a binary marker (elevated vs. normal) but as a stratified marker with varying prognostic implications. Admittedly, there is no consensus on the optimal cut-off value for AFP in diagnosing HCC. Therefore, AFP should be used in combination with other diagnostic and prognostic markers for HCC, such as imaging studies and other serum tumor markers, to improve the accuracy of HCC diagnosis and prognosis.36,37 The results of this study support the association between preoperative high serum AFP levels with OS and recurrence for early-stage HCC patients. Furthermore, different AFP levels in an HCC patient before treatment initiation show great potential for determining the post-hepatectomy prognosis, while the combination of the AFP level and other suitable biomarkers or clinical characteristics are also beneficial for improved risk stratification of prognosis for HCC. Surgeons should consider preoperative AFP levels to optimize patient selection, especially when considering a major resection for high tumor burden disease. Hence, incorporating specific biomarker panels to tumor prognostic estimation may enhance the predictive accuracy and, in turn, maximize clinical benefit through optimization of patient selection and prognostic evaluation for surgical resection.
In the present study, even after adjusting for tumor burden characteristics such as tumor diameter and number, preoperative AFP levels maintained an independent predictor association with postoperative survival and recurrence in patients undergoing curative resection for BCLC early-stage HCC. This finding suggests that preoperative AFP levels are an important tumor biological feature to be considered when assessing HCC surgical prognosis. By incorporating preoperative AFP levels into the evaluation, clinicians may be able to identify patients who could benefit from neoadjuvant or adjuvant therapies to reduce postoperative recurrence risk and improve long-term survival outcomes. While we acknowledge that AFP levels alone may not dictate specific treatment decisions, their inclusion in the evaluation process can provide additional valuable information for individualized patient management.
A unique feature of our study was its focus on early-stage HCC (BCLC stage 0/A). While the prognostic role of AFP has been extensively studied in intermediate- and/or advanced-stage HCC, less is known about its impact in early-stage disease. Our results fill this knowledge gap, showing that even among early-stage HCC patients, AFP levels can significantly affect outcomes. These findings have potential implications for the BCLC staging system. If AFP levels are incorporated into this system, this could enhance its prognostic accuracy, potentially leading to more individualized and effective treatment strategies.
The strengths of our study lie in its large sample size, long follow-up period, and rigorous statistical analysis, which together lend credibility to our findings. However, the implications of our study extend well beyond the data presented here. By revealing the incremental prognostic significance of AFP levels, our study suggests that AFP could be a promising therapeutic target. Further research in this direction could lead to the development of innovative treatments aimed at modulating AFP levels, which could improve outcomes for HCC patients.
It is worth noting that our study has several limitations. First, this was a retrospective analysis based on data from a multicenter database, which may introduce inherent biases and limitations. Second, although we adjusted for several clinicopathologic variables in our multivariate analysis, there may still be unmeasured confounding factors that could influence the results. Future studies incorporating comprehensive molecular profiling and genetic analysis may provide a more comprehensive understanding of the prognostic value of AFP in HCC. Additionally, the study was conducted in a Chinese population and the generalizability of the findings to other ethnic groups should be further investigated. Future studies involving diverse populations are needed to validate the findings and determine any potential ethnic variations in the prognostic significance of AFP. Furthermore, it is worth noting that AFP is not a perfect biomarker and has certain limitations. It lacks specificity and can be elevated in other liver diseases, such as cirrhosis and hepatitis. Therefore, a single AFP measurement may not provide sufficient accuracy for individual patient risk assessment. Future studies could explore the incorporation of AFP kinetics, such as the rate of AFP decline after treatment or the AFP doubling time, to further refine its prognostic value and improve patient risk stratification.
Conclusions
This study highlights the prognostic value of serum AFP levels in patients undergoing liver resection for early-stage HCC. The findings underscore the importance of considering tumor biology in addition to traditional clinical parameters for accurate risk assessment and treatment decision making. Incorporating AFP to prognostic estimation of the BCLC algorithm can enhance its predictive accuracy and guide personalized risk stratification and neoadjuvant/adjuvant treatment necessity. Furthermore, future studies should explore the integration of AFP with other biomarkers, such as ctDNA analysis, genomic profiling, or immune-related features, to further refine risk stratification and improve clinical outcomes in patients with early-stage (BCLC stage 0/A) HCC.
References
Vogel A, Meyer T, Sapisochin G, Salem R, Saborowski A. Hepatocellular carcinoma. Lancet. 2022;400:1345–62.
Yang JD, Hainaut P, Gores GJ, Amadou A, Plymoth A, Roberts LR. A global view of hepatocellular carcinoma: trends, risk, prevention and management. Nat Rev Gastroenterol Hepatol. 2019;16:589–604.
Yang T, Lu JH, Wu MC. Hepatocellular carcinoma in China. BMJ. 2010;340:c1026.
Rumgay H, Arnold M, Ferlay J, Lesi O, Cabasag CJ, Vignat J, et al. Global burden of primary liver cancer in 2020 and predictions to 2040. J Hepatol. 2022;77:1598–606.
Bruix J, Reig M, Sherman M. Evidence-based diagnosis, staging, and treatment of patients with hepatocellular carcinoma. Gastroenterology. 2016;150:835–53.
Dhir M, Melin AA, Douaiher J, Lin C, Zhen WK, Hussain SM, et al. A review and update of treatment options and controversies in the management of hepatocellular carcinoma. Ann Surg. 2016;263:1112–25.
Reig M, Forner A, Rimola J, Ferrer-Fàbrega J, Burrel M, Garcia-Criado Á, et al. BCLC strategy for prognosis prediction and treatment recommendation: the 2022 update. J Hepatol. 2022;76:681–93.
Feng ZH, Wang MD, Chen Z, Sun LY, Xu X, Kong QY, et al. Risk factors and long-term prognosis of beyond-Milan recurrence after hepatectomy for BCLC stage 0/A hepatocellular carcinoma: a large-scale multicenter study. Surgery. 2022;172:1147–55.
Yao LQ, Chen ZL, Feng ZH, Diao YK, Li C, Sun HY, et al. Clinical features of recurrence after hepatic resection for early-stage hepatocellular carcinoma and long-term survival outcomes of patients with recurrence: a multi-institutional analysis. Ann Surg Oncol. 2022;29:4291–303.
Ridder DA, Weinmann A, Schindeldecker M, Urbansky LL, Berndt K, Gerber TS, et al. Comprehensive clinicopathologic study of alpha fetoprotein-expression in a large cohort of patients with hepatocellular carcinoma. Int J Cancer. 2022;150:1053–66.
Tsilimigras DI, Moris D, Hyer JM, Bagante F, Ratti F, Marques HP, et al. Serum α-fetoprotein levels at time of recurrence predict post-recurrence outcomes following resection of hepatocellular carcinoma. Ann Surg Oncol. 2021;28:7673–83.
Trevisani F, Garuti F, Neri A. Alpha-fetoprotein for diagnosis, prognosis, and transplant selection. Semin Liver Dis. 2019;39:163–77.
Guan MC, Ouyang W, Wang MD, Liang L, Li N, Fu TT, et al. Biomarkers for hepatocellular carcinoma based on body fluids and feces. World J Gastrointest Oncol. 2021;13:351–65.
Xu XF, Liang L, Xing H, Shen F, Huang DS, Lau WY, et al. Clinical utility of serum biomarkers for hepatocellular carcinoma. Biomark Med. 2021;15:151–5.
Galle PR, Foerster F, Kudo M, Chan SL, Llovet JM, Qin S, et al. Biology and significance of alpha-fetoprotein in hepatocellular carcinoma. Liver Int. 2019;39:2214–29.
Johnson P, Zhou Q, Dao DY, Lo Y. Circulating biomarkers in the diagnosis and management of hepatocellular carcinoma. Nat Rev Gastroenterol Hepatol. 2022;19:670–81.
Hu X, Chen R, Wei Q, Xu X. The landscape of alpha fetoprotein in hepatocellular carcinoma: where are we. Int J Biol Sci. 2022;18:536–51.
Chalasani NP, Porter K, Bhattacharya A, Book AJ, Neis BM, Xiong KM, et al. Validation of a novel multitarget blood test shows high sensitivity to detect early stage hepatocellular carcinoma. Clin Gastroenterol Hepatol. 2022;20:173-82.e7.
Mitsuhashi N, Kobayashi S, Doki T, Kimura F, Shimizu H, Yoshidome H, et al. Clinical significance of alpha-fetoprotein: involvement in proliferation, angiogenesis, and apoptosis of hepatocellular carcinoma. J Gastroenterol Hepatol. 2008;23:e189–97.
Liang L, Wang MD, Zhang YM, Zhang WG, Zhang CW, Lau WY, et al. Association of postoperative biomarker response with recurrence and survival in patients with hepatocellular carcinoma and high alpha-fetoprotein expressions (> 400 ng/ml). J Hepatocell Carcinoma. 2021;8:103–18.
Mazzaferro V, Sposito C, Zhou J, Pinna AD, De Carlis L, Fan J, et al. Metroticket 2.0 model for analysis of competing risks of death after liver transplantation for hepatocellular carcinoma. Gastroenterology. 2018;154:128–319.
Yang SL, Liu LP, Yang S, Liu L, Ren JW, Fang X, et al. Preoperative serum α-fetoprotein and prognosis after hepatectomy for hepatocellular carcinoma. Br J Surg. 2016;103:716–24.
Witjes CD, Polak WG, Verhoef C, Eskens FA, Dwarkasing RS, Verheij J, et al. Increased alpha-fetoprotein serum level is predictive for survival and recurrence of hepatocellular carcinoma in non-cirrhotic livers. Dig Surg. 2012;29:522–8.
Gómez-Rodríguez R, Romero-Gutiérrez M, Artaza-Varasa T, González-Frutos C, Ciampi-Dopazo JJ, de-la-Cruz-Pérez G, et al. The value of the Barcelona Clinic Liver Cancer and alpha-fetoprotein in the prognosis of hepatocellular carcinoma. Rev Esp Enferm Dig. 2012;104:298–304.
Kim H, Lee SJ, Yoon M. Alpha-fetoprotein is correlated with intrahepatic recurrence of hepatocellular carcinoma after a hepatectomy. Ann Surg Treat Res. 2020;98:168–76.
Ren A, Li Z, Zhou X, Zhang X, Huang X, Deng R, et al. Evaluation of the alpha-fetoprotein model for predicting recurrence and survival in patients with hepatitis B virus (HBV)-related cirrhosis who received liver transplantation for hepatocellular carcinoma. Front Surg. 2020;7:52.
Zhang Q, Shang L, Zang Y, Chen X, Zhang L, Wang Y, et al. α-Fetoprotein is a potential survival predictor in hepatocellular carcinoma patients with hepatitis B selected for liver transplantation. Eur J Gastroenterol Hepatol. 2014;26:544–52.
Ding HF, Yang T, Lv Y, Zhang XF, Pawlik TM. Development and validation of an alpha-fetoprotein tumor burden score model to predict post-recurrence survival among patients with hepatocellular carcinoma. J Am Coll Surg. 2023;236(5):982–92.
Edmondson HA, Steiner PE. Primary carcinoma of the liver: a study of 100 cases among 48,900 necropsies. Cancer. 1954;7:462–503.
Strasberg SM, Phillips C. Use and dissemination of the brisbane 2000 nomenclature of liver anatomy and resections. Ann Surg. 2013;257:377–82.
Toso C, Meeberg G, Hernandez-Alejandro R, Dufour JF, Marotta P, Majno P, et al. Total tumor volume and alpha-fetoprotein for selection of transplant candidates with hepatocellular carcinoma: a prospective validation. Hepatology. 2015;62:158–65.
Furihata T, Sawada T, Kita J, Iso Y, Kato M, Rokkaku K, et al. Serum alpha-fetoprotein level per tumor volume reflects prognosis in patients with hepatocellular carcinoma after curative hepatectomy. Hepatogastroenterology. 2008;55:1705–9.
Xiang C, Xiao Y, Ma Z, Peng Y, Li X, Mao X, et al. Liver resection for large and huge hepatocellular carcinoma: predictors of failure, recurrence patterns, and prognoses. Asia Pac J Clin Oncol. 2023;19:e60–70.
Li WF, Yen YH, Liu YW, Wang CC, Yong CC, Lin CC, et al. Preoperative predictors of early recurrence after resection for hepatocellular carcinoma. Am J Surg. 2022;223:945–50.
Ding HF, Zhang XF, Bagante F, Ratti F, Marques HP, Soubrane O, et al. Prediction of tumor recurrence by α-fetoprotein model after curative resection for hepatocellular carcinoma. Eur J Surg Oncol. 2021;47:660–6.
Labgaa I, Villanueva A, Dormond O, Demartines N, Melloul E. The role of liquid biopsy in hepatocellular carcinoma prognostication. Cancers. 2021;13:659.
Debes JD, Romagnoli PA, Prieto J, Arrese M, Mattos AZ, Boonstra A, et al. Serum biomarkers for the prediction of hepatocellular carcinoma. Cancers. 2021;13:1681.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81972726 and 82273074), Dawn Project Foundation of Shanghai (No. 21SG36), Shanghai Health and Hygiene Discipline Leader Project (No. 2022XD001), Shanghai Outstanding Academic Leader Program (No. 23XD1424900), the Natural Science Foundation of Shanghai (No. 22ZR1477900), and Shanghai Science and Technology Committee Rising-Star Program (No. 22QA1411600).
Author information
Authors and Affiliations
Contributions
L-QY, Z-QF, M-DW, Y-KD, and T-HC contributed equally to this work. Conception and design: L-QY, Z-QF, M-DW, G-YL, TY. Administrative support: FS, G-YL, TY. Provision of study material or patients: L-QY, Z-QF, M-DW, T-HC, Y-YZ, ZC, X-MW, Y-HZ, JL, X-PF, Y-JL, CL, Y-KD. Collection and assembly of data: L-QY, Z-QF, M-DW, Y-KD, TY. Data analysis and interpretation: L-QY, Z-QF, M-DW, Y-KD, T-HC, TY. Manuscript writing: All authors. Final approval of the manuscript all authors.
Corresponding authors
Ethics declarations
Disclosure
Lan-Qing Yao, Zhong-Qi Fan, Ming-Da Wang, Yong-Kang Diao, Ting-Hao Chen, Yong-Yi Zeng, Zhong Chen, Xian-Ming Wang, Ya-Hao Zhou, Jie Li, Xin-Ping Fan, Ying-Jian Liang, Chao Li, Feng Shen, Guo-Yue Lv, and Tian Yang have no financial disclosures or conflicts of interest to declare.
Ethical Approval
This study was performed in accordance with the Declaration of Helsinki and was approved by the Institutional Review Boards of all participating hospitals.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yao, LQ., Fan, ZQ., Wang, MD. et al. Prognostic Value of Serum α‐Fetoprotein Level as an Important Characteristic of Tumor Biology for Patients Undergoing Liver Resection of Early-Stage Hepatocellular Carcinoma (BCLC Stage 0/A): A Large Multicenter Analysis. Ann Surg Oncol 31, 1219–1231 (2024). https://doi.org/10.1245/s10434-023-14525-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-14525-w