Abstract
Background
Although internal hemipelvectomies with sacroiliac resections are not traditionally reconstructed, surgeons are increasingly pursuing pelvic ring reconstruction to theoretically improve stability, function, and early ambulation. This study aims to systematically compare complications and functional and oncologic outcomes of sacroiliac resection with and without reconstruction.
Methods
PubMed and MEDLINE were queried for studies published between January 1990 and October 2020 pertaining to sacroiliac neoplasm resection with subsequent reconstruction. Patient demographics, histopathologic diagnoses, reconstruction techniques, Musculoskeletal Tumor Society (MSTS) functional scores, and oncologic outcomes were pooled.
Results
Twenty-three studies (201 patients) were included for analysis. Reconstruction was performed in 79.1% of patients, most commonly with nonvascularized autografts (45.8%). The overall complication rate was 54.8%; however, resection followed by reconstruction demonstrated significantly higher complication (62.3% versus 25.7%, p < 0.001) and infection rates (13.7% versus 0%, p = 0.020). Mean MSTS functional score trended higher in nonreconstructed patients (82% versus 71.6%).
Conclusions
Reconstruction after sacroiliac resection produced higher complication rates and poorer physical recovery when compared with nonreconstructed resection. This systematic review suggests that patients without spinopelvic junction instability may experience superior outcomes without reconstruction. Ultimately, the need to reconstruct the pelvic girdle depends on tumor size, prognosis, and functional goals.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Wide margin resection via internal hemipelvectomy is the mainstay of curative-intent limb-salvage treatment for appropriately indicated patients with primary osseous sarcomas, aggressive benign tumors, and select metastatic disease affecting the pelvis.1,2,3,4 However, the complex bony and soft tissue anatomy, proximity to critical neural and vascular structures, and extent of tumor burden make pelvic resection and reconstruction among the most difficult and technical procedures in orthopedic oncology.5,6,7 This is particularly true for tumors with involvement of the sacroiliac (SI) region, where the sigmoid-shaped SI joint, robust sciatic buttress bone, and proximity of the sacral plexus and vascular structures complicate the resection, thus increasing the risk for iatrogenic injury.8,9
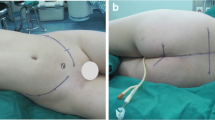
Reconstruction following hemipelvectomy remains controversial as past studies have reported high complication rates without consequential improvements in functional outcomes, justifying the additional procedure.10,11,12 However, resection of the SI joint causing disruption of the pelvic ring without a reconstruction procedure may theoretically lead to compromised stability of the spinopelvic junction.13 This can cause rotation of the hemipelvis and hip joint through the symphysis, increasing the likelihood for postoperative pain, limb-length discrepancies, and altered hip kinematics.14 Efforts to improve postoperative functional and clinical outcomes after internal hemipelvectomy with sacroiliac resection have inspired various techniques for reconstruction. These include the implantation of an allograft or allograft prosthesis composites (APC) (Fig. 1),13,14,15 vascularized and nonvascularized pasteurized autografts,16,17,18,19,20 and rod and screw constructs with or without the augmentation of polymethyl methacrylate (PMMA) bone cement.21,22,23,24 Of course, surgeons may also opt to forgo reconstruction entirely.24,25,26,27
Three-dimensional segmentation of an SI reconstruction in a 77-year-old woman with chondrosarcoma of the right hemipelvis. (1) Posterior view demonstrating the lytic lesion outlined in red, with the planned partial type I resection (orange) and type IV (blue) resection of the sacral ala. (2) Posterior view of the final construct. (3) Anterior view of the allograft prosthesis composite reconstruction demonstrating titanium screw and rod construct (A) and two tibial cortical allograft struts (B). (4) Corresponding postoperative anteroposterior (AP) radiograph of the pelvis
This study sought to perform a systematic review of the current literature in order to develop a better understanding of postoperative complications, functional outcomes, implant survival, and patient survival following the different reconstruction techniques employed for sacroiliac reconstruction after pelvic tumor resection without periacetabular involvement. We also compared outcomes between patients with and without reconstruction of the pelvic defect.
Materials and Methods
Search Strategy
PubMed and MEDLINE were searched in November of 2020 to identify studies in the English language published between January 1990 and October 2020 pertaining to reconstruction techniques following internal hemipelvectomy with sacroiliac resection. The keywords used for the search included “pelvic,” “sacral,” “reconstruction,” and “tumor.” Additional searches through the reference lists of relevant papers were performed to identify additional eligible studies for inclusion.
Study Eligibility
After the initial search, the inclusion criteria were studies describing outcomes of reconstruction methods after hemipelvectomy with type IV and type I/IV resection or any mention of the resection extending through or beyond the SI joint, and specifically without type II (periacetabular) resection. Studies were included regardless of level of evidence, underlying histopathological diagnosis, or age of the subjects. Absolute criteria for exclusion were review articles and other nonclinical studies, and studies that did not distinctly specify outcomes on the basis of the type of resection or the reconstruction technique utilized. The titles and abstracts of all studies were reviewed by two authors (A.G.Z. and N.D.) for increased inter-observer reliability. If the authors agreed that a study did not meet the eligibility criteria, it was excluded. Following the initial screening, the texts of all remaining studies were reviewed independently by the same two authors. If the authors agreed that a study met the eligibility criteria, it was included for data extraction. Conflicts regarding inclusion or exclusion were resolved by a third author (M.P.F.).
Extraction of Outcome Measures
Following full-text screening, data on variables of interest were extracted. If a study described patient outcomes following type IV or I/IV resection in addition to other resection types, patient-level data on only the patients of interest were extracted. These included the number of patients who met the inclusion criteria described by each study and their average age, sex, time of follow-up, primary diagnosis, complication profiles, functional outcomes, and oncologic outcomes. The complications collected included wound complications, deep infection, neurologic complications, failure of the construct used for reconstruction, and any “other” adverse outcomes reported. Oncologic outcomes included the rates of local recurrence, time to recurrence, postoperative metastasis, time to metastasis, and survival status. Functional outcome was determined using the Musculoskeletal Tumor Society (MSTS) functional score, which was documented by most included studies and reported here as a percent value for homogeneity of reporting. Patients whose data were reported in studies discussing outcomes of multiple reconstruction modalities were separated depending on the individual method of reconstruction used in their treatment.
Statistical Analysis
Formal meta-analysis was limited by the heterogeneity of data and limited sample size among the studies included. All statistical methods were performed using Microsoft Excel (Microsoft Corporation, Redmond, WA). Missing data points were treated as null. Weighted means were calculated for continuous variables while estimating missing standard deviations using the range rule of thumb.28 Chi square with adjusted residuals and Bonferroni correction was performed to evaluate differences in complication rates between reconstruction groups. Forest plots were created using the OpenMetaAnalyst statistical software and were utilized to aid in the visualization of complication rates and MSTS functional scores for each reconstruction method.
Results
Search Results
An initial search yielded a total of 2104 results, which after filtering for duplicates, resulted in a total of 1955 studies for screening. The titles and abstracts were reviewed to determine study relevance to the subject matter of interest, which led to the selection of 98 papers for full-text screening. A total of 23 studies satisfied the eligibility criteria and were included for data extraction. A summary of the search strategy is illustrated by Fig. 2.
All studies included were either case reports or small-to-medium-size case series describing patient outcomes after internal hemipelvectomy for a neoplastic indication. The data on patients for whom sacroiliac resection was performed within each study were collected for analysis. The length of follow-up ranged from 2 to 140 months. Fifteen of the 23 studies reported functional outcomes using the MSTS scoring system; however, none reported the preoperative scores for the evaluation of postoperative functional change.
Sample Characteristics
The 23 studies included for analysis evaluated the outcomes of 201 patients who underwent internal hemipelvectomy with either isolated type IV or combined type I/IV resection. Of the total patient sample, 9.5% (n = 19) were treated with type IV resection of the SI joint with minimal iliac involvement, while 90.5% (n = 182) underwent more extensive type I/IV resection (Table 1). The average age of all patients was 33.9 (3–79) years, with an average follow-up of 52.3 (2–240) months. Male patients account for 44.1% (n = 78/177) of the cohort. Overall, 96.5% (n = 193/200) of patients for whom histopathological diagnosis data were available were indicated for hemipelvectomy for the resection of a primary osseous sarcoma or benign tumor compared with 3.5% (n = 7/200) for metastatic disease. The diagnoses within the entire cohort consisted of 14% (n = 28/200) osteosarcoma, 21.5% (n = 43/200) chondrosarcoma, 28.5% (n = 57/200) Ewing’s sarcoma, 7% (n = 14/200) giant cell tumor, and 21% (n = 42/200) other malignant or benign osseous tumors.
There was no reconstruction performed for 20.9% (n = 42/201) of the patients in the total sample.24,25,26,27,29 Of the patients who had a reconstruction procedure, a rod and screw construct was utilized in 5.5% (n = 11/201),21,22,23 nonvascularized autograft in 45.8% (n = 92/201),13,14,16,17,18,20,22,26,27,29,30,31,32,33,34 vascularized autograft in 4.5% (n = 9/201),19,35,36 allograft or APC in 4.5% (n = 8/201),13,14,15 or rod and screws augmented with PMMA in 17.2% (n = 40/201) of patients in the overall cohort.22,23,24,27
Complication Profiles
Complication profiles were reported for 93.5% (n = 188/201) of all patients (Table 2). The complication rate for all patients was 54.3% (n = 102/188), with wound complications being most frequent at a rate of 14.4% (n = 27/188) followed by failure of the construct, defined as a mechanical failure leading either to rapid functional decline or revision surgery, which occurred among 13.3% (n = 25/188) of the entire sample. There was an 11.2% (n = 21/188) infection rate, and postoperative neurological complications (foot drop, paresis, loss of bowel or bladder function, etc.), excluding intentional procedural nerve sacrifice, were the least common complication at a rate of 10.1% (n = 19/188) across the cumulative cohort. The rate of all other reported complications such as graft nonunion was 5.3% (n = 10/188).
On subgroup analysis, patients who did not undergo reconstruction following internal hemipelvectomy with SI resection had a significantly lower complication rate of 25.7% (n = 9/35) compared with a rate of 61.4% (n = 94/153) among all reconstructed patients (p < 0.001). Neurological deficits were the most commonly recorded complications in nonreconstructed patients at a rate of 17.1% (n = 6/35), followed by wound healing issues, which occurred in 5.7% (n = 2/35) of patients. There were no infections reported. In contrast, reconstructed patients experienced wound complications and failure of the construct at an equal rate of 15.3% each (n = 25/153). The infection rate was 13.7% (n = 21/153), and 8.5% (n = 13/153) of patients experienced an unanticipated neurological complication, while 6.5% (n = 10/153) of patients experienced other complications. When comparing the underlying types of complications between nonreconstructed and reconstructed groups, there was a significantly lower incidence of postoperative infection among patients who did not undergo reconstruction (0% versus 13.9%, p = 0.020). There were no differences in the rates of wound complications (p = 0.104), neurological complications (p = 0.123), or other complications (p = 0.118).
Further assessment of reconstructed patients demonstrated that all-cause complications were most prevalent with reconstructions utilizing allografts and APC at a rate of 100% (n = 8/8), and least prevalent with vascularized autografts at a rate of 44.4% (n = 4/11), although sample sizes for both reconstruction techniques were limited and there were no significant differences across all reconstruction groups (p = 0.785). Furthermore, complications occurred at a rate of 60.6% (n = 20/33) in patients reconstructed with PMMA, 54.5% among rod and screw constructs (n = 6/11), and 60.9% in patients treated with nonvascularized autografts (n = 56/92). Wound complications occurred at similar rates regardless of the construct used for reconstruction (p > 0.999). The infection rate was highest after reconstruction with allograft or APC at 37.5% (n = 3/8), whereas none of the patients reconstructed via rod and screw experienced infection, though the difference was nonsignificant (p = 0.839). There were no neurological complications in patients treated with rod and screw constructs with or without PMMA augmentation, while similar rates were seen with other constructs (p = 0.836). Figure 3 demonstrates a forest plot of overall complications between reconstruction techniques, showing significant heterogeneity.
Failure of the construct was reported at similar rates of 27.3% (n = 3/11) of rod and screw constructs, 25% (n = 2/8) of allografts and APC, and 24.2% (n = 8/33) of PMMA constructs, while fewer instances occurred with nonvascularized and vascularized autografts at rates of 12% (n = 11/92) and 11.1% (n = 1/9), respectively, though these differences were not significant (p = 0.929). Failure of rod and screw constructs occurred via aseptic loosening (n = 2/3) and hardware fracture (n = 1/3). Nonvascularized autografts failed via graft fracture (n = 4/11), nonunion (n = 3/11), screw loosening and fracture (n = 2/11), graft resorption (n = 1/11), and failure secondary to tumor recurrence (n = 1/11). The single failure among vascularized autograft patients occurred because of screw fracture (n = 1/1). For allograft and APC, failures included aseptic loosening (n = 1/2) and rod fracture (n = 1/2). All failures in patients treated with PMMA enhanced rod and screw constructs occurred via implant fracture (n = 8/8).
Functional and Oncologic Outcomes
Functional and oncologic outcomes, including MSTS scores and survival data, are summarized by Table 3. MSTS functional scores were reported for 85.1% of patients (n = 171/201), although none of the studies addressing reconstruction via allograft or APC reported this particular outcome. The overall mean MSTS score was 74.0% (13.3–100%). Functional outcomes were best among patients treated with resection without reconstruction, with an average score of 82.0% (43–100%), whereas reconstructed patients reported a lower average MSTS score of 71.6% (13.3–100%). By construct, the highest functional score was reported by patients reconstructed with vascularized autografts at 75.7% (35–92%), while reconstruction with a rod and screw construct demonstrated the lowest functional score at 63.7% (58–72%). This may be appreciated by Fig. 4, which demonstrates a forest plot with significant heterogeneity in outcomes based on the reconstruction construct.
Data on local recurrence and postoperative metastasis were available for 90.5% (n = 182/201) and 85.6% (n = 170/201) of patients, respectively. Local recurrence was recorded among 17.6% of all treated patients (n = 32/182) at an average of 22.8 (6–48) months, while metastasis was seen in 15.6% (n = 29/170) of all patients at an average of 24.3 (5.5–90) months postoperatively. At the time of final follow-up, 68.7% (n = 138/201) of all patients were alive and had no evidence of disease (NED), 8.5% (n = 17/201) were alive with disease (AWD), and 22.4% (n = 45/201) had died of their disease (DOD) after an average of 23.2 (2–168) months postoperatively.
Discussion
Various reconstruction techniques have been employed to ameliorate limb-length discrepancies and improve axial stability with the goal of improving functional outcomes for the patient. This study sought to comprehensively and systematically review the current literature on clinical and oncologic outcomes following sacroiliac neoplasm resection with or without a subsequent reconstruction procedure in order to help guide patient management. The findings show that pelvic ring reconstruction following sacroiliac resection poses a high rate of complications and slightly worse physical function compared with internal hemipelvectomy without reconstruction. Furthermore, although sample sizes were limited, current literature is not able to identify the gold standard construct for sacroiliac reconstruction.
This systematic review has limitations that must be considered when interpreting the findings. One primary limitation included relatively short follow-up periods in several of the included studies. While the short follow-up times observed may in several instances be attributed to high disease burden in the evaluated patient population and high rates of mortality, many reconstruction-specific and oncologic outcomes are best observed with longer-term follow-up. Furthermore, the sizes of the cumulative cohort and the patient samples for each reconstruction technique were small, limiting this review’s ability to detect meaningful differences and increasing the likelihood for heterogeneity in patient demographics and preoperative diagnoses. Additionally, this review relied on data collected from retrospective studies, including case reports. The heterogeneity of data and missing data points inherent to these study designs also make it difficult to compare outcomes among studies with different outcome measures, surgical methodologies, and extents of resections performed. Lastly, functional outcomes reflect long-term results, and may not properly capture nuance such as early functional mobilization with reconstruction. However, this study fills a void that has not previously been explored. Future studies evaluating the influence of defect size on patient functional outcomes following reconstruction with these different constructs could prove a valuable area for comparative analysis.
The decision to reconstruct the pelvic defect after internal hemipelvectomy with sacroiliac resection remains controversial as the choice to perform reconstruction or opt for iliosacral arthrodesis or pseudarthrosis each poses its own risks and benefits. Resection without reconstruction has been shown to provide adequate functional outcomes while reducing operative time, blood loss, hospital stay, and perioperative complications commonly implicated with reconstruction of the hemipelvis.12,25,37,38 Furthermore, some surgeons only advocate for reconstruction if resection of the pelvic tumor leaves a large gap between the sacrum and remaining ilium or acetabulum, or if there is compromise to more than 50% of the SI joint.15,39 In practice, the need for extensive bony resection and pelvic ring disruption due to high tumor burden may lead to vertical and rotational lumbosacral instability, potentially necessitating surgical intervention with a reconstruction procedure to avoid postoperative pain, limb-length discrepancies, or pubic symphysis diastasis.13,21,40 However, the findings from current literature suggest that forgoing reconstruction decreases the risk for complications, particularly decreasing the risk for infection and poor wound healing, while allowing patients to maintain an equivalent or even superior functional status to those undergoing reconstruction.
Complications following pelvic reconstruction for resections of any type have been reported at rates ranging from 50% to 60%, increasing the likelihood for additional surgical procedures and long-term morbidity.40,41,42,43,44 The overall complication rate for patients included in this study who had a reconstruction procedure was similar at 61.4%, with relatively equal rates across constructs for which outcomes on more than ten patients were reported (Fig. 3). While the overall complication rate of 100% seen in patients reconstructed with an allograft or allograft prosthesis composite is likely inflated owing to small sample size, it is worth noting that the complication subtypes that were more prevalent among these patients, such as infection and construct failure via nonunion, hardware failure, or graft fracture, were observed at rates comparable to what has previously been reported in allograft literature.43,45,46,47 When comparing reconstructed patients with those who did not undergo a reconstruction procedure, infection and wound complications were exceedingly more frequent following reconstruction. This can likely be attributed to longer operative time as well as the introduction of metallic implants and grafts, which may serve as a nidus for infection. Furthermore, forgoing reconstruction allows for better wound approximation and decreased tension, thereby minimizing wound complications.
Owing to the complexity of limb-salvage surgery for pelvic tumors, achievement of adequate margins is difficult, yet crucial for local tumor control and the prevention of local disease recurrence. This is particularly true for tumors involving the ilium and sacrum, and those in close proximity to the sciatic notch, where the surgeon runs the risk of unintentional injury to the sacral plexus and iliac vessels in an effort to obtain wide margin resection. Additionally, the extensive venous drainage system around the sacroiliac and presacral regions likely plays a critical role in the development of distant metastases and the overall poor prognosis experienced by these patients.48 This is reflected by the rates of local recurrence and postoperative distant metastases recorded at 17.6% and 15.6%, respectively, among the patients included in this review. In contrast, a recent review of periacetabular tumor reconstructions by Brown et al. discovered a much lower recurrence rate of 6%,44 likely attributed to the fact that wide margin excision of tumors in this area is more easily attained without injury to major neurovascular structures.
One of the main goals of curative-intent internal hemipelvectomy and reconstruction of pelvic defects following tumor resection is to preserve the patient’s functional ability in order to increase the chance for quality-of-life preservation. Among the 15 studies reporting MSTS functional scores, the overall average score was 74%, corresponding to a modest degree of disability. Moreover, patients reported similar functional scores irrespective of the construct used for reconstruction, although the average MSTS score was lower among those reconstructed with isolated rod and screw constructs, suggesting that construct augmentation with bone cement or graft may translate to improved clinical results. However, patients who underwent reconstruction following sacroiliac resection in this review’s patient sample reported worse overall postoperative functional outcomes, with an average MSTS score of 71.6% compared with 82% across nonreconstructed patients (Fig. 4). While this may seem counterintuitive, this finding may be related to the higher complication rate observed among reconstructed patients such as chronic deep tissue infections and construct failures, often ultimately leading to reoperation for debridement, construct revision, or removal. Therefore, while reconstruction following sacroiliac tumor resection has the potential to improve functional outcomes for patients, it also poses a high risk for complication that may ultimately lead to construct removal and functional deterioration. Thus, reconstruction procedures may best be reserved for cases with compromised lumbosacral stability as opposed to being routine in clinical practice.
Conclusions
This study has shown that, regardless of the construct used, reconstruction procedures following internal hemipelvectomy with sacroiliac resection are fraught with complication while resulting in slightly worse ultimate physical function when compared with nonreconstructed patients. Although reconstruction of the pelvic ring is often necessary when the stability of the spinopelvic and lumbosacral junction is compromised, the decision to perform an additional reconstruction is case dependent and should be guided by the patient’s health status, defect size, capacity for rehabilitation, prognosis, and long-term functional goals.
References
O’Connor MI. Malignant pelvic tumors: limb-sparing resection and reconstruction. Semin Surg Oncol. 1997;22:49–54.
Abudu A, Grimer RJ, Cannon SR, Carter SR, Sneath RS. Reconstruction of the hemipelvis after the excision of malignant tumours: complications and functional outcome of prostheses. J Bone Joint Surg Br. 1997;79:773–9.
Carter S, Eastwood D, Grimer R, Sneath R. Hindquarter amputation for tumours of the musculoskeletal system. J Bone Joint Surg Br. 1990;72:490–3.
Pant R, Moreau P, Ilyas I, Paramasivan O, Younge D. Pelvic limb-salvage surgery for malignant tumors. Int Orthop. 2001;24:311–5.
Bird JE. Advances in the surgical management of bone tumors. Curr Oncol Rep. 2014;16:392.
Biermann JS, Adkins DR, Benjamin RS, et al. Bone cancer. J Natl Compr Cancer Netw. 2010;8:688–712.
Jemal A, Siegel R, Xu J. Cancer statistics. CA Cancer J Clin. 2010;60:27–300.
Gokaslan ZL, Hsu W. Surgical resection of sacral tumors. Schmidek and Sweet Operative Neurosurgical Techniques: Indications, Methods, and Results: Sixth Edition: Elsevier Inc.; 2012:2201-16.
Enneking WF, Dunham W. Resection and reconstruction for primary neoplasms involving the innominate bone. JBJS. 1978;60:731–46.
Angelini A, Drago G, Trovarelli G, Calabrò T, Ruggieri P. Infection after surgical resection for pelvic bone tumors: an analysis of 270 patients from one institution. Clin Orthop Rel Res. 2014;472:349–59.
O’connor M, Sim F. Salvage of the limb in the treatment of malignant pelvic tumors. JBJS. 1989;71:481–94.
Beadel GP, McLaughlin CE, Aljassir F, et al. Iliosacral resection for primary bone tumors: is pelvic reconstruction necessary? Clin Orthop Rel Res. 2005;438:22–9.
Michelle JC, Patricia LZ, Mari LG, et al. En bloc hemisacrectomy and internal hemipelvectomy via the posterior approach. J Neurosurg Spine. 2014;21:458–67.
Tepper SC, Blank AT, Gitelis S, Colman MW. Pelvic ring reconstruction with segmental spinal instrumentation after complete type I pelvic resection. J Surg Oncol. 2020;12:358.
Aydinli U, Akesen B, Yalçinkaya U, Hakyemez B, Serifoğlu R. Iliosacral fixation after type-1 hemipelvectomy: a novel technique. Acta Orthop Belg. 2012;78:393–7.
Nassif NA, Buchowski JM, Osterman K, McDonald DJ. Surgical technique: Iliosacral reconstruction with minimal spinal instrumentation. Clin Orthop Rel Res. 2013;471:947–55.
Ozaki T, Hillmann A, Lindner N, Blasius S, Winkelmann W. Chondrosarcoma of the pelvis. Clin Orthop Rel Res. 1997;337:226–39.
Xu M, Zheng K, Zhao J, Bai W, Yu X. En bloc resection and pelvic ring reconstruction for primary malignant bone tumors involving sacroiliac joint. Orthop Surg. 2019;11:1120–6.
Nishida J, Shiraishi H, Okada K, Ehara S, Shimamura T. Vascularized iliac bone graft for iliosacral bone defect after tumor excision. Clin Orthop Rel Res. 2006;447:145–51.
Krieg A, Mani M, Speth B, Stalley P. Extracorporeal irradiation for pelvic reconstruction in Ewing’s sarcoma. J Bone Joint Surg Br. 2009;91:395–400.
Guo W, Sun X, Ji T, Tang X. Outcome of surgical treatment of pelvic osteosarcoma. J Surg Oncol. 2012;106:406–10.
Lin P, Shao Y, Lu H, et al. Pelvic reconstruction with different rod-screw systems following Enneking type I/I+ IV resection: a clinical study. Oncotarget. 2017;8:38978.
Gebert C, Wessling M, Gosheger G, et al. Pelvic reconstruction with compound osteosynthesis following hemipelvectomy: a clinical study. Bone Joint J. 2013;95:1410–6.
Kollender Y, Shabat S, Bickels J, et al. Internal hemipelvectomy for bone sarcomas in children and young adults: surgical considerations. Eur J Surg Oncol. 2000;26:398–404.
Puri A, Gulia A, Jambhekar N, Laskar S. Results of surgical resection in pelvic Ewing’s sarcoma. J Surg Oncol. 2012;106:417–22.
Wang J, Tang Q, Xie X, et al. Iliosacral resections of pelvic malignant tumors and reconstruction with nonvascular bilateral fibular autografts. Ann Surg Oncol. 2012;19:4043–51.
Schwameis E, Dominkus M, Krepler P, et al. Reconstruction of the pelvis after tumor resection in children and adolescents. Clin Orthop Rel Res. 2002;402:220–35.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135.
Tao J, Weifeng L, Hairong X, Yuan L, Lin H, Xiaohui N. How does iliosacral bone tumor resection without reconstruction affect the ipsilateral hip joint? BMC Musculoskelet Disord. 2018;19:1–7.
Zhou Y-J, Yunus A, Tian Z, et al. The pedicle screw-rod system is an acceptable method of reconstructive surgery after resection of sacroiliac joint tumours. Contemp Oncol. 2016;20:73.
Akiyama T, Clark J, Miki Y, Choong P. The non-vascularised fibular graft: a simple and successful method of reconstruction of the pelvic ring after internal hemipelvectomy. J Bone Joint Surgery Br. 2010;92:999–1005.
Sabourin M, Biau D, Babinet A, Dumaine V, Tomeno B, Anract P. Surgical management of pelvic primary bone tumors involving the sacroiliac joint. Orthop Traumatol Surg Res. 2009;95:284–92.
Honl M, Westphal F, Carrero V, et al. Pelvic girdle reconstruction based on spinal fusion and ischial screw fixation in a case of aneurysmal bone cyst. Sarcoma. 2003;7:177–82.
Krieg A, Lenze U, Gaston M, Hefti F. The outcome of pelvic reconstruction with non-vascularised fibular grafts after resection of bone tumours. J Bone Joint Surg Br. 2010;92:1568–73.
Oshima Y, Miyoshi K, Mikami Y, Kawamura N. Pelvic ring reconstruction with a vascularized pedicle iliac bone graft for a large sacral schwannoma. Clin Spine Surg. 2005;18:200–2.
Ogura K, Sakuraba M, Miyamoto S, Fujiwara T, Chuman H, Kawai A. Pelvic ring reconstruction with a double-barreled free vascularized fibula graft after resection of malignant pelvic bone tumor. Arch Orthop Trauma Surg. 2015;135:619–25.
Gerrand CH, Bell RS, Griffin AM, Wunder JS. Instability after major tumor resection: prevention and treatment. Orthop Clin. 2001;32:697–710.
Gupta S, Griffin AM, Gundle K, et al. Long-term outcome of iliosacral resection without reconstruction for primary bone tumours. Bone Joint J. 2020;102-B:779–87.
Gennari L, Azzarelli A, Quagliuolo V. A posterior approach for the excision of sacral chordoma. J Bone Joint Surg Br. 1987;69:565–8.
Campanacci M, Capanna R. Pelvic resections: the Rizzoli Institute experience. Orthop Clin North Am. 1991;22:65–86.
Stephenson RB, Kaufer H, Hankin FM. Partial pelvic resection as an alternative to hindquarter amputation for skeletal neoplasms. Clin Orthop Rel Res. 1989;17:201–11.
Ozaki T, Hillmann A, Bettin D, Wuisman P, Winkelmann W. High complication rates with pelvic allografts: experience of 22 sarcoma resections. Acta Orthop Scand. 1996;67:333–8.
Hillmann A, Hoffmann C, Gosheger G, Rödl R, Winkelmann W, Ozaki T. Tumors of the pelvis: complications after reconstruction. Arch Orthop Trauma Surg. 2003;123:340–4.
Bt S, Sc G, Rp S, Sf H, Ld G, Am P. Reconstruction of the hip after resection of periacetabular oncological lesions. Bone Joint J. 2018;100-B:22–30.
Karim SM, Colman MW, Lozano-Calderón SA, Raskin KA, Schwab JH, Hornicek FJ. What are the functional results and complications from allograft reconstruction after partial hemipelvectomy of the pubis? Clin Orthop Rel Res. 2015;473:1442–8.
Delloye C, Banse X, Brichard B, Docquier P-L, Cornu O. Pelvic reconstruction with a structural pelvic allograft after resection of a malignant bone tumor. JBJS. 2007;89:579–87.
Langlais F, Lambotte J, Thomazeau H. Long-term results of hemipelvis reconstruction with allografts. Clin Orthop Rel Res. 2001;388:178–86.
Guo Z, Li J, Pei G-X, Li X-D, Wang Z. Pelvic reconstruction with a combined hemipelvic prostheses after resection of primary malignant tumor. Surg Oncol. 2010;19:95–105.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors have no conflicts of interest to declare. All co-authors have seen and agree with the contents of the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zavras, A.G., Fice, M.P., Dandu, N. et al. Comparison of Reconstruction Techniques Following Sacroiliac Tumor Resection: A Systematic Review. Ann Surg Oncol 29, 7081–7091 (2022). https://doi.org/10.1245/s10434-022-11890-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-11890-w