Abstract
Background
Cytoreductive surgery (CRS) provides a survival benefit when achieved without residual disease. As diaphragm is frequently affected in peritoneal malignancies, complete cytoreduction often requires surgical techniques over the diaphragm. The purpose of the study was to assess diaphragmatic resection impact on cytoreduction completeness, morbidity and mortality compared to less aggressive diaphragmatic peritonectomy in CRS and hyperthermic intraperitoneal chemotherapy (HIPEC) settings.
Materials and Methods
Patients with peritoneal carcinomatosis and supramesocolic disease undergoing CRS/HIPEC from 2011 to 2019 were included in a prospectively collected database. We compared patients who underwent full-thickness diaphragmatic resection (DR) and diaphragmatic peritonectomy (DP). Epidemiological and clinical data, morbidity, and mortality within 90 days of surgery were documented.
Results
232 patients were initially selected. Inclusion criteria were met by 88 procedures. DR was performed on 32 patients and DP on 56. Number of resected organs was 5.21 in the DR cohort vs. 3.57 in the DP cohort (p<0.0001). Rate of Peritoneal Cancer Index (PCI) score >14 was higher in the DR group (75%) than in the DP group (50.9%) (p=0.027). Tumor invasion of diaphragmatic muscle after DR was confirmed in 89.3% patients. Postoperative pleural effusion was observed in 28 patients (50%) in the DP group and in 17 (53.1%) in the DR group.
Conclusions
CRS/HIPEC requires specific surgical techniques over the diaphragm to achieve complete cytoreduction. As diaphragmatic muscle invasion is frequent, full-thickness resection may allow a cytoreduction completeness increase without an increased morbidity. Pleural drains are not systematically required as these procedures show low incidence of major respiratory complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (CRS/HIPEC) is part of the currently accepted treatment for different peritoneal surface malignancies,1,2 as it has been found to prolong survival in randomized controlled trials3,4 and long retrospective studies.5,6,–7
Given that diaphragmatic infiltration is a frequent finding and that survival benefit is specially obtained when no residual disease is left,5 the ability to perform upper abdominal surgical techniques over the diaphragm influences oncologic outcomes, as cytoreduction completeness is an independent prognostic factor for overall survival (OS) and disease-free survival (DFS).8,9,–10 However, the impact of diaphragmatic peritoneal peritonectomy versus full-thickness resection on postoperative morbidity, mortality, cytoreduction completeness, and survival is not well documented.
The main purpose of this study was to describe the impact of diaphragmatic resection (DR) on cytoreduction completeness, morbidity, mortality, and OS compared with the less aggressive diaphragmatic peritonectomy (DP) procedure in CRS/HIPEC settings.
Materials and Methods
Study Design and Patient Selection
This was a retrospective study of all peritoneal carcinomatosis patients with supramesocolic disease who underwent CRS/HIPEC from January 2011 to October 2019. We compared patients undergoing full-thickness DR (DR group) with those subjected to DP (DP group). Inclusion criteria were Eastern Cooperative Oncology Group (ECOG) score of 0–1, American Society of Anesthesiologists (ASA) score of 0–3, absence of extra-abdominal metastases, identification of resectable peritoneal disease in the preoperative computed tomography (CT) scan, and three or fewer resectable liver metastases not requiring a major hepatectomy. Patients with non-resectable disease, thoracic surgery in the same procedure, ECOG score > 1, or lacking follow-up data were excluded (Fig. 1).
We recorded epidemiological and clinical data, including age, sex, primary cancer type, neoadjuvant chemotherapy, Peritoneal Cancer Index (PCI), organs removed, and postoperative complications, and documented perioperative morbidity and mortality during hospitalization and within 90 days of surgery following the Clavien–Dindo classification.11 We also analyzed respiratory complications comparing both cohorts and using version 5.0 of the National Cancer Institute’s Common Terminology Criteria for Adverse Events (NCI–CTCAE) classification.12 This classification has been validated in the literature and takes into account the specific symptoms for each complication type. A grading (severity) scale is provided for each adverse event term.
We focused the analysis on respiratory complications (pleural effusion, pneumonia, pneumothorax, and respiratory failure) and included all NCI–CTCAE classification grades: Grade 1 (asymptomatic or mild symptoms with clinical or diagnostic observations only); Grade 2 (minimal, local, or noninvasive intervention indicated); Grade 3 (severe or medically significant but not immediately life-threatening, operative intervention including chest tube or pleurodesis indicated); Grade 4 (life-threatening respiratory or hemodynamic compromise; intubation or urgent intervention indicated); and Grade 5 (death related to the respiratory complication). To evaluate pleural effusion, we performed a daily chest radiography for all patients at 24 and 48 h, and repeated the chest radiography if patients showed symptoms during hospitalization. The NCI–CTCAE classification considers respiratory failure as a Grade 4 complication.12
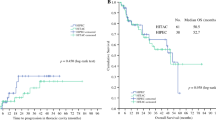
We stratified and analyzed OS and DFS by the most common tumor types (gynecological, colorectal, and appendiceal origin) in order to avoid bias.
The main purpose of this study was to describe the impact of DR on cytoreduction completeness, morbidity, mortality, and OS compared with the less aggressive DP procedure in CRS/HIPEC settings.
This study was approved by our institutional Ethics Committee and has been developed according to the Declaration of Helsinki statements.
Preoperative Planning and Management
All cases were evaluated by a multidisciplinary committee on peritoneal surface malignancies, and indication for surgery was determined according to their assessment.
We evaluated preoperative staging with CT scans of the chest, abdomen, and pelvis in all patients, and with positron emission tomography (PET) when indicated by the committee. When high PCI or thoracic disease were suspected, laparoscopy ± thoracoscopy was performed to assess the possibility of complete cytoreduction in order to avoid unnecessary laparotomies. Extra-abdominal disease or non-resectable liver metastasis were contraindications for CRS/HIPEC.
We applied the same treatment protocol for all patients. Preoperative prophylactic intravenous antibiotics (cefotaxime 2 g and metronidazole 500 mg) were infused 30 min before incision and maintained over a 48-h period. The anesthetic strategy was based on general anesthesia, epidural analgesia, invasive monitoring, and goal-directed fluid balance.13
Operative Technique
An xifopubic incision is performed while the patient is in the Lloyd Davies position. The first step is to evaluate the patient’s PCI and to determine whether complete cytoreduction is achievable with no disease remaining (CC-0).
Peritoneal peritonectomy is performed in the affected areas to obtain a complete macroscopic resection, including anterior parietal peritoneum, pelvis, and diaphragmatic peritoneum. Appendectomy, omentectomy, and cholecystectomy are performed as per protocol.1,2
DR is performed if disease extends beyond the peritoneal surface. In order to do so, we delimitate the resection area using Crile forceps. In coordination with the anesthesiologist, we open the diaphragm. The parietal pleura and the lungs are then assessed to rule out disease. Afterwards, we complete the resection under direct view, ensuring tumor-free resection margins and taking special care to avoid peritoneal fluid leakage inside the thorax to prevent seeding.
Once resection is performed, we use a running polypropylene 0 suture to close the defect. A surgical aspirator is placed inside the defect before closing it and, in coordination with the anesthesiologist, and while performing a Valsalva maneuver, we proceed to knot the suture while aspirating to avoid pneumothorax (Video 1). Neither intrathoracic drains nor mesh are placed to close the defect.14 All patients are extubated in the operating room and start early respiratory rehabilitation using a TriFlow© in order to encourage slow sustained maximal inspiration (SMI).
We use Sugarbaker’s complete cytoreduction (CC) classification: CC-0 (no disease), CC-1 (< 0.25 cm); CC-2 (0.25–2.5 cm); CC-3 (> 2.5 cm).15, 16
The open approach (Coliseum) is our technique of choice for delivering HIPEC. We apply it once we have performed CRS, closed all diaphragmatic defects, and completed all gastrointestinal anastomoses. We used oxaliplatin in colorectal cancer until 2018, then changed to mitomycin C (20 mg/m2 for 60 min and 10 mg/m2 for 30 min diluted in 3 L/m2 of a 1.5% glucose solution at 42 °C)0.17 In ovarian cancer, we used paclitaxel until 2016, then changed to cisplatin (15 mg/m2/2L diluted in 3 L/m2 of a 1.5% glucose solution for 60 min at 42 °C) according to the last published evidence.3
Statistical Analysis
SPSS version 26 was used for data analysis (IBM Corporation, Armonk, NY, USA). For continuous variables, we used Student’s t test if the distribution was normal, and the Mann–Whitney U test if it was not. To compare categorical variables, we used the Chi square or Fisher’s exact tests. Variables with a p-value < 0.05 were considered statistically significant. OS was represented using the Kaplan–Meier method.
Results
From the 232 patients who underwent CRS/HIPEC, 98 presented diaphragmatic involvement. Four patients were excluded from the study: one due to incomplete cytoreduction (CC-2), one due to combined surgery (the abdominal and thoracic approaches), and two because they did not receive HIPEC. Six patients were lost to follow-up, thus resulting in a final sample of 88 patients (Fig. 1).
DR was performed on a total of 32 patients, and DP was performed on 56 patients. The PCI was 14.51 in the DP group and 16.75 in the DR group (p = 0.18). The clinicopathologic characteristics of both groups are reported in Table 1.
The number of resected organs was higher in the DR cohort, with 5.21 organs involved, versus 3.57 in the DP cohort (p < 0.0001). Operative time was 53.4 min longer in the DR group (p = 0.022). PCI score > 14 was higher in the DR group (75%) than in the DP group (50.9%; p = 0.027.
Anatomopathological analysis after DR confirmed tumor invasion of the diaphragmatic muscle in 89.3% of the specimens.
No difference was observed between the two groups regarding other perioperative outcomes (Table 2). Only two (3.6%) patients in the DP cohort and 4 (12.5%) patients in the DR cohort required placement of an intraoperative chest tube (p = 0.110).
Postoperative variables are reported in Table 3. Major complications at 90 days (Clavien–Dindo classification III–IV) were similar in both groups, with no significant differences during hospital stay, intensive care unit (ICU) stay, readmission, or reoperation.
According to the NCI–CTCAE classification, pneumonia was identified in two DP patients and one DR patient, while respiratory failure was identified in one DP patient and two DR patients. No patients experienced postoperative pneumothorax.
Postoperative pleural effusion was identified in 28 patients (50%) in the DP group and 17 patients (53.1%) in the DR group. Placement of the chest tube was necessary in three patients (5.4%) in the DP group and one patient (3.1%) in the DR group, with no significant difference (Table 4).
Discussion
Diaphragmatic Invasion and Complete Cytoreduction
CRS/HIPEC is part of the currently accepted treatment for different peritoneal surface malignancies,1,2 as it has been found to prolong survival in randomized controlled trials.3,4 Furthermore, similar findings based on long retrospective studies are available for appendiceal malignancies, pseudomyxoma peritonei, and malignant mesothelioma.5,6,–7
Cytoreductive surgery is associated with a significant survival benefit, but this benefit is only obtained when no residual disease remains.5 Considering that complete cytoreduction is an independent prognostic factor for OS and DFS in these patients, the ability to perform upper abdominal techniques may influence oncologic outcomes.8,9,–10,18
Techniques such as diaphragmatic procedures, including peritonectomy or full-thickness resection, have been reported to be required in 29.6–50% of CRS/HIPEC surgeries.19,20 We performed these procedures in 42.2% of our CRS/HIPEC cases.
Full-thickness DR is required when tumor has surpassed the peritoneal barrier and infiltrated the diaphragmatic muscle. When diaphragmatic invasion is suspected, peritonectomy or electrovaporization are insufficient, as residual tumor, located in the deeper muscle layers, will not be eradicated.
Such cases can be recognized during surgery if the diaphragmatic peritoneum and muscle cannot be easily detached, and a tumor mass can be detected by digital examination. In these cases, we perform a full-thickness DR along with a peritoneal peritonectomy, as previously described.
Invasion of the diaphragmatic muscle is not unusual. In our series, 89.3% of patients who underwent full-thickness DR had histological confirmation of diaphragmatic muscle involvement. There are no previous reports in the literature regarding the histological confirmation of this involvement, but this figure allows us to estimate that the study CC-0 rate (81.3%) would have been significantly lower if full-thickness DR had not been performed.
Although pleural recurrence has been described as a theoretical risk after DR, there are no published data in peritoneal carcinomatosis contexts. As for our series, no cases of pleural dissemination have been registered.
Overall Morbidity, Particularly Respiratory Complications
Regarding-postoperative overall morbidity, particularly respiratory complications, previous studies of CRS/HIPEC describe complication rates of 27–56% and a mortality rate of 0–11%, but the impact of diaphragmatic CRS on these outcomes is unknown.21
Our findings showed that compared with peritonectomy, full-thickness DR was not associated with higher values for major complications (Clavien–Dindo III–IV) or longer hospital or ICU stays, despite registering significantly higher values for PCI and number of organs removed with statistically significant differences. These results are similar to those reported in other diaphragmatic peritonectomy versus resection studies.22,23
Regarding respiratory complications, previous studies reported a pleural effusion rate of 42–98%.20,22 In our study, 48.9% of patients undergoing a diaphragmatic procedure did not suffer postoperative pleural effusion, and 27.3% had asymptomatic pleural effusion with no intervention indicated (Table 4). Only 4.5% of patients needed a postoperative thoracic drain. The intraoperative chest tube rate was low, after both peritonectomy (3.6%) and DR (12.5%).
No postoperative pneumothorax was registered in any patients, although the incidence reported in other studies reached 16.5–33% after diaphragmatic procedures24,25. The rate of respiratory complications of both peritonectomy and full-thickness DR was low and was not significantly different (Tables 3 and 4).
We hypothesize that low rates of respiratory complications may be explained by a constellation of factors. Our anesthesiology team follows a standardized goal-directed therapy protocol 13 that allows to individually adjust fluid therapy, avoiding overhydration and probably reducing postoperative pleural effusion. Moreover, the previously described surgical technique, consisting of closing the diaphragmatic defect during aspiration while performing a Valsalva maneuver (Video 1), may have an impact regarding pleural effusion and pneumothorax. Likewise, early postoperative respiratory rehabilitation may also contribute to reducing respiratory complications.
According to our experience, thoracic drains are not routinely required.24 We advocate for selective use of thoracostomy tubes during CRS/HIPEC with DR. Only a few patients (4.5%) needed a postoperative thoracic drain, as 95.5% of respiratory complications were minor (NCI–CTCAE classification) and were medically managed.
Limitations
The main limitations of our study are our patient population heterogeneity and a reduced patient sample, which made us focus on the procedure and the perioperative outcomes rather than on OS.
Conclusions
CRS/HIPEC surgery frequently requires specific surgical techniques over the diaphragm to obtain complete cytoreduction. As diaphragmatic muscle invasion is not uncommon, full-thickness DR may allow for an increase in cytoreduction completeness without an increase in morbidity. Patients undergoing diaphragmatic peritonectomy or resection do not systematically need pleural drains. The incidence of major respiratory complications after these procedures is low.
References
NCCN Guidelines insights: colon cancer, version 2.2018. J Natl Comprehens Cancer Netw. 2018;16(4). Available at: https://jnccn.org/view/journals/jnccn/16/4/article-p359.xml. Accessed 19 Feb 2020.
Querleu D, Planchamp F, Chiva L, et al. European society of gynaecological oncology (ESGO) guidelines for ovarian cancer surgery. Int J Gynecol Cancer. 2017;27(7):1534–1542. https://doi.org/10.1097/igc.0000000000001041
Van Driel WJ, Koole SN, Sikorska K, et al. Hyperthermic intraperitoneal chemotherapy in ovarian cancer. N Engl J Med. 2018;378(3):230–240. https://doi.org/10.1056/nejmoa1708618
Verwaal VJ, Bruin S, Boot H, Van Slooten G, Van Tinteren H. 8-Year follow-up of randomized trial: Cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy in patients with peritoneal carcinomatosis of colorectal cancer. Ann Surg Oncol. 2008;15(9):2426–2432. https://doi.org/10.1245/s10434-008-9966-2
Du Bois A, Sehouli J, Vergote I, et al. Randomized phase III study to evaluate the impact of secondary cytoreductive surgery in recurrent ovarian cancer: final analysis of AGO DESKTOP III/ENGOT-ov20. J Clin Oncol. 2020;38(15 Suppl):6000. https://ascopubs.org/doi/10.1200/JCO.2020.38.15_suppl.6000. Accessed June 20, 2020.
Yan TD, Deraco M, Baratti D, et al. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for malignant peritoneal mesothelioma: multi-institutional experience. J Clin Oncol. 2009;27(36):6237–6242. https://doi.org/10.1200/jco.2009.23.9640
Youssef H, Newman C, Chandrakumaran K, Mohamed F, Cecil TD, Moran BJ. Operative findings, early complications, and long-term survival in 456 patients with pseudomyxoma peritonei syndrome of appendiceal origin. Dis Colon Rectum. 2011;54(3):293-299. https://doi.org/10.1007/dcr.0b013e318202f026
Eng OS, Raoof M, Blakely AM, et al. A collaborative surgical approach to upper and lower abdominal cytoreductive surgery in ovarian cancer. J Surg Oncol. 2018;118(1):121–126. https://doi.org/10.1002/jso.25120
Shin KK, Chi DS. Maximal cytoreductive effort in epithelial ovarian cancer surgery. J Gynecol Oncol. 2010;21(2):75–80. https://doi.org/10.3802/jgo.2010.21.2.75
Shashikant L, Kesterson Joshua P. In Pursuit of optimal cytoreduction in ovarian cancer patients: the role of surgery and surgeon. J Obstet Gynaecol India. 2009;59(3):209–216. https://doi.org/10.1126/science.1249098.sleep
11. Bolliger M, Kroehnert JA, Molineus F, Kandioler D, Schindl M, Riss P. Experiences with the standardized classification of surgical complications (Clavien-Dindo) in general surgery patients. Eur Surg. 2018;50(6):256–261. https://doi.org/10.1007/s10353-018-0551-z
National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE) Common Terminology Criteria for Adverse Events (CTCAE) v5.0.; 2017. Available at: https://www.meddra.org/. Accessed 7 April 2020.
Esteve-Pérez N, Ferrer-Robles A, Gómez-Romero G, et al. Goal-directed therapy in cytoreductive surgery with hyperthermic intraperitoneal chemotherapy: a prospective observational study. Clin Transl Oncol. 2019;21(4):451–458. https://doi.org/10.1007/s12094-018-1944-y
Silver DF. Full-thickness diaphragmatic resection with simple and secure closure to accomplish complete cytoreductive surgery for patients with ovarian cancer. Gynecol Oncol. 2004;95(2):384–387. https://doi.org/10.1016/j.ygyno.2004.07.046
Jacquet P, Sugarbaker PH. Clinical research methodologies in diagnosis and staging of patients with peritoneal carcinomatosis. Cancer Treat Res. 1996;82:359–374. https://doi.org/10.1007/978-1-4613-1247-5_23
Bao P, Bartlett D. Surgical techniques in visceral resection and peritonectomy procedures. Cancer J. 2009;15(3):204–211. https://doi.org/10.1097/ppo.0b013e3181a9c6f0
Morales-Soriano R, Esteve-Pérez N, Segura-Sampedro JJ, et al. Current practice in cytoreductive surgery and HIPEC for metastatic peritoneal disease: Spanish multicentric survey. Eur J Surg Oncol. 2018;44(2):220–227. https://doi.org/10.1016/j.ejso.2017.11.012
Segura-Sampedro JJ, Morales-Soriano R, Arjona-Sánchez Á, Cascales-Campos P. Secondary surgical cytoreduction needs to be assessed taking into account surgical technique, completeness of cytoreduction, and extent of disease. World J Surg Oncol. 2020;18(1):92. https://doi.org/10.1186/s12957-020-01853-4
Singh B, Singh G, Pourgholami M, Alzahrani N, Morris DL. Long-term survival and propensity score matched outcomes of bilateral vs. unilateral diaphragm interventions in cytoreductive surgery plus intra-peritoneal chemotherapy. Anticancer Res. 2018;38(10):5917–5921. https://doi.org/10.21873/anticanres.12936
Cascales Campos P, Martinez Insfran LA, Wallace D, et al. Identifying the incidence of respiratory complications following diaphragmatic cytoreduction and hyperthermic intraoperative intraperitoneal chemotherapy. Clin Transl Oncol. 2020;22(6):852–859. https://doi.org/10.1007/s12094-019-02195-8
Tabrizian P, Jibara G, Shrager B, et al. Outcomes for cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in the elderly. Surg Oncol. 2013;22(3):184–189. https://doi.org/10.1016/j.suronc.2013.06.001
Sullivan BJ, Bekhor EY, Carpiniello M, et al. Diaphragmatic Peritoneal Stripping Versus Full-Thickness Resection in CRS/HIPEC: Is There a Difference? Ann Surg Oncol. 2020;27(1):250–258. https://doi.org/10.1245/s10434-019-07797-8
Grotz TE, Mansfield PF, Royal RE, et al. Intrathoracic chemoperfusion decreases recurrences in patients with full-thickness diaphragm involvement with mucinous appendiceal adenocarcinoma. Ann Surg Oncol. 2016;23(9):2914–2919. https://doi.org/10.1245/s10434-016-5209-0
Singh B, Singh G, Alzahrani N, Morris DL. Long term survival and perioperative propensity score matched outcomes of diaphragmatic resections compared to stripping in cytoreductive surgery + intra-peritoneal chemotherapy. Am J Surg. 2020;219(4):673–680. https://doi.org/10.1016/j.amjsurg.2019.06.018
Papadia A, Morotti M. Diaphragmatic surgery during cytoreduction for primary or recurrent epithelial ovarian cancer: A review of the literature. Arch Gynecol Obstet. 2013;287(4):733-741. https://doi.org/10.1007/s00404-013-2715-1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Andrea Craus-Miguel, Juan José Segura-Sampedro, Xavier González-Argenté, and Rafael Morales-Soriano have no disclosures to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (MOV 96344 kb)
Rights and permissions
About this article
Cite this article
Craus-Miguel, A., Segura-Sampedro, J.J., González-Argenté, X. et al. Diaphragmatic Peritonectomy and Full-Thickness Resection in CRS/HIPEC May Allow Higher Completeness of Cytoreduction Rates with a Low Rate of Respiratory Complications. Ann Surg Oncol 28, 4676–4682 (2021). https://doi.org/10.1245/s10434-020-09505-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09505-3