Abstract
Background
The 2015 American Thyroid Association guidelines state that a prophylactic central compartment neck dissection (PCND) should be considered for patients with papillary thyroid carcinoma (PTC) and clinically involved lateral neck lymph nodes (cN1b). The purpose of our study was to determine the rate of central neck recurrence in select cN1b patients, with no evidence of clinically involved central compartment lymph nodes, treated without a PCND.
Methods
After institutional review board approval, adult PTC patients with cN1b disease who were treated with a total thyroidectomy and lateral neck dissection were identified from an institutional database of 6259 patients who underwent initial surgery for well-differentiated thyroid carcinoma from 1986 to 2015. Patients with gross extrathyroidal extension, distant metastases, or no preoperative imaging were excluded. Patients with evidence of clinically involved central compartment lymph nodes, on preoperative imaging or intraoperative evaluation, also were excluded. A total of 152 cN1b patients were included and categorized into non-PCND and PCND groups. Central neck recurrence-free probability (CNRFP) was calculated using the Kaplan–Meier method and log-rank tests.
Results
One hundred three patients (67.8%) did not have a PCND. With a median follow-up of 65 months, the 5- and 10-year CNRFP was 98.4% in the non-PCND group and 93.6% in the PCND group (p = 0.133).
Conclusions
Select PTC patients with cN1b disease but no evidence of clinically involved central compartment lymph nodes, on preoperative imaging and intraoperative evaluation, appear to have a low rate of central neck recurrence. These patients may not require or benefit from a PCND.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Regional lymph node metastases are common in patients with papillary thyroid carcinoma (PTC), occurring in approximately 30.0–80.0% of PTC cases.1,2,3,4 Patients with clinically involved lateral compartment lymph node metastases also often have central compartment lymph node metastases. The reported rate of pathological lateral compartment lymph nodes without evidence of central nodal disease is low.5,6,7 The 2015 American Thyroid Association (ATA) guidelines and 2019 National Comprehensive Cancer Network (NCCN) guidelines state that a prophylactic central neck dissection (PCND) should be considered in PTC patients with clinically involved lateral compartment lymph nodes (cN1b).8,9 However, there is limited evidence to support this recommendation.
Surgery of the central compartment is not without risk, and however minimal, a central compartment neck dissection is associated with injury to the parathyroid glands and recurrent laryngeal nerves, resulting in temporary or permanent hypoparathyroidism and hoarseness. Overall, PTC is associated with excellent survival outcomes. Therefore, the extent of initial surgery should be based on evidence demonstrating improved locoregional control or survival while minimizing the risks and complications. Select patients with clinically involved lateral compartment lymph nodes (cN1b) may, albeit rarely, present with no evidence of central compartment lymph node metastases, on preoperative imaging or intraoperative evaluation. The purpose of this study was to determine the rate of central neck recurrence in this select group of cN1b patients who were treated without a PCND.
Methods
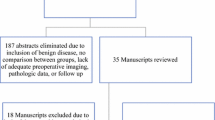
Following institutional review board approval, adult PTC patients with cN1b disease treated with a total thyroidectomy and lateral neck dissection were identified from an institutional database of 6259 patients who underwent initial surgery for well-differentiated thyroid carcinoma (WDTC) from 1986 to 2015. Patients who were < 18 years of age or with non-papillary histologies, gross extrathyroidal extension (ETE), or distant metastases at presentation were excluded from this study (Fig. 1).
For the purpose of this study, clinical nodal status was determined by preoperative imaging and intraoperative evaluation. Preoperative imaging was defined as an ultrasound, computed tomography scan, or magnetic resonance imaging scan of the neck. Intraoperative evaluation was defined as the assessment of the central compartment, based on the appearance and palpation of level 6 and 7 lymph nodes, to determine the likelihood of malignancy and subsequent need for a therapeutic central compartment neck dissection. The patient cohort in this study was comprised of patients with cN1b disease but no evidence of central compartment lymph node metastases on preoperative imaging and intraoperative evaluation. In total, 152 patients met the inclusion criteria and were classified into two groups: those who had a PCND (n = 49), and those who did not have a PCND (non-PCND; n = 103).
The definition of a central compartment neck dissection requires transparency; removal of central compartment lymph nodes was defined as a neck dissection if called such on the operation note, histology report, or at the postoperative assessment with the operating surgeon. If none of the above was found, it was termed lymph node sampling only. Central compartment lymph nodes were either sampled as a frozen-section specimen to guide the need for a central compartment neck dissection, sampled separately as part of the final histopathology specimen or incidentally identified on final histopathological review.
Clinical Endpoints
Patient and tumor characteristics were recorded for each group, as were structural recurrences within the central compartment. Patients were classified according to the 8th edition of the American Joint Committee on Cancer (AJCC) tumor node metastases (TNM) staging system and the 2015 ATA Risk-Stratification System following initial therapy.8,10
Clinical endpoints of interest included central neck recurrence-free probability (CNRFP) and disease-specific survival (DSS). All outcomes were calculated in months from the date of initial surgery. DSS was calculated to the date of final follow-up with a member of the institution’s disease management team or date of death if there was distant disease or pathology-confirmed locoregional disease at final follow-up. CNRFP was calculated to the date of final follow-up with a member of the institution’s disease management team or first structural recurrence within the central compartment, defined as within level VI or level VII cervical lymph nodes. A structural recurrence was confirmed on cyto-histopathology or detected on imaging. Findings on imaging were considered a structural recurrence if identified as “consistent with,” “suspicious for,” or “probably” a PTC metastasis; the use of these keywords on imaging reports aim to give a level of diagnostic certainty > 75.0%.
Statistical Methods
Demographic, clinical, and histopathological variables were collected for each patient. Groups were compared using Pearson’s χ2 test or Fisher’s exact test for categorical variables, and continuous variables were compared using Mann–Whitney U tests. Survival analysis was performed by the Kaplan–Meier method and differences between groups compared via log-rank tests. Outcomes were reported at 5- and 10-years from initial surgery. A p value of < 0.05 was considered statistically significant. All statistical analyses were conducted using SPSS Version 25.0 (IBM, Armonk, NY).
Results
A total of 152 PTC patients with cN1b disease were identified as having no evidence of central nodal disease on preoperative imaging or intraoperative evaluation. Patient and tumor characteristics are reported in Table 1. The median age was 49 years (range 19–79), and 57.2% were female. The majority (96.7%) of patients had ≤ 4 cm primary tumor, and 47.4% had microscopic ETE. According to the ATA risk stratification 71.7% were intermediate-risk, and 24.3% were high-risk.8 All patients were Stage I or Stage II according to the AJCC TNM staging system.10 One hundred three patients (67.8%) did not have a PCND, and 49 patients (32.2%) had a PCND.
Patients between the two groups were similar in the total number of lateral compartment lymph node metastases (p = 0.455), maximum diameter of lateral compartment lymph node metastases (p = 0.551), and number of lateral compartment lymph node levels involved (p = 0.330) (Table 2). Of the 103 non-PCND patients, 13 (12.6%) had lymph node sampling within the central compartment. Eight of the 13 patients had central nodal disease confirmed on histopathology; the median number of positive lymph node metastasis in the central compartment was one, and the median maximum diameter was 0.55 cm. Of the 49 PCND patients, 37 (75.5%) had central nodal disease confirmed on histopathology. In the PCND group, the median number of central compartment lymph nodes removed was seven.
During the study period, central neck recurrence was detected in two patients who did not receive a PCND and in three patients who received a PCND during the study period. With a median follow-up of 65 months, the 5- and 10-year estimated CNRFP was 98.4% in the non-PCND group and 93.6% in the PCND group (p = 0.133; Fig. 2). Table 3 shows the details of the five patients who had a central neck recurrence with details of extent of lateral lymph node metastases at initial surgery, use of adjuvant RAI, and final outcome.
During the study period, lateral neck recurrence was detected in seven patients who did not receive a PCND and in four patients who received a PCND. The 5- and 10-year estimated lateral neck recurrence-free probability was 93.8% and 87.8% in the non-PCND group and 91.5% and 91.5% in the PCND group (p = 0.933). During the study period, there where three disease-specific deaths in the non-PCND group, of which, none had a locoregional recurrence: one patient developed lung, bone, and brain metastases, one patient developed lung and bone metastases, and one patient developed lung metastases. There were no disease-specific deaths in the PCND group during the study period. The 5- and 10-year estimated DSS was 100.0% and 92.0% in the non-PCND group and 100.0% and 100.0% in the PCND group (p = 0.116).
Discussion
The 2015 ATA guidelines endorse the role of PCND in select PTC patients; a PCND should be considered in patients with, “advanced primary tumors…or clinically involved lateral neck nodes (cN1b).”8 In concurrence, the 2019 NCCN guidelines state a central compartment neck dissection is “required ipsilateral to a modified radical neck dissection done for clinically involved lateral neck lymph nodes in most cases.”9 PTC patients have excellent survival outcomes, with the estimated 5-year DSS > 98.0%, despite frequently metastasizing to regional cervical lymph nodes.11 Therefore, the extent of initial surgery should be based on evidence demonstrating improved locoregional control or survival outcomes. Currently, there is a scarcity of evidence to confirm the efficacy or benefit of a PCND in PTC patients.
It is universally accepted that a therapeutic central compartment neck dissection should be performed in the presence of clinically evident nodal disease. However, despite the known efficacy of a therapeutic central neck dissection, the role and benefit of a PCND in PTC patients remains controversial. In a randomized trial of 181 PTC patients, no difference in outcome was observed between patients who received a total thyroidectomy alone compared with a total thyroidectomy and PCND.12 Furthermore, multiple studies demonstrate no survival benefit for patients treated with a PCND.13,14,15
Contrary to this, some observational studies suggest a survival benefit in select PTC patients, and some retrospective studies report reduced rates of regional recurrence in patients treated with a PCND.16,17 Due to inconsistent evidence, it has been suggested that a PCND should be reserved for PTC patients who are at high risk of a central neck recurrence. The European Society of Endocrine Surgeons, ATA, and NCCN guidelines consider patients with clinically involved lateral lymph nodes as candidates for a PCND.8, 9,18 A PCND in patients with clinically involved lateral nodal disease is recommended due to the predictable stepwise fashion of lymphatic spread in PTC from the central compartment to lateral compartment. In addition, the reported rate of skip metastases, where N1b patients have no pathological central nodal disease, is low and estimated from 2.0 to 20.0% in the current literature, and 24.5% in our own study.5,6,7 There is general consensus that there is an increased likelihood of central nodal disease when lateral nodal disease is present;19 multiple studies have reported the clear association between lateral neck involvement and the likelihood of central nodal disease.20,21,22 This study reflects a very select group of PTC patients, as demonstrated in the small cohort, who in the presence of cN1b disease but no evidence of clinically involved central compartment lymph nodes, may not require a PCND.
Regional lymph node metastases have been reported to be present in up to 80.0% of PTC patients.1,2,3,4 However, much of this estimate encompasses microscopic disease, only identified on histopathological review. Furthermore, microscopic lateral nodal metastases have been reported in up to 57.5% of PTC patients when a prophylactic lateral neck dissection is performed.23 In contrast, the estimated risk of recurrence in WDTC ranges from 1.0 to 40.0%.8 Therefore, the rate of pathological nodal metastases does not correlate with the rate of regional nodal recurrence. A proportion of nodal metastases must therefore remain clinically insignificant. Thus, neither a PCND nor a prophylactic lateral neck dissection is required for all PTC patients. Furthermore, adjuvant RAI is “usually favored” in cN1b patients in accordance with the ATA guidelines;8 this may reduce the risk of regional recurrence in the central compartment and further limit the role of a PCND in this select population. In clinical practice, we try to identify patients who would be at an unacceptable risk of a central neck recurrence and would subsequently benefit from a PCND.
The potential complications of a central compartment neck dissection include injury to the parathyroid glands and recurrent laryngeal nerves, resulting in temporary or permanent hypocalcemia and hoarseness. Four of five meta-analyses comparing the complications following total thyroidectomy and central compartment neck dissection to those following total thyroidectomy alone identified a significantly higher incidence of transient hypoparathyroidism after a central compartment neck dissection.24 However, the rate of permanent hypoparathyroidism, as well as temporary or permanent recurrent laryngeal nerve injury, was not statistically different between the two groups.24 The reported incidence of transient hypocalcemia following total thyroidectomy alone is estimated from 8.3 to 36.5% compared with 23.2–51.9% in patients managed with total thyroidectomy and neck dissection.25 One might argue that given the relatively low morbidity of a PCND, it should be routinely performed. However, at our institution, the extent of initial surgery is determined by oncological benefit.
The management of cervical lymph node metastases in PTC at our institution is guided by the clinical nodal status, which is determined by physical examination, preoperative imaging, and intraoperative evaluation. A compartment-orientated neck dissection is performed in the presence of clinical nodal disease. The need for a PCND is reserved to the judgment of the operating surgeon in patients with gross ETE or clinically involved lateral nodal disease. The extent of lateral nodal disease is an influencing factor when determining the benefit of a PCND; in general, patients with bulky lateral nodal disease involving multiple or large metastatic lymph nodes are considered for a PCND. Furthermore, frozen sections are frequently used at our institution to guide the management of the central compartment; during intraoperative evaluation, frozen sections are performed on suspicious lymph nodes in the central compartment to determine the need for a neck dissection.
Not all patients with cervical lymph node metastases carry the same prognostic significance.26 Multiple studies have reported that the risk of recurrence in pN1 PTC patients depends on the number, size, and extranodal extension status of the nodal metastases.4 In our study, 103 patients with cN1b disease did not have a PCND, and only 2 patients in this cohort had developed a central neck recurrence by final follow-up; the 5- and 10-year CNRFP was 98.4%. One might predict that patients with small-volume lateral nodal disease would be at lesser risk of a central neck recurrence. Interestingly, there was no difference in the number of levels involved in the lateral neck, total number of lateral lymph node metastases, or maximum diameter of lateral lymph node metastases between the non-PCND and PCND groups.
The ATA and NCCN guidelines endorse the use of preoperative ultrasound in the assessment of the central and lateral cervical compartments.8,9 Performing an ultrasound is operator-dependent. Consequently, the evidence behind the value of preoperative ultrasound is variable. It is well-recognized that preoperative ultrasound can miss clinical nodal disease; a meta-analysis found preoperative ultrasound to have a sensitivity of 70.0% in the detection of lymph node metastasis.27 Even if a metastatic lymph node is identified on preoperative imaging, there may be a discrepancy between the level or compartment it is classified as on imaging compared with on intraoperative evaluation.
Surgeons were previously thought to be poor at detecting nodal metastasis intraoperatively.28 However, we believe that the decision to perform a central compartment neck dissection relies on the judgement of the surgeon, based on physical examination, preoperative imaging, and intraoperative evaluation. Using this triad of information will compensate for the weaknesses of each investigation individually. Our study suggests that in the absence of central compartment lymph node metastases on preoperative imaging and intraoperative evaluation, select cN1b patients may not benefit from a PCND.
Limitations
As a retrospective study, individual surgeon preference and subsequent selection bias cannot be excluded. In addition, during the 30-year study period, the quality and efficacy of preoperative imaging has significantly improved. Missed detection and localization of lymph node metastases is increasingly rare, and imaging is reliably used to guide the extent of surgery at our institution. Furthermore, we would like to emphasize that given the predictability of regional lymph node metastases; the vast majority of PTC patients with cN1b disease will require a therapeutic central compartment neck dissection.
Our approach to monitoring patients postoperatively has progressed during the study period. During the first 20 years studied, most recurrences were detected clinically rather than sonographically. The use of serial ultrasound and thyroglobulin measurements to detect recurrent disease were introduced at our institution in 2000. Since 2005, they have been used as part of a standardized follow-up protocol. Furthermore, it may take several years or even decades for microscopic nodal disease to become clinically significant; therefore, the median follow-up of 65 months in this study is a significant limitation of this study.
Conclusions
Select PTC patients with cN1b disease but no evidence of clinically involved central compartment lymph nodes, on preoperative imaging and intraoperative evaluation, appear to have a low rate of central neck recurrence. These patients may not benefit from a PCND.
References
Pereira JA, Jimeno J, Miquel J, et al. Nodal yield, morbidity, and recurrence after central neck dissection for papillary thyroid carcinoma. Surgery. 2005;138(6):1095–100.
Salter KD, Andersen PE, Cohen JI, et al. Central nodal metastases in papillary thyroid carcinoma based on tumor histologic type and focality. Arch Otolaryngol Head Neck Surg. 2010;136(7):692–6.
Thompson AM, Turner RM, Hayen A, et al. A preoperative nomogram for the prediction of ipsilateral central compartment lymph node metastases in papillary thyroid cancer. Thyroid. 2014;24(4):675682.
Randolph GW, Duh QY, Heller KS, et al. The prognostic significance of nodal metastases from papillary thyroid carcinoma can be stratified based on the size and number of metastatic lymph nodes, as well as the presence of extranodal extension. Thyroid. 2012;22(11):1144–52.
Roh JL, Park JY, Rha KS, Park CI. Is central neck dissection necessary for the treatment of lateral cervical nodal recurrence of papillary thyroid carcinoma? Head Neck. 2007;29(10):901–6.
Wada N, Duh QY, Sugino K, et al. Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg. 2003;237(3):399–407.
Lee YS, Shin SC, Lim YS, et al. Tumor location-dependent skip lateral cervical lymph node metastasis in papillary thyroid cancer. Head Neck. 2014;36(6):887–91.
Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26(1):1–133.
National Comprehensive Cancer Network. NCCN clinicial practice guidelines in oncology—thyroid carcinoma. https://www.nccn.org/. Accessed 20 April 2019.
Amin MB, Edge SB, Greene FL, et al. AJCC cancer staging manual. 8th ed. New York: Springer; 2017.
National Cancer Institute. Surveillance, epidemiology, and end results program (SEER): thyroid cancer. https://seer.cancer.gov/statfacts/html/thyro.html. Accessed 19 Jan 2019.
Viola D, Materazzi G, Valerio L, et al. Prophylactic central compartment lymph node dissection in papillary thyroid carcinoma: clinical implications derived from the first prospective randomized controlled single institution study. J Clin Endocrinol Metab. 2015;100(4):1316–24.
Toniato A, Boschin I, Casara D, Mazzarotto R, Rubello D, Pelizzo M. Papillary thyroid carcinoma: factors influencing recurrence and survival. Ann Surg Oncol. 2008;15(5):1518–22.
Bardet S, Malville E, Rame JP, et al. Macroscopic lymph-node involvement and neck dissection predict lymph-node recurrence in papillary thyroid carcinoma. Eur J Endocrinol. 2008;158(4):551–60.
Leboulleux S, Rubino C, Baudin E, et al. Prognostic factors for persistent or recurrent disease of papillary thyroid carcinoma with neck lymph node metastases and/or tumor extension beyond the thyroid capsule at initial diagnosis. J Clin Endocrinol Metab. 2005;90(10):5723–29.
Barczynski M, Konturek A, Stopa M, Nowak W. Prophylactic central neck dissection for papillary thyroid cancer. Br J Surg. 2013;100(3):410–8.
White ML, Gauger PG, Doherty GM. Central lymph node dissection in differentiated thyroid cancer. World J Surg. 2007;31(5):895–904.
Sancho JJ, Lennard TW, Paunovic I, Triponez F, Sitges-Serra A. Prophylactic central neck disection in papillary thyroid cancer: a consensus report of the European Society of Endocrine Surgeons (ESES). Langenbecks Arch Surg. 2014;399(2):155–63.
Gimm O, Rath FW, Dralle H. Pattern of lymph node metastases in papillary thyroid carcinoma. Br J Surg. 1998;85(2):252–4.
Stack BC, Jr, Ferris RL, Goldenberg D, et al. American thyroid association consensus review and statement regarding the anatomy, terminology, and rationale for lateral neck dissection in differentiated thyroid cancer. Thyroid. 2012;22(5):501–8.
Machens A, Hauptmann S, Dralle H. Lymph node dissection in the lateral neck for completion in central node-positive papillary thyroid cancer. Surgery. 2009;145(2):176–81.
Roh JL, Kim JM, Park CI. Lateral cervical lymph node metastases from papillary thyroid carcinoma: pattern of nodal metastases and optimal strategy for neck dissection. Ann Surg Oncol. 2008;15(4):1177–82.
Mulla MG, Knoefel WT, Gilbert J, McGregor A, Schulte KM. Lateral cervical lymph node metastases in papillary thyroid cancer: a systematic review of imaging-guided and prophylactic removal of the lateral compartment. Clin Endocrinol Oxf. 2012;77(1):126–31.
Chisholm EJ, Kulinskaya E, Tolley NS. Systematic review and meta-analysis of the adverse effects of thyroidectomy combined with central neck dissection as compared with thyroidectomy alone. Laryngoscope. 2009;119(6):1135–9.
Ardito G, Revelli L, Polistena A, et al. Complications of neck dissections in papillary thyroid carcinoma: a modified procedure to reduce parathyroid morbidity. In Vivo. 2016;30(3):303–8.
Urken ML, Haser GC, Likhterov I, Wenig BM. The impact of metastatic lymph nodes on risk stratification in differentiated thyroid cancer: have we reached a higher level of understanding? Thyroid. 2016;26(4):481–8.
Wu LM, Gu HY, Qu XH, et al. The accuracy of ultrasonography in the preoperative diagnosis of cervical lymph node metastasis in patients with papillary thyroid carcinoma: a meta-analysis. Eur J Radiol. 2012;81(8):1798–805.
Ji YB, Lee DW, Song CM, Kim KR, Park CW, Tae K. Accuracy of intraoperative determination of central node metastasis by the surgeon in papillary thyroid carcinoma. Otolaryngol Head Neck Surg. 2014;150(4):542–7.
Acknowledgement
Funding support: This research was funded in part through the NIH/NCI Cancer Center Support Grant, P30 CA008748.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
No competing financial or personal interests exist for the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Harries, V., McGill, M., Wang, L.Y. et al. Is a Prophylactic Central Compartment Neck Dissection Required in Papillary Thyroid Carcinoma Patients with Clinically Involved Lateral Compartment Lymph Nodes?. Ann Surg Oncol 28, 512–518 (2021). https://doi.org/10.1245/s10434-020-08861-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08861-4