Abstract
Background
Mixed adeno-neuroendocrine carcinoma (MANEC) is a rare pathologic diagnosis recently defined by the World Health Organization in 2010. Due to poor understanding of MANEC as a clinical entity, there is significant variation in the management of these patients. The purpose of our study was to characterize MANEC to develop evidence-based treatment strategies.
Methods
The Ohio State University patient database was queried for the diagnosis of MANEC and 46 patients were identified. For comparison, the database also was queried for goblet cell carcinoid (GCC) of the appendix, signet ring cell carcinoma, and carcinoid/neuroendocrine tumor of the appendix. Charts were then retrospectively reviewed for clinicopathologic characteristics, patient treatment, and survival data.
Results
The mean age of diagnosis of MANEC was 54 years. Eighty-seven percent of MANEC arose from the appendix, with 28 % of patients undergoing appendectomy and 35 % undergoing right hemicolectomy as their index operation. Immunohistochemical staining was positive for chromogranin (82 %), synaptophysin (97 %), and CD56 (67 %). Sixty-seven percent of patients presented with stage IV disease and 41 % had nodal metastases. Overall survival was 4.1 years, which was statistically significantly different (p ≤ 0.05) compared with carcinoid tumors (13.4 years), GCC (15.4 years), and signet ring carcinoma (2.2 years).
Conclusions
MANEC is a more aggressive clinical entity than both GCC of the appendix and carcinoid/neuroendocrine tumors of the appendix. Based on these findings, we recommend patients with MANEC tumors undergo aggressive multidisciplinary cancer management and close surveillance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Mixed adeno-neuroendocrine carcinoma (MANEC) is a rare pathologic diagnosis, which was recently defined by the World Health Organization (WHO) in 2010 as tumors with both epithelial and neuroendocrine cells, and each component represents at least 30 % of the tumor.1 Previously, the WHO defined tumors with both adenocarcinoma and neuroendocrine components as mixed exocrine–endocrine tumors.1 In addition, to diagnose MANEC, two of the three commonly used neuroendocrine markers, synaptophysin, chromogranin, and CD56, must be present.1 , 2
Prior to definition by the WHO, mixed tumors were given many different pathologic designations, including goblet cell carcinoid (GCC), adenocarcinoma ex-GCC, composite tumors, adenocarcinoid, collision tumors, and mixed endocrine–exocrine tumors.3 – 6 Multiple pathologic definitions led to inconsistent reporting in the literature, making it difficult to characterize the disease. Evidence is conflicting regarding the prognosis for patients with MANEC; some studies suggest that the prognosis between colorectal MANEC and neuroendocrine tumors are comparable, whereas others indicate that MANEC may represent a more aggressive clinical entity.7 – 9 Thus, it is unclear whether MANEC is more biologically similar to their neuroendocrine or adenocarcinoma counterparts. With the WHO classification of MANEC and its recognition as a distinct clinical entity, understanding the natural history and prognosis of MANEC is of utmost importance to ensure improved patient outcomes.
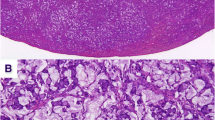
Previous attempts have been made to categorize MANEC to aid in clinical decision-making. La Rosa et al. divided MANEC into high, intermediate, and low-grade tumors. Low-grade tumors were classified as mixed adenocarcinoma-neuroendocrine tumors.10 High-grade tumors usually have a high Ki-67 proliferation index, which can be associated with more aggressive tumors and worse survival.11 , 12 By immunohistochemistry, high-grade tumors stain diffusely for synaptophysin and to a lesser extent, chromogranin. In low-grade MANEC, the exocrine component of the tumor often is more aggressive than the neuroendocrine component.
To date, data and literature aside from case series and case reports regarding MANEC are limited; therefore, it remains not well understood. The purpose of this study was to report our findings with MANEC to better characterize the biology of the disease and thus develop evidence-based treatment strategies.
Materials and Methods
After protocol approval by the Ohio State University (OSU) Wexner Medical Center Institutional Review Board, the pathology database was queried for all patients with the pathologic diagnosis of “mixed adeno-neuroendocrine carcinoma” in the gastrointestinal (GI) tract from January 1990 to December 2014. In order to be considered MANEC, the tumor specimens had to have at least 30 % non-neuroendocrine tissue, consistent with the WHO classification. Cases included both specimens obtained from surgical procedures performed at the OSU, in addition to pathology specimens referred to the OSU Department of Pathology in consultation. OSU pathologists reviewed all specimens and confirmed the diagnosis. Based on these criteria, 46 patients were identified. Mean follow-up time was 1.6 years (range 28 days–8.1 years).
For comparison, the OSU Pathology database also was queried for patients with the diagnosis of GCC of the appendix (n = 15), signet ring cell carcinoma of the appendix (n = 18), and carcinoid/neuroendocrine tumor of the appendix (n = 97). Of note, signet ring cell carcinoma was defined as those tumors that had >50 % signet ring cells, consistent with the WHO classification.13
Charts were retrospectively reviewed for demographic data, including age at diagnosis, race, and gender. Tumor and patient characteristics were reviewed, including location of primary tumor, immunohistochemical markers, stage at diagnosis, treatment regimens, and survival.
Statistical Analysis
Demographics, tumor characteristics, and immunohistochemical markers were summarized using descriptive statistics (median/range for continuous outcomes, and frequency for categorical outcomes) for each group, respectively. Fisher’s exact test was used to the categorical outcomes among the groups, and Kruskal–Wallis test was used for the continuous outcomes. Overall survival (OS) was calculated from the date of diagnosis to death from any cause. Patients who were still alive were censored at the date of last visit. Survival curves were estimated using the method of Kaplan–Meier. Survival curves were compared between groups using log-rank test. Bonferroni method was used to adjust for multiple comparisons. Estimated median with 95 % confidence intervals (CIs) were provided. p < 0.05 were considered statistically significant. All statistical analyses were conducted using SAS version 9.3 (SAS Institute, Cary, NC).
Results
The demographic data for patients with MANEC, GCC, signet ring carcinoma, and carcinoid/neuroendocrine carcinoma are summarized in Table 1. For MANEC, the mean age of diagnosis was 54 (range 19–79) years. There was a greater proportion of female–male patients: 30 (65 %) and 16 (35 %), respectively. There were no statistically significant differences in gender (p = 0.25) or race (p = 0.76) between MANEC, carcinoid/neuroendocrine, GCC, and signet ring carcinoma. There was a statistically significant difference between mean ages of diagnosis (p = 0.0002). Patients with MANEC tended to be older (mean 54 years) than those with carcinoid tumors (mean 42 years) and GCC (mean 47 years), and similar in age to signet ring cell carcinoma (mean 53 years).
Many patients and their pathology slides were sent as referrals to OSU with pathologic diagnosis of MANEC based on existing outside immunohistochemical staining, and additional immunohistochemical stains were only performed if clinically necessary to confirm the diagnosis. Hence, all three neuroendocrine markers were not performed on most patients. Of the patients who underwent immunohistochemical staining, chromogranin, synaptophysin, and CD56 were present in 82, 97, and 67%, respectively. Other tumor markers that were present more than 50 % of the time included cytokeratin AE1/AE3, cytokeratin 7 (CK7), CK20, and CDX2. A complete summary of the MANEC immunohistochemical profile is listed in Table 2. Nineteen patients (49 %) had nodal metastases, 16 (80 %) had perineural invasion, and 9 (47 %) had vascular invasion (Table 3). A complete description of tumor characteristics can be found in Table 3. Similar to the immunohistochemical data, data about tumor characteristics is incomplete. The majority of MANECs arose from the appendix, 40 (87 %), and were incidentally found at the time of appendectomy usually for acute appendicitis. The remaining MANEC tumors arose in the duodenum, small bowel, colon, and one patient had an unknown GI primary (Table 3).
There was significant variability in the way the patients with appendiceal tumors were managed; 13 (33 %) patients initially underwent simple appendectomy and 13 (33 %) patients had right hemicolectomy (RHC) as their index operation (Table 4). Of the patients who had an appendectomy as their initial operation, 7 (54 %) had a subsequent RHC after index pathology review. Of the patients who had RHC following initial appendectomy, two had nodal metastases. The size of the tumor did not seem to determine whether patients underwent subsequent RHC after appendectomy, because tumors greater than or less than 2 cm had RHC. Two patients only had surgical biopsies without tumor resection due to peritoneal disease at the time of presentation.
Surgical intervention for metastatic recurrent disease was performed for two patients. Records showed that two patients initially had simple appendectomy but then had disease recurrence. One patient had cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (HIPEC) for peritoneal disease, and another patient had pelvic debulking with total abdominal hysterectomy, bilateral oophorectomy, and appendectomy followed by systemic chemotherapy. However, she later developed metastatic disease to the spine. Following surgery, 31 (67 %) patients received chemotherapy. Of the 31 patients, 23 (74 %) received chemotherapy in the setting of stage IV metastatic disease (Table 4).
At the time of diagnosis, 31 (67 %) MANEC patients were diagnosed with stage IV disease, and 27 patients had appendiceal only tumors. In comparison, no patients with GCC, 10 % of carcinoid tumors, and 94 % of signet ring tumors had stage IV disease at the time of diagnosis. The OS for MANEC patients was 4.1 years (95 % CI 1.9-not reached). This was statistically significantly different compared with the OS in patients with well-differentiated neuroendocrine tumor/carcinoid (13.2 years, 95 % CI 7.4-not reached, p = 0.007) but not statistically different from GCC (15.2 years, 95 % CI 7.4–15.2, p = 0.52) and signet ring cell carcinoma (2.2 years, 95 % CI 0.8–2.8, p = 0.07; Fig. 1). The OS for stage IV appendiceal only MANEC (NR, 95 % CI 1.5 months-not reached) was statistically significantly different compared with stage IV appendiceal carcinoid (13.2 months, 95 % CI 2.3-not reached) and signet ring (2.0 months, 95 % CI 0.2–2.3). Notably, for the appendiceal only stage IV MANEC patients, 20 of the 27 patients were still alive at the time of this study and the median months survival was not reached. There were no stage IV GCC; therefore, GCC was excluded from this portion of the analysis (Fig. 2).
Discussion
There is significant variability in the way that MANEC tumors of the appendix have been managed secondary to variability in diagnostic criteria leading to poor characterization of the disease. Prior to their distinction from GCCs and carcinoid/neuroendocrine tumors of the appendix, appendiceal MANECs often were treated similarly to their less aggressive counterpart, carcinoid tumors. Based on our study, MANEC, particularly appendiceal MANECs, may represent a more aggressive histology that requires a different treatment strategy than that of neuroendocrine tumors. In our study, the OS for patients with MANEC is 4.1 years, which is shorter than that of GCC and carcinoid tumors of the appendix. Additionally, 67 % of patients had stage IV disease and 49 % had nodal metastases at time of diagnosis. In contrast, La Rosa et al. found that there was no statistically significant difference in survival between neuroendocrine carcinoma and colorectal MANEC patients. Additionally, they found only 17 % of patients had stage IV disease at the time of diagnosis. This difference in survival and rates of metastatic disease between our study and theirs may be related to the different sample size in our two studies. In our study, the majority of cases was appendiceal MANEC. La Rosa et al. included 12 MANEC, 8 from right colon and 4 left colon, whereas we had 46 patients, 40 of which were appendiceal. They did find that vascular invasion, peritumoral lymphoid infiltrate, and presence of CD117 in the MANEC tumors had a statistically significant association with worse survival. Similar to our study, La Rosa et al. also found that the majority (>50 %) of MANEC tumors stain for both chromogranin and synaptophysin, but there were differing rates of lymphatic invasion (92 vs. 48.7 %), vascular invasion (92 vs. 47.4 %), and perineural invasion (92 vs. 80 %) between La Rosa and our study, respectively.7
Based on our analysis, there was no statistically significant difference in OS between MANEC tumors and signet ring carcinoma (p = 0.068) as well as with GCC (p = 0.51), but statistically significant longer OS for carcinoid (p = 0.007). This finding may suggest that while MANEC tumors are a separate pathological entity from signet ring carcinoma, they are similarly aggressive tumors and require more aggressive management than carcinoid tumors of the appendix.
Appendiceal carcinoid/neuroendocrine tumors have generally been regarded to be less aggressive tumors as they uncommonly present with metastatic disease.14 Overall 1- and 5-year survivals are reported as high as 98.1 and 88.7 %, respectively, and some studies have shown 10-year survival rates to be as high as 91 % in patients with tumors >2 cm with positive lymph nodes.15 – 17 Tumors less than 2 cm warrants appendectomy alone.18 This is considered a curative procedure with a limited role for postoperative surveillance assuming no other adverse features.19 Interestingly, due to lack of understanding of atypical histologies and adequate prognostic indicators, the NCCN does recommend that appendiceal tumors with mixed histology be treated similar to colon cancer.20
On the other hand, GCCs of the appendix have been regarded to be more aggressive than their carcinoid counterparts when considering age of diagnosis, the extent of disease spread at diagnosis and the number of cases with lymph node involvement.21 Additionally, signet ring cell carcinoma of the appendix is a rare clinical entity and is felt to be more aggressive than both GCC and carcinoid/neuroendocrine tumors. According to McCusker et al., 76 % of patients with signet ring cell carcinoma present with metastatic disease and 64 % have node-positive disease. In comparison, 31 and 14 % of patients with well-differentiated carcinoid and GCC, respectively, present with stage IV disease.21
There are several limitations associated with this study design to acknowledge. This study was undertaken in a retrospective fashion from a single-institution database. Given the study institution is a comprehensive cancer center and tertiary care center, there is potential for referral bias as well as selection bias playing a role in the patient data and treatments undertaken. Subgroup analyses are generally limited by increased error rates and lower power such that conclusions drawn require careful interpretation. Due to this being an uncommon entity with the resulting small sample size, this may explain the finding of the subgroup analysis that showed 20 of the 27 patients with stage IV appendiceal MANEC were alive at the time of this study and median survival not yet reached in light of a short median follow-up period of only 1.6 years. Additionally, there may be lead-time bias when analyzing MANEC patients, because they were diagnosed later. For MANEC, two patients were diagnosed in 1996 and 2000, and the remaining patients were diagnosed in 2008–2014. For GCC, signet ring, and carcinoid/neuroendocrine tumors, dates of diagnosis spanned 1990–2014 fairly evenly. Other limitations include incomplete pathologic analysis due to the fact that many of the tumor specimens were outside referrals. Despite these limitations, this study is the largest, retrospective review of MANEC.
Based on our findings, appendiceal MANEC is an aggressive entity with a significant proportion of patients presenting with stage IV disease. Unlike carcinoid tumors, tumor size does not appear to have any prognostic significance, because both small (<1 cm) and large (>10 cm) tumors presented with stage IV disease without evidence of metastasis after several years follow-up. Therefore, it is paramount to distinguish appendiceal MANEC from the other appendiceal histologies due to the association of an aggressive disease biology demonstrated with MANEC in this study.
We recommend that patients with MANEC undergo aggressive multidisciplinary oncologic management, which may include systemic therapy and well-selected surgical management with RHC as well as possible cytoreductive surgery with HIPEC in patients with peritoneal metastases. Additional studies are required to define more conclusively the optimal management for MANEC to achieve improved patient outcomes.
References
Komminoth PA, Capella C, Klimstra DS, Klöppel G, Solcia E, Rindi G. Neuroendocrine neoplasms of the appendix. In: WHO classification of tumours of the digestive system. 4th ed. Lyon: IARC Press; 2010.
Rindi G, Bordi C, La Rosa S, et al. Gastroenteropancreatic (neuro)endocrine neoplasms: the histology report. Dig Liver Dis. 2011;43 Suppl 4:S356–60.
Lewin K. Carcinoid tumors and the mixed (composite) glandular-endocrine cell carcinomas. Am J Surg Pathol. 1987;11 Suppl 1:71–86.
Capella C, La Rosa S, Uccella S, Billo P, Cornaggia M. Mixed endocrine–exocrine tumors of the gastrointestinal tract. Semin Diagn Pathol. 2000;17(2):91–103.
Holt N, Gronbaek H. Goblet cell carcinoids of the appendix. Sci World J. 2013;2013:543696–702.
Roy P, Chetty R. Goblet cell carcinoid tumors of the appendix: an overview. World J Gastrointest Oncol. 2010;2(6):251–8.
La Rosa S, Marando A, Furlan D, Sahnane N, Capella C. Colorectal poorly differentiated neuroendocrine carcinomas and mixed adenoneuroendocrine carcinomas: insights into the diagnostic immunophenotype, assessment of methylation profile, and search for prognostic markers. Am J Surg Pathol. 2012;36(4):601–11.
Power DG, Asmis TR, Tang LH, Brown K, Kemeny NE. High-grade neuroendocrine carcinoma of the colon, long-term survival in advanced disease. Med Oncol. 2011;28 Suppl 1:S169–74.
Shia J, Tang LH, Weiser MR, et al. Is nonsmall cell type high-grade neuroendocrine carcinoma of the tubular gastrointestinal tract a distinct disease entity? Am J Surg Pathol. 2008;32(5):719–31.
La Rosa S, Marando A, Sessa F, Capella C. Mixed adenoneuroendocrine carcinomas (MANECs) of the gastrointestinal tract: an update. Cancers. 2012;4(1):11–30.
Scholzen T, Gerdes J. The Ki-67 protein: from the known and the unknown. J Cell Physiol. 2000;182(3):311–22.
Lowe K, Khithani A, Liu E, et al. Ki-67 labeling: a more sensitive indicator of malignant phenotype than mitotic count or tumor size? J Surg Oncol. 2012;106(6):724–7.
Hamilton SR, Aaltonen LA, (eds.). World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of the Digestive System. Lyon: IARC Press; 2000.
Goede AC, Caplin ME, Winslet MC. Carcinoid tumour of the appendix. Br J Surg. 2003;90(11):1317–22.
Nussbaum DP, Speicher PJ, Gulack BC, et al. Management of 1- to 2-cm carcinoid tumors of the appendix: using the national cancer data base to address controversies in general surgery. J Am Coll Surg. 2015;220(5):894–903.
Mullen JT, Savarese DM. Carcinoid tumors of the appendix: a population-based study. J Surg Oncol. 2011;104(1):41–4.
Benedix F, Reimer A, Gastinger I, et al. Primary appendiceal carcinoma—epidemiology, surgery and survival: results of a German multi-center study. Eur J Surg Oncol. 2010;36(8):763–71.
Moertel CG, Weiland LH, Nagorney DM, Dockerty MB. Carcinoid tumor of the appendix: treatment and prognosis. N Engl J Med. 1987;317(27):1699–701.
Murray SE, Lloyd RV, Sippel RS, Chen H, Oltmann SC. Postoperative surveillance of small appendiceal carcinoid tumors. Am J Surg. 2014;207(3):342–5; discussion 345.
Kulke MH, Shah MH, Benson AB, et al. Neuroendocrine tumors, version 1.2015. J Natl Compr Canc Netw. 2015;13(1):78–108.
McCusker ME, Cote TR, Clegg LX, Sobin LH. Primary malignant neoplasms of the appendix: a population-based study from the surveillance, epidemiology and end-results program, 1973–1998. Cancer. 2002;94(12):3307–12.
Disclosures
The authors have no disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brathwaite, S., Rock, J., Yearsley, M.M. et al. Mixed Adeno-neuroendocrine Carcinoma: An Aggressive Clinical Entity. Ann Surg Oncol 23, 2281–2286 (2016). https://doi.org/10.1245/s10434-016-5179-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5179-2