Abstract
Lung cancer is one of the most severe lethal malignancies, with approximately 1.6 million deaths every year. Lung cancer can be broadly categorised into small and non-small-cell lung cancer. The traditional chemotherapy is nonspecific, destroys healthy cells and produces systemic toxicity; targeted inhalation drug delivery in conjunction with nanoformulations has piqued interest as an approach for improving chemotherapeutic drug activity in the treatment of lung cancer. Our aim is to discuss the impact of polymer and lipid-based nanocarriers (polymeric nanoparticles, liposomes, niosomes, nanostructured lipid carriers, etc.) to treat lung cancer via the inhalational route of drug administration. This review also highlights the clinical studies, patent reports and latest investigations related to lung cancer treatment through the pulmonary route. In accordance with the PRISMA guideline, a systematic literature search was carried out for published works between 2005 and 2023. The keywords used were lung cancer, pulmonary delivery, inhalational drug delivery, liposomes in lung cancer, nanotechnology in lung cancer, etc. Several articles were searched, screened, reviewed and included. The analysis demonstrated the potential of polymer and lipid-based nanocarriers to improve the entrapment of drugs, sustained release, enhanced permeability, targeted drug delivery and retention impact in lung tissues. Patents and clinical observations further strengthen the translational potential of these carrier systems for human use in lung cancer. This systematic review demonstrated the potential of pulmonary (inhalational) drug delivery approaches based on nanocarriers for lung cancer therapy.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
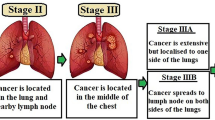
Cancer remains the world’s leading cause of death due to the uncontrolled growth and spread of malignant cells [1]. With approximately 1.6 million fatalities each year, lung cancer is one of the most fatal cancers in the world, among others, like colon, breast and prostate [2, 3]. Lung cancer patients continue to have a poor prognosis, even though its treatment has vastly progressed in the past 50 years. Lung cancer can be caused by a variety of environmental and genetic variables, as well as their interactions. According to the histology of the tumour tissue, there are two forms of lung cancer: small (SCLC) and non-small-cell lung cancer (NSCLC), which are further split into adenocarcinoma, large cell carcinoma and squamous cell carcinoma [4, 5].
SCLC constitutes ~ 15% of all types of lung cancer, which have a very high proliferative rate, a significant propensity for early metastasis, and a poor prognosis [6]. SCLC patients have a poor prognosis, with few years of survival rate (< 5%) and an average total survival time of just 2–4 months for those who are not getting active therapy [7]. NSCLC is the most common type of lung cancer that is less susceptible to treatment than SCLC and accounts for about 85% of all lung malignancies. NSCLC originates from the epithelial cells of the lung placed in the interior bronchi to terminal alveoli [8].
In recent years, the understanding and therapeutic approaches to lung cancer have been improved significantly. The treatment plan is generally determined by the kind and pathological stage of lung cancer. Despite substantial growth in lung cancer treatment to date, anticancer treatment efficiency in different individuals remains poor [9]. In most treatment approaches, non-localized drug administration has a low success rate and poor clinical efficacy; most of the chemotherapeutic medications are taken by the traditional route (i.e. oral or parenteral). As a result, targeted inhalation medication administration has piqued interest as an approach for improving chemotherapeutic drug activity in the management of lung cancer [10].
The pulmonary or inhalational route of treatment leads to rapid systemic absorption without the complications associated with parenteral forms of administration. In addition, clinical and preclinical research is continuing to look into using the pulmonary route of administration to treat cancer and infectious disorders [11]. There are three types of devices that are used to deliver medications to the lungs: metered dose inhalers (MDIs), nebulizers and dry powder inhalers (DPIs). Each of these systems uses a distinct principle to transport aerosols and the chemistry that corresponds to the product differs greatly [12].
Additionally, conventional chemotherapy is nonspecific in terms of targeting drugs to lung cancer cells, which also distributes and causes harm to healthy cells and results in systemic toxicity in patients [13]. Some of the conventional lung cancer treatments, as well as their mechanisms of action and common adverse effects, are summarised in Table I. Hence, the need for alternative treatment methods still exists. One of the most common ways is nanocarrier-based drug delivery. Drug nanocarriers are colloidal carrier systems with submicron particle sizes of less than 500 nm [19]. Nano-scaled drug carriers have received increased interest in comparison to free pharmaceuticals because of their capacity to alter pharmacokinetics (enhanced permeability), sustained release, improved stability, and decreased toxicities [20, 21].
In recent years, many polymer and lipid-based nanocarriers have been developed and evaluated to enhance the drug loading and release features of anticancer medications used to treat lung cancer [22]. For example, bromo-noscapine nanoemulsions [23], paclitaxel liposomes [24], docetaxel-nanoemulsion [25], docetaxel-baicalin solid lipid nanoparticle [26], gemcitabine-paclitaxel nanostructured lipid carrier, etc. [27] showed increased therapeutic activity in the management of lung cancer. For the management of lung cancer, this study summarises the many elements of pulmonary drug administration based on nanocarriers (such as microparticles, nanoparticles, dendrimers, liposomes, niosomes, nanoemulsions and solid lipid nanoparticles) through a description of preclinical and pharmaceutical characteristics. This paper describes the impact of different types of nanocarriers on lung cancer treatment in detail. This study also includes information on the latest investigations performed, clinical studies and patent reports related to pulmonary drug delivery based on nanocarriers for lung cancer management.
Methods
Literature Search Methodology and Selection Criteria
The Scopus, Springer, Elsevier, Science Direct, Bentham Science, Taylor and Francis, and PubMed electronic databases were searched for articles published between 2005 and 2023. PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) standard guidelines were followed when performing the literature search. The terms lung cancer, pulmonary drug delivery, nanocarriers were used to search the data based on inclusion criteria. Reviews and study reports with insufficient data, however, were not included. For further research, the references from the included papers and reviews were examined.
Data Screening and Analysis
Initially, 354 studies were identified, out of which 242 records were excluded on the basis of different reasons (Fig. 1). After this, 112 full-text publications were analysed for inclusion after the screening of the data, using a pre-specified format that takes into account the source, article title and reported characteristics, methodologies, anticancer potential and key outcomes. Figure 1 shows the method utilised for the selection and screening of articles.
Results and Discussion
According to the research’s findings, of the 112 included articles, 35 dealt with the nanocarrier-mediated pulmonary drug delivery in the treatment of lung cancer, and 77 dealt with the important aspects of pulmonary drug delivery based on nanocarriers, patents, and clinical trials associated with the lung cancer therapy.
Important Aspects of Inhalational (Pulmonary) Drug Delivery
Pulmonary drug delivery involves inhaling medication into the lungs, where it passes through the alveolar epithelium and into the bloodstream. Pulmonary drug delivery is a non-invasive alternative to the injectable route of drug administration. The ability to employ a relatively low dose, a low incidence of systemic adverse effects, and for some medications, a quick commencement of action is all benefits of pulmonary administration [28, 29].
In addition to eliminating carbon dioxide and returning it to the lungs for emission, the respiratory system functions in tandem with the cardiovascular system to transport oxygen from the lungs to different cells in the body. The process of breathing involves transferring oxygen and carbon dioxide from the air, blood and tissues of the body. Roughly 12–15 times each minute, a healthy lung takes in approximately 1 pint of air. Every minute, all the blood from different parts of the body passes through the lungs. The whole respiratory tract is divided into two divisions: the upper respiratory tract (includes throat, nose and nasal cavity) and the lower respiratory tract (includes lungs, larynx, trachea and bronchi) [30].
The lungs are very sensitive to disorders/diseases caused by hereditary factors, infections and pollution, and the whole respiratory system is vulnerable to a number of diseases. Asthma, bronchiolitis, COPD, cystic fibrosis, lung cancer, pneumonia and pulmonary hypertension are the major causes that create problems in the functioning of the lungs [31].
Particles enter the lungs by three routes: impaction, sedimentation, and diffusion. Because of curvature and decreasing air velocity, particles travelling through the respiratory system are subjected to continually changing forces [32]. The mechanism of inertial impaction deposits the biggest particles in the pharynx and early bifurcations. The minute particles remain travelling to the central lung (sedimentation), where the air velocity eventually drops to much lower levels. The optimal particle size for inhalation therapy ranges from 1 to 5 µm, depending on the targeted area [33]. Particles entering the respiratory system may vary not only in size and velocity but also in shape and density, depending on the kind of drug and the inhalation mechanism used for aerosol production [34].
The devices used to administer therapeutic agents to the lungs are classified into three types: MDIs, DPIs, and nebulizers. The mentioned systems operate on a distinct principle, and the performance associated with the result differs greatly between them [35]. MDIs are devices that release a set dose of medicine with each pulse and are used to deliver aerosolized pharmaceuticals. The drug is generally administered at a high velocity (> 30 m/s via the mouthpiece) in the form of particulate systems with a mass median aerodynamic diameter of ~ 2–4 µm. The purpose of DPIs was to eliminate MDI’s inherent coordination difficulties. DPIs do not require the administration of propellants, making them more ecologically friendly, and many of them have a dose left indicator. DPIs, unlike MDIs, do not need synchronization during actuation and breathing. DPIs require high rates of inspirations (generally ≥ 60 L/min) to guarantee effective de-agglomeration of powders. De-agglomeration is the change of clumped powder into free-flowing powder fractions called fine particle fractions. Nebulizers are capable of delivering high dosages of medication to patients who are unable to coordinate properly, as well as delivering many medications combined together in one solution. The minimum inspiratory flows required for a nebulizer’s aerosol to reach the lungs are 6–8 L/min [36,37,38].
Studies Based on Nanocarrier-Mediated Inhalational Drug Delivery for Lung Cancer
If controlled or sustained release is needed, drug incorporation in particle carriers provides a way to manipulate drug release. In recent years, colloidal carrier systems have piqued attention as a means of delivering drugs to site-specific targets, particularly in cancer treatment [39]. Figure 2 shows the advantageous features of nanocarrier-based pulmonary drug delivery in lung cancer therapy in comparison to conventional treatment approaches. The vehicles employed as drug carriers may be split into two types based on the carrier material: polymeric nanocarrier systems and lipid-based nanocarrier systems (Fig. 3). In the below sections, a detailed review of polymeric and lipid-based inhalable drug-loaded nanocarriers for lung cancer therapy is presented and summarised in Table II.
Polymer-based Nanocarrier Systems
Polymers are cross-linked polymer networks made up of numerous linear and branching copolymers. Polymer-based nanocarriers generally have matrix or reservoir-type structures made of branched polymers. In recent years, polymeric nanocarrier-based drug delivery systems have attained significant potential targeting drugs to cell surfaces and also intracellularly [40].
Microparticles
The sphere-shaped polymeric microparticles have a size dimension of 1–1000 μm. These carriers are also considered nanocarriers because of their small sizes, and the other reason is that most of the nanocarriers are converted into microparticles to improve physicochemical and aerodynamic characteristics. Due to the fact that they deposit in the deep lung areas and do not aggregate when subjected to shear pressure, microparticles are commonly employed for pulmonary administration. Polymeric microparticles have been used to contain a variety of medications, including corticosteroids, insulin, and chemotherapeutics [41]. Because they are small and easily breathed, porous microparticles are considered to be an effective platform for delivering medications to the lungs. For this purpose, a delivery system consisting of PLGA (poly (d, l-lactic-co-glycolic acid) based microparticles loaded with doxorubicin (DOX) was developed. The mean particle size and mass median aerodynamic diameters were found to be ~ 14.1 µm and ~ 3.6 μm, respectively. Due to their significant potential as a long-term inhalational carrier system for the treatment of lung cancer, DOX was slowly released from DOX-PLGA microparticles over a period of two weeks. After pulmonary administration, it was found that DOX-PLGA microparticles were deposited in high concentrations in the lungs and stayed in situ for a duration of 14 days. The in vitro study showed reduced growth in B16F10 cells within 24 h. Tumours in B16F10-implanted mice treated with DOX-PLGA microparticles were significantly smaller in relation to mass and volume when compared with non-treated cancer-bearing groups [42].
Using an emulsification process, paclitaxel-loaded sodium alginate microparticles were created. Selection of appropriate parameters and methodology enabled the formulation of microparticles with a mean-volume diameter of ~ 3 μm, mass median aerodynamic diameter of ~ 5.9 μm, fine particle fraction of ~ 13.9%, and encapsulation efficiency of ~ 61%. The in vitro cytotoxicity study of paclitaxel-loaded microparticles was evaluated using A549 and Calu-6 (human non-small-cell lung cancer cell lines) and exhibited a significant reduction in the cell viability in comparison to free drug [43]. Sericin microparticles were developed and evaluated by Liu et al. To create DOX-loaded microparticles, tannic acid/ferric iron–based metal networks were coated on the microparticles. The encapsulated microparticles showed a mean particle diameter of 4.6 μm and better encapsulation efficiency of 74.35%. The DOX entrapped microparticles taken up by 4T1 cells and effectively killed cancerous cells. The in vivo study demonstrated high deposition of developed formulation in lungs after pulmonary administration and showed significant inhibition of lung metastatic tumour in comparison to conventional formulation of DOX [44]. In another investigation, PEGylated 6 µm polystyrene microparticles were made that included camptothecin (in the form of norvaline α-amino acid prodrug). In a xenograft lung cancer animal model, anticancer effectiveness was assessed and contrasted to a bolus injection of camptothecin. Compared to untreated rats, animals receiving either free camptothecin (2 mg/kg) or camptothecin-norvaline-microparticles (0.22 mg/kg camptothecin, 100 mg/kg microparticles) had statistically significantly less lung cancerous lesions (P0.05, P0.01, respectively). Additionally, 40% of the rats given camptothecin-norvaline-microparticles were discovered to be cancer-free, leading to a distinguished increase in the anticancer effectiveness of the developed formulation in a xenograft rat model of lung cancer [45].
Polymeric Nanoparticles
Colloidal systems known as polymeric nanoparticles include pharmaceuticals that have either been integrated into the polymeric matrix or have been adsorbed on the surface of particles (nanospheres). In nanospheres, the drug is equally spread, and in nanocapsules, the drug is imprisoned in a cavity surrounded by a polymer layer [46]. Because of their superior pharmacokinetic features, polymer-based nanoparticles have been regarded as the most effective carriers employed in drug delivery applications. With recent advancements in cancer stem cells, methodologies for loading medication onto polymeric nanoparticles and their application for cancer stem cells targeting cancer therapy have been explored [47]. In order to gain higher anticancer activity in lung cancer therapy, methods for developing a nanosystem based on polylactide-tocopheryl polyethylene glycol succinate as a carrier of crizotinib are discussed. Drug trapped in the hydrophobic core of nanoparticles leads to a prolonged release pattern (~ 40% in 24 h). The optimised formulation exhibited cytotoxic activity in lung cancer cells (NCIH3122) in a dose-dependent manner. A typical endocytosis-mediated cellular uptake of the polymeric nanoparticle was also demonstrated by predominate presence in the cytoplasm of the cell. The apoptosis assay (annexin V/PI staining-based) showed significant ~ 40% apoptosis compared to only ~ 25% by free crizotinib [48]. Jung et al. integrated taxanes into polymeric nanoparticles. The average diameter of the polymeric nanoparticle-taxanes was discovered to be 45 nm (based on dynamic light scattering and transmission electron microscopy), and they were highly soluble in water. Moreover, they retained the anticancer effects of free taxanes and showed the features of active cell internalization. The tumour development delay in mice with tumours generated from A549 was investigated following the administration of polymeric nanoparticle-taxanes and/or ionizing radiation. In addition, the results also indicated that the polymeric nanoparticle-taxanes characteristics nominated it as a new and potent chemoradiation therapy agent and may have a useful and promising position in the treatment of human malignancies [49].
For targeted inhalation medication delivery, Elbatanony et al. developed afatinib-loaded biodegradable PLGA-based nanoparticles. Optimised drug-loaded nanoparticles were investigated for physicochemical characteristics (particle size ~ 180.2 nm; zeta potential ~ − 23.1 mV; entrapment efficiency ~ 34.4%). The good inhalable characteristics of Afatinib established by nanoparticle’s median aerodynamic diameter of ~ 4.7 µm and fine particle fraction of ~ 77.8%, and this would result in effective particle deposition in deep lung areas. Optimised drug-incorporated nanoparticles showed sustained drug release characteristics with a cumulative release of ~ 56.8% after 48 h. In addition, cytotoxic studies exhibited that encapsulation of Afatinib into polymeric nanoparticles significantly enhanced cytotoxic potential in A549 and H460 cell lines (KRAS-mutated NSCLC cell lines). 3D tumour spheroid studies showed superior effectiveness of developed nanoparticles in tumour growth inhibition [50].
Zhong et al. investigated the chemotherapeutic efficiency of dual anticancer-loaded drugs (Sorafenib and Crizotinib) into nanoparticles by employing biodegradable triblock poly (ethylene glycol)-poly(-caprolactone)-poly(ethylene glycol) polymer. The Sorafenib- and Crizotinib-loaded nanoparticles showed less polydispersity, with a particle size of ~ 30.45 nm. In vitro drug release analysis revealed that the Sorafenib-Crizotinib nanoparticles released both drugs for a prolonged duration and in a sustained manner. The apoptosis rate of dual drug-loaded nanoparticles was higher when compared to free drugs in A549 and 4T1 cells. Compared to free drugs, co-drug-loaded nanoparticles showed a significant reduction of tumour volume and enhanced survival rate when administered to nude mice (xenograft model) with cancer induction by 4T1 cancer cells [51]. In another report, Tang et al. incorporated etoposide into Poly(ethylene glycol)-co-poly(sebacic acid) copolymers via melt polycondensation. The developed particles showed up to 40% of encapsulation efficiency of etoposide by weight. The release studies revealed an excellent release pattern for a pronged time of over 6 days. In vitro cytotoxic studies (human lung cancer cell line) showed significant anticancer activity. Intratumourally delivered drug-loaded nanoparticles showed suppression of lung tumour in an animal model (xenograft mouse) with a 100% survival rate after 31 days of treatment, and free etoposide showed 0% survival of animals after 24 days of observation [52].
Small interfering RNA (siRNA) blocks the expression of disease-causing gene, and it has become a potent therapeutic tool in recent years. By limiting first-pass metabolism, pulmonary distribution of siRNA-nanoparticles may reduce total medication dosage and off-target effects in comparison to oral or parenteral delivery methods. On the other hand, effective siRNA delivery straight to the lung is somewhat complicated [53]. Ma et al. developed a miktoarm star polymer-siRNA nanoparticle and studied the effects of the complexed star polymer on lung cancer cells’ gene silencing activity, intracellular trafficking, and cell uptake. The developed nanoparticles showed a hydrodynamic diameter of 14.4 nm with a PDI of 0.18 and a surface charge of + 8.5 mV. According to the findings of the in vitro research, star-siRNA nanoparticles integrated into lung cancer cells and bypassed the endo-lysosomal route to prevent the expression of the target gene in these cells. In mouse lung tumours, nebulized star-siRNA nanoparticles collected in the lungs suppressed PLK1 and βIII-tubulin expression, therefore postponing the aggressive development of the tumours. These findings showed that aerosol administration of star-siRNA nanoparticles is a viable therapeutic approach for the management of lung tumours [54].
Polymeric Micelles
Micelles feature a hydrophobic interior core that can be utilised to encapsulate medications with limited solubility in order to enhance the dissolution of aqueous mediums. These nanocarriers can encapsulate and stabilize poorly active pharmaceutical ingredients, increase targeting to the lungs, decrease adverse effects, and improve treatment effectiveness in lung diseases when administered by inhalation route [55]. For clinical investigations, drug-loaded polymeric micelle-based formulations are in different stages, and some of these micelles have demonstrated potential anticancer activity [56]. In an intelligent approach, He et al. developed paclitaxel-loaded micelles utilising polyethylene glycol-polylactic acid and Pluronic P105. The functional activity of developed micelles was designed by incorporating biologically active ambroxol. Ambroxol was added to change the microenvironment of the lungs by regulating the pulmonary surfactant’s secretion. The developed nanomicelles displayed particle size of ~ 16.7 nm, round-shaped particles, low CMC value and sustained drug release characteristics. In vitro findings suggested that ambroxol might boost the secretion of pulmonary surfactant and LC3 protein and enhance the cytotoxic activity against lung cancer cell lines (A549 cells). In vivo results further indicated that the dual drug-loaded micelles improved the drug distribution in the lungs and enhanced the therapeutic efficacy in lung cancer [57].
As an alternative to conventional systemic chemotherapy, Rezazadeh M. et al. formulated a novel micelle formulation of paclitaxel by using tocopheryl succinate-polyethylene glycol (1000 and 5000 Da). Lactose was incorporated into an optimised micellar formulation employing a spray drying procedure to obtain the spherical shape of the particles for easy inhalation. Particle size ranged between 102 and 196 nm, while zeta potential was between − 9.4 and − 13.8 mV. In vitro drug release studies revealed a very slow release of the drug, and ~ 30% was released after 72 h. Cytotoxicity results on A549 (lung cancer cells) demonstrated enhanced cytotoxic activity of paclitaxel-loaded micelles when compared with the free drug [58].
Dendrimers: Dendrimers are new polymer-based nanostructures with highly branched 3D structures and several functional group surfaces, making them suitable for drug delivery applications. They are being investigated to reduce medication toxicity by targeting with improvement in therapeutic efficacy [59]. Dendrimer’s structure helps in the entrapment of chemotherapeutic drugs, which can be engineered for active and passive drug targeting through manipulable surfaces, and this may aid in the development of effective therapeutic as well as diagnostic approaches for cancer therapy [60]. Holt et al. developed polyamidoamine-based nanoparticles and attached a peptide with binding capability for lung cancer cells-based dendrimers. The dendrimers (positively charged) electrostatically bonded with nucleic acids (negatively charged). It was found that the developed platform complexed with DNA plasmids in vitro and transfected lung cancer cell lines. In vivo results established the transfection efficiency of the developed dendrimer-based system in RAG1KO mice [61]. A possible way to increase the therapeutic efficacy of DOX by lowering systemic toxicity is to combine it with carboxyl-terminated poly (amidoamine) dendrimers. The results showed an increase in the efficacy of DOX therapy in the mouse model of melanoma lung metastases (B16-F10) when administered through the pulmonary route, indicated by the decrease in tumour weight, and also showed a higher and longer accumulation/retention of the drug in lungs when compared with intravenous administration [62]. To entrap and transport anticancer drugs, alone or in combination with another substance or therapeutic nucleotide (siRNA/DNA), a variety of polypropylene imine dendrimer types have been developed. Cancer biomarkers may be utilised to make polypropylene imine dendrimers, which may then be employed as biosensors to identify different cancer types early and at different stages [63].
Lipid-Based Nanocarrier Systems
Drug development and cancer therapy have both shown a great deal of interest in lipid-based nanocarrier systems such as liposomes, solid lipid nanoparticles (SLN), niosomes and nanostructured lipid carriers (NLC) [64]. These nanocarriers have less toxicity, can encapsulate and transport both hydrophobic and hydrophilic drug molecules, and can prolong the length of medication’s efficacy by having a longer half-life and controlled drug release characteristics [65].
Liposomes
Lipid bilayer-based vesicles known as liposomes are frequently used as preferred delivery systems for both hydrophobic and hydrophilic bioactive substances [66]. Targeted drug delivery and controlled drug release have both been made possible by advancements in liposomal vesicle formation. This property is essentially helpful for cancer treatment, and liposomes have been found to enhance the therapeutic efficacy of anticancer drugs through the pulmonary route in lung cancer [67]. To treat NSCLC, targeted daunorubicin and dioscin co-delivery-based liposomes were developed using film dispersion and ammonium sulfate gradient technique. Dioscin was encapsulated within the lipid bilayer, and daunorubicin was encapsulated in the hydrophilic area of liposomes. This was modified with PFV peptide for targeted drug delivery. The developed liposomal formulation exhibited excellent physicochemical characteristics with enhanced cellular uptake and strong cytotoxicity against A549 cells. The targeted dual drug-loaded liposomes exhibited significant anticancer effects in tumour-bearing mice (BALB/c nude mice) [68]. Karpuz et al. developed a theranostic approach utilising folate-targeted liposomal platform and encapsulating Tc-99 m radiolabelled, vinorelbine and paclitaxel for NSCLC. In vitro cell line studies demonstrated significant cytotoxicity and enhanced cellular uptake of dual drug-loaded liposomes in LLC1 cells when compared with free drugs. The biodistribution studies conducted in C57BL/6 mice (NSCLC tumour bearing), the uptake of radiolabelled and actively folate-targeted, dual drug-loaded nanoliposomal formulation showed a higher presence in tumour tissues when compared to the formulation without active targeting [69].
For inhalation therapy of primary lung cancer, Zhang M et al. developed a novel paclitaxel-in-liposome-in-bacteria, a live drug-loaded carrier. Using electroporation, liposomal paclitaxel was internalized into bacteria (L. casei or E. coli), and this internalization had no effect on the growth of the mentioned bacteria. Drug-loaded liposomal formulation with E. coli showed the strongest inhibitory effect on A549 lung cancer cell lines. Paclitaxel-loaded bacteria in liposomes delivered the contents into the cells faster than the single components. E. coli-based formulation also exhibited the strongest anticancer activity on primary lung cancer evaluated on rat model of lung cancer [70]. Osimertinib’s systemic delivery frequently leads to inadequate medication levels at the specific location in case of lung cancer and is linked to systemic adverse effects. The development of the drug’s active and passive liposomes through the inhalational route showed a reduction in systemic exposure with accumulation at the tumour site. Active liposomes exhibited better encapsulation (78%) than passive liposomes (25%), and both showed outstanding aerosolization efficiency with an aerodynamic diameter of 4 µm and fine particles of 82%. Osimertinib’s active and passive targeted liposomes decreased IC50 in H1975 cells by 2.2 and 1.2-fold in comparison to free drug, respectively. The 3D spheroid studies demonstrated that the developed liposomes were found effective in inhibiting tumour growth [71]. Adel et al. developed curcumin-loaded proliposomes using a nano-spray dryer technique; lecithin and cholesterol as vesicle matrix components; stearyl amine as positive charge inducer, poloxamer 188 as a surfactant, and hydroxypropyl-beta-cyclodextrin as a carrier to produce freely flowing powders. The optimised formulation had a percentage yield of 52.72 to 81.87%, particle size of 160 to 365 nm, zeta potential between − 25.50 and − 38.90 mV, encapsulation efficiency of 90.15 to 102.20%, and more than 95% in vitro drug release. The mass median aerodynamic diameter and fine particle fraction of spray-dried proliposomes were found to be 2.10 µm and 54.35%, respectively. A lung pharmacokinetic study revealed a higher AUC value of the developed formulation in comparison to free curcumin powder. The cytotoxicity of the optimised curcumin-loaded proliposomal formulation against the A-549 cell line revealed a comparably low IC50 value in comparison to free curcumin [72].
Unlike usual therapies by small organic molecules, which usually target proteins and provide transient effects, nucleic acid therapeutics can attain specific, long-lasting and remedial effects [73]. Loira-Pastoriza et al. used a cationic lipid, dioleoyltrimethylammoniumpropane and dipalmitoylphosphatidylcholine to encapsulate unmethylated oligodeoxynucleotides with CpG motifs and polyinosinic-polycytidylic acid double-stranded RNA in liposomes for local delivery in lung cancer. The cationic lipid in the optimised liposomes produced a positively charged particle (+ 59 mV) with a size of less than 200 nm, a low polydispersity index of 0.107, and an encapsulation efficiency of 98.2%. Additionally, in vivo studies on the pulmonary administration of CpG revealed that, in comparison to its intraperitoneal injection, the lungs produced more granzyme B, a pro-apoptotic protein, T helper type 1 cytokines, and chemokines. CpG encapsulation in cationic lipid-based liposomes significantly reduced tumour growth in metastatic lung cancer (murine B16F10 model) after pulmonary administration [74].
In recent work, Abeesh P et al. functionalized the PEGylated nanoliposomes loaded with withaferin A (PWN) for targeted drug administration using an innovative targeting approach AS1411 (anti-nucleolin aptamer) and was prepared by thin-film hydration technique. With an encapsulation efficiency of 82.5%, the produced formulation PWN contained spherically shaped nanosized particles with a size of ~ 118 nm. The results of the TEM investigation showed that PWN possesses homogeneous, spherical nanoparticles with good dispersibility. The in vivo study conducted on lung metastasis in C57BL/6 mice showed considerably increased anti-metastatic effectiveness of PWN and survival rate when compared to groups given free medication. In mice with metastatic lung tumours treated with PWN, the expression levels of IL-6, TNF-α, and IL-1 β were downregulated. The results exhibited the significant potential of nanoliposomal formulation of withaferin A for targeting metastatic tumours utilising the AS1411 functionalization with PEGylation [75].
Niosomes
The vesicular structures known as niosomes are based on nonionic surfactants and are currently used as cutting-edge drug delivery systems. The size of niosomes can be varied, and nanometric scale is mostly used for drug delivery applications [76]. Niosomes are biodegradable and biocompatible in nature. They provide sustained and controlled release of drug molecules, can be modified to target a specific location in the body, and are more stable with an extended shelf life in comparison to other vesicular structures. The capability of niosomes to encapsulate and transport drugs has generated a lot of interest in formulation scientists in the recent decade [77]. Using various combination of nonionic surfactants and cholesterol, ciprofloxacin hydrochloride was encapsulated in niosomes and evaluated for its suitability in pulmonary drug delivery. Formulations consisting of Tween 60 and Span 60 with 40 mol% cholesterol demonstrated not only high encapsulation efficacy and stability but also a fine particle fraction and nebulization efficiency of around ~ 77.9% and ~ 61.9%, respectively. Against a number of lung pathogens, niosomal ciprofloxacin exhibited a lower minimum inhibitory concentration than free ciprofloxacin. Drug-loaded niosomal formulation showed significantly higher cytotoxicity against A549 cell lines (human lung carcinoma) when compared with the free drug [78].
Saimi et al. developed a low-dosage niosomal formulation for the treatment of lung cancer, encapsulating gemcitabine and cisplatin. This formulation was prepared by utilising a simple heating technique and optimised by D-optimal mixture design. The optimal Gemcitabine-cisplatin formulation showed − 15.28 mV of zeta potential, 0.16 of PDI and 166.45 nm of size, and it was found to be stable at 27 °C for 90 days without any phase separation. The formulation’s capacity to aerosolize was demonstrated by the aerosol output, which was 96.22%. Using the dialysis bag diffusion technique, an in vitro drug release study revealed controlled release for both drugs for up to 24 h. The results of cytotoxicity studies revealed that the optimised formulation showed reduced cytotoxicity activity against both MRC5 (normal lung cell line) and A549 (lung cancer cell line) when compared with the combination of free drugs [79]. In another study, Shukla et al. developed nintedanib-loaded niosomes using thin-film hydration technique for inhalational administration for the management of lung cancer. The optimised niosomal formulation showed a size of ~ 195.5 nm with efficient aerodynamic qualities, sustained and prolonged drug release characteristics. Niosomes loaded with nintedanib demonstrated considerably greater cytotoxicity against A549 cell lines, which was supported by 3D spheroids (demonstrated higher inhibition in tumour growth for niosomal formulation in comparison to control) [80].
Nanoemulsions
Nanoemulsions are colloidal dispersion systems that consist of immiscible liquids with emulsifiers (surfactants and co-surfactants) to create a single phase that is thermodynamically stable. Numerous studies on nanoemulsions as drug delivery systems have been in the literature for different routes of administration [81]. Nanoemulsion droplet size ranges between 10–200 nm. Nanoemulsion-based drug delivery systems are designed to enhance the solubility and bioavailability of active pharmaceutical ingredients [82]. Because they have a high drug loading efficiency, enhanced pulmonary deposition and retention, and lengthen the time that active compounds spend in the lung tissues, nanoemulsions have the potential to deliver active compounds to the lungs [83, 84]. Arbain et al. developed quercetin-loaded nanoemulsions based on palm oil ester employing high-energy emulsification method and optimised by D-optimal mixture design for pulmonary drug delivery. The optimised nanoemulsion showed an aerodynamic diameter of 4.25 µm, aerosols rate of 0.19 g/min and aerosols output of 99.31%. The developed nanoemulsion also showed good stability when stored at 4℃ for a duration of 90 days. The characterization results revealed the potential of palm oil ester–based nanoemulsion encapsulating quercetin for pulmonary drug delivery in lung cancer therapy [85]. Hyaluronic acid-complexed paclitaxel nanoemulsions were fabricated by Kim et al. using ionic complexing technique to solve the solubility issue and for lung cancer targeting. Paclitaxel nanoemulsions were prepared by high-pressure homogenization technique and contained DL-tocopheryl acetate, polysorbate 80, soybean oil, hyaluronic acid and ferric chloride. The developed nanoemulsion showed a droplet size of ~ 85.2 nm and a zeta potential of ~ 35.7 mV. The content of paclitaxel was 3.0 mg/mL, and the encapsulation efficiency was ~ 00%. In vivo anticancer activity of the hyaluronic acid-complexed paclitaxel based nanoemulsions in nude mice showed a significant reduction in tumour volume and showed the potential application of this platform for the treatment of NSCLC [86].
Solid Lipid Nanoparticles
Solid lipid nanoparticles (SLNs) are lipid-based nanoparticles with diameters ranging between 50 and 1000 nm and can encapsulate active pharmaceutical ingredients with appropriate solvent and lipids, which are solid at room temperature. SLN-based delivery systems have emerged to overcome many drawbacks, such as complicated production methods, low percentage entrapment efficiency and difficulty in large-scale manufacture of other lipid carrier systems such as liposomes and ethosomes [87]. When compared to conventional colloidal carriers, SLNs have a number of distinguishing characteristics, including reduced toxicity, high surface area, delayed/sustained drug release, enhanced cellular penetration, and capability to enhance the solubility, bioavailability and targeting potential of pharmaceuticals [88]. Tyrosine kinase inhibitors such as erlotinib were loaded into SLN-based formulation and transformed into dry powder inhalers by Bakhtiary et al., employing optimised concentrations of poloxamer 407/Compritol. The SLNs showed a size of 100 nm with a spherical shape and an entrapment efficiency of 78.21%. The optimised formulation displayed significant anticancer activity against A549 cells. To develop the SLN-based dry powder inhaler, the erlotinib-loaded SLNs were spray-dried into microparticles (1–5 µm). The dried particles showed desirable flow characteristics and aerodynamic attributes. Hausner’s ratio (1.119), Carr’s Index (10.66) and Next Generation Impactor results (fine particle fraction ~ 24.25%) established deep inhalational patterns of developed SLN-based microparticles of erlotinib [89].
Rosiere et al. formulated paclitaxel-loaded SLN with a new folate conjugated copolymer of polyethylene glycol and chitosan and obtained encapsulation efficiency of ~ 100%, mean particle diameter of ~ 250 nm, and zeta potential of + 32 mV. After pulmonary administration, the coated SLN penetrated M109 tumours in vivo, HeLa and M109-HiFR cells in vitro, and entered into folate receptor-expressing cells. The results demonstrated that after pulmonary drug delivery in vivo, the developed SLNs showed a favourable pharmacokinetic profile with prolonged pulmonary exposure of paclitaxel lasting up to 6 h and little systemic drug distribution [90]. Another investigation was conducted to develop dry, aerosolisable lipid nanoparticle powder of siRNA using a thin-film freeze-drying process. The siRNA-loaded SLNs were prepared using the solvent evaporation technique. The particle size, PDI, and zeta potential of SLNs were well-preserved after subjecting them to thin-film freeze-drying and reconstitution. The function of the siRNA-encapsulated in SLNs was not negatively affected by the thin-film freeze-drying process. It was concluded that the thin-film freeze-drying technique was a feasible approach for producing dry, aerosolisable lipid nanoparticles for pulmonary drug delivery [91].
Nanostructured Lipid Carriers
To address some drawbacks of SLNs, a new generation of lipid nanoparticles called Nanostructured Lipid Carriers (NLCs) were developed. NLC also exists as a solid lipid matrix at body temperature in addition to ambient temperature. Instead of using only a solid lipid, a part of the solid lipid is substituted with oil, resulting in a less ordered lipid matrix that improves drug loading and avoids drug leakage during storage [92, 93]. NLCs are being studied as drug delivery carriers for a variety of therapeutic applications due to their excellent biocompatibility and safety profiles. Due to their capability to enhance the physical and chemical stability of active pharmaceutical ingredients and to significantly increase the potential of therapeutically useful substances, NLCs are also being explored for different chemotherapeutic agents [94]. NLCs were developed in lung cancer to treat p-glycoprotein (P-gp) efflux and drug resistance, which is typically linked to overexpression of the MRP1 and BCL2 proteins, which are responsible for the drug efflux from cancer cells. To solve these problems, Garbuzenko et al. fabricated inhalation pulmonary delivery of anticancer drugs in conjunction with pump suppressors and non-pump cellular resistance. To evaluate this hypothesis, a nanoparticle-based delivery system consisting of DOX as cell death inducer and antisense oligonucleotides specifically targeted to MRP1 mRNA as pump resistance suppressor and to BCL2 mRNA non-pump resistance suppressor was developed and evaluated on a murine model (orthotopic) of human lung carcinoma. The results demonstrated the high antitumour activity and fewer adverse effects of the developed inhalable platform, which was not achievable by individual components administered separately [95]. Paclitaxel and DOX are often used together to treat solid tumours; however, the effectiveness of the free medication in combination is less due to non-targeting and improper pharmacokinetic profile. To combat the multidrug resistance brought on by a single treatment, an NLC-based delivery method for co-encapsulating paclitaxel and DOX was developed. Dual drug-loaded NLC-based formulation exhibited the highest cytotoxic activity in vitro against NCL-H460 human NSCLC cell lines in comparison to single drug-loaded NLCs. In vivo investigations on NSCLC animal models further established the potential of co-drug-loaded NLCs in the management of lung cancer [20]. Patlolla et al. encapsulated celecoxib into NLCs employing a high-pressure homogenization technique. Drug-loaded NLCs showed particle size of ~ 217 nm and entrapment efficiency of > 90%. The drug-loaded NLC released the celecoxib in a sustained and controlled manner; in vitro aerosolization of formulation showed a fine particle fraction of ~ 75.6% and aerodynamic diameter of ~ 1.6 µm. The developed NLCs showed time and dose-dependent anticancer activity against A549 cells. Nebulization of celecoxib-loaded NLCs exhibited fourfold higher AUC(t)/D in lungs in comparison to celecoxib solution. The systemic clearance of drug-loaded NLCs was slower (0.93 l/h) when compared to the drug solution (20.03 l/h) [96].
Latest Investigations Related to Nanocarrier-Mediated Inhalational Drug Delivery for Lung Cancer
Much recent research work has been conducted related to polymer and based nanocarriers for the management of lung cancer through the pulmonary route of drug delivery. The section below provides a detailed review of the latest investigations performed and is summarised in Table III.
In a very recent research work airway, mucus barrier was targeted for improvement in anticancer activity of quercetin. Tang et al. developed an inhalable silk fibroin (modified with Pluronic F127) nanoparticles of quercetin. The optimised nanoparticles showed particle size of ~ 200 nm with stable characteristics ascertained by negatively charged surfaces (zeta potential of ~ − 26.3 mV) and showed sustained release characteristics up to 24 h (~ 80%). Superior mucus penetrating capability was shown by Pluronic F127 coated nanoparticles in artificial mucus and monolayer cell model (Calu-3) established by photobleaching assay and transepithelial transport test. In vivo anticancer activity in mice melanoma lung metastasis model showed an enhanced therapeutic effect of coated nanoparticles was significantly improved in vivo in comparison to non-coated nanoparticles [97].
Gonsalves et al. developed an inhalable polymer-based nanoparticle (poly lactic-co-glycolic acid) formulation with Infasurf® (a biomimetic lung surfactant) (LS) for lung cancer therapy. The developed formulation showed a size of ~ 188 nm and was found to be stable in phosphate buffer saline, Gamble’s solution (simulated lung fluid) and serum. Paclitaxel-loaded in Infasurf® lung surfactant exhibited burst release characteristics, and gemcitabine hydrochloride entrapped in polymeric core (PLGA) released the drug in a sustained manner. In vivo studies showed greater retention of lung surfactant-coated nanoparticles in the lungs of cancerous mice (C57BL/6 WT) compared to uncoated nanoparticles after intranasal administration. The results confirmed that Infasurf® coating is a potential platform for covering polymeric nanoparticles to prevent their fast lung clearance and enable prolonged pulmonary drug delivery [98].
siRNA-based therapeutics are showing significant therapeutic capability. However, hydrophilicity, high molecular weight, instability against nuclease and the presence of intrinsic negative charge hinder the translation of siRNA-based products into clinical developmental phases. Liu et al. designed a Tetra(piperazino) fullerene epoxide-based nanocomplex for lung delivery of siRNA through inhalational route. The development and optimisation of this was carried out by molecular dynamic simulation. The formulated siRNA-based nanocomplex protected the encapsulated siRNA against degradation by nucleases, improved cellular uptake, enhanced gene knockdown capability and prolonged the lung retention of siRNA after pulmonary delivery. Through the introduction of siRNA programmed death-ligand 1, this nanostructure significantly inhibited the advancement of metastatic lung cancer without any noticeable adverse event and toxicity observations in a mouse model of lung cancer [99]. In another study, Zimmermann et al. developed spray-dried lipid nanoparticles of siRNA for pulmonary delivery. Spray drying was conducted using lactose solution (5%, m/V), and mass median aerodynamic diameters of all powders obtained were between 2.85 and 2.9 μm. The nanoparticle size after redispersion of spray-dried powders obtained was ~ 200 nm and a PDI value of ~ 0.3. The spray-dried lipid nanoparticles penetrated the mucus layer of the lungs with the maintenance of bioactivity for more than 90% protein downregulation in a lung adenocarcinoma cell line. Additionally, the developed nanoparticles effectively achieved gene silencing (up to 50%) of the house keeping gene (GAPDH) performed in ex vivo lung slices (human precision cut) without any increase in cytokine levels [100].
Gao et al. developed a liposome-based co-delivery formulation of 7-ethyl-10-hydroxyl camptothecin (SN38) prodrug and curcumin for lung cancer therapy via the pulmonary route of drug delivery. SN38 was attached to TAT (cell-penetrating peptide) via polyethylene glycol linker to produce SN38 prodrug. Co-drug-loaded liposomes were prepared by the microfluidic method and exhibited a vesicle size of ~ 171.21 nm. In vitro anticancer cell line studies on A549 cells showed enhanced antiproliferative activity, enhanced induction of cell apoptosis and improved arrest of the cell cycle for developed liposomal formulation in comparison to single drug treatments. In the lung cancer model of BALB/c mouse, the combination drug-loaded liposomes showed significant inhibition of tumour [101].
Clinical Studies
Even though nanocarriers have a lot of potential for the management of lung cancer through the pulmonary route, there are not enough clinical investigations on them yet. As a result, there is a need to broaden their scope of applicability to include clinical trials under suitable ethical guidelines. Some of these approaches have been evaluated in various clinical trials awaiting results or with recently published results, while most of them are still in clinical trials in the recruiting phase (https://clinicaltrials.gov/). Some of the clinical trials related to pulmonary administration and lung cancer are summarised in Table IV.
Patent Reports
An extensive search was performed for patents associated with the formulations for lung cancer through pulmonary route (patentscope.wipo.int, www.uspto.gov, patents.google.com, lens.org). Patent reports were screened, studied and documented. Table V lists the drug formulations that are patented related to lung cancer therapy through the pulmonary route of administration [102,103,104,105,106,107,108,109,110,111].
Conclusion and Future Perspective
Conventional methods of lung cancer therapy have significant difficulties, such as nonspecific targeting, narrow therapeutic efficiency, unfavourable adverse effects, drug resistance and patient noncompliance. Nanocarrier-based drug delivery systems have shown significant potential for diagnosis, monitoring, and therapy of different cancers. Several nanocarrier-based investigational therapies for lung cancer use targeting and tracking elements with anticancer drugs in their structure. Scientists have developed a number of drug-loaded nanocarrier systems via inhalation for lung cancer therapy to improve drug delivery (targeting, sustained release characteristics) and reduce systemic side effects. In light of these considerations, inhalational drug delivery with nanocarriers for use in lung cancer is promising [112]. Although the advancement of nanocarriers has been recognized as a potential option for lung cancer therapy, they cannot be regarded as flawless due to several unmet demands for their proper delivery. The size and shape of the nanocarrier are of primary importance for effective drug delivery to the lungs via the inhalational route. Changes in procedure or composition might have a deleterious impact on drug delivery. In addition, clinical and preclinical research is continuing to look into using the inhalational route of drug administration to treat lung cancer and other lung disorders. More molecular-level studies are required to understand the targeting of nanocarriers in lung cancer.
References
Jin KT, Lu ZB, Chen JY, Liu YY, Lan HR, Dong HY, et al. Recent trends in nanocarrier-based targeted chemotherapy: selective delivery of anticancer drugs for effective lung, colon, cervical, and breast cancer treatment. J Nanomater. 2020;2020:9184284.
Xu CN, Tian HY, Wang YB, Du Y, Chen J, Lin L, et al. Anti-tumor effects of combined doxorubicin and siRNA for pulmonary delivery. Chin Chem Lett. 2017;28:807–12.
Patil TS, Deshpande AS. Nanostructured lipid carriers-based drug delivery for treating various lung diseases: a state-of-the-art review. Int J Pharm. 2018;547:209–25.
Kazmi I, Shaikh MAJ, Afzal O, Altamimi ASA, Almalki WH, Alzarea SI, et al. Chitosan-based nano drug delivery system for lung cancer. J Drug Deliv Sci Technol. 2023;81:104196.
Sristi Fatima M, Sheikh A, Almalki WH, Talegaonkar S, Dubey SK, et al. Recent advancement on albumin nanoparticles in treating lung carcinoma. J Drug Target. 2023;31:486–99.
Rudin CM, Brambilla E, Faivre-Finn C, Sage J. Small-cell lung cancer. Nat Rev Dis Primers. 2021;7:1–20.
Yang S, Zhang Z, Wang Q. Emerging therapies for small cell lung cancer. J Hematol Oncol. 2019;12:1–11.
Vestergaard HH, Christensen MR, Lassen UN. A systematic review of targeted agents for non-small cell lung cancer. Acta Oncol. 2018;57:176–86.
Abdulbaqi IM, Assi RA, Yaghmur A, Darwis Y, Mohtar N, Parumasivam T, et al. Pulmonary delivery of anticancer drugs via lipid-based nanocarriers for the treatment of lung cancer: An update. Pharmaceuticals. 2021;14:725.
Patel AR, Chougule MB, Patlolla R, Wang G, Singh M. Efficacy of aerosolized celecoxib encapsulated nanostructured lipid carrier in non-small cell lung cancer in combination with docetaxel. Pharm Res. 2013;30:1435–46.
Loo CY, Traini D, Young PM, Parumasivam T, Lee WH. Pulmonary delivery of curcumin and quercetin nanoparticles for lung cancer – Part 2: toxicity and endocytosis. J Drug Deliv Sci Technol. 2023;82:104375.
Li L, Yu J, Chen Z, Zhang J. Improved primary lung carcinoma therapeutics utilizing a non-invasive approach of combinatorial drug loaded aerosolized dry inhaler powder. J Clust Sci. 2022;33:1781–91.
Tang L, Li J, Zhao Q, Pan T, Zhong H, Wang W. Advanced and innovative nano-systems for anticancer targeted drug delivery. Pharmaceutics. 2021;13:1151.
Ho GF, Chai CS, Alip A, Wahid MI, Abdullah MM, Foo YC, et al. Real-world experience of first-line afatinib in patients with EGFR-mutant advanced NSCLC: a multicenter observational study. BMC Cancer. 2019;19:896.
Santarpia M, Daffinà MG, D’Aveni A, Marabello G, Liguori A, Giovannetti E, et al. Spotlight on ceritinib in the treatment of ALK+ NSCLC: design, development and place in therapy. Drug Des Devel Ther. 2017;11:2047–63.
Wolf J, Seto T, Han JY, Reguart N, Garon EB, Groen HJ, et al. Capmatinib in MET exon 14–mutated or MET-amplified non–small-cell lung cancer. N Engl J Med. 2020;383:944–57.
Sartore-Bianchi A, Pizzutilo EG, Marrapese G, Tosi F, Cerea G, Siena S. Entrectinib for the treatment of metastatic NSCLC: safety and efficacy. Expert Rev Anticancer Ther. 2020;3(20):333–41.
Saleh K, Khalife N, Felefly T. RET fusions in non-small-cell lung cancer: an emerging target reshaping the treatment paradigm. Future Oncol. 2021;17:1445–8.
Kumari P, Ghosh B, Biswas S. Nanocarriers for cancer-targeted drug delivery. J Drug Target. 2016;24:179–91.
Wang Y, Zhang H, Hao J, Li B, Li M, Xiuwen W. Lung cancer combination therapy: co-delivery of paclitaxel and doxorubicin by nanostructured lipid carriers for synergistic effect. Drug Deliv. 2016;23:1398–403.
Din FU, Aman W, Ullah I, Qureshi OS, Mustapha O, Shafique S, et al. Effective use of nanocarriers as drug delivery systems for the treatment of selected tumors. Int J Nanomedicine. 2017;12:7291–309.
Kaur P, Garg T, Rath G, Murthy RR, Goyal AK. Development, optimization and evaluation of surfactant-based pulmonary nanolipid carrier system of paclitaxel for the management of drug resistance lung cancer using Box-Behnken design. Drug Deliv. 2016;23:1912–25.
Jyoti K, Kaur K, Pandey RS, Jain UK, Chandra R, Madan J. Inhalable nanostructured lipid particles of 9-bromo-noscapine, a tubulin-binding cytotoxic agent: in vitro and in vivo studies. J Colloid Interface Sci. 2015;445:219–30.
Lu B, Sun L, Yan X, Ai Z, Xu J. Intratumoral chemotherapy with paclitaxel liposome combined with systemic chemotherapy: a new method of neoadjuvant chemotherapy for stage III unresectable non-small cell lung cancer. Med Oncol. 2015;32:1–8.
Asmawi AA, Salim N, Ngan CL, Ahmad H, Abdulmalek E, Masarudin MJ, et al. Excipient selection and aerodynamic characterization of nebulized lipid-based nanoemulsion loaded with docetaxel for lung cancer treatment. Drug Deliv Transl Res. 2019;9:543–54.
Li S, Wang L, Li N, Liu Y, Su H. Combination lung cancer chemotherapy: design of a pH-sensitive transferrin-PEG-Hz-lipid conjugate for the co-delivery of docetaxel and baicalin. Biomed Pharmacother. 2017;95:548–55.
Liang Y, Tian B, Zhang J, Li K, Wang L, Han J, et al. Tumor-targeted polymeric nanostructured lipid carriers with precise ratiometric control over dual-drug loading for combination therapy in non-small-cell lung cancer. Int J Nanomedicine. 2017;12:1699–715.
Nanjwade BK, Adichwal SA, Gaikwad KR, Parikh KA, Manvi FV. Pulmonary drug delivery: novel pharmaceutical technologies breathe new life into the lungs. PDA J Pharm Sci Technol. 2011;65:513–34.
Newman SP. Drug delivery to the lungs: challenges and opportunities. Ther Deliv. 2017;8:647–61.
He S, Gui J, Xiong K, Chen M, Gao H, Fu Y. A roadmap to pulmonary delivery strategies for the treatment of infectious lung diseases. J Nanobiotechnology. 2022;20:101.
Smola M, Vandamme T, Sokolowski A. Nanocarriers as pulmonary drug delivery systems to treat and to diagnose respiratory and non respiratory diseases. Int J Nanomed. 2008;3:1–19.
Hickey AJ. Emerging trends in inhaled drug delivery. Adv Drug Deliv Rev. 2020;157:63–70.
Ibrahim M, Verma R, Garcia-Contreras L. Inhalation drug delivery devices: technology update. Med Devices (Auckl). 2015;8:131–9.
de Boer AH, Molema G, Frijlink HW. Pulmonary drug delivery: delivery to and through the lung. In: Molema G, Meijer DKF, editors. Drug Targeting Organ-Specific Strategies. Wiley Online Library; 2001. p. 53–83. https://doi.org/10.1002/352760006X.ch3.
Wang B, Hu L, Siahaan TJ. Drug delivery: principles and applications. 2nd ed. New Jersey: John Wiley & Sons; 2016.
Tena AF, Clarà PC. Deposition of inhaled particles in the lungs. Arch Bronconeumol. 2012;48:240–6.
Patil JS, Sarasija S. Pulmonary drug delivery strategies: a concise, systematic review. Lung India. 2012;29:44–9.
ElKasabgy NA, Adel IM, Elmeligy MF. Respiratory tract: structure and attractions for drug delivery using dry powder inhalers. AAPS Pharm Sci Tech. 2020;21:1–14.
Bahrami B, Hojjat-Farsangi M, Mohammadi H, Anvari E, Ghalamfarsa G, Yousefi M, et al. Nanoparticles and targeted drug delivery in cancer therapy. Immunol Lett. 2017;190:64–83.
Lu H, Zhang S, Wang J, Chen Q. A review on polymer and lipid-based nanocarriers and its application to nano-pharmaceutical and food-based systems. Front Nutr. 2021;8:783831.
El-Sherbiny IM, El-Baz NM, Yacoub MH. Inhaled nano and microparticles for drug delivery. Global Cardiol Sci Pract. 2015;2015:2–14.
Kim I, Byeon HJ, Kim TH, Lee ES, Oh KT, Shin BS, et al. Doxorubicin-loaded highly porous large PLGA microparticles as a sustained-release inhalation system for the treatment of metastatic lung cancer. Biomater. 2012;33:5574–83.
Alipour S, Montaseri H, Tafaghodi M. Preparation and characterization of biodegradable paclitaxel loaded alginate microparticles for pulmonary delivery. Colloids Surf B. 2010;81:521–9.
Liu J, Deng Y, Fu D, Yuan Y, Li Q, Shi L, et al. Sericin microparticles enveloped with metal-organic networks as a pulmonary targeting delivery system for intra-tracheally treating metastatic lung cancer. Bioact Mater. 2021;6:273–84.
Chao P, Deshmukh M, Kutscher HL, Gao D, Rajan SS, Hu P, et al. Pulmonary targeting microparticulate camptothecin delivery system: anti-cancer evaluation in a rat orthotopic lung cancer model. Anticancer Drugs. 2010;21:65–76.
Amararathna M, Goralski K, Hoskin DW, Rupasinghe HV. Pulmonary nano-drug delivery systems for lung cancer: current knowledge and prospects. J Lung Health Dis. 2019;3:11–28.
Li B, Li Q, Mo J, Dai H. Drug-loaded polymeric nanoparticles for cancer stem cell targeting. Front Pharmacol. 2017;8:51.
Jiang ZM, Dai SP, Xu YQ, Li T, Xie J, Li C, et al. Crizotinib-loaded polymeric nanoparticles in lung cancer chemotherapy. Med Oncol. 2015;32:1–8.
Jung J, Park SJ, Chung HK, Kang HW, Lee SW, Seo MH, et al. Polymeric nanoparticles containing taxanes enhance chemoradiotherapeutic efficacy in non-small cell lung cancer. Int J Radiat Oncol Biol Phys. 2012;84:e77-83.
Elbatanony RS, Parvathaneni V, Kulkarni NS, Shukla SK, Chauhan G, Kunda NK, et al. Afatinib-loaded inhalable PLGA nanoparticles for localized therapy of non-small cell lung cancer (NSCLC)—development and in-vitro efficacy. Drug Deliv Transl Res. 2020;11:927–43.
Zhong T, Liu X, Li H, Zhang J. Co-delivery of sorafenib and crizotinib encapsulated with polymeric nanoparticles for the treatment of in vivo lung cancer animal model. Drug Deliv. 2021;28:2108–18.
Tang BC, Fu J, Watkins DN, Hanes J. Enhanced efficacy of local etoposide delivery by poly (ether-anhydride) particles against small cell lung cancer in vivo. Biomater. 2010;31:339–44.
Ding L, Tang S, Wyatt TA, Knoell DL, Oupický D. Pulmonary siRNA delivery for lung disease: review of recent progress and challenges. J Control Release. 2021;330:977–91.
Ma Z, Wong SW, Forgham H, Esser L, Lai M, Leiske MN, et al. Aerosol delivery of star polymer-siRNA nanoparticles as a therapeutic strategy to inhibit lung tumor growth. Biomaterials. 2022;285:121539.
Pham DT, Chokamonsirikun A, Phattaravorakarn V, Tiyaboonchai W. Polymeric micelles for pulmonary drug delivery: a comprehensive review. J Mater Sci. 2021;56:2016–36.
Zhou Q, Zhang L, Yang T, Wu H. Stimuli-responsive polymeric micelles for drug delivery and cancer therapy. Int J Nanomedicine. 2018;13:2921–42.
He W, Xiao W, Zhang X, Sun Y, Chen Y, Chen Q, et al. Pulmonary-affinity paclitaxel polymer micelles in response to biological functions of ambroxol enhance therapeutic effect on lung cancer. Int J Nanomedicine. 2020;15:779–93.
Rezazadeh M, Davatsaz Z, Emami J, Hasanzadeh F, Jahanian NA. Preparation and characterization of spray-dried inhalable powders containing polymeric micelles for pulmonary delivery of paclitaxel in lung cancer. J Pharm Sci. 2018;21:200–14.
Sherje AP, Jadhav M, Dravyakar BR, Kadam D. Dendrimers: a versatile nanocarrier for drug delivery and targeting. Int J Pharm. 2018;548:707–20.
Gorain B, Choudhury H, Pandey M, Nair AB, Amin MCIM, Molugulu N, et al. Dendrimer-based nanocarriers in lung Cancer therapy. In: Kesharwani P, editor. Nanotechnology-Based Targeted Drug Delivery Systems for Lung Cancer. Academic Press; 2019. p. 161–92. https://doi.org/10.1016/B978-0-12-815720-6.00007-1.
Holt GE, Daftarian P. Non-small-cell lung cancer homing peptide-labeled dendrimers selectively transfect lung cancer cells. Immunotherapy. 2018;10:1349–60.
Zhong Q, Bielski ER, Rodrigues LS, Brown MR, Reineke JJ, da Rocha SR. Conjugation to poly (amidoamine) dendrimers and pulmonary delivery reduce cardiac accumulation and enhance antitumor activity of doxorubicin in lung metastasis. Mol Pharmaceutics. 2016;13:2363–75.
Singh V, Sahebkar A, Kesharwani P. Poly (propylene imine) dendrimer as an emerging polymeric nanocarrier for anticancer drug and gene delivery. Eur Polym J. 2021;158:110683.
Ansari MT, Ramlan TA, Jamaluddin NN, Zamri N, Salfi R, Khan A, et al. Lipid-based nanocarriers for cancer and tumor treatment. Curr Pharm Des. 2020;26:4272–6.
Mishra DK, Shandilya R, Mishra PK. Lipid based nanocarriers: a translational perspective. Nanomedicine: Nanotechnol Biol Med. 2018;14:2023–50.
Liu Y, Bravo KM, Liu J. Targeted liposomal drug delivery: a nanoscience and biophysical perspective. Nanoscale Horiz. 2021;6:78–94.
Olusanya TO, Haj Ahmad RR, Ibegbu DM, Smith JR, Elkordy AA. Liposomal drug delivery systems and anticancer drugs. Mol. 2018;23:907.
Wang Y, Fu M, Liu J, Yang Y, Yu Y, Li J, et al. Inhibition of tumor metastasis by targeted daunorubicin and dioscin codelivery liposomes modified with PFV for the treatment of non-small-cell lung cancer. Int J Nanomedicine. 2019;14:4071–90.
Karpuz M, Silindir-Gunay M, Ozer AY, Ozturk SC, Yanik H, Tuncel M, et al. Diagnostic and therapeutic evaluation of folate-targeted paclitaxel and vinorelbine encapsulating theranostic liposomes for non-small cell lung cancer. Eur J Pharm Sci. 2021;156:105576.
Zhang M, Li M, Du L, Zeng J, Yao T, Jin Y. Paclitaxel-in-liposome-in-bacteria for inhalation treatment of primary lung cancer. Int J Pharm. 2020;578:119177.
Sawant SS, Patil SM, Shukla SK, Kulkarni NS, Gupta V, Kunda NK. Pulmonary delivery of osimertinib liposomes for non-small cell lung cancer treatment: formulation development and in vitro evaluation. Drug Deliv Trans Res. 2022;12:2474–87.
Adel IM, ElMeligy MF, Abdelrahim ME, Maged A, Abdelkhalek AA, Abdelmoteleb AM, et al. Design and characterization of spray-dried proliposomes for the pulmonary delivery of curcumin. Int J Nanomedicine. 2021;16:2667–87.
Nsairat H, AlShaer W, Odeh F, Essawi E, Khater D, Al Bawab A, et al. Recent advances in using liposomes for delivery of nucleic acid-based therapeutics. OpenNano. 2023;11:100132.
Loira-Pastoriza C, Vanvarenberg K, Ucakar B, Franco MM, Staub A, Lemaire M, et al. Encapsulation of a CpG oligonucleotide in cationic liposomes enhances its local antitumor activity following pulmonary delivery in a murine model of metastatic lung cancer. Int J Pharm. 2021;600:120504.
Abeesh P, Bouvet P, Guruvayoorappan C. AS1411 aptamer tagged PEGylated liposomes as a smart nanocarrier for tumor-specific delivery of Withaferin A for mitigating pulmonary metastasis. Biomaterials Advances. 2023;154:213661.
Okore VC, Attama AA, Ofokansi KC, Esimone CO, Onuigbo EB. Formulation and evaluation of niosomes. Indian J Pharm Sci. 2011;73:323–8.
Ag Seleci D, Seleci M, Walter JG, Stahl F, Scheper T. Niosomes as nanoparticular drug carriers: fundamentals and recent applications. J Nanomater. 2016;2016:1–13. https://doi.org/10.1155/2016/7372306.
Moazeni E, Gilani K, Sotoudegan F, Pardakhty A, Najafabadi AR, Ghalandari R, et al. Formulation and in vitro evaluation of ciprofloxacin containing niosomes for pulmonary delivery. J Microencapsul. 2010;27:618–27.
Saimi NIM, Salim N, Ahmad N, Abdulmalek E, Abdul Rahman MB. Aerosolized niosome formulation containing gemcitabine and cisplatin for lung cancer treatment: Optimization, characterization and in vitro evaluation. Pharmaceutics. 2021;13:59. https://doi.org/10.3390/pharmaceutics13010059.
Shukla SK, Nguyen V, Goyal M, Gupta V. Cationically modified inhalable nintedanib niosomes: enhancing therapeutic activity against non-small-cell lung cancer. Nanomedicine. 2022;17:935–58.
Gurpreet K, Singh SK. Review of nanoemulsion formulation and characterization techniques. Indian J Pharm Sci. 2018;80:781–9.
Kumar M, Bishnoi RS, Shukla AK, Jain CP. Techniques for formulation of nanoemulsion drug delivery system: A review. Prev Nutr Food Sci. 2019;24:225–34.
Amani A, York P, Chrystyn H, Clark BJ. Evaluation of a nanoemulsion-based formulation for respiratory delivery of budesonide by nebulizers. AAPS PharmSciTech. 2010;11:1147–51.
Wahgiman NA, Salim N, Rahman MB, Ashari SE. Optimization of nanoemulsion containing gemcitabine and evaluation of its cytotoxicity towards human fetal lung fibroblast (MRC5) and human lung carcinoma (A549) cells. Int J Nanomedicine. 2019;14:7323–38.
Arbain NH, Salim N, Wui WT, Basri M, Rahman MB. Optimization of quercetin loaded palm oil ester based nanoemulsion formulation for pulmonary delivery. J Oleo Sci. 2018;67:933–40.
Kim JE, Park YJ. Improved antitumor efficacy of hyaluronic acid-complexed paclitaxel nanoemulsions in treating non-small cell lung cancer. Biomol Ther. 2017;25:411–6.
Duan Y, Dhar A, Patel C, Khimani M, Neogi S, Sharma P, et al. A brief review on solid lipid nanoparticles: Part and parcel of contemporary drug delivery systems. RSC Adv. 2020;10:26777–91.
Mishra V, Bansal KK, Verma A, Yadav N, Thakur S, Sudhakar K, et al. Solid lipid nanoparticles: Emerging colloidal nano drug delivery systems. Pharmaceutics. 2018;10:191. https://doi.org/10.3390/pharmaceutics10040191.
Bakhtiary Z, Barar J, Aghanejad A, Saei AA, Nemati E, EzzatiNazhadDolatabadi J, et al. Microparticles containing erlotinib-loaded solid lipid nanoparticles for treatment of non-small cell lung cancer. Drug Dev Ind Pharm. 2017;43:1244–53.
Rosiere R, Van Woensel M, Gelbcke M, Mathieu V, Hecq J, Mathivet T, et al. New folate-grafted chitosan derivative to improve delivery of paclitaxel-loaded solid lipid nanoparticles for lung tumor therapy by inhalation. Mol Pharmaceutics. 2018;15:899–910.
Wang JL, Hanafy MS, Xu H, Leal J, Zhai Y, Ghosh D, et al. Aerosolizable siRNA-encapsulated solid lipid nanoparticles prepared by thin-film freeze-drying for potential pulmonary delivery. Int J Pharm. 2021;596:120215. https://doi.org/10.1016/j.ijpharm.2021.120215.
Khosa A, Reddi S, Saha RN. Nanostructured lipid carriers for site-specific drug delivery. Biomed Pharmacother. 2018;103:598–613.
Fang CL, Al-Suwayeh SA, Fang JY. Nanostructured lipid carriers (NLCs) for drug delivery and targeting. Recent Pat Nanotechnol. 2013;7:41–55.
Haider M, Abdin SM, Kamal L, Orive G. Nanostructured lipid carriers for delivery of chemotherapeutics: a review. Pharmaceutics. 2020;12:288. https://doi.org/10.3390/pharmaceutics12030288.
Garbuzenko OB, Saad M, Pozharov VP, Reuhl KR, Mainelis G, Minko T. Inhibition of lung tumor growth by complex pulmonary delivery of drugs with oligonucleotides as suppressors of cellular resistance. Proc Natl Acad Sci. 2010;107:10737–42.
Patlolla RR, Chougule M, Patel AR, Jackson T, Tata PN, Singh M. Formulation, characterization and pulmonary deposition of nebulized celecoxib encapsulated nanostructured lipid carriers. JCR. 2010;144:233–41.
Tang Y, Zhang L, Sun R, Luo B, Zhou Y, Zhang Y, et al. Pulmonary delivery of mucus-traversing PF127-modified silk fibroin nanoparticles loading with quercetin for lung cancer therapy. AJPS. 2023;18:100833. https://doi.org/10.1016/j.ajps.2023.100833.
Gonsalves A, Sorkhdini P, Bazinet J, Ghumman M, Dhamecha D, Zhou Y, et al. Development and characterization of lung surfactant-coated polymer nanoparticles for pulmonary drug delivery. Biomater Adv. 2023;150:213430. https://doi.org/10.1016/j.bioadv.2023.213430.
Liu S, Sun X, Lu H, Chen D, Li X, Li L, et al. Fullerene-based nanocomplex assists pulmonary delivery of siRNA for treating metastatic lung cancer. Nano Today. 2023;50:101878. https://doi.org/10.1016/j.nantod.2023.101878.
Zimmermann CM, Baldassi D, Chan K, Adams NBP, Neumann A, Porras-Gonzalez DL, et al. Spray drying siRNA-lipid nanoparticles for dry powder pulmonary delivery. JCR. 2022;351:137–50.
Gao C, Zhang L, Xu M, Luo Y, Wang B, Kuang M, et al. Pulmonary delivery of liposomes co-loaded with SN38 prodrug and curcumin for the treatment of lung cancer. Eur J Pharm Biopharm. 2022;179:156–65.
Huang S, Huang T, Meijia WU. Uses of ergosterol combined with gefitinib, preparation methods of liposome and freeze-dried powder thereof. US Patent 11123353, 2021.
Wang H, Yin R. Erlotinib sustained-release preparation for treating non-small cell lung cancer. China Patent 111617048, 2023.
Rajadurai M, Kulkarni P, Sevilimedu A, Saxena U. Magnetic nanoparticle formulations for targeted delivery of drugs to lungs for treatment of pulmonary diseases. Indian Patent 201741005560, 2018.
Wei Z, Weihua L, Fan L. Targeting beta-cyclodextrin grafted chitosan ion cross-linked nanoparticle drug carrying system, and preparation method and applications thereof. China Patent 108721251, 2020.
Zhu D-M, Guoqiang C. Dual loaded liposomal pharmaceutical formulations. European Patent 3265063, 2018.
Zhijian H, Pengcheng W, Weifeng X, Liangliang C, Haoyuan L. Crizotinib and 17-AAG composite polymer nano-micelle injection as well as preparation method and application thereof. China Patent 109512821, 2021.
Youn YS, Choi SY, Hochoi S, Choi SH, Soochoi J, Soo J. Self-assembling albumin nanoparticle for combined therapy of lung cancer and manufacturing method of same. Republic of Korea Patent 1015853450000, 2016.
Yonghong Z, Xun Z. Lung cancer treatment bufalin liposome preparation and preparation method thereof. China Patent 103462897, 2013.
Juergen B, Shimon B, Nir D, Nour K., Oshrat H-F. Nanoparticles for targeted delivery of active agents to the lung. European Patent 2257312, 2010.
Carter KC, Mullen AB and Ferro VA. Pulmonary drug delivery with vesicles comprising non-ionic surfactants. WO Patent 2009156706, 2009.
Wang Y, Ma R, Sun S, Hu Z, Li C, Lou M, et al. Modeling of inhaled corticosteroids delivery for topical croup treatment in pediatric upper airways. J Drug Deliv Sci Technol. 2023;85:104613.
Acknowledgements
The authors would like to acknowledge the Faculty of Pharmacy and Research Cell, Integral University, for continuous support and guidance during the writing process of this work.
Author information
Authors and Affiliations
Contributions
Both authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Nargis Ara and Abdul Hafeez. The first draft of the manuscript was written by Nargis Ara, and Abdul Hafeez reviewed and commented on previous versions of the manuscript. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Theme: Inhaled Drug Delivery of Biologics for Therapeutic and Vaccination
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ara, N., Hafeez, A. Nanocarrier-Mediated Drug Delivery via Inhalational Route for Lung Cancer Therapy: A Systematic and Updated Review. AAPS PharmSciTech 25, 47 (2024). https://doi.org/10.1208/s12249-024-02758-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-024-02758-1