ABSTRACT
Inhalation is a promising and challenging method in pharmaceutical and biological science research. A stable environment is critical in dynamic inhalation administration. However, the establishment of a stable inhalation system is very challenging. Indacaterol glycopyrronium bromide inhalation powder (IM/GP mixed powder) is composed of indacaterol maleate and glycopyrronium bromide powder to treat chronic obstructive pulmonary disease (COPD). The aim of this study is to build suitable inhalation conditions and then to evaluate the pulmonary safety of this drug in Sprague-Dawley(SD) rats. In the research, through the coordination of the atomization flow, air pump flow, and scraper speed, aerosols were stabilized at 200 ± 20% mg/m3, and then rats were nose-only administered with the IM/GP mixed powder, Ultibro, and lactose-magnesium stearate mixed powder at 2.6 mg/kg/day for 14 days and 14 days of recovery period, respectively. After exposure, hematology, inflammatory cytokines in rats bronchoalveolar lavage fluid (BALF) and serum, histopathological examination were performed. Results showed that the stability of powder aerosols can be realized under the atomization generation flow: 10 L/min, sampling flow: 2 L/min, system pumping capacity: 10 L/min and powder scraper speed: 8–10 L/min, and there were no significant adverse effects on body weight, clinic signs, hematology, and pathology in rats. Overall, the results suggested that the IM/GP mixed powder inhalation at the dose of 2.6 mg/kg/d can be reached when the aerosol concentration is within the range of 200 ± 20% mg/m3, and there were no pulmonary toxicity effects in rats.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Nowadays, inhalation therapy is considered to be the most promising method of administration for many drugs over oral and other gastrointestinal routes (1). Dry powder inhalation (DPI), as one of the effective lung delivery media, has the following unique advantages: stable physical and chemical properties at room temperature, low sensitivity to microbial growth, and adjustable single inhalation dose (2). For DPI preparations, the biggest challenge is their aerodynamic features. The mass median aerodynamic diameter (MMAD) and the geometric standard deviation (GSD) are generally considered to be the most important particle-related factors affecting aerosol deposition. Generally, MMAD should be less than 6 μm, and only within 1–5 μm can aerosol particles be widely distributed in the lungs to achieve the purpose of treatment (3). Thus, these characteristics have increased the technical requirements of the manufacturing process. Besides, nebulizers and metered-dose inhalers (MDI) are also widely used on the clinical market to effectively deliver medicine molecules to the human lungs (4,5,6).
In the current preclinical research of inhaled preparations, intratracheal instillation, oropharyngeal aspiration, and tracheotomy are traditional methods used by researchers to accurately deliver drugs to the target organs (7,8,9,10). However, during the administration, animals need to be anesthetized passively. In addition, these operations are traumatic to animals in a certain extent. Therefore, the dynamic inhalation exposure method has gradually become the preferred trend in inhalation research due to that this exposure model can simulate the real inhalation states in a large degree and reduce some other external damage factors to the animal (11).
Currently, various types of dynamic inhalation systems have been developed including whole body, head-only, and nose-only exposure types to meet different experimental needs (12, 13). Wong pointed out that animal environment, exposure environment, inhalation dose, and biological response of individual animals are the main factors in dynamic inhalation experiments (14). Among them, exposure environment and inhalation dose are the two most difficult parts to maintain balance in preclinical study. First, the exposure environment affects the inhaled dose. Furthermore, it is difficult to evaluate the accurate dose of drugs delivered and deposited during exposure, because the inhaled dose is related to the amount of air exposed to the inhaled respiratory system as well as the test substances that are efficiently absorbed or deposited (11, 14, 15). Besides, the main mechanisms of fine particulate matter deposition in the respiratory tract include deposition, impact and diffusion (16). Although the dose of the drug is very important for the evaluation of its efficacy and toxicity, there is a lack of ways to fully estimate the deposited dose of inhaled drugs in the lungs (17). Nevertheless, this challenge can be addressed by creating a stable inhalation exposure environment, generating stable and uniform aerosols, and choosing appropriate methods to estimate dose. At present, the evaluation of improved new inhalation drugs follows the principle of case by case, and therefore there are no systematic and universal guidelines for toxicology testing (18). All in all, a feasible and stable inhalation exposure method is the prerequisite for achieving the delivery dose of inhaled drugs, laying the basis for scientific preclinical evaluation of inhaled preparations.
Chronic obstructive pulmonary disease (COPD) is the main disease in the chronic respiratory system (19). It is characterized by a persistent airflow limitation with dyspnea, cough, and sputum production symptoms (20). This non-communicable disease is affecting over 10% of the adult population and causing 3.2 million deaths annually worldwide (21). So far, the main drugs for the treatment of COPD include Inhaled Bronchodilators, β2-Agonists, Anticholinergics/Antimuscarinics/Muscarinic Antagonists, Inhaled Corticosteroids (ICS)(22).
Indacaterol brominated inhalation powder spray mixed powder (IM/GP mixed powder) is a generic drug of Ultibro (Novartis) to treat COPD through combination therapy of bronchodilators. In recent years, increasing evidence has proved that bronchodilator drugs alone is not effective enough to control COPD symptoms (23). There are studies showing that combination therapy has better efficacy in the treatment of COPD (22, 24, 25). The 2020 Global Initiative for Chronic Obstructive Lung Disease (GOLD) report stated that combining bronchodilators with different mechanisms and durations of action can increase the degree of bronchodilation with lower risks of side effects compared to increasing the dose of a single bronchodilator (26).
The present research work was carried out to build suitable inhalation conditions through optimizing the parameter configuration of each device with an aim to achieve the stability of the aerosol and meet up a series of standard requirements of preclinical testing. The improved inhalation exposure conditions were evaluated and verified through the application of pulmonary safety evaluation after inhalation of IM/GP mixed powder.
MATERIALS AND METHODS
Chemicals and Reagents
Indacaterol glycopyrronium bromide inhalation powder (IM/GP mixed powder, 200501-B1-103942) was synthesized by Respirent Pharmaceuticals Co., Ltd(Fig. 1). Capsules for indacaterol glycopyrrolate inhalation powder mist (Ultibro, STU97) were developed by Novartis Pharmaceuticals in Switzerland. Lactose-magnesium stearate mixed powder-magnesium stearate mixed powder (LAC, 10392601) was obtained from Respirent Pharmaceuticals Co., Ltd.
Animal Husbandry
Healthy male and female Sprague-Dawley(SD) rats (6–7 weeks) were supplied by Vital River laboratory (Beijing, China). The body weight range at the start of treatment was 256–280 g for males and 226–245 g for females. They were housed for a 7-day acclimation period before study. Environmental conditions were maintained as temperature within 23 ± 3°C, humidity within 40 ± 10%, and 12 h light/dark cycle. Animals had free access to standard rat chow and water.
This study has been carried out in compliance with the guidelines from the China Food and Drug Administration (CFDA). The animal study was approved by the Institutional Animal Care and Use Committee (IACUC) of Jiangsu Center for Safety Evaluation of Drugs, Nanjing Tech University. Animals were maintained in accordance with the Guide for the Care and Use of Laboratory Animals (27, 28).
Doses and Treatment Schedule
Sprague-Dawley (SD) rats (10/sex/group) were selected using a computerized randomization procedure based on body weight. Animals were exposed to IM/GP mixed powder (test group), Ultibro (positive group), and LAC (vehicle group) for 20 min for 14 days at the concentration of 200 mg/m3 in the nose-only inhalation system.
Equipment and Inhalation Environment for Dry Powder Administration
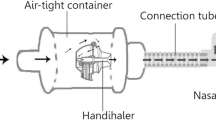
Inhalation exposure in rats was performed using the Tow Systems Nose-Only Exposure Units (Tow Intelligent Technology Limited, China), which is a dynamic external inhalation exposure system jointly developed by our research team and Shanghai Tawang Technology Co., Ltd (Fig. 2).
DPI in powder state can be turned into tablet by independent tablet press (Tow Intelligent Technology Limited, China) and then put into the dry powder generator device, which is composed of 2 independent Wright dust feeders. The inhalation equipment is 24 ports nasal-only inhalation exposure tower. Each animal was placed in a single plastic chamber with a diameter of 5 cm. Each chamber has its own air supply and exhaust port. One end of it can be removed and inserted with a nose piece. The chamber served as holding area for the animal accommodation and aerosol exposure. The effective cavity volume of the exposed tower is 0.0013 m3, and the total amount of air flow through the exposed tower is 27 L/min.
During the experiment, the whole exposure system temperature was maintained at 20–26°C, the oxygen concentration was ≥ 19%, relative humidity was 30–70%, and the carbon dioxide concentration was ≤ 1%.
Inhalation and Exposure Monitoring
Aerosol concentrations were monitored in real time during each exposure period (Tow Daco Software). Besides, the 0.22-μm high-purity quartz membrane filter (Munktell, Sweden) was chosen to collect dry powders from single exposure port and through filter sampling to evaluate the aerosol concentration. After sampling, the filters were weighed on a microbalance (Yingzhan Mechanical and Electrical Enterprise Co., Ltd., China). Aerosol concentration was calculated using the following formula (29):
Particle Size Analysis of Dry Powders
Particle size was monitored using an aerodynamic particle sizer (Winner, China), which measures the aerodynamic diameter of individual particles based on the particle’s velocity immediately downstream of a flow accelerating nozzle. One side of the detector was connected to the exposure tower, and the other side was connected to the computer. The particle sizer was connected to the inhalation exposure tower. The MMAD and GSD were determined by accompanying computer software (Winner311XP Software, Winner Inc, China). Particle size was determined for each group at three distinct intervals on the sampling experiment day: D1, D7, D14.
Observation and Measurements
Mortality and clinical signs were evaluated daily from the beginning of the quarantine period. Each animal was examined every week for any change in body weight, food consumption and every day for behavior. Observations included, but were not limited to the following: changes in skin and fur, eyes and mucous membranes, respiratory, circulatory, autonomic and behavior patterns.
Broncho-Alveolar Lavage Fluid (BALF) and Serum Analysis
Rats were euthanized with 20% urethane (Sinopharm Chemical Reagent Co., Ltd, China) via intraperitoneal injection. The right portion of the lungs of rats was immediately lavaged twice with 5 mL of Ca2+, Mg2+ free phosphate buffered saline (Qidu Pharmaceutical Co., Ltd., China). About 90% of the total volume instilled was retrieved, and the volume was similar in all groups. The collected BAL fluids were then centrifuged at 500 g for 7 min at 4°C. Pro-inflammatory cytokine, i.e., tumor necrosis factoralpha (TNF-α) and pro-fibrotic cytokines, i.e., interleukin-6 (IL-6), interleukin-6 (IL-8), and macrophage inflammatory protein 1α (MIP-1α/CCL3) levels were quantified in BALF using ELISA kits according to the manufacturer instructions (Beyotime, China). The amount of cytokine was estimated using the standard curve obtained from cytokine standards included in the kits. All these inflammation-related cytokines have also been tested in the serum. In addition, the total protein concentration in BALF was determined by BCA protein assay kit (Beyotime, China); the calculation method was the same as above.
Hematological Analysis
From the anaesthetized rats, 0.5 mL of blood collected from the abdominal artery was added to a blood collection tube containing an anticoagulant (K2EDTA) and analyzed using a hematology analyzer (SIEMENS, ADVIA-2120i). Plasma was separated from the collected blood by placing 2 mL in a tube containing 3.2% sodium citrate and centrifuging at 2000 rpm for 10 min.
For the rat study, absolute and relative counts of basophilic leukocyte (BASO), absolute and relative counts of eosinophil (EOS), hematocrit (HCT) level, hemoglobin (HGB) level, lymphocyte level (LYM), mean corpuscular hemoglobin (MCH) level, mean corpuscular hemoglobin concentration (MCHC), mean corpuscular volume (MCV), mean plate volume (MPV), monocyte (MONO) level, neutrophil (NEU) level, platelet (PLT) count, platelet volume distribution width (PDW), total count of white blood cell (WBC) count, WBC count, and red blood cell (RBC) were measured at Day 14.
Histopathological Analysis
A complete gross necropsy was conducted on all animals by visual inspection at the end of the exposure period (Day 14) and the recovery phase (Day 28). The extracted nasal mucosa, throat, trachea, bronchus, lung, and tongue were fixed in 10% neutral buffered formalin and embedded in paraffin. The embedded tissue blocks were cut into 3-μm-thick sections and stained with hematoxylin and eosin. The stained sections were examined using a light microscope (OLYMPUS, Japan).
Statistical Analysis
All the statistical data were presented as mean ± SEM. Statistical analysis was done by performing one-way analysis of variance, statistical significance was determined by Bonferroni’s t test using SPSS 18 software (Chicago, USA), and p values were calculated. A p value < 0.05 was considered significant.
RESULTS
Inhalation Exposure Environment
The entire of the exposure system consists of 5 parts: sample generator, exposure equipment, analysis module, control module, and exhaust gas treatment module (Fig. 2). During the experiment, the temperature of the entire exposure system was maintained at 20–26°C, the oxygen concentration was ≥ 19%, the relative humidity was 30–70%, and the carbon dioxide concentration was ≤ 1% (Fig. 3).
Target Concentration
During the experiment, the exposure system was operated under these parameters: the atomization generation flow rate: 10 L/min, sampling flow rate: 2 L/min, system pumping capacity: 10 L/min, and powder scraper speed: 8–10 L/min, which managed to stabilize aerosols. Good temporal concentration stability was achieved during 14-day inhalation exposure (Fig. 4).
After 14 days of nose-only continuous inhalation exposure, the results of filter sampling are as follows: IM/GP mixed powder, Ultibro, and lactose-magnesium stearate mixed powder groups were 6 ± 0.6 mg, 6 ± 0.5 mg, 6.3 ± 0.2 mg on the D1, D7, and D14, respectively (Table 1). During the inhalation exposure, the concentration of IM/GP mixed powder, Ultibro, and lactose-magnesium stearate mixed powder (as mg/m3) was determined gravimetrically, and the data showed that the mean actual concentrations for IM/GP mixed powder, Ultibro, and lactose-magnesium stearate mixed powder were 198.28 ± 21.75 mg/m3, 196.65 ± 12.75 mg/m3, 204.91 ± 10.98 mg/m3, respectively (Table 1).
Particle Size Distribution of IM/GP Mixed Powder in the Nose-Body Exposure Chamber
In our experiment, MMAD of the aerosols was 3.136, 3.012, 2.465, and 3.279 μm, respectively, and the GSD was 1.546, 1.58, 1.549, and 1.511, on the day before the formal test, first day, the seventh day, and the last day of the experiment (Fig. 5). The MMAD and GSD were within the range recommended by the Organization for Economic Cooperation and Development (OECD, 2018) (30).
Animal Observations
None of the rats in the test groups died during the exposure period. Nasal discharge, deep breathing, asthma, cough, asphyxiation, and other abnormal signs were not observed in the three groups (Table S1). The body weight of rats showed a gradual increase compared with the first day of the inhalation exposure, indicating that IM/GP mixed powder did not have any adverse effects on food intake (Table 2).
Hematology
Among all rats in the test groups, BASO, BAS%, NEU, and NEU% showed statistically significant decreases in the IM/GP mixed powder group compared with that of the vehicle control group rats during the exposure period. LYM% showed a statistically significant increase in the IM/GP mixed powder group compared with that of the vehicle control group rats during this period. There were no significant differences between the test group and control group, and all detection indicators were within the normal range (Table 3).
Analysis of BALF and Serum
IL-1β, IL-6, TNF-α are the critical pro-inflammatory cytokines in the development of acute lung injury (ALI)(31). MIP-1alpha/CCL3 is also a pro-inflammatory cytokine that promotes the metastatic activity of a variety of inflammatory cells and also increases the secretory activity of inflammatory cells (32). In BALF and serum, the concentrations of IL-6, TNF-α, and MIP-1alpha/CCL3 did not show statistically significant changes after exposure in the test substance, but the concentration of IL-1β between the test group and positive control group showed significant decrease trends (Fig. 6a–d). In addition, the increase of protein concentration in BALF is an important marker of damage to the barrier of alveolus capillary in lungs (33). There were no significant differences in total protein concentration in BALF (Fig. 6e).
Inflammatory cytokines analysis in BALF and serum (a–d) and protein concentration in BALF (e). The values are expressed as mean ± SEM (n=3 males and 3 females per group). Significantly different from positive control by Dunnett test: *p < 0.05, **p < 0.01, ***p < 0.0001. Significantly different from positive control by Dunn Rank Sum test: *p < 0.05, **p < 0.01, ***p < 0.0001. Significantly different from vehicle control by Dunnett test: #p < 0.05, ##p < 0.01, ###p < 0.0001. Significantly different from vehicle control by Dunn Rank Sum test: #p < 0.05, ##p < 0.01, ###p < 0.0001
Gross and Histopathological Findings
No gross changes were found in the tongue, upper jaw, nose, pharynx, throat, trachea, bronchitis, left, and right lung leaves of rats. Then, H&E staining was used in this study to access the pathological changes. Histopathological examination showed that mild inflammatory cell infiltration occurred in tracheal mucosa layer in animal no. 1102 and in main bronchial mucosa layer in animal no. 1201. The local respiratory tract (nose, throat, trachea, main bronchus) of other animals has complete tissue structure, no degeneration or necrosis of epithelial cells in the mucosa, no edema and inflammatory cell infiltration in the submucosa. There were no obvious inflammatory cell infiltration, interstitial edema, interalveolar and interstitial patchy hemorrhage, and interalveolar septal thickening in lung tissues. In addition, there were no abnormal symptoms in tongue as well (Fig. 7).
DISCUSSION
Nowadays, inhalation therapy has been used as the main treatment method for patients with respiratory diseases (34). This is due to the fact that the inhalation route offers a direct part to the target organs, avoids the first pass effect in the liver, is not affected by plasma protein binding, and has fewer systemic complications, etc. (35). In this study, IM/GP mixed powder is a generic version of ULTIBRO (Novartis), which consists of 0.19% glycopyrronium (C19H28BrNO3) and 0.42% indacaterol (C24H28N2O3·C4H4O4). This dry powder formulation is used in combination with bronchodilators to treat COPD, with the clinically planned dosage of the test substance once a day, one capsule of medicine (25 mg powder/capsule) inhaled each time. In this study, rats received test and control article by nose-only inhalation at target doses of 2.6 mg/kg/d, which equal to about 1.2 times the recommended human dose on a mg/m2 basis (human body weight as 70 kg, rat body weight as 250 g) according to the conversion of animal body surface area: human vs rat ≈ 1:6 (36). Therefore, 2.6 mg/kg/d is the target dose for inhaled administration in our study.
At present, most of the inhalation studies that have been carried out mainly focus on the application of inhalation equipment, but there are few studies on the improvement and optimization of inhalation stability (37, 38). To achieve the stability of the powder aerosol in the inhalation environment, not only is it necessary to maintain the stability of the inside of the exposure tower, but also the animal exposure tower should also closely cooperate with the air pump and the powder generating device. The former is to ensure that rats can breathe steadily in the exposure chamber, and the latter is to produce the aerosol concentration required to inhale the target dose. Before the administration, the operator used the Concentration Tester (Tow Intelligent Technology Limited, China) to randomly select two holes in the exposure tower to measure the aerosol concentration in the tower. When the exposure tower is in a stable state, the powder generating device was turned on, and the aerosol changes of the entire exposure system were monitored in real time. By adjusting the atomization generating flow rate, the system pumping volume, and the rotating speed of the scraper in the powder generating device, the aerosol concentration is within the range of 200 ± 20% mg/m3 to achieve the target administration dose of 2.6 mg/kg/day according to the previous mentioned formula.
The aerosol concentration affects the administered dose, and its concentration was monitored in real time on Tow Intelligent Software. In addition, this research chose a unique 0.22-μm high-purity quartz filter (Munktell, Sweden) with a saturation rate of 99.95%, which can simulate the deposition in animal lungs through sampling devices. And then the inhaled powders were weighed to calculate the aerosol concentration in exposure environment to further verify the stability of the inhalation process. In the process of optimizing the inhalation conditions, a common commercially available filter membrane was previously used. However, we found that when the drug delivery process was still in progress, the filter membrane had reached the saturated state and could not continue to deposit powder. Therefore, it was impossible to verify the actual inhaled dose. The results of this experiment show that under the conditions of atomization generation flow rate: 10 L/min, sampling flow rate: 2 L/min, system pumping capacity: 10 L/min, powder scraper speed: 8–10 L/min, and sampling time: 15 min with the cooperation of the inhalation exposure system and the dry powder generator, the concentration fluctuation of aerosol was kept within the range of 200 ± 20% mg/m3 during the exposure period.
Ideally, the deposition of DPs in the lung directly depends on the delivery system and physical properties of DPs. The stability of the delivery system gives rise to drug particles of appropriate sizes so that they can penetrate out of the oropharynx, larynx and be deposited in the lungs (39). The particle size, shape, and density are the most prominent physical properties of DPs, which can directly influence the lung deposition. As mentioned earlier, MMAD and GSD are important indicators for evaluating aerodynamic diameter. Specifically, only when the MMAD is within 1–5 μm can the aerosol particles be distributed in the lung and when MMAD is ≤ 3 μm can they widely be distributed in the lung. When aerosol particles are ≥ 6 μm, they are mainly deposited in the oropharynx, and when ≤ 1μm they are exhaled through exhalation (40). In addition, the larger the GSD is, the more aerosols are deposited in the respiratory tract. Generally, aerosol with GSD < 2 is ideal, and the aerosol particles should be as monodispersive as possible to increase deposition at the desired site and to improve the therapeutic effect (41). In this experiment, the particle size detection results showed that all particle sizes are within the ideal range and met the aerosol inhalation test requirements in the OECD TG412 (30).
To evaluate the respiratory toxic effects of repeated exposure to IM/GP mixed powder, the experiment carried out clinical observation, hematology, BALF analysis, inflammatory factor detection, and pathological detection. During the exposure period, nasal discharge, rale, and deep respiration were not observed in the three groups. These clinical signs are usually emergency airway reactions caused by external material stimulation. Besides, the body weight showed increasing trends, and the feed intake was in a normal state correspondingly. The hematological test results showed significant changes in the BASO, NEU, and LYM level when the test group is compared with the vehicle group. But there were no differences in hematological indicators between the test group and the positive control group. This can be explained by that the ingredients contained in IM/GP mixed powder are foreign substances to the respiratory system, so some hematological indicators fluctuate during the inhalation process. All the indicators of the three groups are within the normal value, which indicates that there is no hematological abnormality during IM/GP mixed powder inhalation. In the BALF analysis, there were no significant differences in IL-6, TNF-α, MIP-1 alpha/CCL3, and protein content. The concentration of IL-1β was significantly lower than that of the other two groups in BALF and serum. IL-1β is a pro-inflammatory factor, and this result may indicate that the drug may potentially have better anti-inflammatory effects. In the histopathological examinations, the inflammatory cell infiltration of the trachea and main bronchial mucosa lesions were individual cases, and the degree was relatively mild, indicating that there was no direct correlation between the test substance and the control substance. No obvious lesions were observed in each animal in each group during the recovery period. In short, neither the test substance nor the reference substance caused obvious local pathological changes in the respiratory mucosa.
Therefore, from all the above results, we explored stable inhalation conditions to assess the safety of IM/GP mixed powder, and the dose at 2.6 mg/kg/day did not cause pulmonary toxicity in rats, and there were no obvious adverse changes found.
CONCLUSION
In this study, the method for preclinical testing of dry powder inhalation preparation was established successfully. The stability of the improved nose-only inhalation exposure system was validated through monitoring environmental parameters and aerosol concentration changes, as well as comparison of the target dose with the actual dose in the evaluation process of the pulmonary toxicity of IM/GP mixed powder. Besides, the results indicated that the IM/GP mixed powder had no adverse symptoms in the respiratory system and was non-toxic to lung tissue. Furthermore, these experimental conditions and coordination parameters, which were established to achieve stable dry powder inhalation, can provide a good basis for the subsequent study of the tested drug. Moreover, the equipment can also be opted for investigations on inhalation toxicity of other substances in rodents with an excellent performance, which is favorable for future application.
Data availability
The data presented in this study are available upon request.
REFERENCES
Depreter F, Pilcer G, Amighi K. Inhaled proteins: Challenges and perspectives. Int J Pharm. 2013;447(1-2):251–80.
Sanchis J, Corrigan C, Levy ML, Viejo JL. Inhaler devices—from theory to practice. Respir Med. 2013;107(4):495–502.
Yang MY, Chan JG, Chan HK. Pulmonary drug delivery by powder aerosols. J Control Release. 2014;193:228–40.
Ibrahim M, Verma R, Garcia-Contreras L. Inhalation drug delivery devices: Technology update. Med Devices. 2015;8:131–9.
Pirozynski M, Sosnowski TR. Inhalation devices: From basic science to practical use, innovative vs generic products. Expert Opin Drug Deliv. 2016;13(11):1559–71.
Moon C, Smyth HDC, Watts AB, Williams RO 3rd. Delivery technologies for orally inhaled products: An update. AAPS PharmSciTech. 2019;20(3):019–1314.
Qiu Y, Liao Q, Chow MYT, Lam JKW. Intratracheal administration of dry powder formulation in mice. J Vis Exp. 2020;25(161):61469.
Morimoto Y, Izumi H, Yoshiura Y, Fujishima K, Yatera K, Yamamoto K. Usefulness of intratracheal instillation studies for estimating nanoparticle-induced pulmonary toxicity. Int J Mol Sci. 2016;17(2).
Nielsen TB, Yan J, Luna B, Spellberg B. Murine oropharyngeal aspiration model of ventilator-associated and hospital-acquired bacterial pneumonia. J Vis Exp. 2018;28(136):57672.
Kao RL, Huang W, Martin CM, Rui T. The effect of aerosolized indomethacin on lung inflammation and injury in a rat model of blunt chest trauma. Can J Surg. 2018;61(6):S208–S18.
Pauluhn J. Overview of inhalation exposure techniques: Strengths and weaknesses. Exp Toxicol Pathol. 2005;1:111–28.
Phalen RF, Mannix RC, Drew RT. Inhalation exposure methodology. Environ Health Perspect. 1984;56:23–34.
Świercz R, Wąsowicz W. The distribution and excretion of 1-Methylnaphthalene in rats exposed to 1-Methylnaphthalene by inhalation. Int J Occup Med Environ Health. 2018;31(6):763–70.
Wong BA. Inhalation exposure systems: design, methods and operation. Toxicol Pathol. 2007;35(1):3–14.
Pauluhn J, Mohr U. Inhalation studies in laboratory animals—current concepts and alternatives. Toxicol Pathol. 2000;28(5):734–53.
Cheng YS. Mechanisms of pharmaceutical aerosol deposition in the respiratory tract. AAPS PharmSciTech. 2014;15(3):630–40.
Kolli AR, Kuczaj AK, Martin F, Hayes AW, Peitsch MC, Hoeng J. Bridging inhaled aerosol dosimetry to physiologically based pharmacokinetic modeling for toxicological assessment: nicotine delivery systems and beyond. Crit Rev Toxicol. 2019;49(9):725–41.
Patil TS, Deshpande A, Shende PK, Deshpande S, Gaud R. Evaluation of nanocarrier-based dry powder formulations for inhalation with special reference to anti-tuberculosis drugs. Crit Rev Ther Drug Carrier Syst. 2019;36(3):239–76.
Viniol C, Vogelmeier CF. Exacerbations of COPD. Eur Respir Rev. 2018;27(147):0103–2017.
Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J, Celli BR, Chen R, Decramer M, Fabbri LM, Frith P, Halpin DMG, López Varela MV, Nishimura M, Roche N, Rodriguez-Roisin R, Sin DD, Singh D, Stockley R, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD Executive Summary. Am J Respir Crit Care Med. 2017;195(5):557–82.
GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med. 2017;5(9):691–706. https://doi.org/10.1016/S2213-2600(17)30293-X.
Mirza S, Clay RD, Koslow MA, Scanlon PD. COPD guidelines: a review of the 2018 GOLD report. Mayo Clin Proc. 2018;93(10):1488–502.
Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001;163(5):1256–76.
Rodriquez-Roisin R. Twenty years of GOLD (1997–2017). The origins. 2020. https://goldcopd.org/wp-content/uploads/2019/03/GOLD-Origins-Final-Version-mar19.pdf.
Horita N, Nagashima A, Kaneko T. Long-acting β-agonists (LABA) combined with long-acting muscarinic antagonists or LABA combined with inhaled corticosteroids for patients with stable COPD. Jama. 2017;318(13):1274–5.
Terry PD, Dhand R. Inhalation therapy for stable COPD: 20 years of GOLD reports. Adv Ther. 2020;37(5):1812–28.
Bolon B, Baze W, Shilling CJ, Keatley KL, Patrick DJ, Schafer KA. Good laboratory practice in the academic setting: fundamental principles for nonclinical safety assessment and GLP-compliant pathology support when developing innovative biomedical products. ILAR J. 2018;59(1):18–28.
Nussberger J, Aubert JF, Bouzourene K, Pellegrin M, Hayoz D, Mazzolai L. Renin inhibition by aliskiren prevents atherosclerosis progression: Comparison with irbesartan, atenolol, and amlodipine. Hypertension. 2008;51(5):1306–11.
Alexander DJ, Collins CJ, Coombs DW, Gilkison IS, Hardy CJ, Healey G, Karantabias G, Johnson N, Karlsson A, Kilgour JD, McDonald P. Association of Inhalation Toxicologists (AIT) working party recommendation for standard delivered dose calculation and expression in non-clinical aerosol inhalation toxicology studies with pharmaceuticals. Inhal Toxicol. 2008;20(13):1179–89.
OECD. Test No. 412: subacute inhalation toxicity: 28-day study, OECD guidelines for the testing of chemicals, section 4. Paris: OECD Publishing; 2018. https://doi.org/10.1787/9789264070783-en.
Riva DR, Magalhães CB, Lopes AA, Lanças T, Mauad T, Malm O, Valença SS, Saldiva PH, Faffe DS, Zin WA. Low dose of fine particulate matter (PM2.5) can induce acute oxidative stress, inflammation and pulmonary impairment in healthy mice. Inhal Toxicol. 2011;23(5):257–67.
DiPietro LA, Burdick M, Low QE, Kunkel SL, Strieter RM. MIP-1alpha as a critical macrophage chemoattractant in murine wound repair. J Clin Invest. 1998;101(8):1693–8.
Wang Y, Wang H, Zhang C, Zhang C, Yang H, Gao R, Tong Z. Lung fluid biomarkers for acute respiratory distress syndrome: A systematic review and meta-analysis. Crit Care. 2019;23(1):019–2336.
Barnes PJ, Burney PG, Silverman EK, Celli BR, Vestbo J, Wedzicha JA, et al. Chronic obstructive pulmonary disease. Nat Rev Dis Primers. 2015;1(15076):76.
Yoon HK, Park YB, Rhee CK, Lee JH, Oh YM. Summary of the chronic obstructive pulmonary disease clinical practice guideline revised in 2014 by the korean academy of tuberculosis and respiratory disease. Tuberc Respir Dis. 2017;80(3):230–40.
Reagan-Shaw S, Nihal M, Ahmad N. Dose translation from animal to human studies revisited. FASEB J. 2008;22(3):659–61.
Choi HY, Lee YH, Lim CH, Kim YS, Lee IS, Jo JM, Lee HY, Cha HG, Woo HJ, Seo DS. Assessment of respiratory and systemic toxicity of Benzalkonium chloride following a 14-day inhalation study in rats. Part Fibre Toxicol. 2020;17(1):020–0339.
Lim D, Jeong J, Song KS, Sung JH, Oh SM, Choi J. Inhalation toxicity of polystyrene micro(nano)plastics using modified OECD TG 412. Chemosphere. 2021;262(128330):13.
Labiris NR, Dolovich MB. Pulmonary drug delivery. Part I: Physiological factors affecting therapeutic effectiveness of aerosolized medications. Br J Clin Pharmacol. 2003;56(6):588–99.
Martin AR, Moore CP, Finlay WH. Models of deposition, pharmacokinetics, and intersubject variability in respiratory drug delivery. Expert Opin Drug Deliv. 2018;15(12):1175–88.
Zanen P, Go LT, Lammers JW. The efficacy of a low-dose, monodisperse parasympathicolytic aerosol compared with a standard aerosol from a metered-dose inhaler. Eur J Clin Pharmacol. 1998;54(1):27–30.
Acknowledgements
The authors thank Yangteng Ou (University of Cambridge, UK) for some proofreading work.
Funding
This work was supported by the National Natural Science Foundation of China under Grant (81773479), the National Major Science and Technology Projects of China under Grant (2017ZX09201002-004), and the research project of Jiangsu Commission of Health (H201634).
Author information
Authors and Affiliations
Contributions
ZF: methodology, investigation, validation, data curation, writing—original draft. BZ: methodology, validation, investigation, writing—review and editing. YL: methodology, investigation, validation, writing—review and editing. WS: methodology, investigation, formal analysis. YF: validation, resources, data curation. HL: formal analysis, writing—review and editing. DC: validation, writing—review and editing. KL: validation, writing—review and editing. XW: writing—review and editing. TX: writing—review and editing. WX: resources, writing—review and editing. QB: conceptualization, resources, writing—review and editing, supervision, project administration, funding acquisition. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Fan, Z., Zhou, B., Liu, Y. et al. Optimization and Application of an Efficient and Stable Inhalation Exposure System for Rodents. AAPS PharmSciTech 23, 50 (2022). https://doi.org/10.1208/s12249-021-02191-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-021-02191-8