Abstract
Background
Crohn’s disease is a chronic disease that causes remitting and relapsing inflammatory episodes in the transmural part of the gastrointestinal system. It usually affects young people. The study sought to establish whether ultrasound can visualize important/useful diagnostic features and complications of the disease in the same way that MR enterography (MRE) can. The study is a prospective cohort of 133 patients of various disease stages (active and in remission) who had previously been seen by a gastroenterologist. All patients underwent abdominal and pelvic ultrasound examinations, with each of the five intestine segments checked independently for thickening and active inflammation. Complications of fistulas, abscesses, and stenosis were evaluated. Findings at MRE together with ileocolonoscopic results were deemed the standard reference.
Results
Ultrasound showed wall stenosis ranging from 5 to 12 mm, with a mean ± SD of 7.73 ± 2.30. A single loop was present in 69.2% of cases. The ileum was the most heavily involved loop portion (66.7%). In 72.9% of patients, stenosis and dilatation were present, whereas 69.7% showed active inflammation. Complications such as fistulas and abscess formation (21.2%) were identified. Ultrasound was found to be an effective tool for detecting stenosis and dilatation in the examined patients, with sensitivity of 84% and 87%, and specificity of 91% and 97%, respectively. A high accuracy of 90.9% was demonstrated for abscess formation.
Conclusions
Ultrasound is a noninvasive method that is comparable to MRI for detecting damaged bowel segments and transmural complications such as bowel strictures, fistulas, and abscesses in Crohn’s disease patients. However, MR imaging is more comprehensive in providing detailed information about the disease's extent and activity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Crohn's disease (CD) is a chronic, inflammatory, and destructive bowel disease that can affect the entire digestive system. Medical therapy is the primary mode of treatment. Early diagnosis prevents medication noncompliance, disease activation, fistulas, strictures, and surgical procedures [1].
Beyond just identifying intestinal lesions, radiographic imaging can give important information about the thickening of the intestine wall, which helps the initial assessment and differentiates between fibrosis and active inflammation, which is crucial for choice of treatment [2].
MR enterography (MRE) has become the primary imaging technique for assessing CD in both children and adults at numerous institutions in the USA and around the world, owing to its noninvasive nature, superior soft tissue contrast, and lack of ionizing radiation [3].
For evaluating intra- and extra-luminal CD consequences, MR imaging is the gold standard diagnostic method (fistula, abscess, and stenosis) [4].
Ultrasound (US) is a widely used, inexpensive, radiation-free examination. Because of its narrow field of view, ultrasound is not usually considered for diagnosis for patients with CD. However, it can be helpful in evaluating perianal fistulas and gluteal abscesses. US relies on the use of high-frequency probes and offers two possible approaches: transperineal and endocavitary (using endoanal and/or endovaginal probes) [2].
This study represented a comparison between ultrasound and MR imaging. We aimed to detect diagnostic information for Crohn’s disease by ultrasound to prove the sufficiency of the modality and noninferior to MR imaging in some cases. Our goal was to reduce MRI examination rates with its high cost and contrast media-related complications in favor of ultrasound scans.
Methods
The research and ethical committee of the institution approved this prospective study. Prior to enrollment, all eligible patients provided their informed consent.
The research involved 133 patients across various disease stages (active and in remission). The gastroenterologist (15 years’ of experience in autoimmune gastrointestinal disease) conducted a clinical interview and physical examination on each patient at first. They did not participate in the imaging procedures, but he did set the clinical scoring and ordered any necessary laboratory investigations.
The Crohn’s disease activity index (CDAI) was used as a standard method to quantify the symptoms and record the degree of activity in patients with Crohn’s diseases at the time of study admission. CDAI scores have a range of 0–600. The higher your score, the more severe the disease according to the following interpretations score ranges: (1) 0–149: the disease in remission, (2) 150–220: active disease but mild, (3) 221–450: moderate to severe disease, (4) 451–600: more severe Crohn’s disease. In consideration to response mediation, presence of abdominal pain in the last 7 days, presence of an abdominal mass, patient's current hematocrit and extra-intestinal findings/complications (arthritis/arthralgias, iritis/uveitis, erythema nodosum/pyoderma gangrenosum/aphthous stomatitis, anal fissure/fistula/abscess/other fistula, fever/temperature > 100 °F/37.8 °C) [5].
Inclusion criteria
Regardless of age, cases of Crohn's disease (based on clinical, biologic, and clinical–biologic index scores) were referred for imaging: (1) to assess the whole intestinal involvement (not only for the initial evaluation), (2) provide data to distinguish active disease from fibrosis in bowel wall thickening, (3) define information on the surrounding tissues, where complications arise needed to establish the proper diagnostic path.
Exclusion criteria
Patients with unproven Crohn's disease according to the clinical, biologic, and clinical–biologic index were excluded.
Equipment
All study participants performed the procedures: (1) standard abdominal ultrasonography and (2) MRI imaging.
Abdominal ultrasound
The examination was conducted in the supine position using a linear 5- to 10-MHz probe or a 3.5-MHz convex probe utilizing a PowerVision 5000 scanner (Toshiba, Tokyo, Japan). A method of graduated compression was applied.
Using a unique preset intended for the detection of low-velocity flow in the intestinal wall (filter at low setting, 50 Hz, and lowest velocity scale, 2 cm/s), color Doppler flow parameters were adjusted for maximum sensitivity and remained consistent throughout the tests.
MRI imaging
A 1.5-T MRI machine (Gyroscan, Philips, Best, The Netherlands) was used to conduct the scan. Patients were instructed to fill the distal ileum and cecum with 45 mL of sodium phosphate solution (a hyperosmolar solution) diluted in 250 mL of water and an additional 750 mL of water starting 45 min before imaging. Creatinine levels and glomerular filtration rate (eGFR) were performed before examination to ensure safe administration of contrast agent.
During breath hold, a balanced fast-field echo (B-FFE) sequence was conducted in both axial and coronal orientations. Following GD-DTPA (dose of 20 mL), a coronal and axial-oriented T1-weighted spoiled gradient echo (SGRE) sequence was added.
Image analysis
Two experienced radiologists (15- and 20-years’ of experience in GIT imaging), who were not aware of each patient's pathological information, blinded about each other outcome and separately examined the 133 patients by ultrasound and MR imaging.
Conventional ultrasound images
The thickness and vascularity pattern of the intestinal wall were assessed during the sonographic examination. Any bowel wall thickness greater than 3 mm was deemed abnormal.
Features diagnostic of Crohn’s disease included: (1) involvement of all bowel wall layers (transmural), (2) disrupted layers with loss of mural stratification, (3) inflamed fat presented by increased echogenicity and thickening of the root of the mesentery, (4) skip lesions, (5) presence of complications as abscess, fistula, or obstruction.
Color Doppler ultrasound is used to evaluate intestinal mural blood flow with the parameters: (1) the lowest possible pulse repetition frequency without aliasing and color gain of 40 or the highest color Doppler gain settings without flash artifacts. Velocity is set at 2–7 cm/s per second (cm/s). Bowel loops are interrogated for presence or absence of mural blood flow using a large region of interest (ROI) to compare perfusion of adjacent bowel loops with color Doppler.
Rating for color Doppler flow for the degree of vascularization was classified according to Limberg score following Goertz et al. [6]: zero score if there was no wall thickening nor color Doppler signal. In grades 1–4 there is mural thickening, plus no color Doppler signal (grade 1), or spots of color Doppler signals (grade 2), or longer stretches of color Doppler signals (grade 3) or strong color Doppler signals in both the bowel wall and surrounding mesenteric fat (grade 4).
Grades 3 and 4 were merged and regarded as sonographically active disease for statistical analysis. One Doppler-trained radiologist (10 years’ of experience) conducted the examination who was unaware of the disease's current state of extension or activity.
MRI imaging
The five intestine segments (corresponding to the five types of Crohn’s disease) were looked at independently by each radiologist: (1) the end of the small intestine (ileum) and a portion of the large intestine (colon), (2) the last section of the small intestine (ileum), (3) the stomach and the start of the small intestine (duodenum), (4) the middle part of the small intestine (jejunum), (5) the colon.
The greatest thickness of the colon wall was measured. When the thickness was 3 mm or less, it was regarded as normal.
Additional criteria were assessed included the perivisceral fat and bowel wall post-contrast enhancement and signal intensities on T2. Mural enhancement on the post-contrast T1WI was recorded for assessment of hypervascularity and assigned four grades to correlate with the “Limberg score” grading used for color Doppler into grade 1: iso-intense signal to normal bowel, grade 2: slightly hyperintense but markedly less than the signal elicited by post-contrast vascular enhancement, grade 3: signal is markedly higher than the normal bowel wall signal but still less than the hyperintense vascular signal, and grade 4: hyperintensity comparable to the signal of vascular structures. Stenosis, fistulas, and abscesses were also recorded.
Statistical analysis
The data were collected, edited, coded, and entered into IBM SPSS version 23. When parametric, quantitative data were reported as mean, standard deviation, and range. Additionally, qualitative characteristics were reported as numbers and percentages.
When the predicted count in any cell was less than five, the Chi-square test was used to compare groups with qualitative data. Otherwise, the Fisher exact test was used instead.
In the qualitative mood, the receiver operating characteristic curve (ROC) was employed as a gold standard to determine the diagnostic accuracy of ultrasonography on MRI.
The confidence interval was set at 95%, and the acceptable margin of error was 5%. Thus, the p value was deemed significant as follows: p > 0.05: nonsignificant; p < 0.05: significant; p < 0.01: highly significant.
Results
The study had 133 patients aged 14–59 years old, with a mean of 33.00 ± 13.73 SD. Male patients (n = 81, 60.9%) had a higher illness prevalence than female patients (n = 52, 39.1%).
Complaints included abdominal pain (39.4%), diarrhea (36.4%), rectum bleeding (12.1%), weight loss (6.1%), constipation (3.0%), and an enterocutaneous fistula (3.0%).
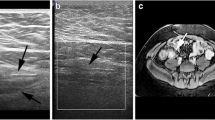
Ultrasound revealed wall thickening ranging from 5 to 12 mm, with a mean ± SD of 7.73 ± 2.30, Figs. 1, 2, 3, and 4. In 69.2% of cases one loop was affected, whereas the remaining 30.8% had two affected loops. The ileum was the most heavily involved loop portion (66.7%), followed by the ileum and caecum (15.2%), ileum and jejunum (9.1%), and ileum and colon (9.1%). In 72.9% of patients, stenosis and dilatation were present, whereas 69.7% showed active inflammation, Figs. 2 and 3.
A 25-year-old woman with Crohn’s disease presented with bleeding per rectum and constipation. A and B Ultrasound shows inflamed echogenic mesenteric fat and thickened walls of the distal ileal loop with a maximum thickness of 8 mm (arrow seen in B image). Magnetic resonance enterography in C coronal T2 WI’s confirmed bowel wall thickening. D Axial T1 post-contrast WI’s showing thickened enhancing walls of the distal ileal loops due to active disease
A 14-year-old female patient with Crohn’s disease. Longitudinal ultrasound images showing mural thickening in the terminal ileum in (A), the jejunum has a dilated proximal loop in (B), and Doppler reveals grade 2 vascularity, indicating active inflammation in (C). D Axial T2-weighted, E coronal T2 weighted, and F post-contrast MR images revealing grade 2 active inflammation in the distal ileum, at the ileocecal junction, and in the distal terminal ileum (10 cm)
A 57-year-old man with Crohn's disease affecting a long segment of the ileum. A Axial and B longitudinal ultrasound images showing a thickened ileal segment. C Doppler reveals increased vascularity (Limberg grade 3) due to active disease. MR images confirmed these suspicions: D The bowel wall was found to be hyperintense in the T2 weighted coronal view and E stratified in the T1 weighted axial view
A 32-year-old man reported abdominal pain and fever. A Long-axis ultrasound image of a thickened small bowel segment with a poorly defined hypoechoic mass (arrows). B The corresponding contrast-enhanced fat-saturated T1-weighted MR image demonstrates marked terminal ileal wall thickening and hyperenhancement (arrows), as well as enhancement of the ill-defined peri-enteric soft tissue, which is consistent with phlegmon. Note, the small, unenhanced areas inside the inflammatory mass. No drainable fluid component has been identified.
Complications such as fistulas and abscess formation (21.2%) were identified.
In MR imaging, the number of loops with wall thickening varied: one loop in 51.1% (n = 68), two loops in 21.1% (n = 28), three loops in 24.1% (n = 32), and four loops in 3.7% (n = 5). The segment(s) involved were the ileum in 48.5%, the ileum, caecum, and colon in 15.2%, the ileum and cecum in 12.1%, the ileum, caecum, and appendix in 9.1%, the ileum and jejunum in 3.8%, the ileum, jejunum, and cecum in 3.8%, the ileum, cecum, colon, and rectum in 3.8%, and the distal ileum, ileojejunal junction, and cecum in 3.7%. Stenosis was discovered in 57.9% (n = 77), loop dilatation in 73.0% (n = 97), active inflammation in 94.0% (n = 125), fistulas in 36.1% (n = 48), and abscesses in 24.1% (n = 32).
There was no statistically significant difference between ultrasound and MR imaging results for stenosis, dilatation, or abscess, but there was a statistically significant difference between the two modalities for the number of loop segments (p value = 0.003). MR imaging had a significantly greater prevalence of active inflammation, and fistulas compared to ultrasound, with p values of < 0.001 and 0.003, respectively, Table 1.
There was no statistically significant relation found between signs of active inflammation (Figs. 2 and 3) and fistula (Figs. 5 and 6) detected by ultrasound and MR imaging (p values = 0.711 and 0.054, respectively). However, there was a statistically significant relation found between ultrasound and MR imaging results regarding stenosis, dilatation, and abscess (p values < 0.001, < 0.001, and < 0.001, respectively).
A 37-year-old woman presenting with right iliac pain. A Ultrasound image B-mode depicts a markedly thickened terminal ileum (arrowheads) with deep ulceration on the mucosal surface seen as a hyperechoic intramural tract containing hyperechoic bubbles of gas (arrow). B Post-contrast axial T1-weighted MR image showing markedly thickened terminal ileum (arrowheads) with deep ulceration on the mucosal surface (arrow)
A 16-year-old male patient with three complex enteroenteric fistula in Crohn’s disease. A Ultrasound images depict diffuse ileal wall thickening with sonographic evidence of enterovesical fistula where a communication could be appreciated between bowel and urinary bladder (arrow), intravesical air/fecal matter leveling. There is also diffuse rectal wall thickening and retro-rectal abscess. B MR images show multiple fistulas in the terminal ileum on post-contrast T1 images. The terminal ileum shows wall thickening (12 mm) and marked enhancement with a layered pattern
The standard reference was findings at MRE and recent ileocolonoscopy, Table 2.
Ultrasound was found to be an effective tool for detecting stenosis in the examined patients, with a sensitivity of 84%, specificity of 91%, and accuracy of 94%. In addition, the ultrasound data showed a sensitivity of 87%, specificity of 97%, and accuracy of 97% in detecting dilatation.
The ultrasound examination sensitivity was significantly reduced to 6.4% and 16.7% in the presence of active inflammation and fistula. A high accuracy of 90.9% was demonstrated in the case of an abscess, Fig. 4.
Discussion
Our study sought to evaluate the impact of ultrasound to assess active disease, extension, and complications of Crohn's disease and compare magnetic resonance imaging as a standard reference. We characterized active bowel involvement in Crohn's disease as a gut wall thickness more than 3 mm, enhanced Doppler signals on ultrasound, or substantial bowel wall enhancement on MRI.
Previous studies considered disease presence and localization of Crohn's disease. Findings of these studies discovered similar tendencies by ultrasound supported by color Doppler to demonstrate noninferior results to post-contrast MRE in the identification, localization, and assessment of Crohn’s disease. In 2022 a meta-analysis by Lee et al. [7] included 752 patients from 10 studies reported pooled sensitivity and specificity for ultrasound of 86% and 88%, respectively.
In Panés et al. [8], systemic analysis reported a pooled sensitivity and specificity of 84–88% and 73–92% compared to endoscopy. Taylor et al. [9] also reported high sensitivity for ultrasound of 92% that was near-MR performance (97%), but specificity was marginally lower (84% for ultrasound and 96% for MR imaging).
In Mahdy et al. [10], comparative analysis of US and MRE found that both imaging modalities had equivalent sensitivity, specificity, and overall accuracy of 97.4%, 100%, and 97.4%, respectively, as referenced to the ileocolonoscopic findings. However, the latter study included limited sample size of only 25 patients.
Retrospectively, Potthast et al. [11] compared 46 individuals who underwent MR enteroclysis with ultrasonography. For intestinal wall alterations, they predicted 22% false negative results for ultrasound and 2.4% false negative results for magnetic resonance imaging enhancement.
In our investigation, we found 38% false negatives for ultrasonography and 6.5% false negatives for MRE.
Lasocki et al. [12] conducted the study in 2013. They published differing findings from a prospective trial of 30 Crohn's disease patients. They compared ultrasonography and MR imaging to determine the extent and transmural consequences of Crohn's disease. Ultrasound was not statistically significantly superior than MR imaging for detecting alterations in the afflicted intestinal wall, with a sensitivity of 91% against 83% for MR imaging. In our investigation, we discovered that MRI has a sensitivity of 87.5% and a specificity of 100%. Therefore, MRI was superior to ultrasonography in the evaluation of this type of involvement.
Tielbeek et al. [13] reported that ultrasound had a sensitivity of 74–100% and a specificity of 91–97% in the diagnosis of stenosis, whereas we discovered a sensitivity of 64.3% and a specificity of 79.4% for ultrasound in the identification of stenosis.
Potthast et al. [11] compared the accuracy of ultrasound with MR imaging in detecting fistulae, and ultrasound had a high sensitivity of 82% and specificity of 100%, compared to 70% and 92% for MR imaging, with no significant differences between the two tests.
In our investigation, ultrasound detected fistulae with an accuracy of 69.9%, sensitivity of 16.7%, and specificity of 100%.
Although diverse findings have been published about ultrasonography or MRI capabilities in diagnosing fistulae, the majority of previously published work [11,12,13] has accuracies of approximately 80%, as elicited by our results.
In this work, we identified a substantial association between color Doppler flow on sonography and bowel wall enhancement on MR imaging, owing to the fact that both metrics assess gut wall vascularization and the specificity for active inflammation reached 100%. Allocca et al. [14] and Moraes et al. [15] aligned with our results and displayed high specificity (92–100%) for bowel vascularity compared to contrast-enhanced MR imaging. However, sensitivity (6.4%) was far beyond previous work values, but this could be attributed to the current work included the disease in all the stages to simulate routine clinical assessment unlike others who presented selection of active stage.
A recent work compared mural vascularity at ultrasound with MR imaging and showed sensitivities of 46.5%, 0%, and 62.5% for grades 1, 2, and 3 Limberg scores, respectively, and specificity ranging from 81.8 to 100%. According to them the highest sensitivity and accuracy were elicited by grade 4 Limberg score at US reached 100% as compared to the corresponding vascular grading by MR enhancement and specificity of 83.3% [10].
Gourtsoyiannis et al. [16] compared dynamic MRI signal enhancement with ultrasound echo-pattern to evaluate bowel wall vascularity and found that both ultrasound and MR imaging are effective techniques for detecting affected bowel segments and transmural complications in Crohn's disease patients.
In our investigation, gut wall thickening, color Doppler flow on ultrasound, and MR bowel wall enhancement were the imaging characteristics that had the strongest connection with clinical or biological activity. There was no statistically significant relation found between signs of active inflammation and fistula detected by ultrasound and MR imaging (p values = 0.711 and 0.054, respectively).
There is a strong association between MR imaging and ultrasound activity (rho = 0.791, p < 0.0001). A strong correlation was established in the evaluation of the small intestine to evaluate wall thickness, lymph nodes, and vasa recta (rho = 0.926; p < 0.0001). An accurate correlation was obtained to measure layered wall appearance, disease extension, and fibro adipose proliferation (rho = 0.716; p < 0.001) [17].
Our results aligned with another recent work which found excellent correlation, between both US and MRE (r = 0.8, p < 0.01—r = 0.96, p < 0.01 for mural thickness and ileal length, respectively) [10]. In contrary Taylor et al. [9] demonstrated lower ultrasound sensitivity (70%) when compared to post-contrast MRE (80%). This can be attributed to our approach using quantified thickness and length by both modalities and then conducting direct correlation, while their study used qualitative visual assessment of diseased segments.
An excellent agreement between imaging and clinical laboratory data was obtained. Both MRI and US are acceptable procedures for diagnosing and monitoring CD activity.
Despite their differing accuracy rates, both imaging modalities can identify the afflicted loop and the primary indications of the disease. In active disease, US allows for the recognition of all typical indications (Figs. 1, 2, and 3). This approach demonstrates intestinal wall augmentation and enhanced vascularization of the afflicted bowel loop.
In contrast, in MR images, contrast uptake presented an initial vascular phase, migrates, and accumulated in the interstitium. As a result, gadolinium can detect chronic disease, Fig. 1.
In chronic disease, there were fibrous, scarred tissue lesions, MRI demonstrated significant venous phase enhancement with a mucosa-specific, multilayer, or homogenous pattern, whereas US showed no abnormal vascularity [18].
Due to its increased cost and acquisition time, MR imaging should only be utilized to detect the extent of disease burden, such as fistulae [12, 19].
The current study was limited by (1) a selection bias, as it only included a small number of people with early-stage disease. (2) Ultrasound examination of the small bowel is an operator-dependent tool that can only be performed by highly experienced operators, and its application protocol is not standardized.
Conclusions
Ultrasound is a noninvasive method that is comparable to MRI for detecting damaged bowel segments and transmural complications such as bowel strictures, fistulas, and abscesses in Crohn's disease patients. However, MR imaging is more comprehensive in providing detailed information about the disease's extent and activity.
Availability of data and materials
The corresponding author is responsible for sending the used data and materials upon request.
Abbreviations
- CD:
-
Crohn’s disease
- CDAI:
-
Crohn’s disease activity index
- B-FFE:
-
Balanced fast-field echo
- GD-DTPA:
-
Gadolinium-diethylenetriamine pentaacetic acid, paramagnetic contrast agent
- GFR:
-
Glomerular filtration rate
- MHz:
-
Megahertz
- MRE:
-
MR enterography
- rho:
-
Spearman rank correlation coefficient, “ρ”
- ROI:
-
Region of interest
- SD:
-
Standard deviation
- SGRE:
-
Spoiled gradient echo
- SPSS:
-
Statistical Package for the Social Sciences
- US:
-
Ultrasound
References
Yilmaz H (2022) Young age and shorter duration of Crohn’s disease are associated with non-adherence to taking medication. North Clin Istanb 9(1):8–13
Cicero G, Mazziotti S (2021) Crohn’s disease at radiological imaging: focus on techniques and intestinal tract. Intest Res 19(4):365–378
Moy MP, Sauk J, Gee MS (2016) The role of MR enterography in assessing Crohn’s disease activity and treatment response. Gastroenterol Res Pract 2016:8168695
Ahmad R, Ajlan AM, Eskander AA et al (2021) Magnetic resonance imaging in the management of Crohn’s disease: a systematic review and meta-analysis. Insights Imaging 12(1):118
D’Incà R, Caccaro R (2014) Measuring disease activity in Crohn’s disease: what is currently available to the clinician. Clin Exp Gastroenterol 7:151–161
Goertz RS, Hensel S, Wildner D et al (2021) Bowel wall thickening and hyperemia assessed by high-frequency ultrasound indicate histological inflammation in Crohn’s ileitis. Abdom Radiol 46:1855–1863
Lee DI, You MW, Park SH et al (2022) Comparison of diagnostic performance of ultrasonography and magnetic resonance enterography in the assessment of active bowel lesions in patients with Crohn’s disease: a systematic review and meta-analysis. Diagnostics 12(8):2008
Panés J, Bouzas R, Chaparro M et al (2011) Systematic review: the use of ultrasonography, computed tomography and magnetic resonance imaging for the diagnosis, assessment of activity and abdominal complications of Crohn’s disease. Aliment Pharmacol Ther 34(2):125–145
Taylor SA, Mallett S, Bhatnagar G et al (2018) Diagnostic accuracy of magnetic resonance enterography and small bowel ultrasound for the extent and activity of newly diagnosed and relapsed Crohn’s disease (METRIC): a multicentre trial. Lancet Gastroenterol Hepatol 3(8):548–558
Mahdy SN, El-Gaafary MS, Abdel Mageed HK et al (2024) Comparative study between ultrasound and MR enterography in evaluation of Crohn’s disease. Egypt J Radiol Nucl Med 55:106
Potthast S, Rieber A, von Tirpitz C et al (2002) Ultrasound and magnetic resonance imaging in Crohn’s disease: a comparison. Eur Radiol 12:1416–1422
Lasocki A, Pitman A, Williams R (2013) Relative efficacy of different MRI signs in diagnosing active Crohn’s disease, compared against a histological gold standard. J Med Imaging Radiat Oncol 55(1):11–19
Tielbeek JAW, Ziech MLW, Li Z (2014) Evaluation of conventional, dynamic contrast enhanced and diffusion weighted MRI for quantitative Crohn’s disease assessment with histopathology of surgical specimens. Eur Radiol 24(3):619–629
Allocca M, Fiorino G, Bonifacio C et al (2018) Comparative accuracy of bowel ultrasound versus magnetic resonance enterography in combination with colonoscopy in assessing Crohn’s disease and guiding clinical decision-making. J Crohn’s Colitis 12(11):1280–1287
Moraes ACDS, Moraes GDF, de Araújo ALE et al (2019) Abdominal ultrasonography with color Doppler analysis in the assessment of ileal Crohn’s disease: comparison with magnetic resonance enterography. Intest Res 17(2):227–236
Gourtsoyiannis N, Papanikolaou N, Grammatikakis J (2002) MR enteroclysis: technical considerations and clinical applications. Eur Radiol 12:2651–2658
Malago R, D’Onofrio M, Mantovani W et al (2012) Contrast-enhanced ultrasonography (CEUS) vs. MRI of the small bowel in the evaluation of Crohn’s disease activity. Radiol Med 117:268–281
Udayasankar UK, Martin D, Lauenstein T et al (2008) Role of spectral presaturation attenuated inversion-recovery fat-suppressed T2-weighted MR imaging in active inflammatory bowel disease. J Magn Reson Imaging 28(5):1133–1140
Pauls S, Gabelmann A, Schmidt SA (2006) Evaluating bowel wall vascularity in Crohn’s disease: a comparison of dynamic MRI and wideband harmonic imaging contrast-enhanced low MI ultrasound. Eur Radiol 16:2410–2417
Acknowledgements
Not applicable.
Funding
No source of funding.
Author information
Authors and Affiliations
Contributions
EH is the guarantor of integrity of the entire study. MH and EH contributed to the study concepts and design. MA and EH contributed to the literature research. MA, MH, and EH contributed to the clinical studies. MA, MH, and EH contributed to the experimental studies/data analysis. MA and EH contributed to the statistical analysis. MA, MH, and EH contributed to the manuscript preparation. MA, MH, and EH contributed to the manuscript editing. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethical Committee of the Radiology Department of Kasr El Ainy Hospital, Cairo University, which is an academic governmental supported highly specialized multidisciplinary Hospital. A waiver of informed consent was obtained.
Consent for publication
All patients included in this research were legible, above 16 years of age. The study was waived to get written informed consent from the included patients.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
El-Assaly, H., Mohamed, A.A.B. & Mustafa, H.A.A.F. Could ultrasound alone substitute MR imaging in evaluation of Crohn’s disease complications?. Egypt J Radiol Nucl Med 55, 170 (2024). https://doi.org/10.1186/s43055-024-01343-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-024-01343-7