Abstract
Background
Zinner syndrome is a rare Wolffian duct anomaly presenting as a triad of unilateral renal agenesis, ipsilateral seminal vesicle cyst and ipsilateral ejaculatory duct obstruction. The condition is due to a developmental anomaly leading to malformation of the mesonephric duct. Magnetic resonance imaging is considered to be the gold standard for the diagnosis of Zinner syndrome. Due to the limited number of cases reported in the literature, the associations of Zinner syndrome are not well established.
Case presentation
In this case report, we are presenting a case of a 38-year-old male with dysuria, intermittent pain in the scrotum and lower abdomen and painful ejaculation for the past six months. Imaging findings led to the diagnosis of Zinner syndrome, with unilateral testicular agenesis and an aberrant course of the left common iliac artery.
Conclusions
Apart from the known associations of Zinner syndrome, testicular agenesis in a patient with Zinner syndrome has not been reported in the literature and is an important addition to the limited literature available.
Similar content being viewed by others
Background
Zinner syndrome is a rare congenital malformation of the urogenital tract. The syndrome is due to maldevelopment of the distal part of the Mullerian duct during early embryogenesis. It is characterised by a triad of unilateral renal agenesis, ipsilateral seminal vesicle cyst and ipsilateral ejaculatory duct obstruction. It was first described in 1914 by A. Zinner [1]. A total of 6 cases of seminal vesicle cysts with ipsilateral renal agenesis or dysplasia were diagnosed during renal ultrasound screening of 280,000 children in a study in China [2]. Magnetic resonance imaging (MRI) is the gold standard of diagnosis. Due to the limited number of cases reported in the literature, the associations of the syndrome are not fully established. Our case is the first in the literature on Zinner syndrome with ipsilateral testicular agenesis and an aberrant course of the left common iliac artery.
Case presentation
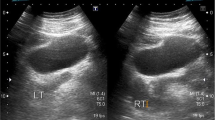
A 38-year-old male presented with dysuria, intermittent pain in the scrotum and lower abdomen and painful ejaculation for the past six months. There was no relevant significant past medical history or intervention. Palpation revealed an absent testis in the left scrotal sac. The rest of the general examination and vital signs were all within normal limits. Palpation of the abdomen revealed slight pain in the pelvic region. Trans-abdominal ultrasonography (USG) revealed non-visualisation of the left kidney in the left renal fossa or elsewhere in the abdominal cavity, which implicated the diagnosis of left renal agenesis. The right kidney was mildly enlarged, suggesting compensatory hypertrophy. The left testis was absent in the patient. In the left peri-prostatic region, a well-defined rounded anechoic lesion was noted measuring about 69 × 70 × 84 mm in its maximum anteroposterior, transverse and craniocaudal dimensions, respectively (Fig. 1). On the left side, the left testis was not sonographically visualised in the scrotal sac. The patient underwent a contrast-enhanced computed tomography (CECT) study of the abdomen, which confirmed the absence of the left kidney, and the left ureter (Fig. 2). The left renal artery and vein were also absent. A low-density cystic lesion was noted in the left peri-prostatic region that did not show any contrast uptake (Fig. 3). The left common iliac artery had an aberrant course, winding around the seminal vesicle cyst (Fig. 4). The rest of the findings were consistent with the USG. The rest of the solid abdominal organs and bowel loops appeared unremarkable. For a more thorough examination, an MRI of the pelvis and the inguinoscrotal area was conducted. MRI revealed a cystic lesion in the left seminal vesicle, demonstrating T2-hyperintense signal and T1-hypointense signal with dilatation of the left ejaculatory duct (Fig. 5). Thus, inclusive findings of USG, CECT abdomen and MRI of left renal agenesis with ipsilateral seminal vesicle cyst and dilated left ejaculatory duct led to the diagnosis of Zinner syndrome. The patient was advised to undergo laparoscopic excision of the cyst. However, the patient opted for conservative management with transrectal aspiration of the cyst and is currently undergoing follow-up with relief of symptoms.
Coronal contrast-enhanced CT study of the abdominopelvic region in the arterial phase reveals the absence of the left kidney in the left renal fossa and a low-density cystic lesion in the pelvic region slightly off-centred to the left side. The cystic lesion does not show any contrast uptake (long arrow). An aberrant left common iliac artery is also noted (short arrow) as it wraps the medial aspect of the cystic lesion. (Additional file 1: Movie 1)
Discussion
Zinner syndrome is a rare birth defect affecting the urogenital system and is characterised by a combination of three conditions: the absence of one kidney, cyst in the ipsilateral seminal vesicle and blockage in the corresponding ejaculatory duct. The affected ureter may be incomplete, absent or follow an abnormal course. The medical literature has reported fewer than 200 cases of this syndrome up to 2018 [3]. The condition can be present without symptoms or may manifest between the second and fourth decade of life [4]. When symptomatic, painful ejaculation, scrotal pain, perineal pain, abdominal pain, urinary urgency, urinary frequency, haemospermia, epididymitis, testis swelling, dysuria or infertility are the usual clinical findings. In our case, the cause of pain is likely caused by the pressure effects of the cyst on adjacent structures and the obstruction of the left ejaculatory duct.
The mesonephric ducts are embryonic tubes that originate from the primitive kidney and connect to the cloaca. From these ducts, the ureteric buds grow out. The primitive kidney is formed when the ureteric bud migrates and fuses with the metanephric blastema under the influence of growth hormones. In males, the mesonephric ducts develop into various structures, including the trigone of the urinary bladder, urethra, seminal vesicle, vas deferens, epididymis and other parts of the male reproductive system [5]. During foetal development, the ureteric bud should separate from the mesonephric duct, but in Zinner syndrome, this separation does not occur, leading to blockages in the seminal vesicle and ejaculatory duct, resulting in cyst formation. The lack of separation also causes renal agenesis. This condition is believed to be the male equivalent of Mayer–Rokitansky–Kuster–Hauser syndrome.
Zinner syndrome is suspected when a male patient presents with recurrent urinary tract infections and unilateral renal agenesis. Imaging is crucial for making a diagnosis, and ultrasound is commonly used. Ultrasound reveals an anechoic lesion in the region of the seminal vesicle and the absence of the kidney, but it cannot accurately distinguish seminal vesicle cysts from other cystic lesions. Computed tomography (CT) urogram confirms the absence of the kidney and ureters and reveals a cystic lesion in the retrovesical peri-prostatic region. MRI is the gold standard for diagnosis, as it can confirm the seminal vesicle cyst and obstruction of the ejaculatory ducts. Fine-needle aspiration of the cyst may reveal spermatozoa, which can differentiate it from other cysts. The differential diagnosis includes prostatic cysts, prostatic utricle cysts, diverticulosis of the vas deferens, ectopic ureterocele, cystic neoplasms and pelvic abscesses. The position, intralesional material, related urogenital system abnormalities and imaging features are used to differentiate between the entities. Mullerian duct cysts and ejaculatory duct cysts are located in the midline, and seminal vesicle cysts are typically hyperintense on T2-weighted imaging and hypointense on T1-weighted imaging. Diverticulosis of the vas deferens ampulla and ectopic ureterocele is found laterally [6].
Because the number of reported cases is limited, there is a lack of research on the associations of Zinner syndrome. Cases were reported in which there was obstruction of the ejaculatory duct, a contralateral hypoplastic testicle, a small-sized testis, an ipsilateral ureterocele and other conditions like ectopic ureter and megaureter [7,8,9]. Some studies reported unique combinations of abnormalities, including cystic dysplasia of the rete testis, partial hemitrigonal development and epididymal dilatation [10]. Two cases of Zinner syndrome reported by Cascini et al. had prenatally been diagnosed with multicystic dysplastic kidneys [11]. Fiaschetti et al. reported a patient with situs inversus, renal agenesis, ipsilateral seminal vesicle cyst, ectopic ureter and contralateral ejaculatory duct obstruction [12]. A systematic review found several comorbidities associated with Zinner syndrome, such as adenocarcinoma of the seminal vesicle, paraganglioma, squamous cell carcinoma of the seminal vesicle, renal cell carcinoma and non-Hodgkin lymphoma [13]. Treatment options depend on the size and clinical features of the cyst and may be conservative or surgical. Conservative management includes antibiotics and transurethral aspiration of the cyst or instillation of alcohol and minocycline, while excision of the cyst is preferred due to the high likelihood of recurrence following cyst puncture [14].
Conclusions
Zinner syndrome, although a rare disorder, is seen in adult males who report nonspecific symptoms such as dysuria, infertility, perineal pain and painful ejaculation. This triad of unilateral renal agenesis, ipsilateral seminal vesicle cyst and ejaculatory duct obstruction is best diagnosed with radiological imaging. Though ultrasonography and CT scans can be useful in suggesting this diagnosis, MRI is the preferred modality that confirms the diagnosis. The known associations of Zinner syndrome include conditions like hypoplastic testicles, ectopic ureter, megaureter and ureterocoele. Testicular agenesis in a patient with Zinner syndrome has not been reported in the literature and is an important addition to the limited literature available on Zinner syndrome.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
- CECT:
-
Contrast-enhanced computed tomography
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- USG:
-
Ultrasonography
References
Zinner A (1914) Ein fall von intravesikaler Samenblasenzyste. Wien Med Wochenschr 64:605
Sheih CP, Hung CS, Wei CF, Lin CY (1990) Cystic dilatations within the pelvis in patients with ipsilateral renal agenesis or dysplasia. J Urol 144(2):324–327
Florim S, Oliveira V, Rocha D (2018) Zinner syndrome presenting with intermittent scrotal pain in a young man. Radiol Case Rep 13(6):1224–1227
van den Ouden D, Blom JH, Bangma C, de Spiegeleer AH (1998) Diagnosis and management of seminal vesicle cysts associated with ipsilateral renal agenesis: a pooled analysis of 52 cases. Eur Urol 33(5):433–440. https://doi.org/10.1159/000019632. (PMID: 9643661)
Denes FT, Montellato NID, Lopes RN, Filho CMB, Cabral AD (1986) Seminal vesicle cyst and ipsilateral renal agenesis. Urology 28(4):313–315
Ghonge NP, Aggarwal B, Sahu AK (2010) Zinner syndrome: a unique triad of mesonephric duct abnormalities as an unusual cause of urinary symptoms in late adolescence. Indian J Urol 26(3):444–447
Abakar D, Badi FE, Sabiri M, El Manjra S, Lezar S, Essodegui F (2021) Zinner syndrome. Eur J Case Rep Intern Med 8(6):002628
Tan Z, Li B, Zhang L, Han P, Huang H, Taylor A et al (2020) Classifying seminal vesicle cysts in the diagnosis and treatment of Zinner syndrome: a report of six cases and review of available literature. Andrologia. https://doi.org/10.1111/and.13397
Di Paola V, Gigli R, Totaro A, Manfredi R (2021) Zinner syndrome: two cases and review of the literature. BMJ Case Rep 14(6):e243002
Casey RG, Stunell H, Buckley O, Flynn R, Torreggiani WC (2008) A unique radiological pentad of mesonephric duct abnormalities in a young man presenting with testicular swelling. BJR 81(963):e93–e96
Cascini V, Di Renzo D, Guerriero V, Lauriti G, Lelli Chiesa P (2019) Zinner syndrome in pediatric age: issues in the diagnosis and treatment of a rare malformation complex. Front Pediatrics. https://doi.org/10.3389/fped.2019.00129
Fiaschetti V, Greco L, Giuricin V, De Vivo D, Di Caprera E, Di Trapano R et al (2016) Zinner syndrome diagnosed by magnetic resonance imaging and computed tomography: role of imaging to identify and evaluate the uncommon variation in development of the male genital tract. Radiol Case Rep 12(1):54–58
Liu T, Li X, Huang L, Li H, Cai K, Jiang J et al (2021) Zinner syndrome: an updated pooled analysis based on 214 cases from 1999 to 2020: systematic review. Ann Palliat Med 10(2):2271–2282
Williams RD (1998) Surgery of the seminal vesicles. Campbell’s Urol 3:3299–3315
Acknowledgements
Authors thank the patient and his family for participating in this study.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
DV is the corresponding author and contributed to data collection, diagnosis and MRI findings. IKU and MKT were involved in manuscript writing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from the patient’s family for publication of this case report and accompanying images, and the study is approved by the ethics committee at Fakhruddin Ali Ahmed Medical College and Hospital.
Consent for publication
Case publication was approved; consent form was signed by the patient’s family.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Movie 1: Scrolling sections of axial contrast-enhanced CT study of the abdominopelvic region in the arterial phase follows the aberrant course of the left common iliac artery, which is displaced medially and winds around the left seminal vesicle cyst.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Varma, D., Ullah, I.K. & Thakur, M.K. A rare case of Zinner syndrome with unilateral testicular agenesis and aberrant course of left common iliac artery. Egypt J Radiol Nucl Med 54, 99 (2023). https://doi.org/10.1186/s43055-023-01045-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-01045-6