Abstract
Background
Pituitary stalk interruption syndrome (PSIS) is one of the rare endocrinal aetiologies of the abnormal short stature. This is a syndrome characterized by a specific tirade, an absent or hypoplastic anterior pituitary gland, thin or absent infundibulum, and ectopic posterior pituitary location. This type of pituitary dwarfism is usually presented in the first decade of life and may be first isolated with normal other pituitary hormones.
Results
Only 3 out of 117 dwarf patients (2.5%) were found to have pituitary stalk interruption syndrome.
Conclusion
Although of rare incidence, pituitary stalk interruption syndrome (PSIS) is an entity which leads to pituitary dwarfism and should be kept in mind while investigating a child with pituitary dwarfism and radiologists should be aware of its rarely encountered diagnostic MRI findings for early diagnosis and treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Child short stature is defined as a height that is 2 or more standard deviations below the mean for age and gender. Many pathogeneses of short stature were well known, including skeletal dysplasia and hormonal disorders. Such endocrinal pathogenesis due to pituitary growth hormone deficiency may also be familial, syndromic or isolated idiopathic as a result of developmental anomaly, malnutrition and chronic debilitating disease. The pituitary gland (hypophysis) is the magistrate endocrine gland, as it the source of the organizing hormones of the whole endocrine glands in the body. Normally, the gland is located at the sella turcica, below the hypothalamus, which is the overnor of the pituitary gland [1, 2].
The pituitary gland is composed of 2 lobes: the anterior lobe (the adenohypophysis) and the posterior lobe (the neurohypophysis). The adenohypophysis has hypothalamic regulation through a portal system (circulatory), while the neurohypophysis activity has direct neural hypothalamic control. Each lobe has a specific group of different hormones, so pituitary gland deficiency can lead to a wide range of clinical conditions, e.g. hypothyroidism, central diabetes insipidus, or growth retardation. Proportional growth retardation usually has a hormonal cause, such as growth hormone deficiency, called pituitary dwarfism. Unlike skeletal dysplasia which is a disproportionate dwarfism, the hormonal dwarfism may be associated with some mental disability [3, 4].
One of the rare aetiologies of the hormonal dwarfism is the pituitary stalk interruption syndrome (PSIS), which is also known as pituitary stalk transection syndrome. This is a syndrome characterized by a specific triad, an absent or hypoplastic anterior pituitary gland, thin or absent infundibulum, and ectopic posterior pituitary location. This type of pituitary dwarfism is usually presented in the first decade of life and may be first isolated with normal other pituitary hormones. However, deficiencies of other hormones present afterwards, with end stage anterior pan-hypopituitarism, with preservation of posterior pituitary function, regardless it is usually ectopic in location [5, 6].
The aim of this study was to detect the incidence of pituitary stalk interruption syndrome in cases of pituitary dwarfism in our institute and to highlight the magnetic resonance imaging (MRI) findings in such syndrome.
Methods
Approval of this retrospective study was obtained from the research ethics committee in our institute. All the study procedures were performed in agreement with the Declaration of Helsinki regarding research involving human participants. An informed consent was obtained from the parents of every patient.
The study population
This study included 117 patients, whom referred to do pituitary MRI, investigating their hormonal dwarfism, who were treated at our hospital from November 2019 to March 2022. It was a retrospective study, through revision of the patients records. The clinical data including height and weight of the children and their growth charts were reviewed as well as the laboratory data including growth hormone and other pituitary hormones levels. PACS MRI pituitary images were then reviewed. Inclusion criteria included all short stature children, below 15 years, with height that is 2 or more standard deviations below the mean for age and gender with laboratory evidence of growth hormone deficiency. Exclusion criteria included all patients with other proven metabolic causes or dysplasias as an aetiology for dwarfism.
MRI protocol
All MRI examinations were performed through Intera 1.5 T, Closed Magnet MRI, Philips Medical Systems, 5656 AE Eindhoven, Netherlands. The examinations were done with a dedicated head coil. Thin slices (three millimetre thickness) for the sella turica were taken including T1 weighted (T1W) and T2 weighted images (T2W) images in the coronal and sagittal planes. T1W sequences were repeated after administration of intravenous gadolinium with a dose of 0.1 mmol/kg. General anaesthesia were used in children younger than seven years old.
Imaging evaluation
Two experienced pediatric neuroradiologists (10&8 years experience), reviewed the images in the same session and agreed together on the findings followed by writing a detailed report. Images were carefully revised for evaluation the size and the components of the pituitary gland. The size was considered abnormal, if the height is less than 3.5 mm, and the volume is less than 150 mm3. The pituitary stalk was considered hypoplastic, if its AP diameter at optic chiasm level is less than 2.5 mm [7, 8]. The site and signal of the posterior pituitary lobe was assessed as well as the hypothalamus.
Statistical analysis of the data
Data were then fed to the computer and analysed using IBM SPSS software package version 20.
Results
The study included 117 patients all of which presenting with height that is 2 or more standard deviations below the mean for age and gender and with laboratory evidence of growth hormone deficiency. Their ages ranged between 4 and 14 years and included 55 males (47%) and 62 females (53%). After reviewal of the images, three patients (2.5%) were found to have PSIS, all sharing the same features including hypoplastic anterior pituitary, defective or absent stalk and hypothalamic ectopic site of the posterior pituitary lobe. The three patients included a 7-year-old girl, and two boys aging 8 and 10 years, respectively.
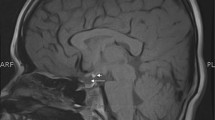
The heights of the gland were 1, 1.2 and 1.5 mm in heights, respectively, and the pituitary stalk was absent in the three patients. The site of the ectopic posterior pituitary marked by the T1W hyperintense bright spot was in the region of the tuber cinereum in the three patients. Figures 1, 2, 3 are showing the different MRI findings encountered in the three patients.
A 7-year-old girl with signs of pituitary dwarfism. MRI of the sella was performed. Coronal non contrast (A) & coronal post contrast T1w (B, C), Sagittal T1 contrast (D, E) and Sagittal T2w images (F) showing: hypoplastic anterior pituitary gland (Arrows), hypothalamic ectopic posterior pituitary (Curved Arrows) and absent stalk (Notched arrow)
Discussion
PSIS is an uncommon congenital cause of with its reported incidence is around 0.5 per one million births [9, 10]. In this study, three patients out of 117 patients presenting with pituitary dwarfism were diagnosed with this syndrome with percent around 2.5% confirming rarity of this syndrome.
Various hypotheses have been proposed to this syndrome such as defective migration of the pituitary gland during intrauterine life or ischemia with subsequent reorganization of the infundibular axons and development of ectopic posterior pituitary [11, 12].
The key imaging diagnostic findings of this syndrome are the absence of the pituitary stalk combined with ectopic site of the bright T1W posterior pituitary in the infundibular recess of the hypothalamus together with hypoplasia of the pituitary gland [10]. This was encountered in the three patients with confirmed diagnosis in this study.
Reported associated anomalies were noted to involve the midline structures (e.g. cleft lip, optic nerves hypoplasia and cerebral midline congenital anomaly). This may suggest that the gene responsible for these midline defects is the same responsible for PSIS. However, owing to the limited number of the diagnosed cases of PSIS, there is still no complete standard edited sources for the full clinical presentation of this disease, which is usually complex and diverse. Some shared signs were reported, as neonatal hyperbilirubinemia, hypoglycemia and small external genitalia, however the dwarfism and growth is the most common presentation adolescent presentation [13]. In this study, signs of dwarfism were noted in the three diagnosed patients without other definite associated anomalies.
Conclusion
Although of rare incidence, pituitary stalk interruption syndrome (PSIS) is an entity which leads to pituitary dwarfism and should be kept in mind while investigating a child with pituitary dwarfism and radiologists should be aware of its rarely encountered diagnostic MRI findings for early diagnosis and treatment.
Availability of data and materials
Available on request with the corresponding author. The authors declare that they had full access to all data in this study and the authors take complete responsibility for the integrity of the data and the accuracy of the data analysis.
Abbreviations
- MRI:
-
Magnetic resonant imaging.
- PSIS:
-
Pituitary stalk interruption syndrome
References
Vikas C, Bano S (2012) Imaging in short stature. Review Article. Indian J Endocrinol Metab. 16(5):692–7
Rerucha C, Darnall C (2015) Evaluation of short and tall stature in children. Am Fam Physician 92(1):43–50
Dietrich RB, Lis LE, Greensite FS, Pitt D (1995) Normal MR appearance of the pituitary gland in the first 2 years of life. AJNR Am J Neuroradiol 16(7):1413–1419
AmarA WM (2003) Pituitary anatomy and physiology. NeurosurgClin N Am 13:11–23
Nawaz A, Azeemuddin M, Shahid J (2018) Pituitary stalk interruption syndrome presenting in a euthyroid adult with short stature. Radiol Case Rep 13(2):503–506
Wang W, Wang S, Jiang Y, Yan F, Su T, Zhou W (2015) Relationship between pituitary stalk (PS) visibility and the severity of hormone deficiencies: PS interruption syndrome revisited. ClinEndocrinol (Oxf) 83(3):369–376
Yadav P, Singhal S, Chauhan S, Harit S (2017) MRI evaluation of size and shape of normal pituitary gland: age and sex related changes. J Clin Diagnost Res 11(12):1–4
Satogami N, Miki Y, Koyama T, Kataoka M, Togashi K (2010) Normal pituitary stalk: high-resolution MR imaging at 3T. AJNR Am J Neuroradiol 31(2):355–359
Gutch M, Kumar S, Razi S, Saran S, Gupta K (2014) Pituitary stalk interruption syndrome: Case report of three cases with review of literature. J Pediatr Neurosci 9(2):188–191
Vergier J, Castinetti F, Saveanu A, Girard N, Brue T, Reynaud R (2019) DIAGNOSIS OF ENDOCRINE DISEASE: pituitary stalk interruption syndrome: etiology and clinical manifestations. Eur J Endocrinol 181(5):R199–R20
Brauner R, Topalovic J, McElreavey K (2020) Pituitary stalk interruption syndrome is characterized by genetic heterogeneity. PLoS ONE 15(12):1–19
Zwaveling-Soonawala N, Alders M, Jongejan A, Kovacic L, Duijkers FA, Maas SM, Fliers E, van Trotsenburg ASP, Hennekam RC (2018) Clues for polygenic inheritance of pituitary stalk interruption syndrome from exome sequencing in 20 patients. J Clin Endocrinol Metab 103(2):415–428
Tatsi C, Sertedaki A, Voutetakis A, Valavani E, Magiakou MA, Kanaka-Gantenbein C, Chrousos GP, Dacou-Voutetakis C (2013) Pituitary stalk interruption syndrome and isolated pituitary hypoplasia may be caused by mutations in holoprosencephaly-related genes. J Clin Endocrinol Metab 98:E779-84
Acknowledgements
None.
Funding
All authors declare that no funding or any source of financial interest.
Author information
Authors and Affiliations
Contributions
MA: Corresponding author, collected data and the major editor. MS: Clinical pathology consultant, who helped in growth hormone level tests. AA: Shared in writing of the research and interpretation and gathering of the clinical and radiological data. MSA: Major sharer in data collection and analysis.All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written consents were assigned by the head of the family of the included patients, and the study was approved by the ethics committee of our institute (Almana General Hopital- KSA-Eastern Province).
Consent for publication
All researchers are accepting to publish this original article. This study is not previously published.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Agha, M., Sallam, M.S.M., Abougabal, A.M. et al. Pituitary stalk interruption syndrome (PSIS): do not miss this diagnosis. Egypt J Radiol Nucl Med 53, 192 (2022). https://doi.org/10.1186/s43055-022-00879-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-022-00879-w