Abstract
Background
The aim of the study was to evaluate the diagnostic efficacy of utilization of oblique sagittal and oblique coronal MRI techniques separately and concurrently in improving the diagnosis of anterior cruciate ligament (ACL) complete and partial tears. Between December 2017 and November 2018, 71 patients, with suspected ACL injury, were examined by MRI using four diagnostic approaches: standard routine images only (approach A), standard and oblique coronal images (approach B), standard and oblique sagittal images (approach C), and standard images with both oblique coronal and sagittal images (approach D). Two experienced musculoskeletal radiologists evaluated the MRI images separately and in a random order using the four methods, and findings were compared with arthroscopy results as a gold standard.
Results
The diagnostic accuracy, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for approach A in diagnosis of partial ACL tear was significantly lower than that for approaches B, C, and D (p value < 0.05). The PPV and NPV for approaches B (82% and 85%) and C (83% and 87%) in diagnosis of partial ACL tear which were significantly lower than that for approach D (94% and 95%). The four approaches revealed no significant difference in diagnosis of complete ACL tear (p value > 0.05). Approach D demonstrated highest interobserver agreement (94% in complete and 88% in partial ACL tears) in comparison to B (79% in complete and 66% in partial) and C (85% in complete and 71% in partial) when combining oblique sagittal and oblique coronal images in identifying both complete and partial ACL tears
Conclusion
The addition of oblique sagittal and coronal images improved diagnostic accuracy of detection of complete and partial ACL tears. The concurrent use of sagittal and coronal oblique images enhanced the diagnostic efficacy of diagnosis of partial ACL tears only.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
The anterior cruciate ligament (ACL) tears constitute approximately half of all knee ligamentous injuries encountered in high impact or sporting activities [1]. Prompt diagnosis and management of ACL injuries prevent aggravation of cartilage degeneration and accelerated traumatic arthritis [2]. Magnetic resonance imaging (MRI) of knee joints aids in the detection of the site and degree ACL injury [3]. However, arthroscopy remains the gold standard for assessment of internal derangement of the knee joint with the limitation of being an expensive and invasive procedure [4]. The ACL possesses a unique diagonal course extending from the inner surface of the lateral femoral condyle and attaching to a fossa in front and lateral to the anterior tibial spine [5]. Thus, the diagnostic potential of routine orthogonal MRI techniques for partial ACL injury is limited with fallible diagnosis [6]. To overcome this limitation, non-orthogonal MRI techniques such as coronal oblique and sagittal oblique techniques have been investigated for optimal visualization of ACL and better delineation of partial tears [7]. The aim of the study was to evaluate the diagnostic efficacy of utilization of oblique sagittal and oblique coronal MRI techniques separately and concurrently in improving the diagnosis of anterior cruciate ligament (ACL) complete and partial tears.
Methods
Study population
From December 2017 to November 2018, 71 patients (28 females and 43 males) performing MRI examination of the knee joint were prospectively evaluated for knee injuries. The age ranged between 18 years and 62 years (mean age 35.5). The patients were referred from the orthopedic department, and the study was approved by the ethics committee of our institute.
Inclusion criteria
The inclusion criteria are as follows: patients with painful knee joint, joint instability, or history of trauma; positive anterior drawer test, occurs when there is increased anterior tibial translation; positive Lachman test, occurs when there is increased forward translation of the knee without a decisive “end-point”; and positive pivot shift test, occurs when the lateral tibial plateau begins anteriorly subluxed and returns to neutral as you flex the knee to around 30°.
Exclusion criteria
The exclusion criteria are as follows: history of previous ACL or meniscal repair, active intra-articular infection, metabolic or neoplastic bone disease, or absolute contraindications including the presence of intra-cardiac devices such as pacemaker or cardiac defibrillator, or the presence of conductive metallic devices. Cases that performed arthroscopy with an interval exceeding 1 month from the time of performing the MR examination were also excluded from this study.
Magnetic resonance imager
A Philips Gyroscan Intera 1.5 T scanner (Philips Medical Systems, Netherlands) was used with a dedicated knee coil.
Patient position
All patients were examined in a supine position with a slight external knee rotation. The patient was offered headphones to reduce the repetitive gradient noise.
Imaging parameters (Fig. 1)
The imaging protocol includes the following:
- 1.
Standard T2 WI: 4-mm slice thickness, 1-mm interval, TR/TE = 4000/95.
- 2.
Oblique coronal T2 WI: obtained from superimposing 2-mm-slice thickness cuts with 0.5-mm interval on the orthogonal sagittal T2 images, in a plane parallel to femoral intercondylar roof along the course of the ACL: TR/TE = 4000/95.
- 3.
Oblique sagittal T2 WI: obtained from superimposing 2-mm-slice thickness cuts with 0.5-mm interval on the oblique coronal T2 images, in a plane parallel to the medial border of the lateral femoral condyle: TR/TE = 4000/95.
A technique to obtain oblique coronal and sagittal MR images of a normal ACL. a Orthogonal sagittal T2 image used to obtain b oblique coronal T2 image by superimposing 2-mm-slice thickness cuts with 0.5-mm interval on it in a plane parallel to the femoral intercondylar roof along the course of the ACL. c Topogram of oblique coronal T2 image used to obtain d oblique sagittal T2 image by superimposing 2-mm-slice thickness cuts with 0.5-mm interval on the former in a plane parallel to the medial border of the lateral femoral condyle
Arthroscopy
It was performed by two orthopedic surgeons with 5 and 7 years of experience, respectively, for all patients included in the study within a period not exceeding 1 month from the time of performing the MR examination.
Image interpretation
The MRI images were interpreted by two experienced musculoskeletal radiologists with 8 and 10 years of experience, respectively, using four diagnostic approaches: standard images only (approach A), standard and oblique coronal images (approach B), standard and oblique sagittal images (approach C), and standard images with both oblique coronal and sagittal images (method D). Each radiologist evaluated the MRI images separately and in a random order using the four methods to avoid any recall bias.
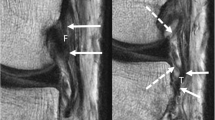
A three-point grading system was deployed to assess the severity of ACL injury. Grade 0, intact ACL; grade 1, partial ligamentous tear; and grade 2, complete ligamentous tear. The ACL was considered intact if it presented low-signal intensity, well-preserved continuation, and taut orientation. Partial ACL tear was considered if there is a focal or diffuse intrasubstance increased signal intensity, direct visualization of partial fibril disruption, or focal thinning/swelling of the ACL with maintained continuity. A complete tear was considered if there is the lack of continuity, full thickness abnormal signal intensity, or an edematous mass totally replacing the ligament (Figs. 2, 3, 4, and 5).
A female patient, 35 years old, complaining of knee pain following from falling down the stairs. a Sagittal T2 image revealed a focal intrasubstance area of intermediate signal intensity at the site ACL tibial attachment suggesting partial ACL tear (white arrow). b Oblique sagittal and c oblique coronal T2 MRI images revealed a well taut ACL showing normal signal intensity with intact tibial and femoral attachments consistent with normal ACL
A male patient, 22 years old, who suffered from twisting knee injury while playing football. a Sagittal T2 image revealed an intact ACL (white arrows). b Oblique coronal T2 and c, d oblique sagittal T2 MRI of right knee showing intraligamentous areas of intermediate signal intensity along the distal and mid-substance of the ACL (white arrows), but with some fibers still intact which are compatible with partial tear of the ACL
A female patient, 45 years old, complaining of knee trauma after a road traffic accident. a Sagittal T2 and b sagittal T2 fat suppression showing intrasubstance areas of increased signal intensity with ACL fibril discontinuity of ACL at the mid-substance in all pulse sequences (white arrows), compatible with high-grade partial tear of the ACL. Residual stumps on femoral and tibial sides (blue arrows) are thickened and increased in MR signal intensity. c Oblique coronal T2 and d oblique sagittal MRI images showing complete fiber discontinuity across the mid-substance of ACL with intrasubstance areas of high-signal intensity (white arrows) compatible with complete tear of the ACL. Residual stumps on femoral and tibial sides (blue arrows) are lax, thickened, and increased in signal intensity
A male patient, 43 years old, complaining of knee trauma after a rotational knee injury during playing basketball. a Orthogonal sagittal T2 image revealing a complete thickness tear near the femoral attachment of the ACL. b Oblique coronal T2 and c oblique sagittal MRI images showing abnormal bright signal intensity at the ACL mid-substance confirming the complete ACL thickness tear with better delineation of the mild retraction of the femoral and tibial attachments
Statistical analysis
Statistical Package for Social Sciences for Windows 15.0 (SPSS Inc., Chicago, IL, USA) was utilized to perform statistical analysis. The accuracy, sensitivity, and specificity for partial and complete ACL tears were compared to arthroscopic results, which were considered as a gold standard. A p value of less than 0.05 was considered statistically significant. Weighted kappa statistics were used to calculate interobserver agreement. The strength of agreement was interpreted according to the Landis and Koch guidelines as follows: 0, poor; 0.01–0.20, slight; 0.21–0.40, fair; 0.41–0.60, moderate; 0.61–0.80, substantial; and 0.81–1.00, almost perfect.
Results
Arthroscopic results revealed 46 patients with ACL tear, 25 complete and 21 partial tears. The accuracy, sensitivity, and specificity of detection of complete ACL tears for each diagnostic approach are demonstrated in Table 1. The sensitivity for the use of each diagnostic approach in detection of complete ACL tear revealed no significant statistical difference (p value > 0.05). However, the specificity and accuracy for approach A was significantly lower than that for B, C, and D approaches (p value < 0.05). The accuracy, sensitivity, and specificity for approaches B, C, and D in detection of complete ACL tears showed no statistical significant difference amongst them.
The accuracy, sensitivity, and specificity for diagnosis of partial ACL tears for each diagnostic approach are demonstrated in Table 2. The accuracy, sensitivity, and specificity for approach A in detection of partial ACL tear was significantly lower than that for approaches B, C, and D (p value < 0.05). The accuracy, sensitivity, and specificity and accuracy of approaches B and C for detection of partial ACL tears were significantly lower than that for approach D.
The interobserver agreement for the diagnosis of complete ACL tear is summarized in Table 3, while the interobserver agreement for the diagnosis of partial ACL tear is summarized in Table 4. The study revealed that the interobserver agreement improved using approaches B and C in comparison to approach A. However, approach D demonstrated highest interobserver agreement in comparison to B and C when combining oblique sagittal and oblique coronal images in identifying both complete and partial ACL tears.
Discussion
The normal ACL anatomy can be readily delineated by orthogonal sagittal and coronal MRI images [8]. However, due to its oblique course, 5–10% of the normally imaged anterior cruciate ligaments are difficult to visualize by orthogonal sagittal MRI [9]. Additionally, artifacts from the popliteal artery, partial volume, osteoarthritis, and post traumatic fibrous scarring increase the false-positive diagnosis of an ACL tear [10].
Nowadays, identifying ACL partial tear is of utmost importance in the management of ACL tears as it improves the outcome of ACL reconstruction. However, the diagnosis of partial ACL tears is diagnostically challenging owing to the striated appearance of a normal ACL which is aggravated with the use of fluid-sensitive sequences mimicking the appearance of partial ACL [11, 12].
To overcome these anatomical and technical limitations, various techniques were utilized to allow delineation of the entire course of the ACL in a single slice through parallel imaging along the ACL longitudinal axis [13].
Several methods to obtain oblique sagittal images were described in literature; Buckwalter and Pennes acquired an imaging plane angled 15° to the standard sagittal plane [9], and Do-Dai et al sliced parallel to the medial border of the lateral femoral condyle to develop oblique sagittal images for the ACL [14]. Nakanishi et al. sliced on axial image at an angle of 10° [15]. In this study, we acquired the oblique sagittal image plane parallel to the inter-condylar surface of the lateral femoral condyle.
Oblique coronal images were also utilized in previous studies to evaluate for ACL injuries. Staeubli et al. stated that the best sequence to visualize the ACL diagonal course is achieved by oblique coronal images as it clearly delineates the relation of the ACL attachment to the inter-condylar notch as well as its orientation towards the posterior cruciate ligament [16]. Hong et al. also concluded that oblique coronal MRI sequences increased the diagnostic efficacy in differentiating between partial and complete ACL tears [17]. In this study, we acquired the oblique coronal image plane parallel to femoral inter-condylar roof along the course of the ACL.
In the present study, we investigated the accuracy, sensitivity, and specificity of utilizing additional oblique sagittal and oblique coronal images with standard sagittal images both separately and in combination with the evaluation of complete and partial ACL tears.
This study showed that the addition of oblique sagittal and oblique coronal images to the standard sagittal images whether separately or in combination (approaches B, C, and D) improved the specificity and accuracy of the diagnosis of complete ACL tears in comparison to the standard sagittal images only (approach A). However, there was no statistical significance in diagnosis of complete ACL tear obtained from a combined use of oblique sagittal and coronal images (approach D) in comparison to the use of only one of the oblique images (approaches B and C. This was in agreement with the study performed by Kwon et al., which demonstrated that additional oblique imaging improved the specificity for diagnosing complete ACL tear. It also showed that either method of oblique imaging alone is sufficient with no statistical significance detected in combining both oblique methods [18].
As for diagnosis of partial ACL tears, this study revealed that the accuracy, sensitivity, and specificity for approach A in diagnosis of partial ACL tear was significantly lower than that for approaches B, C, and D (p value < 0.05). This was also in agreement with the findings described by Kwon et al. [18].
However, on the contrary to Kwon et al. [18] which stated that there was no statistical significance between the use of a single oblique method and their concurrent use in the diagnosis of ACL partial tears, this study revealed that the accuracy, sensitivity, and specificity of concurrent utilization of oblique sagittal and coronal images (approach D) for detection of partial ACL tear were significantly higher than that for approaches B and C (p value < 0.05). This is likely attributed to the advantage of the concurrent use of both obliques in detection of the entire course and femoral attachment of the ACL on two different planes enhancing the accuracy of diagnosis of changes in ACL thickness, signal intensity, continuity, and contour.
In 2018, Ghasem et al. [19] showed that the addition of oblique sagittal to standard images was better than the addition of oblique coronal images in the detection of complete and partial ACL tears with PPV and NPV of 78% and 88% in partial and 83% and 100% in complete ACL tears. Our results showed that there was no statistical significance in using either sagittal oblique or coronal oblique separately in diagnosis of partial and complete ACL tears; however, our study revealed that there is a statistical significant difference in diagnosing partial ACL tears when both oblique methods were performed together instead of performing it separately. The PPV and NPV for (approach D) in partial ACL tears were 94% and 95% in comparison to 82% and 85% in (approach B) and 83% and 87% in (approach C).
Our study showed that there is a higher interobserver agreement in diagnosis of complete and partial ACL tears using approaches B, C, and D in comparison to approach A, being highest with approaches C and D. This is in agreement with Kosaka et al., which showed higher diagnostic performance and interobserver agreement when using additional oblique coronal images [20]. The main reason for this is that oblique coronal images clearly delineate the course and femoral attachment of the ACL.
The present study had some limitations: First, the inconsistency as regards the duration between the onset of symptoms or time of injury and the MRI examination. However, the time interval between MRI examination and arthroscopy was limited to 1 month. Secondly, the difference in slice thickness between the standard sagittal images (4-mm slice thickness) and oblique sagittal and coronal images (2-mm slice thickness) was not taken into consideration in our study when comparing the different imaging techniques.
Conclusion
The addition of oblique sagittal and coronal images improved diagnostic accuracy of detection of complete and partial ACL tears. The concurrent use of sagittal and coronal oblique images enhanced the accuracy, sensitivity, and specificity of diagnosis of partial ACL tears only. Thus, we advise the use of concurrent sagittal and coronal oblique images in cases of partial ACL tear suspicion.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- MRI:
-
Magnetic resonance imaging
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
References
Park JS, Nam DC, Kim DH, Kim HK, Hwang SC (2012) Measurement of knee morphometrics using MRI: a comparative study between ACL-injured and non-injured knees. Knee Surg Related Res 24(3):180–185
AHN JH, JEONG, Hyo S, KANG HW (2016) Risk factors of false-negative magnetic resonance imaging diagnosis for meniscal tear associated with anterior cruciate ligament tear. Arthroscopy 32(6):1147–1154
Vassalou EE, Klontzas ME, Kouvidis GK, Matalliotaki PI, Karantanas AH (2016) Rotational knee laxity in anterior cruciate ligament deficiency: an additional secondary sign on MRI. AJR. Am J Roentgenol 206:151–154. https://doi.org/10.2214/AJR.15.14816
Roßbach BP, Pietschmann MF, Gülecyüz MF, Niethammer TR, Ficklscherer A, Wild S, Jansson V, Müller PE (2014 Dec 22) Indications requiring preoperative magnetic resonance imaging before knee arthroscopy. Arch Med Sci. 10(6):1147–1152
Li K, Du J, Huang L-X, Ni L, Liu T, Yang H-L (2017) The diagnostic accuracy of magnetic resonance imaging for anterior cruciate ligament injury in comparison to arthroscopy: a meta-analysis. Scientific Rep 7.1:7583
Khan HA, Ahad H, Sharma P, Bajaj P, Hassan N, Kamal Y (2015) Correlation between magnetic resonance imaging and arthroscopic findings in the knee joint. Trauma Mon 20(1):e18635
Volokhina YV, Syed HM, Pham PH, Blackburn AK (2015) Two helpful MRI signs for evaluation of posterolateral bundle tears of the anterior cruciate ligament: a pilot study. Orthop J Sports Med 3(8):2325967115597641
Mesgarzadeh M, Schneck CD, Bonakdarpour A (1988) Akbar. Magnetic resonance imaging of the knee and correlation with normal anatomy. Radiographics 8(4):707–733
Buckwalter KA, Pennes DR (1990) Anterior cruciate ligament: oblique sagittal MRI imaging. Radiology 175:276–277
Link TM, Steinbach LS, Ghosh S, Ries M, Lu Y, Lane N, Majumdar S (2003) Osteoarthritis: MRI imaging findings in different stages of disease and correlation with clinical findings. Radiology 226:373–381
Simpfendorfer C, Polster J (2014) MRI of the knee: what do we miss? Curr Radiol Rep 2(4):43
Borbon CA, Mouzopoulos G, Siebold R (2012) Why perform an ACL augmentation? Knee Surg Sports Traumatol Arthrosc 20:245–251
Fuss FK (1989) Anatomy of the cruciate ligaments and their function in extension and flexion of the human knee joint. Am J Anat 184:165–176
Do-Dai DD, Stracener JC, Youngberg RA (1994) Oblique sagittal MRI of anterior cruciate ligament. J. Comput. Assist. Tomogr. 18:160–162
Nakanishi K, Horibe S, Shiozaki Y, Ishida T, Narumi Y, Ikezoe J, Nakamura H (1997) MRI of normal anterior cruciate ligament (ACL) and recon-structed ACL: comparison of when the knee is extended with when the knee is flexed. Eur. Radiol 7:1020–1024
Staeubli HU, Adam O, Becker W, Burgkart R (1999) Anterior cruciate ligament and intercondylar notch in the coronal oblique plane: anatomy complemented by magnetic resonance imaging in cruciate ligament-intact knees. Arthroscopy 15:349–359
Hong SH, Choi JY, Lee GK, Choi JA, Chong HW, Kang HS (2003) Grading of anterior cruciate ligament injury. Diagnostic efficacy of oblique coronal magnetic resonance imaging of the knee. J Comput Assist Tomogr 27:814–819
Kwon JW, Yoon YC, Kim YN, Ahn JH, Choe BK (2009) Which oblique plane is more helpful in diagnosing an anterior cruciate ligament tear? Clinical Radiology. March 64:291–297
Hanafi MG, Gharibvand MM, Gharibvand RJ, Sadoni H (2018) Diagnostic value of oblique coronal and oblique sagittal magnetic resonance imaging (MRI) in diagnosis of anterior cruciate ligament (ACL) tears. J Med Life 11(4):281–285
Kosaka M, Nakase J, Toratani T, Ohashi Y, Kitaoka K, Yamada H, Komura K, Nakamura S, Tsuchiya H (2014) Oblique coronal and oblique sagittal MRI for diagnosis of anterior cruciate ligament tears and evaluation of anterior cruciate ligament remnant tissue. The Knee 21:54–57
Acknowledgements
Not applicable
Funding
The study has no funding from any resources.
Author information
Authors and Affiliations
Contributions
Hazem Hamed Soliman (HHS) designed the research, performed the research, analyzed data, and wrote the paper. The author read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the research ethic committee of the Radiology Department of the Faculty of Medicine at Cairo University on March 04, 2017, reference number of approval 653-2017. All patients included in this study gave written informed consent to participate in this research.
Consent for publication
All patients included in this research gave written informed consent to publish the data contained within this study.
Competing interests
The author declares that he has no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Soliman, H.H. Concurrent use of oblique sagittal and oblique coronal MRI: does it enhance the specificity and the accuracy of diagnosing complete and partial ACL tears?. Egypt J Radiol Nucl Med 51, 22 (2020). https://doi.org/10.1186/s43055-020-0145-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-020-0145-1