Abstract
Aims
Compared to primary breast sarcoma (BSs), radiotherapy-induced sarcoma (RIS) is a less frequent type of secondary breast sarcoma. Undifferentiated pleomorphic sarcoma (UPS) is an even rarer occurrence within the RIS category. This study aimed to present the clinicopathologic and molecular features of breast radiotherapy-induced UPS.
Methods
A retrospective study was conducted at the Third Affiliated Hospital of Soochow University to analyze three patients with radiation-induced undifferentiated pleomorphic sarcoma (UPS) following breast cancer, spanning from 2006 to 2023. The clinical and pathological variables were extracted from the medical records, while immunohistochemistry was employed to analyze the immunophenotypes of these tumors. Genomic characteristics were assessed through DNA and RNA sequencing techniques. Another 15 cases from the literature were also reviewed to better characterize the tumor.
Results
The affected areas encompass the chest wall and breasts, with an incubation period ranging from 6 to 17 years. The tumor cells exhibit pleomorphism and demonstrate a high degree of pathological mitosis. Notably, two cases displayed an accelerated disease progression, characterized by recurrent tumors and metastases occurring within short intervals of 48 and 7 months respectively subsequent to the initial diagnosis. The two prevailing identified genes were TP53 (2/3, 66.7%) and RB1 (1/3, 33.3%). Through analysis of somatic copy number variation (CNV), it was discovered that two oncogenes, MCL1 (1/3, 33.3%) and MYC (1/3, 33.3%), had experienced gains in CNV. The Tumor Mutational Burden (TMB) values for case 1, case 2, and case 3 were 5.9 mut/Mb, 1.0 mut/Mb, and 3.0 mut/Mb, respectively. Moreover, the analysis of RNA-NGS (next-generation sequencing) revealed the presence of a novel gene fusion, named COL3A1-GULP1, in case 2.
Conclusions
Based on our thorough analysis of research findings and previous reports, it is evident that radiotherapy-induced UPS exhibits a highly diverse and frequently severe clinical and biological behavior. Identifying tumor formation using genome sequencing can help understand its biological behavior and determine personalized treatments.
Similar content being viewed by others
Introduction
Breast sarcoma (BS) is an extremely uncommon form of breast tumor, much rarer than cancer, and makes up less than 1% of all breast malignancies and less than 5% of all sarcomas [1]. The majority of sarcomas are primary and typically occur in individuals aged between 55 and 59 years [2]. After breast-conserving surgery, adjuvant radiation therapy is an important part of breast cancer treatment, but it can also lead to certain issues. Sarcomas can arise in areas that have undergone radiation therapy, such as the breast, chest wall, axilla, sternum and supraclavicular region [3]. Although uncommon, this is a recognized complication of radiotherapy for breast cancer.
Radiotherapy-induced sarcomas (RISs) were first identified in 1948 and defined in 1971 to include a minimum incubation period of 3 years prior to the newly diagnosed sarcomas, occurs in the radiating region of the previous tumor, and the primary tumor is histologically different from the sarcoma [3]. The cumulative incidence of RIS is 0.3% at 15 years after radiotherapy which is rarer than primary BSs, of which, the most common were angiosarcoma, morphologically identical to primary BSs [3, 4]. Undifferentiated pleiomorphic sarcoma (UPS) accounts for 10.5%–24% of primary BSs, but there is no definite data on the incidence of secondary BSs [3, 5].
Primary UPS is a highly aggressive tumor with a high rate of local recurrence and distant metastasis, as is in the breast [2, 6,7,8,9]. Although radiotherapy-induced UPS is rare, cases of high aggressiveness and poor prognosis have been reported [4, 9]. Studies that did not focus on particular sites have indicated that sarcomas caused by radiotherapy may be more aggressive and have a poorer prognosis compared to primary sarcomas [3, 10, 11]. Currently, there is a lack of comparative reports on the biological behavior between primary and secondary UPS of the breast. In terms of radiotherapy-induced UPS in the breast being rare, only a limited number of case reports exist, and treatment options are primarily based on extrapolation from similar sarcomas found in other anatomical regions [2, 12]. The advent of next-generation sequencing (NGS) technology has significantly enhanced our comprehension of tumor pathogenesis and biological behavior. It is noteworthy that gene sequencing has unveiled substantial disparities in the genomic constitution between primary breast angiosarcoma and radiotherapy-induced angiosarcoma, which underlie their divergent biological behaviors.
Our study presents a comprehensive report on three patients who developed radiation-induced UPS in the breast and chest wall, diagnosed based on the specified criteria. The study provides detailed analysis of the clinicopathological characteristics of radiotherapy-induced UPS following breast cancer, aiming to enhance our understanding of its pathogenesis and biology, as well as identify potential therapeutic targets.
Materials and methods
Case selection
A retrospective search of the pathology database at the Third Affiliated Hospital of Soochow University for radiation-induced UPS of the breast was carried out from 2006 to 2023 year. All available slides and blocks of the three known breast cancer patients who developed sarcoma after surgery were retrieved from the Department of Pathology, the Third Affiliated Hospital of Soochow University. Finally, three cases with the diagnosis of radiotherapy-induced UPS were identified. Patient history, treatment, and outcomes were obtained from institutional medical records, managed healthcare providers, and telephone follow-ups. Before the study, all patient samples were anonymized and used in alliance with the ethical rules and regulations presented in the Declaration of Helsinki.
Immunohistochemistry (IHC) staining
IHC analysis was performed for AE1/AE3 (ZSGB- BIO, Beijing, China), EMA (ZSGB- BIO, Beijing, China), smooth-muscle actin (SMA) (MXB Biotechnology, Fujian, China), desmin (MXB Biotechnology, Fujian, China), h-caldesmon (MXB Biotechnology, Fujian, China), MyoD1(MXB Biotechnology, Fujian, China), Myogenin (MXB Biotechnology, Fujian, China), CD34 (ZSGB- BIO, Beijing, China), S-100 (ZSGB- BIO, Beijing, China), Sox10 (ZSGB- BIO, Beijing, China), estrogen receptor (ER) (Ventana, Tucson, Arizona, USA), progesterone receptor (PR) (Ventana, Tucson, Arizona, USA), HER2/neu (Ventana, Tucson, Arizona, USA), and Ki-67 (Ventana, Tucson, Arizona, USA). After dewaxing and hydration, 4 μm sections from formalin-fixed paraffin-embedded tissue were treated by an immunohistochemical automatic staining machine according to the protocol provided by the Benchmark XT system, and there were positive and negative tissues for comparisons in every case.
DNA-NGS
For DNA sequencing, formalin-fixed paraffin-embedded (FFPE) samples, five 10 μm tumor slices were used for DNA extraction using the QIAamp DNA FFPE Kit (QIAGEN, Valencia, CA, USA) following the manufacturer’s instructions. DNA quality was assessed by spectrophotometry with absorbance at 230, 260, and 280 nm, and quantified by Qubit 2.0. Target-enriched libraries (481-cancer-relevant genes, Geneseeq Technology Inc.) were sequenced on the HiSeq4000 platform (Illumina) with 2 × 150 bp pair-end reads. Sequencing data were demultiplexed by bcl2fastq v2.19, analyzed by Trimmomatic to remove low-quality (quality < 15) or N bases, and mapped to the reference hg19 genome (Human Genome version 19) using the Burrows-Wheeler Aligner. The data analysis was conducted in accordance with the previously described methodology [13].
RNA-NGS
Total RNA from FFPE samples was extracted using miRNeasy FFPE kit (QIAGEN, Valencia, CA, USA). Ribosomal RNA was depleted using KAPA Stranded RNA-seq Kit with RiboErase (HMR) (KAPA Biosystems). Base calling was performed on bcl2fastq v2.16.0.10 (Illumina, Inc.). STAR (version 2.5.3a) is used for transcriptome mapping followed by isoform and gene level quantification performed by RSEM (version 1.3.0). Differential expression analysis was conducted by R packages DESeq2 (version 1.16.1) and edgeR (version 3.18.1). Corresponding volcano plots and heatmaps were generated by in-house R scripts. GO and KEGG enrichment analysis was performed by ClusterProfiler (version 3.4.4). Fusion Catcher (version 0.99.4e) was used with parameters (aligners blat, bowtie2, star, otherwise default parameter) which uses Bowtie aligner to perform both transcriptome and genome mapping and then respectively uses BLAT aligner, bowtie2 aligner, and star aligner to further map unmapped reads and count fusion supporting evidence (RNA-seq Kit, Geneseeq Technology Inc.). Meanwhile, we analyze fusion using blast by in-house script. The combined fusion results from all tools were manually reviewed on IGV for confirmation.
Results
Clinical findings
Case 1
A chest wall lump that was rapidly expanding was brought to the attention of the breast surgery department by a 57-year-old female. Reviewing her medical history reveals that she was diagnosed with breast cancer 17 years prior, at which point she underwent a left mastectomy and ipsilateral axillary dissection. She underwent radiotherapy (Synchronous radiotherapy: 50 Gy in 25 fractions on the chest wall and 50 Gy in 25 fractions on the lymphatic nodes) and chemotherapy following the operation. The initial opinion was that the lesion was a return of breast cancer because it was hard and immobile, located in the chest wall just below the surgical incision. Computed tomography (CT) imaging revealed a 2.4*0.9 hypoechoic mass subcutaneously on the left chest wall, with an uneven border and burr change (Fig. 1A). The positron emission tomography (PET)/computed tomography (CT) scan revealed an increase in FDG metabolism in the left chest wall (inferior ensisternum), while taking into consideration breast cancer recurrence. Following an excisional biopsy, it was discovered that the patient had UPS. The postoperative pathology was the same even though the patient underwent tumor removal at a different facility. The patient did not receive any adjuvant therapy and recurred 48 months follow-up in the chest wall. At a different facility, the tumor was removed once more without adjuvant therapy, and a 20-month follow-up revealed no progression.
Case 2
A 50-year-old female who had been experiencing a two-month-old tumor in her left chest wall presented to the breast surgery department. A 5.0*3.0 cm hard mass was found in the left chest wall during the examination, and the left breast was missing. According to the patient’s medical history, she underwent a modified radical mastectomy for breast cancer on the left breast 14 years ago along with adjuvant radiotherapy (Synchronous radiotherapy: 50 Gy in 25 fractions on the chest wall and 50 Gy in 25 fractions on the lymphatic nodes), chemotherapy, and endocrine therapy. After the left breast cancer was removed, a CT scan revealed that the left breast was absent. Additionally, a nodular soft tissue shadow with a maximum layer of 4.1*3.7 cm and an unclear boundary was seen on the left chest wall (Fig. 1B). The PET/CT scan showed no additional lesions apart from elevated FDG uptake on the left chest wall. A core needle biopsy (CNB) was then performed on the patient and UPS was diagnosed. Tumor resection was performed at another facility, and the postoperative pathology was the same. Up to now 60 months, no recurrence or metastasis has been observed in this patient. A month after the surgery, the patient was diagnosed with cervical cancer and has since undergone chemotherapy and immunotherapy.
Case 3
A 32-year-old female patient incidentally detected a palpable mass in her right breast. Given her history of previous breast-conserving surgery for breast cancer on the same side six years ago, she presented to the Department of Breast Surgery for further evaluation. A mass measuring approximately 3.0*2.0 cm centimeters was palpable at the site of the original surgical incision on the right breast, with no associated nipple discharge or erosion of the nipple and areola, and absence of enlarged axillary lymph nodes. Ultrasound showed a solid mass in the right breast, and CT showed a mass in the lower quadrant of the right breast (Fig. 1C), considering the possibility of recurrence. Following CNB, the patient was diagnosed with a spindle cell tumor containing pleomorphic cells, indicating a tendency towards sarcoma based on immunohistochemistry results. A comprehensive review of the patient’s medical history revealed that she underwent breast-conserving surgery for breast cancer six years ago and subsequently received chemotherapy, radiotherapy (Synchronous radiotherapy:45 Gy to the breast in 25 fractions, 60 Gy to the boost in 25 fractions, and 48 Gy were applied to the lymphatic nodes), and anti-Her2-targeted therapy. The disease onset is situated within the radiation field of the breast adjacent to the initial breast-conserving incision. A simple mastectomy was performed, followed by a postoperative pathological report indicating UPS. The PET/CT examination simultaneously excluded the possibility of a metastatic tumor. After the surgical procedure, the patient proceeded to another medical facility for a consultation, wherein the pathological findings remained consistent. No adjuvant therapy was administered after surgery, and supraclavicular metastases emerged at 7 months of follow-up.
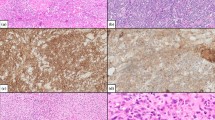
Histopathologic and IHC features
Histologically, the tumor group exhibited a heterogeneous high-grade sarcoma with pleomorphic nuclei and visible pathological mitosis. The case 1 exhibited a dense arrangement of adipose fusiform and oval neoplastic cells interspersed with pleomorphic neoplastic cells containing numerous mitotic figures (Fig. 2A and B). The tumor cells exhibit diffuse arrangement with abundant and eosinophilic cytoplasm, coarse nuclear chromatin, discernible nucleoli, and a profusion of small vessels (Fig. 2C and D). The tumor in case 2 exhibited a composition of round, oval, and spindle cells with vacuolar or pale cytoplasm and coarse nuclear chromatin (Fig. 3A and B). Additionally, the presence of giant pleomorphic tumor cells was observed along with easily identifiable mitotic figures (Fig. 3C and D). The histomorphology of case 3 exhibited heterogeneity, with spindle-shaped cells present in some areas and relatively sparse cells with rough chromatin (Fig. 4A and F). Nucleoli were visible in some cells, and a large number of collagen fibers were observed between the cells (Fig. 4A and F). In other parts, there were relatively dense cells that featured prototype oval giant tumor cells with rough chromatin (Fig. 4G and H). The corresponding metastases exhibit high density and a significant presence of tumor giant cells (Fig. 4I and L). Considering that all the patients had a history of breast cancer, various differential diagnoses were taken into account, including metaplastic carcinoma, malignant phyllodes tumor, malignant melanoma of the breast, and high-grade sarcoma of another type of soft tissue. Immunohistochemistry (IHC) was performed to differentiate these possibilities. All the immunohistochemical parameters, including AE1/AE3, EMA, CK7, CK8/18, smooth muscle actin (SMA), desmin, h-caldesmon, CD34, CD31, S-100 protein, Sox10, estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor 2 (HER2), and Ki-67 index were evaluated in all the three cases encompassing both the primary and metastatic lesions of case 3. A high Ki-67 index was observed in all three cases (Figs. 2E, 3E and 4M and N). Except for SMA which showed focal positivity in case 2 (Fig. 3F) and the primary lesion of case 3 (Fig. 4O); all other biomarkers were negative.
Morphologic and immunohistochemical findings in Case 1. Fat fusiform or oval neoplastic cells are interspersed with pleomorphic neoplastic cells containing numerous mitotic Fig. (200x A, B); The cells exhibit a diffuse pattern with abundant and eosinophilic cytoplasm, coarse nuclear chromatin, discernible nucleoli, and a profusion of small vessels (400x C, D); The Ki-67 index in the hotspot area was approximately 50% (200x E)
Morphologic and immunohistochemical findings in Case 2. Case 2’ s patient presented with a composition of round, oval, and spindle cells with vacuolar or pale cytoplasm and coarse nuclear chromatin (200x A, B); pleomorphic tumor cells with briskly mitosis (400x C, D); High Ki-67 index was about 60% in hotspot area (200x E) and SMA was focally positive (200x F)
Morphologic and immunohistochemical findings in Case 3. The tumor in Case 3 exhibited heterogeneity: The core needle biopsy (CNB) specimen exhibited a loosely arranged cellular structure characterized by polymorphic macro-cells and mitosis (200x A, C, 400x B, D); The resection showed relatively sparse tumor cells with rough chromatin, interspersed between collagen fibers in some area (200x E, 400x F); In other area, relatively dense cells that featured prototype oval giant tumor cells with rough chromatin (200x G, 400x H); The metastatic lesion exhibited a relatively dense arrangement of spindle-shaped and oval cells interspersed with megakaryocytes, and mitotic figures was observed (200x I, K, 400x J, L). The Ki-67 index in the primary lesion (200x M) was approximately 35%, whereas it exhibited a relatively higher value of around 50% in the metastatic lesion (200x N). The primary lesion in case 3 demonstrated focal positivity for SMA (200x O), whereas the metastatic lesion exhibited negativity for SMA
DNA-NGS identifies recurrent mutations in TP53
The genomic landscape of UPS was explored through the application of DNA-NGS on the three tumors. For DNA-NGS analysis, a total of 7 variations corresponding to 6 genes including TP53, FANCC, STAG2, EED, SPRY4, and RB1 which were all tumor suppressor gene (TSC) were identified in the three samples (Table 1). Two genes among the above with significant abnormalities: TP53 missense mutation (c.643 A > G (p.S215G)), TP53 frameshift mutation (c.459del (p. G154Afs*16)), and RB1 splice mutation (c.2660_2663 + 16del), predicated to be pathogenic by predicted tools (Table 1). The only recurrent gene (TP53) was identified as a potentially druggable gene by the drug–gene interaction database (DGIdb).
Somatic copy number alteration and TMB analysis using DNA-NGS data
The somatic copy number variation (CNV) analysis was conducted on all three samples, revealing CNV gains in two oncogenes, namely MCL1 and MYC in case 2 (Table 1). The respective TMB values were 5.9 mut/Mb, 1.0 mut/Mb, and 3.0 mut/Mb for case 1 to case 3.
RNA-NGS identifies a novel gene fusion COL3A1-GULP1
Using two bioinformatic fusion callers and following a series of filtering steps described in the materials and methods, a novel COL3A1-GULP1 fusion (COL3A1: exon23-GULP1: exon5) was detected in case 2 (Fig. 5).
Discussion
The occurrence of radiotherapy-induced sarcoma is infrequent presenting a complex and clinically challenging category of tumors. These tumors are highly aggressive and offer very few effective therapeutic options [2, 14]. The reported incidence rates in the literature ranged from 0.008 to 0.8% [2, 14]. And, the occurrence of RIS followed by breast cancer was approximately 0.11% among the cohort of 2700 breast cancer patients who received radiotherapy at our institution between 2006 and 2023.
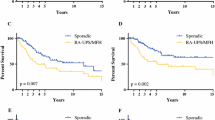
The most frequently reported RIS is angiosarcoma, which distinguishes itself from primary breast angiosarcoma or soft tissue angiosarcoma in terms of clinicopathologic and genomic characterization [1]. To date, no prognostic and genomic studies have conducted a comparative analysis between primary breast UPS and UPS induced by radiotherapy. The present study provides a comprehensive review of radiotherapy-induced UPS based on the available English literature, as summarized in Table 2. The analysis includes key factors such as age of onset, latency period, tumor size, and treatment regimen. Among the 10 cases with available follow-up information, two patients succumbed to the disease within one year, while two patients remained alive despite experiencing multiple relapses. The remaining patients were followed up for a period ranging from 44 months to 174 months without any evidence of recurrence or metastasis. Nevertheless, given its high-grade malignancy and limited therapeutic options, UPS carries an unfavorable prognosis regardless of whether it arises de novo or as a consequence of prior irradiation.
The etiology of radiotherapy-induced sarcoma is associated with double-stranded DNA damage caused by radiation, leading to genomic instability that may result in the development of sarcomas [3, 14, 27]. The risk of radiotherapy-induced sarcoma generally increases with higher radiation doses, exposure during childhood, concurrent chemotherapy, and the presence of genetic disorders such as ataxia-telangiectasia and BRCA-1 mutation [2]. Molecular investigations of sarcomas induced by radiotherapy commonly reveal inactivation of the p53 pathway [28]. The genomic variants of the three patients exhibited significant dissimilarities, with only shared TP53 variants identified in patient 1 and patient 2 but at distinct variant sites. The TP53 gene is frequently mutated in both primary and secondary soft tissue UPS, with a mutation rate ranging from 13 to 32% [27,28,29,30,31]. Radiation therapy immediately induces DNA damage in cells within the treatment field, which is repaired sequentially, minimizing double-strand breaks and deletions formation [3]. The mutation of the TP53 gene results in the impairment of its repair function, consequently leading to the development of radiotherapy-induced sarcoma. Besides the radiotherapy-induced UPSs documented in this study, TP53 is also a prevalent variant observed in other cases of radiotherapy-induced sarcomas [32]. In this study, both TP53 mutation sites (exon 6 missense mutations c.643 A > G (p. S215G) and exon 5 c.459del (p. G154Afs*16)) are predicted to be pathogenic, resulting in impaired DNA damage repair function. Another pathogenic gene is the retinoblastoma susceptibility gene RB1, which is the first molecular-defined tumor suppressor gene and a crucial regulator of the G1/S transition in the cell cycle [33]. RB1 mutations are present in nearly all familial and sporadic cases of retinoblastoma, and this gene exhibits variable mutation frequencies in various other human cancers [34]. Lesluyes et al. reported RB1 is a common variant gene in both sporadic and post-radiation sarcomas, which is loss of function in nearly 75% of all such tumors [28]. The RB1 gene’s exon 25 (c.2660_2663 + 16del) shear mutation may cause the loss of the RB1 protein’s ability to inhibit tumor growth, impair transcriptional control, promote unchecked cell proliferation, prevent apoptosis, postpone cell senescence, and contribute to the occurrence and growth of tumors. No other genes typically seen in radiotherapy-induced UPS were discovered in our analysis, in addition to the two genes mentioned above.
Additionally, our cases exhibit amplification of MCL1 and MYC. MCL1, a member of the BCL-2 family with anti-apoptotic properties, hinders mitochondrial outer membrane penetration (MOMP) and the release of mitochondrial cytochrome C [35]. The survival of various cell types, including nerve cells, lymphocytes, and myocardial cells, is reliant on the presence of MCL[36,37,38]. Additionally, MCL1 exhibits a high oncogenic potential and has been found to be amplified in 10.9% of tumor samples across multiple malignant carcinoma subtype [36,37,38]. Overexpression of the MCL1 protein or amplification of the MCL1 gene can result in drug resistance or poor prognosis in certain tumors [37,38,39]. In a study, it was reported that there is co-amplification of MCL1 and MYC, which is associated with poor survival in patients with non-small cell lung cancer [40]. The MYC oncogene encodes a transcription factor, MYC, which is believed to trigger selective gene expression amplification in order to promote cell growth and proliferation based on current evidence [40, 41]. MYC is a frequently amplified gene in radiotherapy-induced angiosarcomas, accounting for approximately more than 90%, whereas it is infrequent in primary breast angiosarcomas [1]. In pan-cancer copy number analysis, MYC was identified as the third most frequently amplified gene [41, 42]. The dysregulation of MYC expression in various transgenic mouse tissues leads to tumorigenesis, thereby demonstrating its transformative activity in vivo and providing support for the notion that MYC functions as a human oncogene [43, 44]. The present study identified concurrent amplification of MYC and MCL1 in case 2, suggesting a potential collaborative role of these two genes in promoting tumorigenesis. Significant advancements have been achieved in the development of MCL-1 inhibitors, several of which have progressed to clinical trials [45]. The direct targeting of MYC for therapeutic purposes has proven challenging due to the absence of a well-established ligand-binding domain [46]. Consequently, attention has shifted towards upstream regulators or MYC co-activators as potential targets. Targeting these molecular inhibitors has demonstrated reduced MYC transcription and protein levels in leukemia and lymphoma cell lines, exhibiting promising antitumor effects in mouse models of Burkitt lymphoma, acute myeloid leukemia, and multiple myeloma [46, 47]. All these genes hold potential as therapeutic targets for tumors with limited treatment options.
We performed a comprehensive genome-wide analysis of radiotherapy-induced sarcomas and correlated it with their transcriptomic consequences to gain deeper insights into the underlying biology of these tumors. While primary undifferentiated pleomorphic sarcomas (UPS) have been found to harbor multiple fusion genes, such as CLTC-VMP1, FARP1-STK24, and MED12-PRDM10, no fusion gene has been reported for radiation-induced UPS [31, 48, 49]. Our study unveiled a novel COL3A1-GULP1 fusion gene; however, its functional implications remain yet to be elucidated.
In summary, this study presents a comprehensive analysis of the genetic and transcriptomic alterations landscape in radiotherapy-induced UPS after breast cancer, providing valuable insights into its pathogenesis and expanding our understanding of this tumor. The genomic variability and morphological diversity observed suggest that UPS is highly heterogeneous with a poor prognosis. Genetic testing results reveal potential targeted therapeutic options for this type of tumor. As more cases are accumulated, researchers will gain a better understanding of the genome of these tumors and develop effective treatments for these aggressive malignancies.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- BS:
-
breast sarcoma
- RIS:
-
radiotherapy-induced sarcoma
- UPS:
-
undifferentiated pleomorphic sarcoma
- CNV:
-
copy number variation
- TMB:
-
Tumor Mutational Burden
- NGS:
-
Next-generation sequencing
- IHC:
-
immunohistochemistry
References
Rakha EAR-FJ, Sasano H, Wu Y. WHO classifcation of tumours editorial board: breast tumours. WHO classifcation of tumours series, 5th ed.; 2019.
Lim SZ, Ong KW, Tan BK, Selvarajan S, Tan PH. Sarcoma of the breast: an update on a rare entity. J Clin Pathol. 2016;69(5):373–81.
Sheth GR, Cranmer LD, Smith BD, Grasso-Lebeau L, Lang JE. Radiation-induced sarcoma of the breast: a systematic review. Oncologist. 2012;17(3):405–18.
Kong J, Shahait AD, Kim S, Choi L. Radiation-induced undifferentiated pleomorphic sarcoma of the breast. BMJ Case Rep. 2020;13(2):e232616
Srinivasamurthy BC, Kulandaivelu AR, Saha K, Saha A. Primary undifferentiated pleomorphic sarcoma of the breast in a young female: a case report. World J Surg Oncol. 2016;14(1):186.
Yamazaki H, Shimizu S, Yoshida T, Suganuma N, Yamanaka T, Yamashita T, Rino Y, Masuda M. A case of undifferentiated pleomorphic sarcoma of the breast with lung and bone metastases. Int J Surg Case Rep. 2018;51:143–6.
Gambichler T, Horny K, Mentzel T, Stricker I, Tannapfel A, Scheel CH, Behle B, Quast DR, Lee YP, Stucker M, et al. Undifferentiated pleomorphic sarcoma of the breast with neoplastic fever: case report and genomic characterization. J Cancer Res Clin Oncol. 2023;149(4):1465–71.
Hartel PH, Bratthauer G, Hartel JV, Fanburg-Smith JC. Primary malignant fibrous histiocytoma (myxofibrosarcoma/pleomorphic sarcoma not otherwise specified) of the breast: clinicopathologic study of 19 cases. Ann Diagn Pathol. 2011;15(6):407–13.
Vera-Sempere F, Llombart-Bosch A. Malignant fibrohistiocytoma (MFH) of the breast. Primary and postirradiation variants - an ultrastructural study. Pathol Res Pract. 1984;178(3):289–96.
Gladdy RA, Qin LX, Moraco N, Edgar MA, Antonescu CR, Alektiar KM, Brennan MF, Singer S. Do radiation-associated soft tissue sarcomas have the same prognosis as sporadic soft tissue sarcomas? J Clin Oncol. 2010;28(12):2064–9.
Riad S, Biau D, Holt GE, Werier J, Turcotte RE, Ferguson PC, Griffin AM, Dickie CI, Chung PW, Catton CN, O’sullivan B, Wunder JS. The clinical and functional outcome for patients with radiation-induced soft tissue sarcoma. Cancer. 2012;118(10):2682–92.
Kokkali S, Moreno JD, Klijanienko J, Theocharis S. Clinical and molecular insights of Radiation-Induced breast sarcomas: Is there hope on the Horizon for Effective Treatment of this aggressive disease? Int J Mol Sci. 2022;23(8):4125.
Lei T, Yang Y, Shi Y, Deng X, Peng Y, Wang H, Chen T. Clinicopathological features and genomic profiles of a group of secretory breast carcinomas in which progressive cases have more complex genomic features. Diagn Pathol. 2022;17(1):101.
Mery CM, George S, Bertagnolli MM, Raut CP. Secondary sarcomas after radiotherapy for breast cancer: sustained risk and poor survival. Cancer. 2009;115(18):4055–63.
Hardy TJ, An T, Brown PW, Terz JJ. Postirradiation sarcoma (malignant fibrous histiocytoma) of axilla. Cancer. 1978;42(1):118–24.
Tsuneyoshi M, Enjoji M. Postirradiation sarcoma (malignant fibrous histiocytoma) following breast carcinoma: an ultrastructural study of a case. Cancer. 1979;45(6):1419–23.
Meunier B, Levêque J, Prisé EL,Kerbrat P, Grall JY. Three cases of sarcoma occurring after radiation therapy of breast cancers. Eur J Obstet Gynecol Reprod Biol. 1994;57(1):33–6.
Kirova YM, Vilcoq JR, Asselain B, Sastre-Garau X, Fourquet A. Radiation-induced sarcomas after radiotherapy for breast carcinoma: a large-scale single-institution review. Cancer. 2005;104(4):856–63.
Horii R, Fukuuchi A, Nishi T, Takanashi R. A case of malignant fibrous histiocytoma after breast conserving therapy for breast cancer. Breast Cancer. 2000;7(1):75–7.
Komaei I, Guccione F, Sarra F, Palmeri E, Ieni A, Cardia R, Currò G, Navarra G, Palmeri R. Radiation-induced undifferentiated pleomorphic sarcoma of the breast: a rare but serious complication following breast-conserving therapy. A case report and literature review. G Chir. 2019;40(6):544–50.
Hatta N, Horita Y. Undifferentiated pleomorphic sarcoma in a patient with Cowden syndrome after radiotherapy for breast cancer. J Dermatol. 2019;46(2):e73–5.
Kadouri L, Sagi M, Goldberg Y, Lerer I, Hamburger T, Peretz T. Genetic predisposition to radiation induced sarcoma: possible role for BRCA and p53 mutations. Breast Cancer Res Treat. 2013;140(1):207–11.
Noh JM, Huh SJ, Choi DH, Park W, Nam SJ. Two cases of post-radiation sarcoma after breast cancer treatment. J Breast Cancer. 2012;15(3):364–70.
Quadros CA, Vasconcelos A, Andrade R, Ramos RS, Studart E, Nascimento G, Trajano A. Good outcome after neoadjuvant chemotherapy and extended surgical resection for a large radiation-induced high-grade breast sarcoma. Int Semin Surg Oncol. 2006;3:18.
S M Pierce, A Recht, T I Lingos, A Abner, F Vicini, B Silver, A Herzog, J R Harris. Long-term radiation complications following conservative surgery (CS) and radiation therapy (RT) in patients with early stage breast cancer.Int J Radiat Oncol Biol Phys. 1992;23(5):915–23
Joo MW, Kang YK, Ogura K, Iwata S, Kim JH, Jeong WJ, Niu XH, Chinder PS, Kim HS, Seo SW, Chung YG. Post-radiation sarcoma: A study by the Eastern Asian Musculoskeletal Oncology Group. PLOS ONE. 2018;13(10):e0204927.
Cui YY, Han LY, Shang JF, Fang W, Zhao M, Chen D, Liu HG. Primary cardiac undifferentiated pleomorphic sarcoma is associated with TP53 mutation during lack of MDM2 amplification, and targeted sequencing analysis reveals potentially actionable targets. Hum Pathol. 2022;123:113–22.
Lesluyes T, Baud J, Perot G, Charon-Barra C, You A, Valo I, Bazille C, Mishellany F, Leroux A, Renard-Oldrini S,Terrier P, Cesne AL, Laé M, Piperno-Neumann S, Sylvie Bonvalot S, Neuville A, Collin F, Maingon P, Coindre JM, Chibon F. Genomic and transcriptomic comparison of post-radiation versus sporadic sarcomas. Mod Pathol. 2019;32(12):1786–94.
Cancer Genome Atlas Research Network. Comprehensive and Integrated Genomic Characterization of Adult Soft Tissue Sarcomas. Cell. 2017;171(4):950–65.
Thoenen E, Curl A, Iwakuma T. TP53 in bone and soft tissue sarcomas. Pharmacol Ther. 2019;202:149–64.
Ali NM, Niada S, Brini AT, Morris MR, Kurusamy S, Alholle A, Huen D, Antonescu CR, Tirode F, Sumathi V, Latif F. Genomic and transcriptomic characterisation of undifferentiated pleomorphic sarcoma of bone. J Pathol. 2019;247(2):166–76.
Petry V, Bonadio RC, Cagnacci AQC, Senna LAL, Campos RdNG, Cotti GC, Hoff PM, Fragoso MCBV, Estevez-Diz MDP. Radiotherapy-induced malignancies in breast cancer patients with TP53 pathogenic germline variants (Li–Fraumeni syndrome). Familial Cancer. 2020;19(1):47–53.
Knudsen ES, Pruitt SC, Hershberger PA, Witkiewicz AK, Goodrich DW. Cell Cycle and Beyond: Exploiting New RB1 Controlled Mechanisms for Cancer Therapy. Trends Cancer. 2019;5(5):308–24.
Di Fiore R, D'Anneo A, Tesoriere G, Vento R. RB1 in cancer: different mechanisms of RB1 inactivation and alterations of pRb pathway in tumorigenesis. J Cell Physiol. 2013;228(8):1676–87.
Widden H, Placzek WJ. The multiple mechanisms of MCL1 in the regulation of cell fate. Commun Biol. 2021;4(1):1029.
Hong AL, Guerriero JL, Doshi MB, Kynnap BD, Kim WJ, Schinzel AC, Modiste R, Schlauch AJ, Adam RM, Kwiatkowski DJ, Beroukhim R, Letai A, Rosenberg JE, Hahn WC. MCL1 and DEDD Promote Urothelial Carcinoma Progression. Mol Cancer Res. 2019;17(6):1294–304.
Stine ZE, Walton ZE, Altman BJ, Hsieh AL, Dang CV. MYC, Metabolism, and Cancer. Cancer Discov. 2015;5(10):1024–39.
Sio TT, Mansfield AS, Grotz TE, Graham RP, Molina JR, Que FG, Miller RC. Concurrent MCL1 and JUN amplification in pseudomyxoma peritonei: a comprehensive genetic profiling and survival analysis. J Hum Genet. 2014;59(3):124–8.
Vrana JA, Bieszczad CK, Cleaveland ES, Ma Y, Park JP, Mohandas TK, Craig RW. An MCL1-overexpressing Burkitt lymphoma subline exhibits enhanced survival on exposure to serum deprivation, topoisomerase inhibitors, or staurosporine but remains sensitive to 1-beta-D-arabinofuranosylcytosine. Cancer Res. 2002;62(3):892–900.
Allen TD, Zhu CQ, Jones KD, Yanagawa N, Tsao MS, Bishop JM. Interaction between MYC and MCL1 in the genesis and outcome of non-small-cell lung cancer. Cancer Res. 2011;71(6):2212–21.
Lourenco C, Resetca D, Redel C, Lin P, MacDonald AS, Ciaccio R, Kenney TMG, Wei Y, Andrews DW, Sunnerhagen M, Arrowsmith CH, Raught B, Penn LZ. MYC protein interactors in gene transcription and cancer. Nat Rev Cancer. 2021;21(9):579–91.
Dang CV. MYC on the path to cancer. Cell. 2012;149(1):22–35.
Romieu-Mourez R, Kim DW, Shin SM, Demicco EG, Landesman-Bollag E, Seldin DC, Cardiff RD, Sonenshein GE. Mouse mammary tumor virus c-rel transgenic mice develop mammary tumors. Mol Cell Biol. 2003;23(16):5738–54.
Morton JP, Sansom OJ. MYC-y mice: from tumour initiation to therapeutic targeting of endogenous MYC. Mol Oncol. 2013;7(2):248–58.
Tron AE, Belmonte MA, Adam A, Aquila BM, Boise LH, Chiarparin E, Cidado J, Embrey KJ, Gangl E, Gibbons FD, Gregory GP, Hargreaves D, Hendricks JA, Johannes JW, Johnstone RW, Kazmirski SL, Kettle JG, Lamb ML, Matulis SM, Nooka AK, Packer MJ, Peng B, Rawlins PB, Robbins DW, Schuller AG, Su N, Yang W, Ye Q, Zheng X, Secrist JP, Clark EA, Wilson DM, Fawell SE, Hird AW. Discovery of Mcl-1-specific inhibitor AZD5991 and preclinical activity in multiple myeloma and acute myeloid leukemia. Nat Commun. 2018;9(1):5341.
Jovanović KK, Roche-Lestienne C, Ghobrial IM, Facon T, Quesnel B, Manier S. Targeting MYC in multiple myeloma. Leukemia. 2018;32(6):1295–306.
Fitzel R, Secker-Grob KA, Keppeler H, Korkmaz F, Schairer R, Erkner E, Schneidawind D, Lengerke C, Hentrich T, Schulze-Hentrich JM, Schneidawind C. Targeting MYC in combination with epigenetic regulators induces synergistic anti-leukemic effects in MLLr leukemia and simultaneously improves immunity. Neoplasia. 2023;41:100902.
Hofvander J, Puls F, Pillay N, Steele CD, Flanagan AM, Magnusson L, Nilsson J, Mertens F. Undiferentiated peomorphic sarcomas with PRDMl0 fusions have a distinct gene expresion profile. J Pathol. 2019;249(4):425–34.
Hofvander J, Tayebwa J, Nilsson J, Magnusson L, Brosjö O, Larsson O, Vult von Steyern F, Mandahl N, Fletcher CD, Mertens F. Recurrent PRDM10 gene fusions in undifferentiated pleomorphic sarcoma. Clin Cancer Res. 2015;21(4):864–9.
Funding
This work was supported by grants from the Changzhou Science and Technology Project (Grant No. QN202114), Changzhou Science and Technology Program (Grant NO. CJ20220084) and Top Talent of Changzhou “The 14th Five-Year Plan” High-level Health Personnel Training Project (Grant No.2022260).
Author information
Authors and Affiliations
Contributions
Ting Lei and Qing Li contributed in the writing of the manuscript; Zhiyi Shen, Mengjia Shen, and Lingfang Du prepared the Figs. 1, 2 and 3; Yongqiang Shi, Yan Peng, Zidi Zhou, Wenyue Da, and Xi Chen prepared the Figs. 4 and 5 and the Tables 1 and 2. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lei, T., Shen, Z., Shen, M. et al. Clinicopathological and genetic characterization of radiotherapy-induced undifferentiated pleomorphic sarcoma following breast cancer: a case series of three tumors and comprehensive literature review. Diagn Pathol 19, 110 (2024). https://doi.org/10.1186/s13000-024-01534-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13000-024-01534-w