Abstract
Background
Repetitive transcranial magnetic stimulation (rTMS) has recently gained relevance in treating different psychiatric disorders. Limited evidence suggests that the beneficial effects of rTMS on psychopathology could be at least partly mediated through changes in inflammatory response. This systematic review summarizes the literature on whether rTMS can modulate inflammatory markers and thus positively influence the course of psychiatric illnesses.
Materials and methods
A systematic review of rTMS and inflammatory markers in psychiatric diseases was conducted according to PRISMA guidelines. Information on the association between rTMS treatment response and changes of inflammatory markers was extracted. The quality of the studies was assessed using the National Heart, Lung, and Blood Institute for human studies and the Systematic Review Center for Laboratory Animal Experimentation for animal studies.
Results
This review includes 17 studies (2 animal and 15 human studies) on the relationship between rTMS treatment response and changes of inflammatory markers. Positive changes in microglial activity and anti-inflammatory effects were associated with behavioral improvement in animal models of depression. However, these findings have not been consistently replicated in human studies focusing on treatment-resistant depression. While several studies reported rTMS-induced alterations in peripheral inflammatory markers, only two could demonstrate their association to clinical treatment response. Notably, most studies showed poor or moderate quality in the bias assessment.
Conclusions
While certain human studies suggest an association between rTMS-induced anti-inflammatory effects and improvement in psychopathology, heterogeneity, and underpowered analyses constrain the generalizability of these results. The discrepancy between animal and human findings highlights the need for larger, standardized human studies.
Trial registration
(PROSPERO Registration: CRD42023492732).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transcranial Magnetic Stimulation (TMS) is a non-invasive technique that facilitates targeted stimulation of cortical areas by generating an electromagnetic alternating field using a magnetic stimulator [1]. This technique induces an intracortical tissue current, depolarizing the membrane and eliciting an action potential in pyramidal cells of the stimulated area [2]. When administered repetitively, known as repetitive TMS (rTMS), this non-invasive neuromodulation technique has proven to be an effective and well-tolerated alternative therapy for neurological conditions [3] and various psychiatric disorders [4].
Both 10 Hz rTMS and intermittent theta burst stimulation (iTBS) of the left dorsolateral prefrontal cortex (DLPFC) have been approved by the U.S. Food and Drug Administration (FDA) for patients with unipolar depression who have not responded to at least one antidepressant pharmaceutical treatment [5,6,7,8]. Additionally, focal stimulation of other distinct brain regions has exhibited symptom improvement in various studies with schizophrenia, obsessive-compulsive disorder, and bipolar depression [9,10,11]. Although the evidence is not as robust as for depressive disorders, it is possible that rTMS could be used clinically on a larger scale in the near future.
Through the modulation of cortical excitability and synaptic plasticity, rTMS can increase or decrease neuronal firing rates, dependent on the stimulation frequency [12]. How this general mechanism translates into positive clinical outcomes in different neuropsychiatric disorders remains unclear.
In recent years, numerous studies have illustrated a profound bidirectional association between inflammatory processes and psychiatric diseases such as depression and schizophrenia [13, 14]. This association between inflammation and mental health conditions has been established to such an extent that some researchers propose to classify depression as a chronic inflammatory disease [15]. In addition, the extent of systemic inflammation appears to influence the efficacy and clinical response to pharmacotherapy in depression [16]. Recent evidence also suggests a direct link between neuroplasticity and the anti-inflammatory effects of treatment [17]. As an example, the occurrence of depression-like symptoms in a rat model of induced intranigral inflammation was associated with the decrease of the neuroplasticity-associated brain-derived neurotropic factor (BDNF) in the hippocampus [18, 19]. Given that rTMS directly influences synaptic and brain plasticity [20], it is possible that this pathway could contribute to the anti-inflammatory effects of rTMS procedures in general. Luo et al. demonstrated, for instance, in an experimental animal study on ischemic stroke that long-term rTMS can promote the anti-inflammatory polarization of microglia [21]. Further, mice under rTMS treatment exhibited activation of the BDNF signaling pathway, leading to a proliferative effect in the hippocampus [22].
Considering this recent evidence, it is crucial to integrate possible anti-inflammatory mechanisms and treatment effects of rTMS to gain further insights into the therapeutic impact of this clinical intervention. Despite existing evidence of associations between rTMS treatment and individual cytokines in affective disorders, a comprehensive overview of general influencing factors is lacking. Moreover, no studies have systematically investigated the transdiagnostic and translational anti-inflammatory effects of rTMS and its impact on peripheral and systemic inflammation in psychiatric disorders.
The primary objective of this systematic review is to compile state-of-the-art findings on whether rTMS can modulate inflammatory markers and thus positively influence the course of psychiatric symptomatology. This review includes studies on humans and animals as well as on different psychiatric disorders.
Materials and methods
Study selection criteria
We included studies that met the following criteria: (1) studies involving both humans and animals; (2) human participants aged 18 years or older; (3) individuals with psychiatric disorders who received repetitive transcranial magnetic stimulation (rTMS) as a treatment, regardless of the specific rTMS protocol used; (4) in the case of animal studies, models in which transcranial magnetic stimulation was tested for psychiatric diseases; (5) prospective study designs, including longitudinal studies, cohorts, and randomized clinical trials, or experimental studies; (6) rTMS studies that assessed either peripheral or central inflammation. Conversely, we excluded studies involving participants under 18, pregnant participants with psychiatric disorders (e.g., postpartum depression), participants with any substance use disorder, animal models for substance use disorders, individuals or animal models with primary neurological or neurodegenerative disorders, or studies investigating other types of non-invasive brain stimulation. Additionally, we excluded case reports, case series, literature reviews, systematic reviews, meta-analyses, and retrospective studies. Articles that were not available as full-text were also excluded.
The year of publication and the language of the articles were not considered exclusion criteria. In cases of potential language barriers, we utilized a freely available translation tool (Google Translate, Google Inc., United States of America) to extract the primary information from the manuscripts.
Literature search strategies
A systematic literature search was conducted between 15/04/2023 and 25/11/2023 across various scientific literature databases, including MEDLINE (PubMed, National Center for Biotechnology Information, National Library of Medicine, United States of America), EBSCO (EBSCO Industries Incorporated, United States of America), Web of Science (Clarivate Analytics, United States of America), and CENTRAL (Cochrane Central Register of Controlled Trials, Cochrane Library, United States of America).
To select articles, we performed the literature search by defining three distinct categories: the “psychiatric disorders” category (depression; depressive disorder; depressive disorder, treatment-resistant; depressive disorder, major; obsessive-compulsive disorder; obsessive behavior; compulsive behavior; stress disorders, post-traumatic; anxiety disorders; bipolar disorder; schizophrenia), the “inflammation” category (immunity, cytokines, interleukins, inflammation, acute phase proteins, blood cell count), and the “repetitive transcranial magnetic stimulation” category (transcranial magnetic stimulation, repetitive). The selection of psychiatric disorders was based on recommendations found in various international guidelines for rTMS treatment [23, 24]. Subsequently, we employed the defined search categories with the following Boolean operations: “category inflammation” (one term) AND “category repetitive transcranial magnetic stimulation” (one term), as well as “category psychiatric disorders” (one term) AND “category inflammation” (one term) AND “category repetitive transcranial magnetic stimulation” (one term).
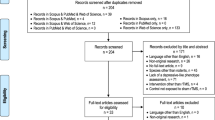
The selection process is visually presented following the PRISMA guidelines [25] in Fig. 1.
Selection process
Subsequently, the literature search results were extracted in formats such as .csv, .ris, or .txt files, primarily depending on the search platform and database utilized. These data were then imported into the web application Rayyan.ai [26], where BPP and SI independently reviewed all prospective study designs and experimental studies, adhering to the inclusion criteria based on the title or abstract. Any discrepancies in the selection of articles were resolved through consensus among all authors. Each author subsequently conducted a full-text screening of the articles to exclude those not meeting the inclusion criteria. Similarly, disagreements on inclusion and exclusion criteria were addressed through a consensus-based approach (Fig. 1).
Quality of studies
For human studies, we evaluated quality and risk of bias using the National Heart, Lung, and Blood Institute (NHLBI) criteria, as previously described [27]. In the case of animal studies, we utilized the SYRCLE checklist to assess both quality and risk of bias [28].
Following the initial screening, the remaining human studies were randomly allocated to three authors (BPP, SI, EL), while the animal studies were similarly assigned to four authors (JR, MS, SI, EL). The authors were instructed not to disclose the titles or content of the randomly assigned articles to their colleagues to ensure a blinded evaluation. Additionally, authors were explicitly advised not to seek assistance or support from other team members while reviewing and assessing the quality of the assigned studies.
PRISMA flow diagram. *Stekic et al. 2022 was excluded because it was an animal study mainly centered on Alzheimer’s Disease (see exclusion criteria). From Page MJ et al. [25]
Results
Description of the studies and bias assessment
The literature search yielded a total of 531 potential studies. After removing 211 duplicates, 320 studies remained. Among these, 303 studies were excluded during the screening phase as they did not meet the inclusion criteria, and one study was excluded later due to its focus on animal models of Alzheimer’s Disease [29]. The remaining 17 studies were retrieved and included in the quality control analysis. Out of these, 2 were animal studies [30, 31], 7 were human longitudinal studies [32,33,34,35,36,37,38], and 8 were human clinical trials [39,40,41,42,43,44,45,46]. While the year of publication was not an exclusion criterion, the papers included in the systematic review covered the time period from 2019 to 2023. Among the 17 selected papers, 2 were published in 2019, 3 in 2020, 5 in 2021, 6 in 2022, and 1 in 2023.
For the included human studies, we used the NHLBI tools for clinical and observational cohort studies to assess and rate their quality. In the case of animal studies, we applied the SYRCLE checklist to evaluate the risk of bias. Two independent blinded raters assessed the included studies after the screening process. Tables S1 to S3 present the inter-rater agreement of quality ratings and the scores assigned to each study for human (observational cohort studies and clinical studies) and animal studies.
Animal studies
We found two animal studies relating to rTMS effects on inflammation in models of psychiatric diseases [30, 31]. The first animal study investigated the anti-inflammatory effects of rTMS in a depression animal model using mice and focusing on glial activation [30]. For the measures of the cytokines, enzyme-linked immunosorbent assay (ELISA) was used to measure the concentrations of the cytokine IL-1β, IL-6 and TNF-α in specific brain regions [30]. In case of microglia activation, immunofluorescence was performed on brain tissue, studying specific cellular markers in different brain regions [30]. Western blot and quantitative real-time polymerase chain reaction was used to study protein and gene expression in brain tissue, respectively [30]. The study revealed that rTMS treatment, following exposure to chronic unpredictable mild stress (CUMS), increased sucrose intake, decreased immobility time in the forced swim test, and enhanced exploratory behavior in the open field test. These findings suggest a reversal of CUMS-induced depressive-like behavior after rTMS treatment. Regarding neuroinflammatory mechanisms, rTMS treatment reduced microglial activation levels. Furthermore, rTMS reversed the polarization of microglia from the M1 to M2 phenotype and increased astrocyte levels. Additionally, rTMS lowered the concentrations of pro-inflammatory cytokines such as IL-6, β, and TNF-α in the hippocampus and prefrontal cortex (PFC) by modulating the TLR4/NF-κB/NLRP3 signaling pathway in the animal model of depression.
The second animal study examined the effects of rTMS on depression and anxiety-like behavior and on Nuclear Factor-E2-related Factor 2-mediated (Nrf2) anti-inflammatory processes in rats [31]. A one-week rTMS treatment successfully prevented CUMS-induced depression- and anxiety-like behaviors. The one-week treatment with real rTMS significantly increased the nuclear expression of the Nrf2 protein compared to sham rTMS. Moreover, after rTMS treatment, the expression of TNF-α, inducible nitric oxide synthase (iNOS), IL-1β, and IL-6 decreased in the hippocampus, which counteracted the initial elevation induced by CUMS. All the above-mentioned effects of rTMS were nullified after Nrf2 knockdown by transfection of Nrf2 small interfering RNA. These results imply that Nrf2 may play a crucial role in the antidepressant and anti-inflammatory effects of rTMS.
Human studies - longitudinal observational studies
Of the 15 human studies included, we identified seven longitudinal studies, as described in Table 1 [32,33,34,35,36,37,38]. The quality control of these clinical studies is reported in Table S2 and the overview of the rTMS-induced changes in Table 2. Generally, these studies assessed peripheral cytokines and other inflammation-related markers, including BDNF, metabolites of the kynurenine pathway, oxidized phosphatidylcholines and oxylipins, as well as soluble Triggering receptor expressed on myeloid cells-2 (sTREM2) during rTMS treatment in patients with depression. Only one study reported findings with microRNA involved in inflammatory processes (miRNA-16-5p, miRNA-93-5p, and miRNA-146a-5p). Initially, all studies reported a significant reduction in depression severity following rTMS therapy. However, the reported inflammatory parameter changes after rTMS treatment exhibited broad variability.
Peripheral cytokines
Three longitudinal studies evaluated changes in peripheral cytokines after rTMS therapy in patients with TRD [35,36,37]. In a pilot longitudinal study, following rTMS therapy, IL-1β, TNF-α, and IL-6 did not change significantly in the 11 participants with TRD [35]. Further, no significant differences were observed between responders and non-responders after rTMS therapy [35]. However, the decrease in IL-1β after rTMS therapy was associated with an improvement in part 3 of the Color Stroop Test. Changes in other cytokines and cognitive tests did not show significant correlations [35]. In the second longitudinal study [36], the authors reported no significant effects of rTMS on TNF-α concentration in patients with TRD. However, TNF-α concentrations showed a positive significant correlation with the final HAM-D scores in the rTMS group [36]. Finally, the third longitudinal study [37] reported significant differences in IL-18 concentrations between both treatment groups (rTMS and medication groups) and the control group (baseline only assessed). Upon excluding the control group from the analysis, the authors found significant differences for IL-8 and IFN-γ when comparing the rTMS to the medication group [37]. Furthermore, rTMS treatment increased the TGF-β1 level. In contrast, the medication groups exhibited increased IL-18, IL-6, and IL-1β after two weeks of treatment [37]. However, in the last study, is unclear whether the changes in inflammatory parameters were associated with improvement in psychopathology, finding only significant results between baseline inflammation and symptom improvement, as described in Table 1 [37].
Metabolites of the kynurenine pathway
One pilot longitudinal study in patients with TRD, which compared three different treatment options (pharmacotherapy, ECT, and rTMS), showed no significant reductions of metabolites of the kynurenine pathway (kynurenine, kynurenic acid, 3-hydroxykynurenine or quinolinic acid), which is related to inflammatory processes [47], before and after rTMS treatment [32]. Despite the lack of significant changes in kynurenine pathway metabolites, a reduction in TNF-α was observed during rTMS treatment. Similarly, the rTMS group showed a significant increase of 3-hydroxykynurenine-to-kynurenine (HK/KYN) ratio after four weeks of treatment. However, no analyses were performed to establish an association between the decrease in TNF-α or HK/KYN and the improvement of depressive symptoms.
Lipid mediators and steroids
In a longitudinal study with an exploratory design, oxidized phosphatidylcholines (OxPc) and oxylipins were assessed before and after rTMS treatment in patients with major depressive disorders [33]. As reported by the author, oxylipins is produced by enzymes such as cyclooxygenase or lipoxygenase and plays a crucial role in inflammation [33, 48]. At baseline, non-fragmented OxPc and long-chain products were significantly elevated in patients compared to healthy controls [33]. When comparing rTMS remitters and non-remitters at baseline, the remitters exhibited significantly higher total OxPc than the non-remitters, with significant differences observed in fragmented OxPCs, aldehydes, carboxylic acids, PONPC, and 1-palmitoyl-2-azelaoyl-sn-glycero-3-phosphocholine [33]. However, there were no significant alterations in OxPCs following rTMS treatment in patients with MDD. Further, no significant changes in OxPC concentration were observed after rTMS treatment when categorizing the patient group into remitters and non-remitters. Additionally, in identifying 32 different oxylipin species, no differences were discerned between remitters and non-remitters concerning pre-rTMS concentrations [33].
Testosterone, a steroid hormone, presents an inhibitory effect on the expression of TNF-α, IL-6, and IL-1 [49]. One included study evaluated if testosterone changed after rTMS along with symptom improvement. However, testosterone levels did not show significant group, time, or group-by-time interaction effects. Moreover, the decrease in testosterone was not associated with the rTMS treatment [38].
Growth factors
One longitudinal study assessed the concentrations of BDNF and VEGF before and after rTMS treatment in participants with major depression [36]. As previously noted, BDNF and VEGF have been reported to be associated with inflammatory processes [17, 50]. In this study [36], rTMS revealed significant increase between the third and the first measurement time point for BDNF concentrations. Conversely, changes in VEGF during rTMS treatment were non-significant in pairwise differences tests [36]. Nevertheless, initial BDNF serum levels correlated negatively with BDNF increase after five rTMS procedures. Furthermore, the overall percentage of BDNF increase during treatment correlated negatively with the initial MADRS and HAM-D scores [36]. BDNF correlations with clinical scores after treatment were not significant. Similarly, no significant correlations were observed between VEGF and clinical scores [36].
Micro-RNA involved in inflammatory processes
Regarding miRNAs involved in inflammatory processes, all three tested miRNAs (miRNA-16-5p, miRNA-93-5p, and miRNA-146a-5p) demonstrated higher ΔCt values in the rTMS group compared to the medication group, indicating lower expression of these miRNAs in the rTMS group [37]. Additionally, lower expression of miRNA-146a-5p at baseline correlated with less successful rTMS treatment as assessed with HAM-D-17, MADRS, and PHQ-9 scores. Interestingly, in the rTMS group, ΔCt values of miRNA-93-5p positively correlated with IL-18 concentrations [37].
Other inflammatory and immune response markers
Soluble triggering receptor expressed on myeloid cells – 2 (sTREM2)
No significant reduction of sTREM2 level could be observed before and after rTMS treatment. The changes in sTREM2 were not correlated with age, sex, BMI, smoking status and symptom improvement [34].
Serum amyloid A (SAA)
Serum amyloid A (SAA), an acute-phase protein [51], did not showed changes in a longitudinal study during rTMS treatment in patients with MDD [38]. In addition, the authors reported no significant group, time, or group-by-time interaction effects. The decrease of SAA was not associated with the rTMS treatment. However, the authors reported a significant relationship between the reduction of SAA levels and the decrease in HAM-D in the rTMS group during the second week of treatment [38].
Study limitations
Overall, the included longitudinal studies had several limitations that must be considered when evaluating the quality of the results. Firstly, none of the studies reported a power analysis. Additionally, there were non-uniform rTMS protocols across the studies, comparisons between different diseases using various stimulation methods, exploratory designs with small sample sizes (i.e., n < 30), no correction for medication effects, a loss of information exceeding 20%, and a lack of adjustment for sample characteristics (i.e., sex, age, or BMI).
Human studies - clinical studies
Out of the 15 included human studies, we identified eight clinical studies [39,40,41,42,43,44,45,46]. The quality control of these clinical studies is reported in Table S3. Similar to the included longitudinal studies, these clinical trials evaluated peripheral cytokines as well as other inflammation-related markers, such as white blood cells (WBC), acute-phase proteins (e.g., CRP, antithrombin III), metabolites of the kynurenine pathway, and growth factors (e.g. BDNF), and their relations to clinical outcomes. Six out of eight trials included patients with depression, one with schizophrenia, and one post-stroke patients. The latter was included since the authors also evaluated the effects of rTMS on depressive symptoms assessed with the geriatric depression scale (GeDS) after the ischemic event. Short descriptions of the clinical studies are summarized in Table 3 and the overview of the rTMS-induced effects is summarized in Table 4. In the clinical trials, the reported changes of inflammatory parameters after rTMS treatment exhibited similar variability as in the longitudinal studies.
Peripheral cytokines
One prospective clinical study in patients with post-stroke cognitive impairment demonstrated by performing a reverse transcription polymerase chain reaction just after the rTMS treatment a downregulated expression of mRNA IL-1β, IL-6, TNF-α, and TGF-β, in comparison to the mRNA expression before the rTMS-treatment of the above-mentioned cytokines [39]. Twelve weeks after competition of the rTMS treatment, a sustained reduction in gene expression of IL-1β was found [39]. Furthermore, changes in mRNA expression of IL-6 correlated negatively and significant with changes in the Auditory Verbal Learning Test and with negatively with changes in Complex Figure Test scores. However, rTMS treatment did not reduce depressive symptoms in the GeDS in post-stroke participants, and rTMS showed only marginal effects on participants with moderate-to-severe depression. In addition, there were no correlations between changes in inflammatory parameters and depression symptomatology based on the GeDS scores in the study participants with post-stroke cognitive impairment.
In another prospective clinical study [40] examining 58 elderly patients with treatment-resistant depression (29 in rTMS group and 23 in control group with medication), the effects of rTMS on serum levels of IL-1β and TNF-α and their association to changes in depressive symptoms were investigated. HAMD-24 scores significantly reduced in the rTMS group during the treatment. Additionally, both IL-1β and TNF-α concentrations were significantly reduced in the rTMS group. Finally, HAMD-24 scores were positively correlated with both IL-1β and TNF-α concentrations. Nevertheless, it was not specified which HAMD-24 scores (e.g., at the beginning or the end of the trial) correlated with IL-1β or TNF-α.
A prospective, double-blind, controlled trial involving 57 patients with depression (29 in the rTMS group and 28 in the sham-stimulation group) and 30 healthy controls focused on differences in baseline inflammatory cytokines between patients and healthy controls, changes in inflammatory cytokines during rTMS treatment, and correlations between changes in HAMD-24 scores and inflammatory cytokines after rTMS treatment [41]. Regarding baseline inflammatory cytokines, TNF-α concentrations were significantly lower in the healthy controls than in the patients with depression; however, IFN-γ, IL-4, and IL-2 were significantly higher in the healthy controls. Concerning changes in inflammatory cytokines during rTMS treatment, the rTMS group exhibited significant increase in IL-2 and CRP-hs levels after two weeks of treatment. Between weeks 2 and 12, the levels of TNF-α and IFN-γ underwent significant decrease. Finally, after 12 weeks of treatment, significant increases were observed in the levels of CRP-hs. Furthermore, the change in depressive symptoms (measured with the HAMD-24) was negatively correlated with the changes of TNF-α after two weeks and negatively correlated with the changes of IL-2 after 12 weeks; however, changes in depressive symptoms positively correlated with changes of IL-4 in both the rTMS and the sham group.
In another randomized sham-controlled trial involving 53 patients with depression (27 in the rTMS treatment group and 26 in the sham-stimulation group), the study aimed to investigate the effects of theta-burst stimulation (TBS), a variant of rTMS treatment, on inflammatory cytokine levels and depressive symptoms. No significant changes in serum inflammatory cytokines, including IL-1β, IL-2, IL-4, IL-5, IL-6, IL-12p40, and IP-10, were observed after the treatment in either group. However, an increase in CRP was observed in the sham-stimulation group [42]. There was a significant difference in changes in HAMD-21 scores between the groups (sham > TBS) after four weeks of treatment.
Cellular immunity
One randomized double-blinded controlled trial [46] investigated the clinical effects of high-frequency rTMS on 47 long-term hospitalized veterans with schizophrenia (27 in the rTMS group, 20 in the sham group). The study aimed to identify possible correlations between clinical improvement and inflammatory parameters. No significant correlation was observed between WBC count and overall changes in the Positive and Negative Syndrome Scale (PANSS). However, an in-depth analysis of specific items within the PANSS revealed a negative association between WBC count at baseline and the improvement of a subgroup of positive symptoms, which was also confirmed by a regression analysis.
Acute phase proteins
One randomized double-blinded controlled trial reported no significant correlations between CRP and overall changes in the PANSS in patients with schizophrenia [46]. Finally, one clinical trial [43] examined the effects of occipital rTMS treatment on four different inflammation-related proteins (ATIII, CRP, ITIH4, and VDB) in 74 patients with Major Depressive Disorder (MDD), who were drug-naive or had been drug-free for at least two weeks. In this study, participants were allocated into three groups: a standard rTMS group, an individualized rTMS group, and a sham-stimulation group (see Table 1). After individualized rTMS therapy, the concentrations of all proteins were significantly reduced, with the exception of CRP. Participants in the standard rTMS group showed significant reductions in all four proteins. Sham-group did not show significant differences for the four parameters mentioned above. Regarding psychometric assessments, in the individualized rTMS group, only changes in ATIII showed significant positive correlations with changes in HAMD-24, SDS, BHS, and SAS. Moreover, changes in ATIII showed a significant positive effect in a multiple linear regression model with changes in HAMD-24 in the individualized rTMS group. Finally, baseline ATIII in both the standard and the individualized rTMS groups exhibited good predictive performance for the response after five days of rTMS treatment and predicted the values of HAMD-24 at follow-up. HAMD-24 values at follow-up were also predicted by changes in ATIII following rTMS treatment.
Metabolites of the kynurenine pathway
Two randomized controlled trials [44, 45] studied the effects of changes of metabolites of the kynurenine pathway along changes in the psychopathology. In both trials, no significant changes on the metabolites of the kynurenine pathway correlated with changes in psychopathology. As a secondary finding for this systematic review, only phenylalanine showed a significant effect for time during rTMS treatment in both trials. Interestingly, neopterin correlated positively before rTMS with the KYN/TRP, but this correlation was not found after rTMS [45].
Growth factors
One clinical trial reported negative correlations between HAMD-24 scores and BDNF [40]. However, it was not specified which HAMD-24 scores (e.g., at the beginning or the end of the trial) correlated with BDNF [40]. Another trial reported that after rTMS, BDNF concentrations correlated negatively with neopterin values but positively with nitrite concentrations [45]. Neopterin before rTMS was inversely correlated with BDNF, but this correlation was not found after rTMS [45].
Study limitations
Firstly, all studies lacked of a power analysis and an intention-to-treat analysis. One study had an exploratory design with small sample sizes (i.e., n < 30) [39, 46]. Some studies reported no blinding in the clinical trial [43,44,45]. In a clinical trial, the control group was described as a “historical control” without an “active” control group – e.g., the sham-stimulation group [39]. Additionally, in one trial the changes in HAMD-24 and inflammatory markers during rTMS treatment were not analyzed [40]. Finally, it remains unclear in some trials whether the concomitant administration confounded the therapeutic effects attributed to rTMS treatment [40,41,42]. Finally, in a trial, randomization was only applied to the healthy controls, and the clinical technician was not blinded [41].
Discussion
Our systematic literature search provides limited evidence that rTMS can positively influence inflammatory markers in animal models and thereby improve their depression-like phenotypes. However, the findings from human studies are more heterogeneous: While some studies have shown positive effects of rTMS on either peripheral inflammatory markers or psychopathology, there has been little solid link between the two. In addition, the identified rTMS studies in humans focused primarily on major depression or treatment-resistant depression and did not provide a solid database for other psychiatric disorders. Similarly, all animal studies included in our search were based on CUMS models.
rTMS is an approved treatment for treatment-resistant depression, supported by robust evidence [52,53,54,55,56]. Guidelines advocate for using rTMS in treating this affective disorder [57]. Beyond depression, rTMS has shown promise and positive effects in treating various disorders such as OCD, PTSD, anxiety disorders, bipolar disorder, and schizophrenia [9, 58,59,60]. Given that depression is the most frequently treated disorder with rTMS, our literature search revealed an abundance of CUMS animal models in rTMS studies. CUMS stands out as a widely used and comprehensive model for depression, recognized for its efficacy in exploring pathophysiological mechanisms [61]. This model has played a crucial role in unraveling the molecular mechanisms of rTMS, enabling a deeper understanding of its antidepressant properties [62]. Chronic stress models, including chronic unpredictable stress (CUS) or CUMS, are particularly sensitive to antidepressant interventions [63].
To our knowledge, this study represents the first systematic review delving into the impact of rTMS on inflammatory diseases across a spectrum of psychiatric disorders. Similarities are reported in the review of Perrin and Pariante, reporting that changes in the HPA axis and levels of cytokines in response to non-convulsive neurostimulation (including rTMS) frequently was not associated with changes in symptoms of depression [64]. However, our investigation employs a translational perspective, from animal experimental models to clinical trials involving human subjects applying rTMS. A recent comparable study - a systematized literature review exploring the effects of rTMS treatment on inflammatory processes in depressive disorders in humans – has been published [65]. The author reported twelve studies, of which only seven indicated a positive association, suggesting an effect of rTMS treatment on inflammatory mechanisms to a certain degree [65]. In our case, we found 7 studies (three longitudinal observational studies and four clinical studies) that reported a modulatory effect of rTMS on inflammatory markers and only two studies (all clinical studies) that reported significant associations between rTMS-induced changes in symptoms and changes in inflammatory markers. While our review yields similar results, disparities arise in the quality assessment of the studies. According to the NLHBI and SYRCLE tool, most studies exhibited poor to fair bias. In some cases, studies reported unclear results concerning association the rTMS-induced changes in symptoms and inflammatory markers (three longitudinal studies and one clinical study). Conversely, the authors of the first scoping review on rTMS and inflammation in depression reported a moderate to good quality in human research [65].
Overall, the low power of the studies included in this systematic review, coupled with methodological heterogeneity and a lack of randomization, hampers the generalization of findings across different studies. Considering the numerous pitfalls in the human studies incorporated in this review, achieving a good quality score seems challenging, even though the topic is underreported. Consequently, further research on this topic is imperative, prioritizing studies with larger sample sizes and a standardized method for rTMS application. Interestingly, the two studies in CUMS animal models exhibited a direct effect of rTMS treatment on inflammatory markers and on depressive-like behavior; a response not adequately replicated in the human studies involving participants with treatment-resistant depression. This discrepancy might arise from a specific limitation of the animal model: While the CUMS model can report that a novel intervention is antidepressant-like, because the model also responds to conventional antidepressants, it cannot predict whether a novel intervention will also be effective in patients who are treatment-resistant [63]. As long as this limitation in animal models persists, there is urgent need for more human studies with sufficient power, larger samples, and standardized rTMS protocols. It should also be noted that the human studies on rTMS shows a smaller effect size compared to other stimulation methods such as electroconvulsive therapy (ECT) [66, 67]. In case of IL-6, for example, the findings of our reports in rTMS-CUMS experiments show very similar results to ECT studies in depressed patients [68] but not in the included rTMS studies in this systematic review.
Results of the systematic review concerning animal studies
Our literature search demonstrates that rTMS can effectively reduce microglial activation in CUMS models, leading to decreased concentrations of key inflammatory cytokines such as IL-6, IL-1β, and TNF-α, accompanied by the suppression of iNOS, specifically in brain regions like the hippocampus and PFC. Furthermore, rTMS shows the potential to enhance the nuclear expression of Nrf2, a key factor in cellular defense mechanisms. Both alterations went along with improvement of the depressive-like phenotype.
Previous literature has suggested that electromagnetic fields, also generated during rTMS treatment, might mitigate neurodegeneration and decrease neuroinflammatory processes within the central nervous system (CNS) [69]. Specifically, these electromagnetic fields have been shown to reduce the production of HIF1α, concurrently decreasing microglial production of inflammatory cytokines (IL-1α, IL-1β, IL-8, and TNF-α). This reduction in inflammation rates induces the recruitment of A2 reactive astrocytes, promoting neurorestoration [69]. In vitro models have demonstrated that electromagnetic fields from rTMS play a modulatory role in cytokine release in microglia, particularly in stimulated brain regions [70]. Furthermore, various animal models for different disorders further support the beneficial effects of electromagnetic fields produced by rTMS, including the promotion of neurogenesis, reduction of apoptosis, and the induction of an anti-inflammatory microglial polarization by decreasing the production of pro-inflammatory cytokines such as IL-1β and TNF-α [21] along with the modulation of Nrf2 expression [71] and reduction of iNOS [72] in the CNS. The consistent findings across various non-psychiatric disease models, mirroring those observed in the included studies with CUMS models, indicate that the electromagnetic fields generated by rTMS exert anti-inflammatory and neuromodulatory effects on the CNS. In case of the included animal studies this anti-inflammatory effect is associated with improvement in depressive-like phenotype.
Results of the systematic review in human studies
On the contrary, only two of 15 human studies – both of them involving participants with depression - reported associations between rTMS-induced changes in symptoms and changes in inflammatory markers – decrease in symptoms associated with a decrease in TNF-α, IL-2 and ATIII concentrations as well as increase in IL-4 concentrations [41, 43]. No association was observed between rTMS-induced changes in psychiatric symptoms and changes in various inflammatory parameters (Tables 2 and 4).
Following our findings, one study reported decrease in symptoms associated with changes in cytokine concentrations, specifically with a decrease in in TNF-α and IL-2 and with an increase in IL-4. The correlation between changes in pro-inflammatory cytokines and changes in psychopathology during drug therapy with antidepressants differ depending on the treatment options. For instance, a meta-analysis reported that, in general, antidepressant drug treatment did only reduce the concentrations of IL-1β, but not of TNF-α and IL-6. After using a stratified subgroup analysis, however, the use of SSRI treatment was also associated with reduced concentrations of IL-6 [73]. However, similar to our findings, another recent meta-analysis revealed that antidepressant treatment significantly reduced peripheral TNF-α concentrations in patients who responded to treatment but not in non-responders [74]. Thus, this meta-analysis concluded a clear relationship between changes in inflammatory markers and changes in psychopathology. ECT, as a treatment option for TRD, also revealed different results compared to rTMS [75]. Specifically, a longitudinal study showed that ECT-induced changes in the cytokine expression of TNF-β correlated to changes in depression severity [76]. Other studies found an increase in anti-inflammatory markers such as IL-4 [77, 78], similar to our results described above. In another multivariate analysis of longitudinal data, it was reported that in parallel to the ECT-induced decrease in depression severity in the MADRS, IL-6 levels also changed, with a primary increase followed by a significant reduction [68, 79]. In contrast to rTMS, these findings showed that ECT significantly reduced pro-inflammatory markers alongside improved symptoms. Besides the different immune modulatory effects, it is also considered that there are differences concerning the stimulation method, being rTMS a treatment option with a lower effect size than ECT, as mentioned before [66, 67].
According to our findings, one study reported significant reductions of ATIII after symptom improvement in TRD patients treated with rTMS. In this case, the open-label nature of the study design, and the fair risk of bias should be considered. ATIII is a protein that regulates the proteolytic activity of procoagulant proteases, inhibiting the coagulation cascade and exhibiting an anticoagulatory effect [80]. As a negative acute-phase protein, ATIII reduces the inflammatory response by inhibiting cytokine and tissue factor production in endothelial cells and monocytes, thereby influencing leukocyte activation [81]. In the case of major depression, ATIII was paradoxically found to be significantly increased in a multi-level proteomics study compared to healthy controls [82]. The study also revealed positive correlations between depression psychopathology and immunological regulation and suggested that coagulation correlates with the severity of psychopathology in depression [82]. On the other hand, one study in patients with anxiety and depression demonstrated that treatment with reduced markers of coagulation in comparison to patients without [83]. Thus, this study postulated that may counteract a procoagulant effect of anxiety or depression [83]. In this study, the patients with serotonergic antidepressants showed higher concentrations of thrombin-antithrombin complex agents (including ATIII). Still, this difference was not significant between both patient groups (with vs. without serotoninergic antidepressants) and between patients and controls [83]. Finally, an ECT study by Stalzhammer and colleagues showed that ATIII was significantly reduced in patients with depression after the first ECT session compared to baseline. However, in this study only the platelet factor 4, and not ATIII, correlated with changes in depressive symptoms [84].
While rTMS did not demonstrate a correlation between changes in psychopathology and inflammation markers in most studies, there were notable correlations between the reduction of inflammation and cognitive improvement since rTMS stimulates a specific brain region, i.e., the DLPFC. In this case, our results of the systematic search showed that a reduced mRNA expression of IL-6 strongly correlated with improved cognitive performance in post-stroke patients [39]. Additionally, a decrease in IL-1β after rTMS therapy was associated with an improvement in part 3 of the Color Stroop Test in patients with depression [35]. IL-6 and IL-1β are critical in cognitive impairments, including working memory and learning impairments [85]. Two longitudinal studies demonstrated that higher IL-β concentrations were associated with poorer cognitive function [86, 87], and overproduction of IL-1β was correlated with negative cognitive function in another study [88, 89]. Therefore, modifying the concentrations of these cytokines through treatment, such as rTMS, might provide a mechanism to improve cognitive performance. Interestingly, two studies in animal models could demonstrate that the neutralization of IL-1β and IL-6 production positively influenced cognitive function [90, 91].
Limitations
The data included in systematic review presents some limitations that have to be considered when interpreting the results. As already mentioned, power analyses were not reported in any of the studies, making it difficult to extrapolate the results of this systematic review. The relatively small sample sizes of at least some studies (i.e., n < 20) cast doubt on sufficient power. In addition, the rTMS protocols in the human studies differed drastically, providing some explanation for the heterogeneity of the results. Medication was not tapered out in most studies. Thus, the results obtained from the studies are possibly confounded by medication. Most clinical trials required additional randomization and most studies had a poor to fair bias in the quality assessment. Therefore, the results in this systematic review should be interpreted with caution. Finally, most of the studies investigated the effects of rTMS in depressive patients or in the CUMS animal model, making conclusion of rTMS-induced anti-inflammatory effects in other psychiatric disorders impossible.
Conclusions
In conclusion, rTMS has demonstrated an anti-inflammatory effect in parallel with an improvement of psychopathology in animal studies and two human studies. Most of the rTMS studies included animal studies with CUMS models and human studies with treatment-resistant depressive patients. However, the majority of the included human studies had not demonstrated rTMS-induced changes in symptoms and changes in inflammatory markers, mainly due to the small sample sizes, the effect size of rTMS treatment (in comparison with other stimulation procedures, such as ECT) and heterogeneity of the findings. In addition, even if CUMS models are commonly used to prove an antidepressant effect of a treatment option, these models are not representative (e.g., for treatment-resistant depression), being the results of these models, therefore not directly translatable [63]. In the case of human studies, more studies are needed with larger sample sizes, mostly due to the lower treatment effect sizes, to detect whether anti-inflammatory properties are a mechanism underlying rTMS-induced improvement in psychopathology.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- ΔCt:
-
(Change) Cycle threshold
- APGAR:
-
Adaptation, Partnership, Growth, Affection, Resolve scale
- ATIII:
-
Antithrombin III
- AUC:
-
Area under the ROC Curve
- AVLT:
-
Auditory Verbal Learning Test
- BDI:
-
Beck Depression Inventory
- BDNF:
-
Brain-derived neurotrophic factor
- BSI-CV-C:
-
Beck Scale for Suicide Ideation – Chinese version
- BHS:
-
Beck Hopelessness Scale
- CDR-SB:
-
Clinical Dementia Rating – Sum of Boxes
- CFT:
-
Complex Figure Test
- CLIA:
-
Chemiluminescence analysis
- CNS:
-
Central nervous system
- CST:
-
Color Stroop Test
- CTQ-SF:
-
Childhood Trauma Questionnaire-Short Form
- CRP:
-
C-reactive protein
- CRP-hs:
-
High-sensitive C-reactive protein
- CUS:
-
Chronic unpredictable stress
- CUMS:
-
Chronic unpredictable mild stress
- DLPFC:
-
Dorsolateral prefrontal cortex
- ECT:
-
Electroconvulsive therapy
- ELISA:
-
Enzyme-linked immunoassay
- FDA:
-
U.S. Food and Drug Administration
- GeDS:
-
Geriatric Depression Scale
- HAM-D:
-
Hamilton Depression Rating Scale
- HAM-D-7:
-
Hamilton Depression Rating Scale 7 items
- HAM-D-17:
-
Hamilton Depression Rating Scale 17 items
- HAM-D-21:
-
Hamilton Depression Rating Scale 21 items
- HAM-D-24:
-
Hamilton Depression Rating Scale 24 items
- Hz:
-
Hertz
- HPLC-MS:
-
High-performance liquid chromatography-mass spectrometry
- IFN-γ:
-
Interferon gamma
- IL-1:
-
Interleukin 1
- IL-1β:
-
Interleukin 1 beta
- IL-2:
-
Interleukin 2
- IL-4:
-
Interleukin 4
- IL-5:
-
Interleukin 5
- IL-6:
-
Interleukin 6
- IL-12p40:
-
Interleukin 12 subunit beta
- IL-18:
-
Interleukin 18
- iNOS:
-
Inducible nitric oxide synthase
- IP-10:
-
Interferon-gamma induced protein 10 kD
- iTBS:
-
Intermittent theta burst stimulation
- ITIH4:
-
Inter-alpha-trypsin inhibitor heavy chain H4
- KYN/TRP:
-
Kynurenine-to-tryptophan ratio
- LES:
-
Life Event Scale
- MADRS:
-
Montgomery–Åsberg Depression Rating Scale
- MDD:
-
Major depressive disorder
- mRNA:
-
Messenger RNA
- miRNA:
-
MicroRNA
- NaSSA:
-
Noradrenergic and specific serotonergic antidepressant
- NF-κB:
-
Nuclear factor kappa-light-chain-enhancer of activated B cells
- NHLBI:
-
National Heart, Lung, and Blood Institute
- NLRP3:
-
NLR family pyrin domain containing 3
- Nrf2:
-
Nuclear Factor-E2-related Factor 2
- OCD:
-
Obsessive-compulsive disorder
- OxPc:
-
Oxidized phosphatidylcholines
- PANSS:
-
Positive and Negative Syndrome Scale
- PETIA:
-
Particle-enhanced turbidimetric immunoassay
- PFC:
-
Prefrontal cortex
- PHQ-9:
-
Patient Health Questionnaire 9 items
- PONPC:
-
1-palmitoyl-2-(9-oxo-nonanoyl)-sn-glycero-3-phosphocholine
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PTSD:
-
Post-traumatic stress disorder
- RCT:
-
Randomized controlled trial
- RNA:
-
Ribonucleic acid
- rTMS:
-
Repetitive transcranial magnetic stimulation
- RT-qPCR:
-
Reverse transcription quantitative PCR
- SAA:
-
Serum amyloid A
- SAS:
-
Self-rating anxiety scale
- SCSR:
-
Self-Consciousness Scale Revisited
- SDS:
-
Self-rating depression scale
- SNRI:
-
Serotonergic-noradrenergic reuptake inhibitor
- SSRI:
-
Selective serotonergic reuptake inhibitor
- sTREM2:
-
Soluble Triggering receptor expressed on myeloid cells-2
- SYRCLE:
-
Systematic Review Center for Laboratory Animal Experimentation
- TBS:
-
Theta burst stimulation
- TGF-β:
-
Transforming growth factor beta
- TLR4:
-
Toll-like receptor 4
- TMS:
-
Transcranial magnetic stimulation
- TNF-α:
-
Tumor necrosis factor-alpha
- TRD:
-
Treatment-resistant depression
- TRS:
-
Treatment-resistant schizophrenia
- U.S.:
-
United States of America
- VDB:
-
Vitamin D binding protein
- VEGF:
-
Vascular Endothelial Growth Factor
- WCST:
-
Wisconsin Card Sorting Test
- WBC:
-
White blood cells
- WFT:
-
Word Fluency Test
References
Klomjai W, Katz R, Lackmy-Vallée A. Basic principles of transcranial magnetic stimulation (TMS) and repetitive TMS (rTMS). Ann Phys Rehabil Med. 2015;58(4):208–13.
Fitzgerald PB. An update on the clinical use of repetitive transcranial magnetic stimulation in the treatment of depression. J Affect Disord. 2020;276:90–103.
León Ruiz M, Rodríguez Sarasa ML, Sanjuán Rodríguez L, Benito-León J, García-Albea Ristol E, Arce Arce S. Current evidence on transcranial magnetic stimulation and its potential usefulness in post-stroke neurorehabilitation: opening new doors to the treatment of cerebrovascular disease. Neurologia (Engl Ed). 2018;33(7):459–72.
Hyde J, Carr H, Kelley N, Seneviratne R, Reed C, Parlatini V, et al. Efficacy of neurostimulation across mental disorders: systematic review and meta-analysis of 208 randomized controlled trials. Mol Psychiatry. 2022;27(6):2709–19.
Brooks M, Medscape. 2018 [cited 2023 Dec 29]. FDA clears 3-minute brain stimulation protocol for depression. https://www.medscape.com/viewarticle/901052
Mendlowitz AB, Shanbour A, Downar J, Vila-Rodriguez F, Daskalakis ZJ, Isaranuwatchai W, et al. Implementation of intermittent theta burst stimulation compared to conventional repetitive transcranial magnetic stimulation in patients with treatment resistant depression: a cost analysis. PLoS ONE. 2019;14(9):e0222546.
Lefaucheur JP, André-Obadia N, Antal A, Ayache SS, Baeken C, Benninger DH, et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS). Clin Neurophysiol. 2014;125(11):2150–206.
Blumberger DM, Vila-Rodriguez F, Thorpe KE, Feffer K, Noda Y, Giacobbe P, et al. Effectiveness of theta burst versus high-frequency repetitive transcranial magnetic stimulation in patients with depression (THREE-D): a randomised non-inferiority trial. Lancet. 2018;391(10131):1683–92.
Tseng PT, Zeng BS, Hung CM, Liang CS, Stubbs B, Carvalho AF, et al. Assessment of Noninvasive Brain Stimulation interventions for negative symptoms of Schizophrenia: a systematic review and network Meta-analysis. JAMA Psychiatry. 2022;79(8):770–9.
Hansbauer M, Wagner E, Strube W, Röh A, Padberg F, Keeser D, et al. rTMS and tDCS for the treatment of catatonia: a systematic review. Schizophr Res. 2020;222:73–8.
Guttesen LL, Albert N, Nordentoft M, Hjorthøj C. Repetitive transcranial magnetic stimulation and transcranial direct current stimulation for auditory hallucinations in schizophrenia: systematic review and meta-analysis. J Psychiatr Res. 2021;143:163–75.
Kricheldorff J, Göke K, Kiebs M, Kasten FH, Herrmann CS, Witt K, et al. Evidence of neuroplastic changes after transcranial magnetic, electric, and deep brain stimulation. Brain Sci. 2022;12(7):929.
Pedraz-Petrozzi B, Elyamany O, Rummel C, Mulert C. Effects of inflammation on the kynurenine pathway in schizophrenia — a systematic review. J Neuroinflammation. 2020;17(1):56.
Miller AH, Raison CL. The role of inflammation in depression: from evolutionary imperative to modern treatment target. Nat Rev Immunol. 2016;16(1):22–34.
Berk M, Williams LJ, Jacka FN, O’Neil A, Pasco JA, Moylan S, et al. So depression is an inflammatory disease, but where does the inflammation come from? BMC Med. 2013;11:200.
Strawbridge R, Arnone D, Danese A, Papadopoulos A, Herane Vives A, Cleare AJ. Inflammation and clinical response to treatment in depression: a meta-analysis. Eur Neuropsychopharmacol. 2015;25(10):1532–43.
Calabrese F, Rossetti AC, Racagni G, Gass P, Riva MA, Molteni R. Brain-derived neurotrophic factor: a bridge between inflammation and neuroplasticity. Front Cell Neuroscience [Internet]. 2014 [cited 2023 Dec 29];8. https://www.frontiersin.org/articles/https://doi.org/10.3389/fncel.2014.00430
Hritcu L, Gorgan LD. Intranigral lipopolysaccharide induced anxiety and depression by altered BDNF mRNA expression in rat hippocampus. Prog Neuropsychopharmacol Biol Psychiatry. 2014;51:126–32.
Leal G, Comprido D, Duarte CB. BDNF-induced local protein synthesis and synaptic plasticity. Neuropharmacology. 2014;76:639–56. Pt C.
Jannati A, Oberman LM, Rotenberg A, Pascual-Leone A. Assessing the mechanisms of brain plasticity by transcranial magnetic stimulation. Neuropsychopharmacology. 2023;48(1):191–208.
Luo J, Feng Y, Li M, Yin M, Qin F, Hu X. Repetitive transcranial magnetic stimulation improves neurological function and promotes the anti-inflammatory polarization of Microglia in ischemic rats. Front Cell Neurosci. 2022;16:878345.
Heath A, Lindberg DR, Makowiecki K, Gray A, Asp AJ, Rodger J, et al. Medium- and high-intensity rTMS reduces psychomotor agitation with distinct neurobiologic mechanisms. Transl Psychiatry. 2018;8(1):1–13.
Lefaucheur JP, Aleman A, Baeken C, Benninger DH, Brunelin J, Di Lazzaro V, et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS): an update (2014–2018). Clin Neurophysiol. 2020;131(2):474–528.
Tikka SK, Siddiqui MA, Garg S, Pattojoshi A, Gautam M. Clinical practice guidelines for the therapeutic use of Repetitive Transcranial Magnetic Stimulation in Neuropsychiatric disorders. Indian J Psychiatry. 2023;65(2):270–88.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210.
National Institute of Health. Study Quality Assessment Tools | NHLBI [Internet]. 2021 [cited 2023 Dec 30]. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
Hooijmans CR, Rovers MM, de Vries RB, Leenaars M, Ritskes-Hoitinga M, Langendam MW. SYRCLE’s risk of bias tool for animal studies. BMC Med Res Methodol. 2014;14(1):43.
Stekic A, Zeljkovic M, Zaric Kontic M, Mihajlovic K, Adzic M, Stevanovic I, et al. Intermittent Theta Burst Stimulation ameliorates cognitive deficit and attenuates neuroinflammation via PI3K/Akt/mTOR signaling pathway in alzheimer’s-like disease model. Front Aging Neurosci. 2022;14:889983.
Zuo C, Cao H, Feng F, Li G, Huang Y, Zhu L, et al. Repetitive transcranial magnetic stimulation exerts anti-inflammatory effects via modulating glial activation in mice with chronic unpredictable mild stress-induced depression. Int Immunopharmacol. 2022;109:108788.
Tian L, Sun SS, Cui LB, Wang SQ, Peng ZW, Tan QR, et al. Repetitive transcranial magnetic stimulation elicits antidepressant- and anxiolytic-like Effect via Nuclear Factor-E2-related factor 2-mediated anti-inflammation mechanism in rats. Neuroscience. 2020;429:119–33.
Yilmaz NS, Sen B, Karadag RF, Aslan S, Ekmekci Ertek I, Bozkurt A, et al. A kynurenine pathway enzyme aminocarboxymuconate-semialdehyde decarboxylase may be involved in treatment-resistant depression, and baseline inflammation status of patients predicts treatment response: a pilot study. J Neural Transm (Vienna). 2022;129(12):1513–26.
Stirton H, Meek BP, Edel AL, Solati Z, Surendran A, Aukema H et al. Oxolipidomics profile in major depressive disorder: Comparing remitters and non-remitters to repetitive transcranial magnetic stimulation treatment. Li Z, editor. PLoS ONE. 2021;16(2):e0246592.
Tateishi H, Matsushima J, Kunitake H, Imamura Y, Kunitake Y, Murakawa T, et al. Serum soluble triggering receptor expressed on myeloid cells-2 was not altered by rTMS in patients with treatment‐resistant depression. Neuropsychopharm Rep. 2023;43(2):222–7.
Tateishi H, Mizoguchi Y, Kawaguchi A, Imamura Y, Matsushima J, Kunitake H, et al. Changes in interleukin-1 beta induced by rTMS are significantly correlated with partial improvement of cognitive dysfunction in treatment-resistant depression: a pilot study. Psychiatry Res. 2020;289:112995.
Valiuliene G, Valiulis V, Dapsys K, Vitkeviciene A, Gerulskis G, Navakauskiene R et al. G Thut editor 2021 Brain stimulation effects on serum BDNF, VEGF, and TNFα in treatment-resistant psychiatric disorders. Eur J Neurosci 53 11 3791–802.
Valiuliene G, Valiulis V, Zentelyte A, Dapsys K, Germanavicius A, Navakauskiene R. Anti-neuroinflammatory microRNA-146a-5p as a potential biomarker for neuronavigation-guided rTMS therapy success in medication resistant depression disorder. Biomed Pharmacother. 2023;166:115313.
Xu Y, Han L, Wei Y, Mao H, Yu Z. Combined repetitive transcranial magnetic stimulation and medication treatment for depression is associated with serum amyloid a level: evidence from naturalistic clinical practice. Front Neurosci. 2022;16:1002816.
Cha B, Kim J, Kim JM, Choi JW, Choi J, Kim K, et al. Therapeutic effect of Repetitive Transcranial Magnetic Stimulation for post-stroke vascular cognitive impairment: a prospective pilot study. Front Neurol. 2022;13:813597.
Zhao X, Li Y, Tian Q, Zhu B, Zhao Z. Repetitive transcranial magnetic stimulation increases serum brain-derived neurotrophic factor and decreases interleukin-1β and tumor necrosis factor-α in elderly patients with refractory depression. J Int Med Res. 2019;47(5):1848–55.
Wang Q, Zeng L, Hong W, Luo M, Zhao N, Hu X, et al. Inflammatory cytokines changed in patients with Depression before and after repetitive transcranial magnetic stimulation treatment. Front Psychiatry. 2022;13:925007.
Chou PH, Lu MK, Tsai CH, Hsieh WT, Lai HC, Shityakov S et al. Antidepressant efficacy and immune effects of bilateral theta burst stimulation monotherapy in major depression: A randomized, double-blind, sham-controlled study. Brain, Behavior, and Immunity. 2020;88:144–50.
Song R, Shi Y, Li X, Zhu J, Zhang H, Li K, et al. Potential of Antithrombin III as a biomarker of Antidepressive Effect in Major Depressive Disorder. Front Psychiatry. 2021;12:678384.
Leblhuber F, Steiner K, Fuchs D. Treatment of patients with geriatric depression with repetitive transcranial magnetic stimulation. J Neural Transm. 2019;126(8):1105–10.
Leblhuber F, Geisler S, Ehrlich D, Steiner K, Reibnegger G, Fuchs D, et al. Repetitive transcranial magnetic stimulation in the treatment of resistant depression: changes of specific neurotransmitter precursor amino acids. J Neural Transm. 2021;128(8):1225–31.
Su X, Zhao L, Shang Y, Chen Y, Liu X, Wang X, et al. Repetitive transcranial magnetic stimulation for psychiatric symptoms in long-term hospitalized veterans with schizophrenia: a randomized double-blind controlled trial. Front Psychiatry. 2022;13:873057.
Haroon E, Welle JR, Woolwine BJ, Goldsmith DR, Baer W, Patel T, et al. Associations among peripheral and central kynurenine pathway metabolites and inflammation in depression. Neuropsychopharmacol. 2020;45(6):998–1007.
Solati Z, Ravandi A. Lipidomics of bioactive lipids in Acute Coronary syndromes. Int J Mol Sci. 2019;20(5):1051.
Bianchi VE. The anti-inflammatory effects of testosterone. J Endocr Soc. 2018;3(1):91–107.
Reinders MEJ, Sho M, Izawa A, Wang P, Mukhopadhyay D, Koss KE, et al. Proinflammatory functions of vascular endothelial growth factor in alloimmunity. J Clin Invest. 2003;112(11):1655–65.
Eklund KK, Niemi K, Kovanen PT. Immune functions of serum amyloid A. Crit Rev Immunol. 2012;32(4):335–48.
Timäus C, Vogelgsang J, Kis B, Radenbach K, Wolff-Menzler C, Mavridou K, et al. Current clinical practice of electroconvulsive therapy and repetitive transcranial magnetic stimulation in psychiatry, a German sample. Eur Arch Psychiatry Clin Neurosci. 2021;271(1):181–90.
Milev RV, Giacobbe P, Kennedy SH, Blumberger DM, Daskalakis ZJ, Downar J, et al. Canadian Network for Mood and anxiety treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder. Can J Psychiatry. 2016;61(9):561–75.
McClintock SM, Reti IM, Carpenter LL, McDonald WM, Dubin M, Taylor SF, et al. Consensus recommendations for the clinical application of repetitive transcranial magnetic stimulation (rTMS) in the treatment of depression. J Clin Psychiatry. 2018;79(1):16cs10905.
Vida RG, Sághy E, Bella R, Kovács S, Erdősi D, Józwiak-Hagymásy J, et al. Efficacy of repetitive transcranial magnetic stimulation (rTMS) adjunctive therapy for major depressive disorder (MDD) after two antidepressant treatment failures: meta-analysis of randomized sham-controlled trials. BMC Psychiatry. 2023;23(1):545.
Somani A, Kar SK. Efficacy of repetitive transcranial magnetic stimulation in treatment-resistant depression: the evidence thus far. Gen Psychiatr. 2019;32(4):e100074.
Chail A, Saini RK, Bhat PS, Srivastava K, Chauhan V. Transcranial magnetic stimulation: a review of its evolution and current applications. Ind Psychiatry J. 2018;27(2):172–80.
Rostami R, Kazemi R, Jabbari A, Madani AS, Rostami H, Taherpour MA, et al. Efficacy and clinical predictors of response to rTMS treatment in pharmacoresistant obsessive-compulsive disorder (OCD): a retrospective study. BMC Psychiatry. 2020;20(1):372.
Hett D, Marwaha S. Repetitive transcranial magnetic stimulation in the treatment of bipolar disorder. Therapeutic Adv Psychopharmacol. 2020;10:2045125320973790.
Kan RLD, Zhang BBB, Zhang JJQ, Kranz GS. Non-invasive brain stimulation for posttraumatic stress disorder: a systematic review and meta-analysis. Transl Psychiatry. 2020;10(1):1–12.
He LW, Zeng L, Tian N, Li Y, He T, Tan DM, et al. Optimization of food deprivation and sucrose preference test in SD rat model undergoing chronic unpredictable mild stress. Anim Models Experimental Med. 2020;3(1):69–78.
De Risio L, Borgi M, Pettorruso M, Miuli A, Ottomana AM, Sociali A, et al. Recovering from depression with repetitive transcranial magnetic stimulation (rTMS): a systematic review and meta-analysis of preclinical studies. Transl Psychiatry. 2020;10(1):1–19.
Willner P. The chronic mild stress (CMS) model of depression: history, evaluation and usage. Neurobiol Stress. 2016;6:78–93.
Perrin AJ, Pariante CM. Endocrine and immune effects of non-convulsive neurostimulation in depression: a systematic review. Brain Behav Immun. 2020;87:910–20.
Rajkumar RP. Immune-inflammatory markers of response to repetitive transcranial magnetic stimulation in depression: a scoping review. Asian J Psychiatr. 2023;91:103852.
Berlim MT, Van den Eynde F, Daskalakis ZJ. Efficacy and acceptability of high frequency repetitive transcranial magnetic stimulation (rTMS) versus electroconvulsive therapy (ECT) for major depression: a systematic review and meta-analysis of randomized trials. Depress Anxiety. 2013;30(7):614–23.
Micallef-Trigona B. Comparing the effects of repetitive transcranial magnetic stimulation and electroconvulsive therapy in the treatment of depression: a systematic review and meta-analysis. Depress Res Treat. 2014;2014:135049.
Järventausta K, Sorri A, Kampman O, Björkqvist M, Tuohimaa K, Hämäläinen M, et al. Changes in interleukin-6 levels during electroconvulsive therapy may reflect the therapeutic response in major depression. Acta Psychiatr Scand. 2017;135(1):87–92.
Isaković J, Gorup D, Mitrečić D. Molecular mechanisms of microglia- and astrocyte-driven neurorestoration triggered by application of electromagnetic fields. Croat Med J. 2019;60(2):127–40.
Eichler A, Kleidonas D, Turi Z, Fliegauf M, Kirsch M, Pfeifer D et al. Microglial cytokines mediate plasticity induced by 10 Hz repetitive magnetic stimulation. J Neurosci Off J Soc Neurosci [Internet]. 2023; https://search.ebscohost.com/login.aspx?direct=true%26db=mdc%26AN=36977586%E8;=es%26site=ehost-live
Tasset I, Pérez-Herrera A, Medina FJ, Arias-Carrión Ó, Drucker-Colín R, Túnez I. Extremely low-frequency electromagnetic fields activate the antioxidant pathway Nrf2 in a Huntington’s disease-like rat model. Brain Stimul. 2013;6(1):84–6.
Hong Y, Liu Q, Peng M, Bai M, Li J, Sun R, et al. High-frequency repetitive transcranial magnetic stimulation improves functional recovery by inhibiting neurotoxic polarization of astrocytes in ischemic rats. J Neuroinflamm. 2020;17(1):150.
Hannestad J, DellaGioia N, Bloch M. The effect of antidepressant medication treatment on serum levels of inflammatory cytokines: a meta-analysis. Neuropsychopharmacology. 2011;36(12):2452–9.
Liu JJ, Wei YB, Strawbridge R, Bao Y, Chang S, Shi L, et al. Peripheral cytokine levels and response to antidepressant treatment in depression: a systematic review and meta-analysis. Mol Psychiatry. 2020;25(2):339–50.
Strawbridge R, Izurieta E, Day E, Tee H, Young K, Tong CC, et al. Peripheral inflammatory effects of different interventions for treatment-resistant depression: a systematic review. Neurosci Appl. 2023;2:101014.
Rotter A, Biermann T, Stark C, Decker A, Demling J, Zimmermann R, et al. Changes of cytokine profiles during electroconvulsive therapy in patients with major depression. J ECT. 2013;29(3):162–9.
Kartalci S, Karabulut AB, Erbay LG, Acar C. Effects of electroconvulsive Therapy on some inflammatory factors in patients with treatment-resistant schizophrenia. J ECT. 2016;32(3):174.
Zincir S, Öztürk P, Bilgen AE, İzci F, Yükselir C. Levels of serum immunomodulators and alterations with electroconvulsive therapy in treatment-resistant major depression. Neuropsychiatr Dis Treat. 2016;12:1389–96.
Kruse JL, Congdon E, Olmstead R, Njau S, Breen EC, Narr KL, et al. Inflammation and improvement of Depression following electroconvulsive therapy in treatment-resistant depression. J Clin Psychiatry. 2018;79(2):9042.
Rezaie AR, Giri H. Anticoagulant and signaling functions of antithrombin. J Thromb Haemost. 2020;18(12):3142–53.
Wiedermann CJ, Römisch J. The anti-inflammatory actions of antithrombin–a review. Acta Med Austriaca. 2002;29(3):89–92.
Shi Y, Song R, Wang L, Qi Y, Zhang H, Zhu J, et al. Identifying plasma biomarkers with high specificity for major depressive disorder: a multi-level proteomics study. J Affect Disord. 2020;277:620–30.
Geiser F, Conrad R, Imbierowicz K, Meier C, Liedtke R, Klingmüller D, et al. Coagulation activation and fibrinolysis impairment are reduced in patients with anxiety and depression when medicated with serotonergic antidepressants. J Neuropsychiatry Clin Neurosci. 2011;65(5):518–25.
Stelzhammer V, Guest PC, Rothermundt M, Sondermann C, Michael N, Schwarz E, et al. Electroconvulsive therapy exerts mainly acute molecular changes in serum of major depressive disorder patients. Eur Neuropsychopharmacol. 2013;23(10):1199–207.
Bourgognon JM, Cavanagh J. The role of cytokines in modulating learning and memory and brain plasticity. Brain Neurosci Adv. 2020;4:2398212820979802.
Weaver JD, Huang MH, Albert M, Harris T, Rowe JW, Seeman TE. Interleukin-6 and risk of cognitive decline. Neurology. 2002;59(3):371–8.
Gimeno D, Kivimäki M, Brunner EJ, Elovainio M, De Vogli R, Steptoe A, et al. Associations of C-reactive protein and interleukin-6 with cognitive symptoms of depression: 12-year follow-up of the Whitehall II study. Psychol Med. 2009;39(3):413–23.
Jin K, Lu J, Yu Z, Shen Z, Li H, Mou T, et al. Linking peripheral IL-6, IL-1β and hypocretin-1 with cognitive impairment from major depression. J Affect Disord. 2020;277:204–11.
Huang ZB, Sheng GQ. Interleukin-1β with learning and memory. Neurosci Bull. 2010;26(6):455–68.
Clausen F, Hånell A, Björk M, Hillered L, Mir AK, Gram H, et al. Neutralization of interleukin-1β modifies the inflammatory response and improves histological and cognitive outcome following traumatic brain injury in mice. Eur J Neurosci. 2009;30(3):385–96.
Jiang S, Shi D, Bai L, Niu T, Kang R, Liu Y. Inhibition of interleukin-6 trans-signaling improves survival and prevents cognitive impairment in a mouse model of sepsis. Int Immunopharmacol. 2023;119:110169.
Acknowledgements
Not applicable.
Funding
No funding for this research was done.
Author information
Authors and Affiliations
Contributions
BPP: idea, conceptualization, data curation, data collection formal analysis, writing - original draft, visualization. BPP shares the first authorship with SI. SI: idea, conceptualization, data curation, data collection, formal analysis, writing - original draft, visualization. SI shares the first authorship with BPP. MS: data curation, data collection, formal analysis, resources, writing – review and editing. JR: data curation, data collection, formal analysis, resources, writing – review and editing. EKL: data curation, data collection, formal analysis, resources, writing – review and editing. MG: data curation, writing - review and editing. MD: data curation, writing - review and editing. AS: conceptualization, writing – review and editing, supervision.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Pedraz-Petrozzi, B., Insan, S., Spangemacher, M. et al. Association between rTMS-induced changes in inflammatory markers and improvement in psychiatric diseases: a systematic review. Ann Gen Psychiatry 23, 31 (2024). https://doi.org/10.1186/s12991-024-00514-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12991-024-00514-0