Abstract
Background
Telemedicine represents an important strategy to facilitate access to medication abortion (MAB) procedures, reduces distance barriers and expands coverage to underserved communities. The aim is evaluating the self-managed MAB (provided through telemedicine as the sole intervention or in comparison to in-person care) in pregnant people at up to 12 weeks of pregnancy.
Methods
A literature search was conducted using electronic databases: MEDLINE, Embase, Cochrane (Central Register of Controlled Trials and Database of Systematic Reviews), LILACS, SciELO, and Google Scholar. The search was based on the Population, Intervention, Comparison, Outcome, and Study Design (PICOS) framework, and was not restricted to any years of publication, and studies could be published in English or Spanish. Study screening and selection, risk of bias assessment, and data extraction were performed by peer reviewers. Risk of bias was evaluated with RoB 2.0 and ROBIS-I. A narrative and descriptive synthesis of the results was conducted. Meta-analyses with random-effects models were performed using Review Manager version 5.4 to calculate pooled risk differences, along with their individual 95% confidence intervals. The rate of evidence certainty was based on GRADE recommendations.
Results
21 articles published between 2011 and 2022 met the inclusion criteria. Among them, 20 were observational studies, and 1 was a randomized clinical trial. Regarding the risk of bias, 5 studies had a serious risk, 15 had a moderate risk, and 1 had an undetermined risk. In terms of the type of intervention, 7 compared telemedicine to standard care. The meta-analysis of effectiveness revealed no statistically significant differences between the two modalities of care (RD = 0.01; 95%CI 0.00, 0.02). Our meta-analyses show that there were no significant differences in the occurrence of adverse events or in patient satisfaction when comparing the two methods of healthcare delivery.
Conclusion
Telemedicine is an effective and viable alternative for MAB, similar to standard care. The occurrence of complications was low in both forms of healthcare delivery. Telemedicine services are an opportunity to expand access to safe abortion services.
Plain English summary
Globally, unsafe abortion causes 47,000 deaths and 5 million sexual and reproductive dysfunctions in young pregnant people due to complications of the procedure. This practice is related to barriers to accessing safe abortion services secondary to health system limitations and inequities in the distribution of resources.
Telemedicine has proven to be an efficient care alternative to reduce distancing gaps, decrease waiting time and rationalize the costs derived from the procedure. Consequently, several health systems in the world use this model with differences in treatment schemes, weeks of gestation, pregnancy confirmation methods and measurement of reported outcomes. For this reason, evaluating the effectiveness and safety of self-managed medication abortion (MAB) by telemedicine is a support for decision makers who consider implementing or expanding remote care services.
This systematic review integrated studies that evaluated MAB only by Telemedicine or in comparison with standard care on pregnant people with 12 weeks gestation or less. Available studies until January 2023 were chosen. Screening and selection of studies, data extraction, and risk of bias assessment were performed by expert reviewers. Aspects such as the effectiveness, safety, and satisfaction of the procedure, among other outcomes, were reviewed. A narrative and descriptive synthesis was carried out, as well as several meta-analyses of the differences in risks between Telemedicine and in-person care.
The meta-analysis of studies comparing telemedicine care with standard services reveals that the type of care provided does not affect the effectiveness and safety of MAB, nor does it affect user satisfaction, follow-up, or medication adherence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Unsafe abortion poses significant challenges to pregnant people’s health, public health, and the overall well-being of nations. Each year, approximately 47 000 pregnant people die and nearly 5 million experience sequelae or sexual and reproductive dysfunctions due to complications associated with this procedure [1, 2]. Unsafe abortion predominantly occurs among pregnant people aged 20 to 25 or those in vulnerable situations, such as migrants and those living in poverty, belonging to specific ethnic groups, or with low levels of education [3]. According to estimates, 90% of unsafe abortions occur in low- and middle-income countries, particularly in Africa, Southeast Asia, Latin America, and the Caribbean, where there is a higher burden of morbidity, mortality, and increased healthcare costs due to procedure-related complications [3, 4].
The political and legal landscape surrounding abortion plays a pivotal role in this regard, as, in countries with more favorable laws and well-funded healthcare systems, pregnant people have better access to safe abortion procedures. Conversely, in nations where abortion is either prohibited or restricted to specific circumstances, pregnant people seeking to terminate their pregnancies are compelled to undergo procedures performed by unqualified individuals or in unsanitary environments. This significantly heightens the risk of complications and fatal outcomes [1, 5].
To provide high-quality abortion services, it is crucial to establish a comprehensive political, legal, and healthcare framework that safeguards pregnant people’s rights and considers their specific needs and social, economic, and cultural contexts [6, 7]. As a result, most countries have decriminalized abortion either entirely or under specific circumstances and have adapted their institutional guidelines to provide care to pregnant people seeking voluntary termination of pregnancy. However, universal access to sexual and reproductive health services remains a distant goal given the limitations within the healthcare system and social inequities, which turn a right into a privilege mostly accessible to pregnant people residing in urban areas with sufficient financial resources to afford such services [2, 4, 8, 9].
Safe abortion refers to the induced termination of pregnancy by healthcare professionals or qualified individuals using methods recommended by the World Health Organization (WHO), which are selected based on weeks’ gestation [2]. For instance, a medication abortion (MAB) considered a safe option for pregnancies up to twelve weeks, involves orally administering a single 200-mg dose of mifepristone, followed by the use of misoprostol 24–48 h later. In some cases, additional doses of misoprostol are taken every 3–4 h. The concentrations and administration routes of misoprostol may vary depending on gestational weeks and user preference [1]. This treatment can be provided by healthcare professionals or, if users have received sufficient information and counseling, it can be self-managed at home [10]. Consequently, the outpatient option somewhat liberates users from the structural limitations of healthcare services [11] and opens up possibilities for innovative care alternatives such as the use of Information and Communication Technologies (ICTs), including telemedicine services [11, 12].
As part of the broader concept of digital health or e-health, telemedicine is defined by the WHO as ““the practice of healthcare using interactive audio, visual, and data communications. This includes healthcare delivery, consultation, diagnosis, and treatment, as well as education and transfer of medical data”” [13]. This form of healthcare delivery has seen significant growth over the past 20 years, due to advancements in mobile technologies and the widespread availability of digital media, especially the internet [13,14,15]. Furthermore, the COVID-19 pandemic and the declaration of a public health emergency by the WHO in January 2020 led to a shift in healthcare delivery models due to mobility restrictions and lockdown measures. In response to these new and adverse public health conditions, remote care services were massively implemented worldwide, demonstrating their effectiveness in reducing geographical barriers, improving the quality and timeliness of care, optimizing costs for both patients and healthcare systems, and reducing healthcare disparities [11, 16,17,18,19,20,21].
One particular application of remote care is the provision of healthcare services during a MAB. Currently, several studies have shown that self-managed and telemedicine-guided MAB is a comparable alternative to in-person care in terms of effectiveness, safety, and patient satisfaction [10, 18, 20,21,22,23,24,25,26,27,28,29,30,31,32,33,34]. It also reduces the time required to access care and brings healthcare services to remote or underserved communities [35]. Yet, in order to promote the integration and appropriate use of these technologies, ongoing evaluation is necessary alongside the implementation and strengthening of these services [15, 16].
In most countries, the use of scientific evidence serves as the basis for prescribing interventions in healthcare services. Therefore, providing data on the effectiveness and safety of MAB provided through telemedicine is crucial for decision-makers to justify its implementation and widespread adoption. Moreover, given variations in treatment protocols, gestational weeks, methods of pregnancy confirmation, and outcome measurements reported in studies assessing MAB provided via telemedicine, it is important to consolidate the information through a Systematic Literature Review (SLR). Hence, the purpose of this study is to evaluate the effectiveness, safety, satisfaction, and acceptability of self-managed and telemedicine-guided MAB, either as the sole intervention or in comparison to standard or in-person care.
Materials and methods
For this SLR, we used Cochrane methods [36] and the PRISMA 2020 guidelines [37] as the reporting standard. The SLR protocol employed in this study can be accessed on PROSPERO (CRD42023416407).
Eligibility criteria
This SLR included studies that evaluated MAB provided through telemedicine as the sole intervention or in comparison with standard or in-person care. The research question was defined using the Population, Intervention, Comparison, Outcome, and Study Design (PICOS) framework [36].
Population
Pregnant people of childbearing age (aged 10–50 years) who used telemedicine services for MAB before or during the twelfth week of pregnancy, without restriction to any specific country or region.
Intervention
Telemedicine as a comprehensive model for self-managed MAB care. This involved the provision of healthcare services (in this case, MAB) through remote communication technologies.
Comparison
MAB through standard or in-person care.
Outcome
The primary outcomes assessed in this study were effectiveness of the procedure (successful completion of MAB without the need for additional medications and/or surgical intervention), safety (adverse effects/complications: death, surgical intervention, blood transfusion, hospitalization, antibiotic treatment, and emergency department visits), and user acceptability or satisfaction with the service. Other outcomes included follow-up (completion of all phases of MAB), user feelings regarding the procedure, emotional support provided to users, waiting time to treatment (in days), and adherence to prescribed regimens (compliance with correct dosage, administration route, and recommended intake times).
Study design
Experimental studies (Randomized Controlled Trials -RCTs-) and observational studies (cohort studies, case–control studies, and cross-sectional studies). To be eligible, studies had to be available as full publications, and pre-print publications were also considered. Publications in English or Spanish were accepted, and there were no restrictions on the publication date. Excluded publications included abstracts, narrative reviews, expert consensus, study protocols, case studies or case series, comments, and letters to the editor.
Sources of information
A literature search was conducted in January 2023 using the following electronic databases: MEDLINE (via PubMed), Embase (via Elsevier), Cochrane Library (including the Cochrane Database of Systematic Reviews and the Cochrane Central Register of Controlled Trials), LILACS (via the Virtual Health Library), and SciELO. Additionally, Google Scholar was consulted as a source of gray literature, with the first ten pages of results being examined. To identify additional relevant research, the snowball search method was employed, checking the references of the included studies.
The search strategy was designed by two of the authors (KCG and LCES) and subsequently reviewed by the main author (JLCA). For the searches, key terms were chosen from the list of Medical Subject Headings (MeSH) and Health Sciences Descriptors (DeCS), and free terms based on opinions from subject-matter experts were used as well. The search strategies were tailored to each specific database, incorporating field identifiers, truncation, proximity operators, and Boolean operators as appropriate. Detailed information on the search terms and search strategies used for each database can be found in Appendix A.
Study selection
The study selection process consisted of two stages. In the first stage, the titles and abstracts of the retrieved papers were downloaded, duplicates were removed using Rayyan [38], and the papers were screened based on title and abstract. This initial screening was performed by two reviewers (KCG and LCES) in a double-blind peer review format. Disagreements were resolved through consensus, and if consensus could not be reached, a third reviewer (JLCA) was consulted.
In the second stage, the full text of the pre-selected studies was reviewed by the same two authors in a double-blind peer review format. Disagreements were resolved using the same methodology employed in the initial screening.
Data extraction
Data were extracted independently by two of the authors (KCG and LCES) using Excel®, and disagreements were resolved either between them or with the involvement of the main author (JLCA). The following details were documented: study title, first author, year of publication, country, study design, timeframe, objective, characteristics of the population (age group and diagnoses), number of participants (total and per group), intervention and comparison details (dose, frequency, duration), outcomes (measurement method and follow-up time), specific results for each outcome, and conclusion.
Risk of bias assessment
The risk of bias of the selected studies was assessed independently by two evaluators (KCG and LCES), and any disagreements were resolved through consensus between them. If disagreements persisted, a third evaluator (JLCA) was involved in the discussion.
To assess the risk of bias of the RCTs, Version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2) [36] was used, and for the observational studies, the Risk of Bias In Non-randomized Studies—of Interventions (ROBINS-I) tool [39] was employed.
Data synthesis
A narrative and descriptive synthesis was conducted for each outcome. In studies that included a comparator, similar results were grouped together. For meta-analyses, Cochrane’s Review Manager version 5.4 [40] was used to generate random-effects models and calculate pooled risk differences, along with their corresponding 95% Confidence Interval (CI) and p-values, which were then presented in a forest plot. Statistical heterogeneity was estimated using the I2 statistic, where a value greater than 75% indicates significant heterogeneity. For the effectiveness outcome, two a-posteriori subgroup analyses were carried out: the first, according to gestational week (up to weeks 9, 10 and 12); and the second, according to the test used to determine the treatment results (self-assessment, blood test, ultrasound, or a combination of these methods). A Summary of Findings (SoF) table was elaborated to summarize the main results for each outcome (patients and studies, relative and absolute effects, certainty and observations), as well as an assessment of the quality of evidence rating based on GRADE recommendations [41] (rate evidence certainty as high, moderate, low or very low) using the GRADEpro tool [42].
Results
Data search
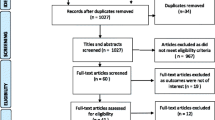
A total of 821 records were retrieved in the initial search, out of which 87 were duplicates. After reviewing the 734 remaining publications, only 21 met the eligibility criteria (Fig. 1).
Characteristics and risk of bias of the selected studies
Table 1 summarizes the characteristics of the 21 studies included in our review. Out of such studies published between 2011 and 2022, 20 were cross-sectional [18, 20, 24, 26, 28,29,30,31, 33, 34, 43,44,45,46,47,48,49,50,51,52] and 1 was an RCT [32]. Regarding their geographical distribution, 7 (33.3%) originated from.
European countries, 6 (28.6%) from the United States (US), 3 (14.3%) from Latin America, 2 (9.5%) from Australia, 2 (9.5%) were multi-country studies, and 1 (4.8%) was from South Africa. The overall risk of bias was from low to serious in the cross-sectional studies, while the RCT exhibited a high risk of bias (Fig. 2).
Furthermore, 14 (66.7%) evaluated MAB provided through telemedicine as the sole intervention, and 7 (33.3%) compared it with standard care. In terms of gestational weeks, 9 studies (42.8%) included pregnant people at up to 9 weeks of pregnancy, 7 (33.3%) at up to 10 weeks, 3 (14.3%) at up to 12 weeks, and 2 (9.5%) beyond 12 weeks. 16 studies (76.2%) reported on the effectiveness of MAB, 16 (76.2%) examined the safety of the procedure, and 9 (42.8%) addressed user acceptability or satisfaction with the service. Other outcomes assessed in the studies included follow-up (n = 4; 19%), feelings regarding the procedure (n = 3; 14.3%), and average waiting time to treatment (n = 1; 4.8%).
Effectiveness
Sixteen studies evaluated the effectiveness of MAB, with ten exclusively evaluating telemedicine patients [18, 30, 31, 33, 34, 43, 45,46,47,48], and the remaining six comparing this outcome among telemedicine patients and standard patients [20, 26, 29, 32, 50, 52]. Treatment success was primarily confirmed through blood tests, followed by ultrasound. Only one study [20] used self-assessment to confirm termination of pregnancy.
In the studies that focused on telemedicine patients, the average effectiveness was 91.9%. All studies reported a standard regimen of 200 mg of orally, vaginally, or sublingually administered mifepristone, followed by an 800 µg dose of misoprostol after 24–48 h. Moreover, additional doses of misoprostol were administered after 3–4 h: six studies [18, 30, 34, 43, 46, 47] reported doses of up to 400 µg, three studies [31, 45, 48] reported doses of up to 800 µg, and one study [33] reported doses of up to 1600 µg. According to the results, increasing additional doses resulted in higher effectiveness rates (90.2%, 93.1%, and 98% respectively).
Six studies [26, 29, 32, 50, 52, 53] were conducted to compare the effectiveness of MAB between patients receiving telemedicine compared with standard care. 77,682 pregnant individuals made up the total sample size, with 43% using the telemedicine modality and 57% using standard care. A meta-analysis of the comparative effectiveness of the studies revealed no statistically significant differences between the two modalities of care (98.6% for telemedicine vs. 97.1% for standard care; RD = 0.01; 95% CI 0.00, 0.02).
Three of them [26, 32, 52] included pregnant people at up to nine weeks of pregnancy, two [20, 29] at up to ten weeks, and one [50] at up to twelve weeks. Moreover, one study [20] reported an additional 400-µg dose of misoprostol after 3–4 h, and two studies [26, 50] reported additional doses of up to 800 µg of misoprostol after the same time interval.
A subgroup analysis according to gestational age (Fig. 3) revealed that, in pregnancies of less than 12 weeks of gestation, there were 10 more successful cases in the standard care group than in the telemedicine group for every 1,000 MAB performed (RD = 0.01; 95% CI 0.01, 0.02). No statistically significant differences were observed among the subgroups of pregnancies under 9 and 10 weeks of gestation (RD = 0.01; 95% CI -0.00, 0.03 and RD = 0.01; 95% CI 0.00, 0.01, respectively).
Assessing effectiveness based on the method used to confirm successful abortion (Fig. 4), the meta-analysis revealed a slight advantage for standard care when either a blood test alone (RD = 0.02; 95%CI 0.01, 0.02) or informed clinical opinion (RD = 0.01; 95%CI 0.01, 0.02) were used, where for 1000 abortions performed, 20 or 10 cases of successful abortion were found in favour of standard care than in telemedicine, respectively. The certainty of the evidence for this outcome was low and moderate (supplementary Table 1).
In their study, Kohn et al. [50] demonstrated a higher rate of ongoing pregnancy in standard patients compared to telemedicine patients (1.8% vs. 0.5%.; OR = 0.23; 95%CI 0.14, 0.39).
Adverse effects
Mortality
Two cross-sectional studies investigated the mortality associated with MAB provided via telemedicine [50, 52]. Both studies employed a standard dose of 200 mg of mifepristone and 800 µg of misoprostol, with variations in the additional doses of misoprostol. One of the studies did not employ any additional dose [52], whereas the other used up to an additional 800-µg dose [50]. No deaths were reported during the follow-up period.
Surgical intervention
Thirteen studies included surgical intervention as an adverse effect of MAB, with nine reporting the incidence of this event for telemedicine patients only [18, 30, 31, 34, 43, 45,46,47,48] and the other four comparing this outcome between telemedicine patients and standard patients [20, 26, 50, 52].
In the studies that focused on telemedicine patients, the average percentage of surgical interventions was 8.1%. In all these studies, additional doses of misoprostol were administered. Six studies [18, 30, 34, 43, 46, 47] used additional doses of up to 400 µg [20], and the average percentage of surgical interventions was 10.4%. The other 3 studies [31, 45, 48] reported using additional doses of up to 800 µg, and the average percentage of surgical interventions was 3.6%.
In the four studies that compared the percentage of surgical interventions between telemedicine patients and standard patients, the treatment regimens varied in terms of the additional doses of misoprostol. One study did not employ any additional dose [52], another used a 400-µg dose [20], and two studies reported using 800 µg of misoprostol [26, 50]. Regarding gestational weeks, two studies included pregnant people up to nine weeks [20, 26], one up to ten weeks [52], and one up to twelve weeks [50]. The combined effect analysis did not reveal any differences between the two forms of healthcare delivery (RD = 0.00; 95%CI—0.00, 0.00; n = 78, 098; I2 = 94%) (Fig. 5). In the subgroup meta-analyses (based on gestational weeks), no differences were found in the occurrence of surgical interventions following MAB. The certainty of the evidence was very low (supplementary Table 1).
Blood transfusion
Eight studies examined the occurrence of blood transfusion events following MAB, with four exclusively focusing on telemedicine patients [18, 34, 43, 45] and the other four comparing this outcome among telemedicine patients and standard patients [26, 28, 32, 50]. Considering telemedicine patients alone, the incidence of this adverse effect was found to be approximately 0.5%.
Among the four studies that compared the occurrence of blood transfusion events between telemedicine patients and standard patients, one study used the standard dose of mifepristone and an initial dose of 800 µg of misoprostol without any additional doses [32], while the other three studies employed an additional dose of 800 µg of misoprostol [26, 28, 50]. Three of the studies included pregnant people up to nine weeks [26, 28, 32], and one up to twelve weeks [50]. The combined effect analysis did not reveal any significant differences between the telemedicine and standard groups (RD = 0.00; 95%CI -0.00, 0.00; n = 26,307; I2 = 0%). In the subgroup meta-analyses (based on gestational weeks), no differences were found in the need for blood transfusions following MAB. The certainty of the evidence was low (supplementary Table 1).
Hospitalization
Six studies analyzed hospitalization cases following MAB, with three [31, 45, 49] exclusively focusing on telemedicine patients and the other three [28, 50, 52] comparing this outcome among telemedicine patients and standard patients.
In the three studies that solely considered telemedicine patients, the average occurrence of this event was 1.3%. In the other three comparative studies [28, 50, 52], no statistically significant differences were observed between the telemedicine group, which had an average hospitalization rate of 0.1%, and the standard care group, which had an average hospitalization rate of 0.2% (RD = 0.00, 95%CI -0.00, 0.00; n = 34,677; I2 = 58%) (Fig. 6). In the subgroup meta-analyses (based on gestational weeks), no differences were found in hospitalization rates following MAB. The certainty of the evidence was low (supplementary Table 1).
Antibiotic treatment
Five studies assessed the need for antibiotic treatment in patients with a clinical suspicion of infection following MAB. Three of such studies focused exclusively on telemedicine patients [30, 34, 43], revealing an average incidence of 4.1% for this outcome. In the other two studies [29, 52], the average incidence of antibiotic treatment in the telemedicine group was 0.4%, while it was 0.05% in the standard group (RD = 0.00; 95%CI -0.00, 0.01; n = 19,913; I2 = 0%). The certainty of the evidence was moderate (supplementary Table 1).
Emergency department visits
One cross-sectional study [45] examined the frequency of emergency department visits among pregnant people who used MAB services provided through telemedicine and reported a frequency of 7.8%. Another cross-sectional study [28] compared this outcome between telemedicine patients and standard patients. The frequency of emergency department visits in the telemedicine group was 0.1%, while it was 0.2% in the standard group. No significant risk difference was observed between the two groups of interest (n = 20,343; p = 0.3).
Acceptability/Satisfaction
Acceptability
Three observational studies [18, 24, 46] evaluated the acceptability of MAB provided via telemedicine, with an average acceptability rate of 93.2%.
Satisfaction
Three observational studies [45, 48, 51] analyzed user satisfaction with MAB provided via telemedicine, with an average satisfaction rate of 98.3%. One clinical trial [32] and one cross-sectional study [26] compared this outcome between two forms of healthcare delivery. According to their results, the average satisfaction rate among telemedicine users was 99.3%, while it was 98.2% among standard users (RD = 0.01; 95%CI -0.02, 0.03; n = 1,134; I2 = 0%) (Fig. 7). The certainty of the evidence was low (supplementary Table 1).
Another noteworthy finding was the preference for telemedicine services. In a clinical trial [32], significant differences were observed in the proportion of pregnant people who preferred remote care, being higher in telemedicine care (97%) than in standard care (46%) (n = 717; p < 0.001).
Other outcomes
Successful follow-up
Two observational studies [31, 49] reported that, on average, 92% of patients who used telemedicine services for MAB had successful follow-up, typically occurring 45 days after taking the mifepristone dose.
Additionally, three cross-sectional studies [26, 29, 50] analyzed the follow-up rates after MAB, indicating that 77% and 70% of pregnant people using standard care group and telemedicine respectively, had successful follow-ups. The meta-analysis revealed no significant differences in lost to follow-up (RD = 0.05; 95%CI -0.18, 0.08; I2 = 95%), although it is evident that remote care exhibited higher rates of lost to follow-up. The certainty of the evidence was low (supplementary Table 1).
Waiting time to treatment
One prospective study [20] reported a reduction of 4.2 days in the waiting time to treatment for MAB via telemedicine when compared to standard care (Median Difference-MD = -4.2; 95%CI -7.07, -1.33; n = 52,147) (Fig. 8). The certainty of the evidence was low (supplementary Table 1).
Adherence to prescribed regimens
One clinical trial [32] evaluated adherence to abortion medication regimens. According to the results, the adherence rate was 94.7% in the telemedicine group and 96.1% in the standard care group, with no significant differences (n = 732; p = 0.89). The evaluation considered proper medication intake in terms of dosage, dose interval, route or manner of administration, and weeks’ gestation limits.
Discussion
This SLR included twenty studies published between 2011 and 2022, half of them between 2021 and 2022. Nineteen studies have an observational design. Of these, seven present data collected during the COVID-19 global health crisis. One of the included studies is an RCT conducted between February 2020 and October 2021, which compares telemedicine abortion care with in-person services. Overall, the risk of bias for the cross-sectional studies ranged from low to severe, while the RCT had a high risk of bias. Taken together, this body of literature provides up-to-date evidence on indicators of success, safety, and acceptability in the use of telemedicine to expand the provision of abortion care in the first trimester of pregnancy.
Based on observational studies with no control group, a 91.1% effectiveness was identified. This is similar to what Ngo et al. [54] reported in an SLR published in 2011, which evaluated the same research question and reported an 86–97% effectiveness of home MAB.
The effectiveness found in this SLR increased when care protocols included additional doses of misoprostol to the basic drug regimen (200 mg of mifepristone and 800 µg of misoprostol).
The meta-analysis of studies comparing telemedicine with standard care services indicates that the effectiveness of MAB is not influenced by the type of care provided. The analysis of effectiveness by subgroups, including weeks’ gestation and method of confirming treatment success, suggests that there are no significant interactions between the variables, as the estimated risk differences are minimal or negligible. Additionally, the results of the chi-square tests suggest that there is no statistically significant heterogeneity between the subgroups. It is important to note that, in forming the subgroups, the sample size was significantly reduced in some of them, which may affect the statistical power of the tests and, consequently, generate erroneous inferences.
Effectiveness decreases as the gestational limit increases; however, there were no statistically significant differences between telemedicine and in-person services for this variable. The effectiveness of MAB in pregnant people at 10-week gestation or less has been reported, with no differences between modalities of care [55]. In 2002, Ashok et al. [56] supported the effectiveness and safety of MAB between gestational weeks 10 and 13. However, in 2020, Schmidt-Hansen [55] proposed that more research is needed to support MAB in this period.
Effectiveness increased when doses of misoprostol were added to the basic drug regimen (200 mg of mifepristone plus 800 µg of misoprostol). A study on the use of abortion medications [57] identified that the use of 800 µg of misoprostol is more effective than 400 µg of misoprostol. Furthermore, it may increase the success of abortion if administered on the first day rather than on the third day, and there is no difference in its effectiveness if administered at home or in a clinic. In their study, Phupong et al. [58] concluded that the use of 600 µg and 1200 µg of misoprostol are equally effective, although the first dose reduces the occurrence of diarrhea as an adverse event. Another study that compared these two misoprostol regimens found a slightly greater effectiveness with the use of 1200 µg (66% with 600 µg and 70% with 1200 µg) and found no difference in the adverse effects produced [59]. The study recommended 800 µg of misoprostol for pregnant people under 10 weeks of gestation and 1000 to 1200 µg of misoprostol for pregnant people at 10–13 weeks of gestation. Another RCT [60] comparing these two doses of misoprostol found no difference in effectiveness between the two regimens given.
There are three methods that can be used for this: ultrasound, β-hCG levels in serum or urine. The most widely used for telemedicine services is the urine pregnancy test because it is easy to use at home. Studies support the use of this test [61, 62], although it should be considered that due to the detection threshold of β-hCG (< 50 mIU/mL), it may take a few weeks to become negative and thus interpret the result as a continuation of pregnancy, when it was actually a successful abortion. The other two tests (serum β-hCG and ultrasound) have been described as equally effective in measuring the outcome of abortion [63, 64].
Outcome on the need for surgery after MAB was measured both in observational studies without a comparison group and in those that compared the telemedicine care model with in-person services. As with the effectiveness indicator, surgical interventions interact with the additional doses of misoprostol added to the basic drug regimen. In this regard, the studies that added doses of misoprostol had a lower average prevalence of surgical interventions. In the meta-analysis of the comparative studies, no differences were found between the groups in the prevalence of postabortion surgery.
The safety of the telemedicine abortion procedure was documented in most of the included studies, with low rates of adverse events. No maternal deaths were reported. In observational studies without a comparison group, an average of 7.8%, 4.1%, 1.3%, and 0.5% of telemedicine patients attended the emergency department, required antibiotics, were hospitalized, or had a blood transfusion, respectively. However, there were no statistically significant differences in these indicators when comparing in-person services with telemedicine. The SLR by Ngo et al. [54] conducted in 2011 also found a low proportion of complications of MAB, finding that pain and vomiting were slightly longer lasting (0.3 days longer) among pregnant people who performed the procedure at home rather than in a medical facility.
In the meta-analysis, there were no differences in the proportion of pregnant people with follow-up after the abortion procedure, nor in adherence to treatment between the two modalities (telemedicine and in-person care). Nevertheless, the waiting time to receive abortion treatment was shorter among telemedicine patients.
The 2011 study by Grossman et al. went beyond establishing overall patient satisfaction, finding that initiating the abortion procedure as early as possible was a highly important factor [26]. This SLR found a significant difference in the waiting time for treatment initiation in favor of telemedicine. As in the satisfaction analysis, it is not possible to analyze this difference at all stages of the process. This result comes from an RCT conducted in a United States population [32], with a high risk of bias, which may vary significantly in regions with fewer human, financial, and technological resources. The same study reports that telemedicine is the preferred modality. In fact, nearly half of the pregnant people who used in-person modality preferred telemedicine[32]. This result may be affected by situations of availability or timeliness of telemedicine care, thus showing that there is room for strengthening virtual care services to meet their demand.
In 2022, Endler et al. [32] reported that adherence to the recommended drug regimens in telemedicine and in-person care was 94.7% and 96.1%, respectively, with no statistically significant differences between the two groups. This result may indicate that the information provided by the counseling staff of both health care modalities is sufficient and understandable to the public at large.
The average acceptability of telemedicine from three non-comparative studies was greater than 90%. Systematic reviews [25, 65] as well as observational studies [66] report results in the same trend, but with ranges of 60–100% acceptability [25]. However, several of the studies were developed based on data from organizations that provide abortion care exclusively by remote consultation, such as Women on Web; therefore, it is not known whether users had access to other care alternatives to choose from in terms of convenience or cost. These results contrast with those obtained by Dagousset et al., who reported that 55% of the pregnant people accepted home treatment if the health institution gave them the option of choosing place for treatment [67].
Similar to the results reported by Ngo et al. in their 2011 SLR [54], satisfaction was 88.4% in the telemedicine care group and 85.4% in the in-person care group. Since satisfaction is an indicator of the quality perceived by patients, the values obtained may be explained by the effectiveness and safety of the procedure. It should be noted that both modalities of care include several stages that are not documented in all studies, such as the assessment of the means of communication, appointment scheduling, care provided by health professionals, delivery or acquisition of medication, instructions for the home abortion process, and other related issues, which may be the subject of evaluation in future research.
The results of this study and the contrast with the scientific evidence that supports interventions in sexual and reproductive health provide sufficient evidence to sustain the effectiveness and safety of MAB managed through the provision of in-person or remote health services.
However, there is no consensus on the conditions necessary for the implementation of telemedicine services that can be adapted to each context, including the description of technological, infrastructure, cultural, and social needs for the widespread use of this abortion modality. This method also requires proposing solutions when Internet connection difficulties arise, in addition to promoting training on information and communication technologies and the provision of equipment that adequately supports the service.
This SLR does not address the analysis of the potential impact of intermediate determinants such as educational level or social representations of abortion of those who access it and those who perform it and promote it as a sexual and reproductive health right, and how these elements may affect the outcomes assessed. This is illustrated in the study by Ennis et al. (2023), which concludes that existing stigma toward health workers who provide abortion services impacts service delivery in terms of quality and frequency [68]. Regarding the experience of individuals accessing abortion services, social support is a determining factor in the mental health of patients, as noted in the study by Hendrix et al. [69].
Patient safety is a major concern when providing telemedicine care. Health care providers must ensure that patients meet the established eligibility criteria for MAB and that they receive the necessary information to make informed decisions. In this regard, there is extensive literature showing the ability of pregnant people to establish their weeks’ gestation from the date of last menstrual period [70,71,72,73]. Moreover, it is crucial to establish clear protocols for emergency care and appropriate referral in case of complications and adverse events.
Conclusions
Providing data of MAB provided through telemedicine is crucial for decision-makers to justify its implementation and widespread adoption. The published data support that MAB in the first-trimester abortion with telemedicine is an effective and safe alternative, similar to standard care. There were no differences between the care modalities in terms of other outcomes like user satisfaction, follow-up, and adherence; however, the telemedicine modality had a shorter waiting time for medication delivery.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- β-hCG:
-
Beta-human chorionic gonadotropin
- CI:
-
Confidence interval
- DeCS:
-
Descriptores en Ciencias de la Salud (Health Sciences Descriptors)
- ICT:
-
Information and Communication Technology
- MeSH:
-
Medical Subject Headings
- MAB:
-
Medication abortion
- MD:
-
Median difference
- PICOS:
-
Population, Intervention, Comparison, Outcome, and Study Design
- RCT:
-
Randomized Controlled Trial
- RD:
-
Risk difference
- SLR:
-
Systematic Literature Review
- WHO:
-
World Health Organization
References
World Health Organization. Safe abortion: technical and policy guidance for health systems, 2nd ed. [Internet]. 2° Edición. 2012. https://apps.who.int/iris/handle/10665/77079
World Health Organization. Abortion care guideline: executive summary. In 2022. http://apps.who.int/bookorders.
Singh S, Remez L, Sedgh G, Kwok L, Onda T. Abortion Worldwide 2017: Uneven Progress and Unequal Access [Internet]. 2018. https://www.guttmacher.org/report/abortion-worldwide-2017
Warriner I, Shah I. Preventing unsafe abortion and its consequences: priorities for research and action. New York: Guttmacher Institute [Internet]. 2006 [cited 2023 May 16]; https://www.guttmacher.org/sites/default/files/report_pdf/preventingunsafeabortion_0.pdf
Zane S, Creanga AA, Berg CJ, Pazol K, Suchdev DB, Jamieson DJ, et al. Abortion-related mortality in the United States: 1998–2010. Obstet Gynecol. 2015;126(2):258–65.
Directrices sobre la atención para el aborto Resumen ejecutivo [Internet]. Available from: http://apps.who.int/bookorders.
Organización Mundial de la Salud. Funciones del personal sanitario en la atención para un aborto sin riesgos. 2015 [cited 2023 Feb 12]; https://apps.who.int/iris/handle/10665/204374
Ministerio de Salud y Protección Social. Prevención del Aborto Inseguro en Colombia. Protocolo para el sector salud. 2014.
Ministerio de Salud y Protección Social. Determinantes del aborto inseguro y barreras de acceso para la atención de la IVE en mujeres colombianas. 2014 [cited 2023 Feb 12]; https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/SM-Determ-aborto-inseguro.pdf
World Health Organization. Medical management of abortion [Internet]. 2019. http://apps.who.int/bookorders.
Profamilia. Asociación Profamilia y MEXFAM (2021). Acceso al aborto seguro en tiempos de COVID-19: desafíos y oportunidades para la prestación del servicio de aborto por telemedicina en Colombia y México. [Internet]. Bogotá D.C y Ciudad de México; 2021 [cited 2023 May 29]. https://profamilia.org.co/wp-content/uploads/2021/05/Acceso-al-aborto-seguro-en-tiempos-de-COVID-19-Digital.pdf
WHO Global Observatory for eHealth. (2010). Telemedicine: opportunities and developments in Member States: report on the second global survey on eHealth. World Health Organization [Internet]. 2009 [cited 2023 Feb 13]; https://apps.who.int/iris/handle/10665/44497
World Health Organization. Informática de la salud y telemedicina. Informe del director general [Internet]. 1997 Jan [cited 2023 Jun 7]. https://apps.who.int/iris/bitstream/handle/10665/194008/EB99_30_spa.pdf
Universidad Politécnica de Madrid. Grupo de bioingeniería y telemedicina. Bases metodológicas para evaluar la viabilidad y el impacto de proyectos de telemedicina [Internet]. Organización Panamericana de la Salud, editor. Madrid, España: Organización Panamericana de la salud; 2000 [cited 2023 Jun 7]. https://www3.paho.org/hq/dmdocuments/2009/BasesMetologicasparaEvaluar.pdf
World Health Organization. WHO guideline: recommendations on digital interventions for health system strengthening. [Internet]. Ginebra; 2022 [cited 2023 Jun 6]. Available from: https://apps.who.int/iris/bitstream/handle/10665/354399/9789240046993-spa.pdf?sequence=1&isAllowed=y
Organisation for Economic Co-operation and Development. The future of telemedicine after COVID-19 [Internet]. 2023 Jan [cited 2023 May 29]. Available from: https://read.oecd-ilibrary.org/view/?ref=1178_1178746-yy7ysc5k0j&title=The-future-of-telemedicine-after-COVID-19
Centers for Disease Control and Prevention. Telemedicina, ¿qué significa y por qué le debería importar? [Internet]. 2020 [cited 2023 Feb 8]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/global-covid-19/telemedicine-sp.html
Nortén H, Ilozumba O, Wilkinson J, Gemzell-Danielsson K, Gomperts R. 10-year evaluation of the use of medical abortion through telemedicine: a retrospective cohort study. BJOG. 2022;129(1):151–9.
Lee S, Hitt WC. Clinical Applications of Telemedicine in Gynecology and Women’s Health. Vol. 47, Obstetrics and Gynecology Clinics of North America. W.B. Saunders; 2020. p. 259–70.
Aiken A, Lohr P, Lord J, Ghosh N, Starling J. Effectiveness, safety and acceptability of no-test medical abortion (termination of pregnancy) provided via telemedicine: a national cohort study. BJOG. 2021;128(9):1475–6.
Grossman D. Telemedicine for medical abortion – time to move towards broad implementation. Vol. 126, BJOG: An International Journal of Obstetrics and Gynaecology. Blackwell Publishing Ltd; 2019. p. 1103.
Deza S. Teleatención de abortos. Primera edición. Florencia Sabaté, editor. 2022.
WHO Global Observatory for eHealth. (2010). Telemedicine: opportunities and developments in Member States: report on the second global survey on eHealth. World Health Organization [Internet]. 2009 [cited 2023 Feb 13]; Available from: https://apps.who.int/iris/handle/10665/44497
Reynolds-Wright JJ, Johnstone A, McCabe K, Evans E, Cameron S. Adherence to treatment and prevalence of side effects when medical abortion is delivered via telemedicine: a prospective observational cohort study during COVID-19. BMJ Sex Reprod Health. 2022;48(3):185–92.
Endler M, Lavelanet A, Cleeve A, Ganatra B, Gomperts R, Gemzell-Danielsson K. Telemedicine for medical abortion: a systematic review. Vol. 126, BJOG: An International Journal of Obstetrics and Gynaecology. Blackwell Publishing Ltd; 2019. p. 1094–102.
Grossman D, Grindlay K, Buchacker T, Lane K, Blanchard K. Effectiveness and acceptability of medical abortion provided through telemedicine. Obstet Gynecol. 2011;118(2):296–303.
Glasier A, Regan L. Induced abortion via telemedicine should become the norm: a commentary. Vol. 128, BJOG: An International Journal of Obstetrics and Gynaecology. John Wiley and Sons Inc; 2021. p. 1475–6.
Grossman D, Grindlay K. Safety of medical abortion provided through telemedicine compared with in person. In: Obstetrics and Gynecology. Lippincott Williams and Wilkins; 2017. p. 778–82.
Wiebe ER, Campbell M, Ramasamy H, Kelly M. Comparing telemedicine to in-clinic medication abortions induced with mifepristone and misoprostol. Contracept X. 2020;2:100023.
Larrea S, Palència L, Perez G. Medical abortion provided by telemedicine to women in Latin America: complications and their treatment. Gac Sanit. 2015;29(3):198–204.
Peña M, Figueroa Flores K, Muñoz Ponce M, Facio Serafín D, Camarillo Zavala AM, Ruiz Cruz C, et al. Telemedicine for medical abortion service provision in Mexico: a safety, feasibility, and acceptability study. Contraception. 2022;1(114):67–73.
Endler M, Petro G, Danielsson KG, Grossman D, Gomperts R, Weinryb M, et al. A telemedicine model for abortion in South Africa: a randomised, controlled, non-inferiority trial. The Lancet [Internet]. 2022; Available from: www.thelancet.com
Reynolds-Wright JJ, Johnstone A, McCabe K, Evans E, Cameron S. Telemedicine medical abortion at home under 12 weeks’ gestation: a prospective observational cohort study during the COVID-19 pandemic. BMJ Sex Reprod Health. 2021;47(4):246–51.
Aiken ARA, Romanova EP, Morber JR, Gomperts R. Safety and effectiveness of self-managed medication abortion provided using online telemedicine in the United States: a population based study. Lancet Regional Health - Americas. 2022;10:100200.
World Health Organization. Consolidated telemedicine implementation guide. 2022.
Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [Internet]. 2011. Available from: www.cochrane-handbook.org.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, PRISMA, et al. explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2020;2021:372.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):1–10. https://doi.org/10.1186/s13643-016-0384-4.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:1.
Cochrane. Review Manager RevMan5.4. 2020.
Schünemann H, Brożek J, Guyatt G, Oxman A. Manual GRADE. Grading of Recommendations, Assessment, Development and Evaluation. [Internet]. 2017 [cited 2023 Jan 28]. Available from: https://gdt.gradepro.org/app/handbook/translations/es/handbook.html
McMaster University and Evidence Prime Inc. GRADEpro [Internet]. 2021 [cited 2023 Jan 28]. Available from: https://www.gradepro.org/
Aiken ARA, DIgol I, Trussell J, Gomperts R. Self reported outcomes and adverse events after medical abortion through online telemedicine: Population based study in the Republic of Ireland and Northern Ireland. BMJ. 2017;357:1.
Aiken A, Gomperts R, Trussell J, Hall SR. Experiences and characteristics of women seeking and completing at-home medical termination of pregnancy through online telemedicine in Ireland and Northern Ireland: a population-based analysis. BJOG [Internet]. 2016; Available from: www.bjog.org
Chong E, Shochet T, Raymond E, Platais I, Anger HA, Raidoo S, et al. Expansion of a direct-to-patient telemedicine abortion service in the United States and experience during the COVID-19 pandemic. Contraception. 2021;104(1):43–8.
Gomperts R, Petow SAM, Jelinska K, Steen L, Gemzell-Danielsson K, Kleiverda G. Regional differences in surgical intervention following medical termination of pregnancy provided by telemedicine. Acta Obstet Gynecol Scand. 2012;91(2):226–31.
Gomperts R, Van Der Vleuten K, Jelinska K, Da Costa CV, Gemzell-Danielsson K, Kleiverda G. Provision of medical abortion using telemedicine in Brazil. Contraception. 2014;89(2):129–33.
Comendant R, Cook C, Hodorogea S, Sagaidac I, Bubulici C, Platais I. Medical abortion via telemedicine for women and adolescents: experience from Moldova. Reprod Female Child Health. 2022;1(1):80–7.
Hyland P, Raymond EG, Chong E. A direct-to-patient telemedicine abortion service in Australia: retrospective analysis of the first 18 months. Aust N Z J Obstet Gynaecol. 2018;58(3):335–40.
Kohn JE, Snow JL, Simons HR, Seymour JW, Thompson TA, Grossman D. Medication abortion provided through telemedicine in four US States. Obstetr Gynecol. 2019;134(2):343–50.
Meurice ME, Whitehouse KC, Blaylock R, Chang JJ, Lohr PA. Client satisfaction and experience of telemedicine and home use of mifepristone and misoprostol for abortion up to 10 weeks’ gestation at British Pregnancy Advisory Service: A cross-sectional evaluation. Contraception. 2021;104(1):61–6.
Seymour JW, Melville C, Thompson TA, Grossman D. Effectiveness and safety of a direct-to-patient telehealth service providing medication abortion targeted at rural and remote populations: cross-sectional findings from Marie Stopes Australia. Contraception. 2022;1(115):67–8.
Aiken A, Lohr P, Lord J, Ghosh N, Starling J. Effectiveness, safety and acceptability of no-test medical abortion (termination of pregnancy) provided via telemedicine: a national cohort study. BJOG. 2021;128(9):1464–74.
Ngo TD, Park MH, Shakura H, Free C. Comparación de la efectividad, la seguridad y la aceptación de los abortos médicos practicados en el domicilio con aquellos realizados en la clínica: Una revisión sistemática. Bull World Health Organ. 2011;89(5):360–70.
Schmidt-Hansen M, Pandey A, Lohr PA, Nevill M, Taylor P, Hasler E, et al. Expulsion at home for early medical abortion: a systematic review with meta-analyses. Acta Obstet Gynecol Scand. 2021;100(4):727–35.
Ashok PW, Kidd A, Flett GMM, Fitzmaurice A, Graham W, Templeton A. A randomized comparison of medical abortion and surgical vacuum aspiration at 10–13 weeks gestation. Hum Reprod. 2002;17(1):92–8.
Zhang J, Zhou K, Shan D, Luo X. Medical methods for first trimester abortion. Vol. 2022, Cochrane Database of Systematic Reviews. John Wiley and Sons Ltd; 2022.
Phupong V, Taneepanichskul S, Kriengsinyot R, Sriyirojana N, Blanchard K, Winikoff B. Comparative study between single dose 600 μg and repeated dose of oral misoprostol for treatment of incomplete abortion. Contraception. 2004;70(4):307–11.
Blanchard K, Taneepanichskul S, Kiriwat O, Sirimai K, Svirirojana N, Mavimbela N, et al. Two regimens of misoprostol for treatment of incomplete abortion. Obstetr Gynecol. 2004;103(5):860–5.
Nguyen TNN, Blum J, Durocher J, Quan TTV, Winikoff B. A randomized controlled study comparing 600 versus 1200 μg oral misoprostol for medical management of incomplete abortion. Contraception. 2005;72(6):438–42.
Raymond EG, Shochet T, Bracken H. Low-sensitivity urine pregnancy testing to assess medical abortion outcome: A systematic review. Vol. 98, Contraception. Elsevier USA; 2018. p. 30–5.
Fiala C, Bombas T, Parachini M, Agostini A, Lertxundi R, Lubusky M, et al. hCG Testing to Determine Outcome after Medical Abortion: A Review. 2019;
Behnamfar F, Mahdian M, Rahimi F, Samimi M. Misoprostol abortion: Ultrasonography versus beta-hCG testing for verification of effectiveness. Pak J Med Sci. 2013;29:6.
Peracheh M, Teymouri B, Noori N, Arbabzadeh T, Ghasemi M. Evaluating the agreement of ultrasound imaging and beta-human chorionic gonadotropin (β-hCG) measurement in confirming completed medical abortion: Cross-sectional study. Qatar Med J. 2021;2021:2.
Gambir K, Garnsey C, Necastro KA, Ngo TD. Effectiveness, safety and acceptability of medical abortion at home versus in the clinic: a systematic review and meta-analysis in response to COVID-19. BMJ Glob Health. 2020;5(12): e003934.
Erlank CP, Lord J, Church K. Early medical abortion using telemedicine – acceptability to patients. medRxiv [Internet]. 2020 Jan 1;2020.11.11.20229377. Available from: http://medrxiv.org/content/early/2020/12/19/2020.11.11.20229377.abstract
Dagousset I, Fourrier E, Aubény E, Taurelle R. Enquête d’acceptabilité du misoprostol à domicile pour interruption volontaire de grossesse par méthode médicamenteuse. Gynecol Obstet Fertil. 2004;32(1):28–33.
Ennis M, Renner RM, Olure B, Norman W V, Begun S, Martin L, et al. Experience of stigma and harassment among respondents to the 2019 Canadian abortion provider survey. Contraception [Internet]. 2023 May [cited 2023 Jun 13];0(0):110083. Available from: http://www.contraceptionjournal.org/article/S0010782423001646/fulltext
Hendrix T, Roncoroni J, Magdamo B, Whitaker S, Zareba K, Grieco N. Stigma, Social Support, and Decision Satisfaction in Terminations of Pregnancy for Medical Reasons. Women’s Health Reports [Internet]. 2023 [cited 2023 Jun 13];4(1):271. Available from: /pmc/articles/PMC10240332/
Saavedra-Avendano B, Schiavon R, Sanhueza P, Rios-Polanco R, Garcia-Martinez L, Darney BG. Early termination of pregnancy: Differences in gestational age estimation using last menstrual period and ultrasound in Mexico. Reprod Health. 2020;17:1.
Ralph LJ, Ehrenreich K, Barar R, Biggs MA, Morris N, Blanchard K, et al. Accuracy of self-assessment of gestational duration among people seeking abortion. Am J Obstet Gynecol. 2022;226(5):710.e1-710.e21.
Kaneshiro B, Edelman A, Sneeringer RK, Ponce De Leon RG. Expanding medical abortion: Can medical abortion be effectively provided without the routine use of ultrasound? Vol. 83, Contraception. Elsevier USA; 2011. p. 194–201.
Schonberg D, Wang LF, Bennett AH, Gold M, Jackson E. The accuracy of using last menstrual period to determine gestational age for first trimester medication abortion: A systematic review. Vol. 90, Contraception. Elsevier USA; 2014. p. 480–7.
Acknowledgements
Not applicable.
Funding
This research was supported by Profamilia (Colombia) and Ipas Latin America and the Caribbean. Ipas researchers have worked in the conceptualization and manuscript development.
Author information
Authors and Affiliations
Contributions
LCA, KCG and LCES contributed with the conception and design of the SLR. Data curation and analysis was performed by LCA, KCG and LCES. Interpretation of data was done by LCA, KCG, LCES, BSA and GAOA. The manuscript was written by LCA, KCG, LCES and BSA. LCES produced the figures. KCG elaborated the table. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix A.
Search terms and search strategies used for each database.
Additional file 2: Table S1.
Summary of findings and certainty of evidence: telemedicine compared with standard care for provision of medication abortion.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Cely-Andrade, L., Cárdenas-Garzón, K., Enríquez-Santander, L.C. et al. Telemedicine for the provision of medication abortion to pregnant people at up to twelve weeks of pregnancy: a systematic literature review and meta-analysis. Reprod Health 21, 136 (2024). https://doi.org/10.1186/s12978-024-01864-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12978-024-01864-4