Abstract
Background
This study investigated the mediating effects of self-efficacy and social support on the relationship between stress and burnout among infection control nurses (ICNs) during an emerging infectious disease pandemic.
Methods
The study participants encompassed 210 ICNs with at least six months’ experience in an infection control unit at a general hospital in South Korea during the COVID-19 pandemic. Data were analyzed using independent t-tests or one-way analysis of variance (ANOVA), while descriptive statistics were performed using SPSS/WIN 26.0 software. Hayes’s PROCESS macro 4.2 software was used to verify the significance of the indirect effects of the mediators.
Results
Stress had a significant positive effect on burnout (β = 0.80, p < .001), accounting for 73% of the variance. Self-efficacy (β = − 0.26, p < .001) and social support (β = − 0.11, p = .034) had a significant negative effect on burnout, accounting for 78% of the variance. Stress was lower when self-efficacy and social support were entered into the model (β = 0.80 → 0.59), indicating that self-efficacy and social support mediated the relationship between stress and burnout.
Conclusion
This study is significant in that it confirms the effects of self-efficacy and social support on the relationship between stress and burnout among ICNs. The results highlight the importance of establishing organizational support systems and developing and implementing programs for enhancing self-efficacy in order to reduce burnout among ICNs.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The global spread of coronavirus disease 2019 (COVID-19), initiated by the SARS-CoV-2 virus in December 2019, led the World Health Organization (WHO) to declare a pandemic in March 2020, the highest warning level for infectious diseases [1]. The emergence of new variants, such as Beta, Delta, and Omicron, intensified COVID-19’s global threat and the populace’s anxiety [2]. Despite international efforts to combat the virus, the WHO declared it endemic in May 2023 after three years of fighting the pandemic [1]. The history of infectious diseases, including severe acute respiratory syndrome (SARS) in 2003, H1N1 in 2009, and Middle East respiratory syndrome (MERS) in 2015, suggests that the threat of both new and reemerging infectious diseases is ongoing [3]. The unprecedented crisis presented by the COVID-19 pandemic significantly impacted healthcare services, society, and the economy, highlighting the need for developing and implementing proactive management and prevention strategies against such infectious diseases [4].
To ensure systematic infection control, relevant laws were amended in 2016, in South Korea while the standards for infection control staffing were strengthened for each type of hospital, thereby intensifying the roles and responsibilities of infection control nurses (ICNs) [5]. ICN nurses play a pivotal role in preventing disease outbreaks and curbing the spread of infections among patients, caregivers, and staff [6]. During the COVID-19 pandemic, their duties expanded from standard infection control practices to tasks such as information gathering, reporting, policy-related decision-making and implementation, staff education (e.g., regarding infection, isolation procedures, and use of personal protective equipment), advising and consulting, coordination of epidemiological investigations, and management of exposed individuals. The additional responsibilities also increased their administrative workload [6].
During the prolonged COVID-19 pandemic, ICNs experienced significant physical and mental exhaustion due to overwhelming workloads and the pressure to manage all aspects of infection control at the frontline [7]. The broad scope of their responsibilities increased their stress [8, 9]. Continuous work-related stress in nurses can cause them to become disinterested in their patients, decrease their work efficiency and productivity, increase their turnover and absenteeism rates, increase depression, and, ultimately, cause burnout—a state of physical, emotional, and mental exhaustion [9, 10]. Thus, it is important to assess the extent of the increased stress and burnout among ICNs in a challenging context such as the COVID-19 pandemic.
Burnout is a negative experience caused by repetitive exposure to stressors; it refers to a state of energy depletion that induces emotional exhaustion, feelings of anger, powerlessness, and depression [11]. Nurses who fail to cope with increases in work-related stress and consequently experience burnout have reduced job satisfaction, exhibit a poor quality of care, and have high turnover rates, thereby creating a cycle of negative outcomes [12]. Persistent burnout not only affects individuals but also impacts organizational efficiency and effective personnel management [13]. Thus, nurses’ burnout is a major issue for clinical practice.
Self-efficacy and social support have been identified as factors that mitigate stress and reduce burnout [13,14,15,16,17,18]. Self-efficacy is a belief in one’s ability to achieve desired goals in a particular situation [19], and a lack of self-efficacy in nurses can lead to low confidence in their work to manage and prevent infectious diseases [20]. Social support is the support and encouragement nurses receive from their peers, supervisors, family members, and others [18, 21]. Infection control work involves a high degree of emergency and risk, which can place a high emotional burden on nurses [8]. Inadequate social support can lead to nurses feeling isolated, which increases the risk of burnout [13]. On the other hand, nurses with enhanced self-efficacy and social support are better able to cope with and manage the stress of their work, thereby reducing burnout [18].
Previous studies on ICNs have examined the relationship between work satisfaction, ego resilience, and job stress [8], path models for burnout and retention intention [22], the core competencies of ICNs [5], and the important roles of ICNs [23]. Studies have also explored ICNs’ work experiences during the COVID-19 outbreak [7]; however, few studies have examined ICN burnout.
In this study, we established a conceptual framework of the study’s variables based on Lazarus & Folkman’s [24] stress, appraisal-coping model to investigate the relationship between stress and burnout among ICNs. Previous studies on stress-coping and adaptation have used this model as a theoretical framework because it provides a systematic and logical framework for understanding the processes of appraisal, coping, and adaptation in response to stressful events [25, 26]. As stress is conceptualized as an interaction between the individual and their environment, as opposed to a simple stimulus [24], we included personal-level factors (gender, age, education, spouse, position, salary, type of hospital, clinical career, infection control career, and certification) as contextual factors that could affect burnout. We used stress as the environmental variable, social support and self-efficacy as coping resources (mediators), and burnout as the negative outcome.
To effectively prepare for future emerging infectious disease crises, it is crucial to identify factors influencing burnout among ICNs. Utilizing this data can help mitigate ICN burnout, foster expertise in infection prevention within healthcare facilities, and enhance patient safety and nursing care quality.
Therefore, this study aims to provide basic data for developing nursing intervention programs by identifying the relationship between stress and burnout in infection control nurses during the COVID-19 pandemic based on Lazarus & Folkman’s [24] stress, appraisal-coping model; in this way, this study sought to confirm the mediating effect of self-efficacy and social support in burnout alleviation.
Method
Study design
This descriptive correlation study attempted to confirm the mediating effect of self-efficacy and social support on the relationship between stress and burnout in infection control nurses who worked in general hospitals during the pandemic based on Lazarus & Folkman’s [24] stress, appraisal-coping model.
Participants
Inclusion criteria were ICNs who had worked in the infection control department of a general hospital in South Korea for at least six months between January 2020, when the first case of COVID-19 was confirmed in South Korea, and May 2023 (Endemic declaration). Exclusion criteria were temporary seconded nurses, even if they had worked in an infection control unit for more than six months during the pandemic. The study included 210 ICNs who understood the purpose of the study and gave consent. The sample size was determined using G-power 3.1 software. For a regression analysis with a significance level of 0.05, a medium effect size of 0.15 [27], a power of 95%, and 14 predictor variables, the minimum sample size was determined as 194. Thus, our study sample size was adequate for the intended statistical analyses.
Instruments
The relevant instruments were used after obtaining permission from the authors via e-mail. The structured questionnaire was validated by two nursing professors and two ICNs.
Burnout
We purchased the Korean version of the Maslach burnout inventory-human services survey (medical personnel) (MBI-HSS [MP]), which was originally developed by Maslach and Jackson [11]. The MBI-HSS (MP) is a 22-item scale with three subscales: emotional exhaustion (9 items), depersonalization (5 items), and reduced personal accomplishment (8 items). Each item is rated on a seven-point scale, ranging from 0 (“none”) to 6 (“every day”). A higher score indicates a higher degree of burnout. In this study, we used the mean total score. The Cronbach’s α values in Maslach and Jackson [11] was 0.76; this value was 0.86 and 0.93 in our study.
Self-efficacy
We used six items for self-efficacy from the Korean version of the Copenhagen psychosocial questionnaire II (COPSOQ-K) [28]; the original scale had been developed by Pejtersen et al. [29]. Each item is rated on a five-point scale ranging from 0 (“never/hardly ever”), 25(‘’seldom’’), 50(‘’sometimes’’), 75(‘’often’’), to 100 (“always”). A higher score indicates higher self-efficacy. In this study, we used the mean total score. “The Cronbach’s α values in Jeon and Choi’s study [28] was .80; this value was .92 in our study.”
Stress
We used four items for stress and four items for perceived stress from the COPSOQ-K [28]. Each item was rated on a five-point scale ranging from 0 (“never/hardly ever”), 25(‘’seldom’’), 50(‘’sometimes’’), 75(‘’often’’), to 100 (“always”). A higher score indicated a greater degree of stress. The Cronbach’s α values in Jeon and Choi’s study [28] was 0.81; this value was 0.82 in our study.
Social support
We used three items for support from Social Support from Colleagues and three items for Social Support from Supervisor from the COPSOQ-K [28]. Each item was rated on a five-point scale ranging from 0 (“never/hardly ever”), 25(‘’seldom’’), 50(‘’sometimes’’), 75(‘’often’’), to 100 (“always”). A higher score indicated a greater degree of social support. The Cronbach’s α values in Jeon and Choi’s study [28] were 0.76 and 0.86; these values were 0.86 and 0.91 in our study.
Data collection
Data were collected from 4 October to 30 November 2023 from ICNs who had experience in infection control work in the infection control departments of Korean general hospitals during the COVID-19 pandemic. The research assistants contacted infection control units a general hospital to explain the purpose and method of the study and obtained permission to conduct the study. Next, ICNs received a link to the online survey. Purposive sampling was used to recruit eligible ICNs. The questionnaire took approximately 20 min to complete, and a small gift was provided as a token of appreciation after the survey completion.
Ethical considerations
This study was approved by the Institutional Review Board at the authors’ institution (IRB NO: KCN-2023-0901-02-2). Participants who checked the box “I agree” on the online survey’s consent page were allowed to proceed with the questionnaire. The information page provided information about the purpose of the study, the anonymity of the participants, the freedom to withdraw from the study at any time without any repercussions, and the anticipated benefits and risks of study participation. Participants’ data were assigned individual IDs to maintain their anonymity. All study-related data were stored on a password-protected computer for strict management and control. These data will be discarded after the legally specified period of three years.
Data analysis
The collected data were analyzed using SPSS Statistics 26 software and the Process macro ver. 4.2, while statistical significance was determined as 0.05.
Participants’ general characteristics were analyzed using a frequency analysis, while the differences in burnout experiences based on general characteristics were tested using independent t-tests and one-way analysis of variance (ANOVA). For factors that differed significantly, a Scheffé test was performed as a post-hoc comparison. Levels of stress, self-efficacy, social support, and burnout were examined using descriptive statistics. Correlations between stress, self-efficacy, social support, and burnout were analyzed using Pearson correlation analysis.
The effects of the relationships between stress, self-efficacy, social support, and burnout; the estimation of the indirect effect size of stress with regard to burnout through the mediation of self-efficacy and social support; and the statistical significance of the mediating effects were analyzed using the bootstrapping method as proposed by Hayes. Bootstrapping was performed using Process macro model 4.
Results
Burnout according to participants’ general characteristics
A frequency analysis was performed to analyze participants’ general characteristics. There were five male (2.4%) and 205 female (97.6%) participants. The mean age was 33.35 years, with 57 individuals aged 20–29 years (27.1%), 121 aged 30–39 years (57.6%), and 32 aged 40–49 years (15.2%). Regarding education, 24 participants had an associate degree (11.4%), 134 had a bachelor’s degree (63.8%), and 52 had a master’s degree or higher (24.8%). Eighty-six participants were married (41.0%), and 124 were single (59.0%). In terms of job position, 148 were staff nurses (70.5%), 48 were charge nurses (22.9%), and 14 were nurse managers or higher (6.7%). The mean annual salary was 47.41 million KRW. Sixty-four participants earned < 40 million KRW (30.5%), 73 earned 40–49 million KRW (34.8%), and 73 earned ≥ 50 million KRW (34.8%). Hospital type was secondary (n = 134, 63.8%) or tertiary (n = 76, 36.2%). Mean clinical experience was 8.63 years. Thirty-three participants had < 5 years (15.7%) of experience, 107 had 5–9 years (51.0%) of experience, and 70 had ≥ 10 years (33.3%) of experience. The mean infection control experience was 3.28 years. Fifty-one participants had < 2 years (24.3%) of experience, 107 had 2-3.9 years (51.0%) of experience, and 52 had ≥ 4 years (24.8%) of experience. In terms of certification, 49 participants were certified as ICNs (23.3%), 26 were certified as infection control practitioners (12.4%), and 135 were not certified (64.3%).
We analyzed differences in burnout according to the general characteristics of ICNs using independent t-tests and one-way ANOVAs. Burnout significantly differed according to job position (F = 7.96, p < .001), clinical career (F = 3.93, p = .021), and certification (F = 6.87, p = .001).
A post-hoc comparison was performed using a Scheffé test for the three factors that significantly differed in terms of their impact on burnout. In terms of job position, burnout was significantly higher among charge nurses than among nurse managers or those with higher designations. Burnout was also significantly higher among those with a clinical career of 5–9 or ≥ 10 years of experience, compared to among those with < 5 years of experience. Burnout was also significantly higher among certified infection control practitioners, compared to that among certified ICNs and non-certified ICNs (Table 1).
Participants’ stress, self-efficacy, social support, and burnout
Descriptive statistics were used to describe participants’ stress, self-efficacy, social support, and burnout. The mean stress score was 56.55 out of 100; the mean self-efficacy score was 54.62 out of 100; the mean social support score was 58.71 out of 100; and the mean burnout score was 4.08 in a range of 0–6. Skewness and kurtosis were calculated to test the normality of the data. The absolute value of skewness was < 2, while that of kurtosis was < 7, confirming the normality of the data [30]. In short, the data were suitable for statistical analysis (Table 2).
Correlations between participants’ stress, self-efficacy, social support, and burnout
The correlations between participants’ stress, self-efficacy, social support, and burnout were analyzed using Pearson correlation analysis. Stress was significantly negatively correlated with self-efficacy (r = − .64, p < .001) and social support (r = − .47, p < .001) and significantly positively correlated with burnout (r = .81, p < .001). Self-efficacy was significantly positively correlated with social support (r = .63, p < .001) and significantly negatively correlated with burnout (r = − .71, p < .001). Social support was significantly negatively correlated with burnout (r = − .56, p < .001) (Table 3).
The relationships among participants’ stress, self-efficacy, social support, and burnout
We analyzed the effect relationships between participants’ stress, self-efficacy, social support, and burnout, and the mediating effects of self-efficacy and social support in the relationship between stress and burnout by using Hayes’ bootstrapping with Process macro model 4. Bootstrapping was performed with 5,000 samples and a 95% confidence interval (CI). Job position, clinical career, and certification differed significantly vis-à-vis burnout and were selected as control variables. As job position and certification were categorical variables, dummy variables were created for charge nurses and ICNs who showed relatively higher levels of burnout.
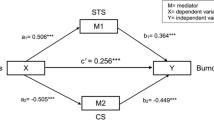
First, the model for the effects of stress on self-efficacy accounted for 51% of the variance, while stress had a significant negative effect on self-efficacy (β = − 0.63, p < .001). The model for the effects of stress on social support accounted for 27% of the variance, while stress had a significant negative effect on social support (β = − 0.42, p < .001). In short, self-efficacy and social support declined with increasing stress. The model for the effects of stress on burnout accounted for 73% of the variance, while stress had a significant positive effect on burnout (β = 0.80, p < .001), suggesting that burnout increases with increasing stress.
Next, self-efficacy and social support were added to the model to examine their effects on burnout. The regression model accounted for 78% of the variance, and self-efficacy (β=-0.26, p < .001) and social support (β = − 0.11, p = .034) had a significant negative effect on burnout. In short, burnout decreased with increasing self-efficacy and social support. Conversely, stress was reduced after adding self-efficacy and social support to the model (β = 0.80 → 0.59), suggesting that self-efficacy and social support mediate the relationship between stress and burnout (Table 4).
Next, we examined the direct effect of stress on burnout, the indirect effect of stress on burnout through the mediation of self-efficacy and social support, and their 95% CIs. The direct effect size of stress on burnout was 0.68, while the 95% CI was 0.01-0.12. In both cases, CI do not include 0, thereby confirming statistical significance.
The indirect effect size of stress on burnout through the mediation of self-efficacy was 0.19, while the 95% CI was 0.10-0.29. The indirect effect size of stress on burnout through the mediation of social support was 0.05, while the 95% CI was 0.01-0.12. In both cases, CI included 0, thereby confirming statistical significance. In essence, the results show that stress had an indirect effect on burnout through the mediation of self-efficacy and social support. That is, ICNs who had high levels of stress during the COVID-19 pandemic also had lower self-efficacy and less social support, which, in turn, led to higher levels of burnout (Table 5) (Fig. 1).
Discussion
Based on Lazarus & Folkman’s [24] stress, appraisal-coping model l, this study attempted to confirm the mediating effect of self-efficacy and social support in the relationship between stress and burnout in infection control nurses who worked in general hospitals during an emerging infectious disease pandemic.
In this study, the mean burnout score during the COVID-19 pandemic was 4.08. The mean burnout score of staff nurses was 2.61 [31]. The mean burnout score of nurses who provided direct patient care on a medical-surgical floor and isolation floor or in an ICU and emergency department was 2.80 [12]. This showed that the burnout scores of other nurses were markedly lower than the burnout scores of ICNs, despite being substantially higher compared to the pre-COVID-19 period. A previous study [22] showed that the mean burnout score among ICNs was 2.30 before the COVID-19 pandemic and that this figure nearly doubled to 4.08 during the pandemic. Particularly, before the COVID-19 pandemic, ICNs had lower burnout rates compared with other nurses [22]; this highlights the need to pay attention to the dramatic increase in the level of burnout among ICNs. Thus, there is a pressing need to discern burnout predictors among ICNs following the COVID-19 pandemic and to promptly implement interventions that reduce burnout in these nurses.
In our study, stress had a direct effect on burnout among ICNs. Although a direct comparison is difficult to establish due to the lack of research on these variables among ICNs, burnout increase accompanied stress increase in nurses during the COVID-19 pandemic [12] and job stress was the most potent predictor of burnout among nurses during the COVID-19 pandemic [10], thereby supporting our findings. Grzelak and Szwarc [32] reported that 89.2% of nurses experienced increased stress symptoms due to the pandemic, and Tomaszewska et al. [9] reported that 50% of nurses experienced burnout.
ICNs faced significant levels of stress owing to the extremely high transmissibility of COVID-19, which contributed to the rapid spread of the virus; it had higher morbidity and mortality rates compared with SARS and MERS [17]. Although not involved in direct patient care, ICNs were frequently placed in situations calling for independent decision-making based on expert knowledge and were expected to demonstrate a wide array of competencies to engage in interdisciplinary collaborations within and outside the hospital [6]; these added responsibilities and psychological burdens caused high levels of stress [8]. Individuals who experience burnout define it as physical, emotional, and mental exhaustion—a point at which they can no longer cope with stress. Unresolved burnout engenders psychological impairments, such as a sense of failure and guilt, as well as reduced job productivity and nursing performance [10].
Prolonged burnout causes job dissatisfaction and negative work attitudes, which, in turn, lead to high turnover intentions and actual turnover, thereby causing a shortage of nursing staff and decreased quality of care [9]. Turnover intention was reported to be higher among nurses who provided care for patients with COVID-19, compared with nurses working on a regular medical-surgical floor [12]. Therefore, another infectious disease crisis in the future may result in a shortage of staff, which would be detrimental to the effective management of and response to infectious diseases [10, 13]. Considering the prolonged stress caused by an emerging infectious disease pandemic, it is of paramount importance to provide adequate and appropriate health management—including environmental and personnel management—to reduce stress among ICNs. Measures, such as the establishment of flexible staff management that considers work intensity and work hours (depending on the severity of the emerging infectious disease crisis), inter-departmental work coordination, and environmental improvement, must be implemented concurrently. As the burnout caused by high levels of persistent stress among ICNs can impact both individuals and organizations, nursing organizations should develop policies and stress reduction programs that promote psychological replenishments to prevent and manage nurses’ burnout.
In our study, self-efficacy and social support were identified as the significant mediators of the relationship between stress and burnout among ICNs, where burnout increased with decreasing self-efficacy and social support. In a study on burnout among emergency department nurses, self-efficacy and social support were significantly correlated with burnout alleviation, while self-efficacy was a key predictor of burnout [13]; this is consistent with our findings. A study on clinical nurses’ burnout found that self-efficacy and social support were moderators that reduced the negative impact of burnout [18]. Furthermore, burnout increased with decreasing social support among ICU nurses providing care for patients with COVID-19 [16] and among floor nurses [14], while social support was identified as a predictor of burnout in other studies [14, 16], supporting our findings.
Self-efficacy refers to an individual’s expectation or belief that they can successfully carry out appropriate actions in a given situation [19]. Having self-efficacy allows nurses to believe that they can overcome the stressors and adversities prevalent in a clinical setting [33]. Nurses with high self-efficacy demonstrate better professional nursing performance, provide high-quality care, and enhance organizational performance [18]. Furthermore, self-efficacy allows nurses to believe that they have the necessary nursing competence [33]. Thus, self-efficacy is the most important competency for ICNs because they have many responsibilities and high work autonomy [8]. As shown in the present study, ICNs frequently experience high levels of stress and burnout during infection control activities [10], while self-efficacy moderates stress symptoms and burnout [18]. Thus, organizations should develop and implement programs to strengthen self-efficacy to alleviate stress and burnout among ICNs.
Social support refers to the positive support and resources individuals derive from interpersonal relationships, including various forms of mental and material assistance as well as positive resources provided by family members, friends, colleagues, and their superiors [18, 21]. Nurses with high levels of social support have reduced stress [34]; as such, support has a positive impact on their mental health and provides them with the strength to overcome the extreme challenges presented by an infectious disease outbreak, thus alleviating burnout [15]. As nurses are highly dependent on one another in their work processes and frequently bond with one another, support from co-workers enhances work performance, while increased support from their superiors facilitates psychological adjustment and reduces stress and tension, thereby decreasing burnout [13]. As COVID-19 personnel, ICNs received tremendous social attention and encouragement during the pandemic while serving in the frontline against the pandemic, which bolstered their camaraderie and bonds [17].
In the present study, we confirmed that social support, which helps individuals overcome crises, is a critical factor in reducing burnout among ICNs. Thus, to reduce burnout among ICNs, it is important to implement intervention strategies that enhance social support and establish social and organizational support systems, such as fostering a supportive work environment in which nurses feel they can receive adequate support from their colleagues and superiors.
Conclusion
This study revealed the mediating effects of self-efficacy and social support on the relationship between stress and burnout among ICNs in healthcare facilities during an emerging infectious disease pandemic—specifically, the COVID-19 pandemic—based on Lazarus & Folkman’s [24] stress, appraisal-coping model. Our results indicate that stress has a direct effect on burnout and that self-efficacy and social support mediate this effect. To mitigate burnout among ICNs, it is important to alleviate their stress and increase their self-efficacy and social support. This requires the development and implementation of stress reduction and self-efficacy programs at the organizational level, and the development of support systems for a supportive work environment. There is also a need for universalized policy support for social connections and psychological functioning for infection control nurses.
Limitations
As ICNs in healthcare facilities were purposively sampled during an emerging infectious disease pandemic in South Korea, this study’s findings have limited generalizability. Thus, future studies should examine burnout in different regions and hospital types. Based on these results, we recommend that qualitative studies be conducted for an in-depth exploration of the predictors of burnout among ICNs during an emerging infectious disease crisis. Furthermore, we recommend conducting interventional studies to develop and evaluate the effects of nursing intervention programs that reduce stress and improve self-efficacy and social support in order to reduce burnout among ICNs.
Data availability
The datasets during and / or analyzed during the current study available from the corresponding author on reasonable request.
References
World Health Organization. WHO Director-General’s opening remarks at the media briefing – 5. May 2023. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing---5-may-2023 (2023). Accessed 8 Jan 2024.
He X, Hong W, Pan X, Lu G, Wei X. SARS-CoV-2 Omicron variant: characteristics and prevention. MedComm. 2021;2:838–45.
Cho HJ, Lee HI, Lee SW. Patterns of infectious disease in the future according to major environmental changes. Public Health Weekly Report. Korea Disease Control and Prevention Agency. 2017;10:1024-28. https://www.bioin.or.kr/board.do?num=273712&cmd=view&bid=policy&cPage=5&cate1=all&cate2=all2&s_key=title&s_str=%EA%B0%90%EC%97%BC%EB%B3%91. Accessed Jan 08, 2024.
Jeon SH, Lee MH, Choi MJ. COVID-19 infection control-related fatigue, job stress, and burnout in nurses. J Korean Acad Soc Home Care Nurs. 2021;28:16–25.
Choi JS. Changes of the core competency of infection control nurses in accordance with the New Law supporting infection Control Manpower. Korean J Healthc Assoc Infect Control Prev. 2019;24:35–42.
Cha KS, Shin MJ, Lee JY, Chun HK. The role of infection control nurse during emerging infection disease epidemic: focusing on the middle east respiratory syndrome. Korean J Health Assoc Infect Control Prev. 2017;23(1):31–41.
Kim AR, Park LH, Park ES, Kim JH, Kang SR, Jeong JS, et al. Exploring the experiences of nurse managers during the COVID-19 pandemic. J Korean Acad Nurs Adm. 2022;28:460.
Cha KS, Lee HS. Relationships between job satisfaction, resilience and job stress among infection control nurses. Korean Soc Muscle Joint Health. 2019;26:251–60.
Tomaszewska K, Majchrowicz B, Snarska K, Telega D. Stress and occupational burnout of nurses working with COVID-19 patients. Int J Environ Res Public Health. 2022;19:12688.
Lee MR. Infection control compliance, job stress and burnout of nurses in the COVID-19 pandemic. J Korea Acad Ind Coop Soc. 2022;23:648–57.
Maslach C, Jackson SE. The measurement of experienced burnout. J Organ Behav. 1981;2:99–113.
Bae JY, Lee EK, Kim BJ, Lee EJ. The influencing factors of burnout in nurses in the COVID-19 pandemic disaster. Stress. 2021;29(2):80–6.
Kim MR, Seo EJ, Shin SH. The influence of the emotional labor, professional self-concept, self-efficacy and social support of emergency room nurse’s burnout. STRESS. 2019;27:404–11.
Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: a systematic review and meta‐analysis. J Adv Nurs. 2021;77:3286–302.
Kang HJ, Lee MH, Im HN, Lee KH. Influence of infection control fatigue and social support on nurses’ burnout during the coronavirus disease 2019 pandemic. J Korean Clin Nurs Res. 2022;28:299–307.
Park JW, Cha CY. Factors influencing burnout among intensive care unit nurses caring for COVID-19 patients. J Korean Data Anal Soc. 2023;25:813–26.
Shin MY, Chung WJ. Effects of job stress, social support, and infection control fatigue on professional quality of life among nurses in designated COVID-19 hospitals. J Korean Acad Nurs Adm. 2023;29:603–13.
Song JS, Heo SY. Moderating effects of self-efficacy and social support on the relationship between resilience and burnout: focusing on nurses’ experiences. Health Soc Welf Rev. 2018;38:544–70.
Bandura A. Self-efficacy: the exercise of control. New York: Freeman and Company; 1977.
Kim YH, Song YS. Organizational culture for infection control and practice of standard precaution in veterans hospital nurses: the mediating effect of self-efficacy. J Health Info Stat. 2021;46:124–30.
Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress. J Appl Soc Psychol. 1983;13:99–125.
Lee MH, Park YI. A path analysis for burnout and intent to stay for infection control nurses. J Korean Clin Nurs Res. 2015;21:1–10.
Cha KS, Shin MJ, Lee JY, Chun HK. The role of infection control nurse during emerging infectious disease epidemic: focusing on the Middle East Respiratory Syndrome. Korean J Healthc Assoc Infect Control Prev. 2017;22:31–41.
Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984.
Kwon JH, Hong GRS. Influence of self-care on burnout in primary family caregiver of person with dementia. J Korean Acad Nurs. 2021;51:217–31.
Kim SH, Lee J, Jang M. Factors affecting clinical practicum stress of nursing students: using the Lazarus and Folkman’s stress-coping model. J Korean Acad Nurs. 2019;49:437–48.
Kim H, Kim D, Kim M, Kim Y, Bang S, Lee G, et al. Factors influencing burnout of nurses working in a hospital nationally designated for COVID-19 patients. Korean J Adult Nurs. 2022;34:74–84.
June KJ, Choi ES. Reliability and validity of the Korean version of the Copenhagen psycho-social questionnaire scale. Korean J Occup Health Nurs. 2013;22:1–12.
Pejtersen JH, Kristensen TS, Borg V, Bjorner JB. The second version of the Copenhagen Psychosocial Questionnaire. Scand J Public Health. 2010;38:8–24.
Curran PJ, West SG, Finch JF. The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychol Methods. 1996;1:16–29.
Baik DW, Yom YH. Effects of social support and emotional intelligence in the relationship between emotional labor and burnout among clinical nurses. J Korean Aca Nurs Adm. 2012;18:271–80.
Grzelak L, Szwarc P. Wpływ pracy w czasie pandemii COVID-19 na Stres Personelu pielęgniarskiego. Innow Pielęgniarstwie Nauk Zdr. 2021;6–1:7–21.
Kim SJ, Yoon SY, Lee BR, Hong JH, Hwang DY, Yoo SK et al. Concept analysis of clinical nurses’ self-efficacy. J Soc Digit Policy Manag. 2023;2:25–32. https://www.earticle.net/Article/A435770. Accessed 8 Jan 2023.
Kim JY. Nurses’ experience of Middle East Respiratory Syndrome patients’ care. J Korea Acad Ind Coop Soc. 2017;18:185–96.
Acknowledgements
I would like to thank all participants who participated in this study.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (No. RS-2022-00165644).
Author information
Authors and Affiliations
Contributions
Conceptualization, Data curation, Formal analysis, Funding acquisition, Project administration and Supervision: S-JL. Investigation, Methodology, Resources, Software, Validation, Visualization, Writing-original draft and Writing-review & editing: S-JL, S-HK, J-YP. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board at the authors’ institution Kunsan College of Nursing (IRB NO: KCN-2023-0901-02-2) and was conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lee, Sj., Park, JY. & Kim, SH. Effects of stress on burnout among infection control nurses during the COVID-19 pandemic: the mediating effects of social support and self-efficacy. BMC Nurs 23, 537 (2024). https://doi.org/10.1186/s12912-024-02209-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12912-024-02209-z