Abstract
Background
Chronic pain and depression are frequent comorbidities in primary care. Depression among other psychosocial factors play a role in the clinical course of chronic pain.
Objective
To study the short and long-term predictive factors of severity and interference of chronic pain in primary care patients with chronic musculoskeletal pain and major depression.
Methods
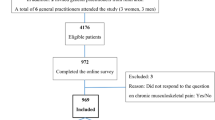
Longitudinal study of a cohort of 317 patients. The outcomes are severity and functional interference of pain (Brief Pain Inventory) measured at 3 and 12 months. We performed multivariate linear regression models to estimate the effects the explanatory baseline variables on the outcomes.
Results
83% participants were women; average age was 60.3 years (SD = 10.2). In multivariate models, baseline pain severity predicted pain severity at 3 months (β = 0.53; 95% CI = 0.37–0.68) and at 12 months (β = 0.48; 95% CI = 0.29–0.67). Also, pain > 2 years of evolution predicted long term pain severity (β = 0.91; CI95%=0.11–1.71). Baseline pain interference predicted interference at 3 and 12 months (β = 0.27; 95%CI = 0.11–0.43 and β = 0.21; 95%CI = 0.03–0.40, respectively). Baseline pain severity predicted interference at 3 and 12 months (β = 0.26; 95%CI = 0.10–0.42 and β = 0.20; 95%CI = 0.02–0.39, respectively). Pain > 2 years predicted greater severity and greater interference at 12 months (β = 0.91; CI95%=0.11–1.71, and β = 1.23; CI95%=0.41–2.04). Depression severity predicted more interference at 12 months (β = 0.58; CI95%=0.04–1.11). Occupational status as active worker predicted less interference throughout the follow-up (β=-0.74; CI95%=-1.36 to -0.13 and β=-0.96; CI95%=-1.71 to -0.21, at 3 and 12 months). Currently working also predicts less pain severity at 12 months (β=-0.77; CI95%=1.52 − 0.02). With regard to the psychological variables, pain catastrophizing predicted pain severity and interference at three months (β = 0.03; 95% CI = 0.00-0.05 and β = 0.03; 95% CI = 0.00-0.05), but not at long term.
Conclusion
In a sample of adults with chronic pain and depression, this primary care study has identified prognostic factors that independently predict the severity and functional interference of pain. If confirmed in new studies, these factors should be targeted for individualized interventions.
Trial registration
ClinicalTrials.gov (NCT02605278), registered 16/11/2015.
Similar content being viewed by others
Introduction
Musculoskeletal pain is one of the main causes of disability globally. It is estimated that chronic low back pain caused over 146 million disability-adjusted life years (DALYs) globally in 2013. Major depression was the second cause in this list, with 51 million DALYs. Other musculoskeletal conditions also in the top 10 causes of disability are chronic cervical pain and osteoarthritis [1]. The sustained upward trend of musculoskeletal pain from 1990 is expected to continue due to increasing life expectancy, elderly population, sedentary lifestyle and obesity [2], with a significant burden of suffering and disability in patients and important repercussions in the health systems and society [3, 4]. Chronic pain of musculoskeletal origin causes a third of all primary care consultations [5], and represents the main cause of disability [6].
In primary care, chronic pain and depression commonly present as comorbidities [7]. The relationship between chronic pain and depression is complex, it involves pathophysiological mechanisms and determines clinical expression. Moreover, it influences prognosis and response to treatment; that is to say, pain exacerbates the clinical course of depression and depression interferes in the management and response to pain treatment [8]. Research has shown that psycholosocial factors have a significant role in the adjustment to and coping with chronic pain. For example, there is mounting evidence showing that cognitive factors such as catastrophic thinking [9] and patients’ attitudes and beliefs towards pain are key to understand the severity and interference of chronic pain [10]. Most of this research has been conducted in individuals with chronic back pain in hospitals or occupational settings [11, 12]. It remains to be seen if the findings are also valid for patients in diverse locations (e.g., primary care facilities) were the caseload of patients and their characteristics will be different. A recent meta-analysis of studies on prognostic factors for musculoskeletal pain reported on the clinical importance of generic factors, not specific to a single anatomical location [13]. In primary care settings, widespread pain, that is, pain in multiple body areas, is more common than single pain [14]. In a previous study from our group, we already analyzed the associations between psychological variables and pain, with the limitation that it was a cross-sectional study [15]. Here, we go one step further and evaluate the predictive power of these variables on pain prognosis with a longitudinal study. Thus, the objective of this prospective study is to build on the body of knowledge on the predictors of pain in primary care patients, with the distinctive contribution of analyzing a sample of patients with comorbidity of chronic pain and depression. Increase our understanding of the implications of this frequent comorbidity [7] and the factors associated with the prognosis of musculoskeletal pain could help to improve the management of musculoskeletal conditions in these patients, and the design of new and better treatments [16] that address potentially modifiable factors [17].
Methods
Objective
To analyse which factors independently predict the severity and interference of short- and long-term chronic pain (3 and 12 months, respectively) in patients with chronic musculoskeletal pain and major depression in the primary care setting.
Design
This study consists of a secondary analysis of the data from the DROP (DepRessiOn and Pain) study, a primary care clinical trial that evaluated a program for the integrated management of chronic pain and major depression in adults. The design and development of the DROP study has been detailed in previous publications [18, 19]. The protocol has been approved by the Institut d’Investigació en Atenció Primària (IDIAP) Jordi Gol Clinical Research Ethics Committee (P14/142) and is registered at ClinicalTrials.gov (NCT02605278).
In summary, it was a randomized clinical trial to investigate the effectiveness of a collaborative care model to improve the primary care clinical management of adult patients with chronic musculoskeletal pain and comorbid depression. The intervention included various components: (1) optimized management of depression using electronic clinical guidelines integrated into the primary care electronic medical records system; (2) a care manager that assisted the family doctors during patient monitoring and follow-up, and also accompanied the patients with follow-up and support by means of scheduled telephone calls; and (3) a group psychoeducational programme directed by the care manager that helped patients better understand their health and encouraged them to play an active role in the management of their pain, depression and associated difficulties. After 12 months, results showed that the programme improved depression compared to regular management, but no clinical benefits in pain outcomes were observed [19].
Setting and participants
Participants were recruited from patient lists of 41 family physicians from primary care centres in the province of Tarragona (Catalonia, Spain). Inclusion criteria were as follows: age between 18 and 80 years; diagnosis of moderate or severe chronic musculoskeletal pain (Brief Pain Inventory pain severity scale ≥ 5 points) lasting over three months –according to a standard definition of chronic pain– [20], despite pain treatment; and meeting the diagnostic criteria of major depression at the time of inclusion (DSM-5 codes F32 or F33), ascertained by means of the major depression module of the SCID [21]. Exclusion criteria were any physical or mental limitation, or any comorbidity preventing participation in study evaluations (e.g., conditions such as severe deafness, cognitive impairment, intellectual disability, or serious physical illness), inability in Catalan and/or Spanish language, patients with a recorded diagnostic in his or her medical history of bipolar or somatization disorder, psychosis, fibromyalgia, alcohol or drug dependence, patients pregnant or breastfeeding, patients with an unresolved claim for occupational disability, and patients with a scheduled intervention for a prosthetic joint during the follow-up period.
Measurements
The evaluations were conducted by an independent interviewer who administered in person a set of standardized questionnaires in the baseline assessment. Subsequently, the patients were monitored with telephone interviews during one year. In this study, we analyse the 3 and 12 month outcomes.
Outcomes: pain interference and severity
We used the 15-item version of the Brief Pain Inventory (BPI) to evaluate pain interference and severity [22, 23]. Pain severity is measured in several domains (worst pain, least pain, pain on average, and pain right now), using numerical scales from 0 (“no pain”) to 10 points (“worst pain”). The severity value is obtained from the average of the four domains. Interference is measured by scales from 0 (“no interference”) to 10 points (“total interference”) in seven areas of life: general activity, mood, walking, normal work, relationships, sleep, and enjoyment of life. The score on the interference scale is obtained by averaging the seven domains.
Baseline explanatory variables
Sociodemographic information
sex, age, marital status (single, married or living with a partner, divorced or separated, and widow or widower; dichotomized as living with a partner versus the other options), educational level (no formal education, primary school, lower secondary school, upper secondary school, and university; dichotomized as secondary or higher education versus the other options) and occupational situation (active, unemployed, permanent work disability, retired, and household chores; then dichotomized as current active working versus the other options).
Depression
Severity of depression was measured with the Hopkins Symptom Checklist, (HSCL-20) [24, 25], where the items investigate depressive symptoms scored on a Likert scale with five options, from 0 (“not at all”) to 4 (“extremely”). The overall score is the average of the 20 items. The medical history was checked for prior episodes of depression, and the duration of the current depressive episode was determined.
Pain characteristics
location (spine, limbs or both) and duration.
Catastrophic thinking
We used the Pain Catastrophizing Scale (PCS) [26, 27] to evaluate catastrophic thoughts related to pain. Catastrophizing is characterized by the perception of the painful stimulus as a threat, by the feeling of helplessness, and by being unable to avoid recurring thoughts related to pain. The PCS consists of 13 items scored on a Likert scale with 5 possible answers, from 0 (“this never happens to me”) to 4 (“it always happens to me”). The total score is the sum of the scores on all the items, and ranges between 0 and 52 points. The higher the scores, the greater the pain catastrophizing.
Attitudes towards pain
Beliefs or attitudes toward pain were measured with the Survey of Pain Attitudes (SOPA) [28, 29], which consists of 35 items with 5 answer options, from 0 (= totally false) to 4 (= totally true). The SOPA questionnaire investigates 7 dimensions: (1) control : to which extent the patient believes they can control their pain; (2) emotion: the patient believes that her or his emotions affect her or his experience of pain; (3) disability: the patient considers pain as a cause of disability; (4) harm: the patient beliefs that pain is a sign of physical injury and thus she or he should avoid exercise; (5) drugs: the patient beliefs that the pharmacological treatment is appropriate and effective for her or his pain; (6) solicitude: the extent to which the patient believes that others should be concerned for her or his pain; and (7) medical care: the patient believes that the physician is responsible for curing or improving her or his pain. Scores for each dimension, ranging from 0 to 4, were created by averaging item responses for each dimension, taking into account that some items have a reverse scoring.
Physical comorbidity
measured with the Duke Severity of Illness Checklist (DUSOI) [30, 31]. For each diagnosis, a score is assigned to the symptoms, complications, prognosis, and expected response to treatment. The overall severity of the patient is assessed on a scale of 0 to 100.
Comorbid anxiety
evaluated using the anxiety section of the Primary Care Evaluation of Mental Disorders (PRIME-MD). This section includes three screening yes/no questions. If one of the answers is yes, the full diagnostic module must be applied. It consists of a structured interview that assesses panic disorder and generalized anxiety disorder diagnostic criteria [32, 33].
Statistical analysis
We performed a descriptive analysis of the sample characteristics calculating means and standard deviations for continuous variables and percentages for categorical variables. To study the associations between the variables we calculated the baseline Spearman’s correlation coefficients.
The outcomes of the study were pain severity and pain interference, measured at 3 (short-term) and 12 months (long-term). We performed a bivariate linear regression to estimate the effects of each of the potentially explanatory baseline variables on the outcomes. The variables with p < 0.05 in the first analyses were then selected for the multivariate linear regression models. Only cases with complete data were considered in these analyses and no imputation methods of missing data were used.
Since we wanted to avoid any possible effect of the original clinical trial on the results, we included “study arm” as an adjustment variable in all multivariate models. A p value < 0.05 determined statistical significance. The statistical package R was used for all analyses.
Results
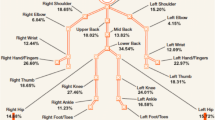
The sample consisted of 317 patients, of which 272 (83%) were women and the average age was 60.3 years (SD = 10.2). Average pain severity was 6.52 (SD = 1.82) and the average functional impact was 6.35 (SD = 2.31), considering a score ≥ 7 as the cutting point between moderate and severe pain in both subscales. Most patients (84%) reported pain lasting over two years. Depression was chronic (> 2 years) in over half of the patients (58%), and the average severity was 1.68 points (SD = 0.74) (in the HSCL-20, the cutting point between moderate and severe depression is > 1.7) (Table 1).
Of the 317 patients assessed at baseline, 305 were assessed at 3 months (4% dropout rate), and 274 at 12 months (14% dropout rate). As there were no differences between the patients who dropped out and those who remained in terms of age, gender, work condition, severity or pain interference, depression severity, or psychiatric or physical comorbidity, the patients who dropped out are considered to have done at random (Table A1, supplementary files).
When we analysed the correlation coefficients at baseline, we found linear relationships ranging from negligible to moderate. No strong correlations were found between the variables (Table A2, Supplementary files).
Throughout the follow-up, we observed great stability in the clinical expression of chronic pain, both in the severity of the pain and in the associated interference (Table 2).
Bivariate analysis. Factors associated with pain severity and interference at 3 and 12 months
Table 3 shows the associations between baseline characteristics and pain severity at 3 and 12 months. Pain severity and interference at baseline, pain lasting over 2 years, and aspects related to psychiatric comorbidity were associated with greater pain severity at 3 and 12 months. Male gender and living with a partner were associated with lower severity of pain at three months. A higher educational level was associated with lower severity of pain at 3 and 12 months. Working predicted a better result at 12 months.
Table 4 shows that both severity and interference at baseline are associated with pain interference at 3 and 12 months. The baseline severity of depression and anxiety disorders as comorbidities are associated with greater interference at 3 and 12 months. Health-related quality of life at baseline was associated with less interference at 3 and 12 months. Working was associated with less interference throughout.
We analysed the associations of various psychological variables with outcomes (Tables 2 and 3). Catastrophizing was associated with both variables at 3 and 12 months. Some dimensions of SOPA show significant associations at 3 and 12 months.
As expected, since the original clinical trial did not show improvement on the evolution of pain, the arm of the clinical trial where the patient was allocated was not associated with any pain outcome during follow-up.
In linear regression models, baseline pain severity predicted greater pain severity at 3 and 12 months. Pain lasting over two years predicted greater long term severity. Actively working predicted less pain severity at 12 months (Table 5).
Table 6 shows the results with interference as outcome. Both baseline pain severity and interference predicted interference at 3 and 12 months. Pain lasting over two years and baseline severity of depression predicted a greater interference at 12 months. Actively working predicted less interference throughout the follow-up.
Regarding the role of psychological variables as prognostic factors, we identified catastrophizing as a predictor of pain severity and interference at three months, but not long term (Tables 5 and 6). The SOPA domain ‘disability’ is associated with greater interference at 3 months. Our models did not identify any other attitudes and beliefs about pain measured by SOPA as predictive factors.
Discussion
The objective of this primary care study is to analyse independent factors able to predict the severity and interference of short- and long-term chronic pain in patients with chronic musculoskeletal pain and major depression. We have identified various modifiable and non-modifiable factors associated with clinical pain outcomes. We have observed that the baseline severity and interference of pain is predictive of the short and long-term evolution of pain. Our results in patients with chronic pain and depression agree with the results of a recent meta-analysis [13] on the evolution of musculoskeletal pain in the primary care setting. This work also identified the severity and interference of baseline pain as prognostic factors in the evolution of pain. This meta-analysis also reports that generalized pain or pain in multiple locations might be a negative predictive factor. Although we did not identify this factor in our analyses, we note that in our study 90% of patients experienced pain at multiple sites.
In our study, working at baseline was identified as an independent predictor of a lesser interference of short- and long-term pain. This result must be interpreted cautiously because it is possible that patients with higher pain interference, and with a worse prognosis, had stopped working for this reason before the baseline assessment. Moreover, the interrelationship between occupational status and disability associated with chronic pain are complex and influenced by other clinical and socioeconomic factors [34, 35]. Studies have often reported a longitudinal association between not working with adverse pain outcomes [36, 37]. As suggested by other researchers [38], our results could align with the hypothesis that promoting job reinstatement in patients with chronic pain may benefit them.
Except for an isolated result in which baseline depression severity is independently associated with less long-term interference, our study does not confirm psychiatric comorbidities as predictive factors, although in previous studies they are emphasized as prognostic factors in the evolution of pain [39, 40]. The widespread presence of psychological pathology in our sample, where all patients have depression and the vast majority have anxiety disorders, may have prevented a more clear observation of a possible predictive effect of psychological variables in the course of pain.
Regarding cognitive variables, catastrophizing was associated with worse short-term outcomes, while personal attitudes or beliefs toward pain could not be considered independent predictors of pain severity and interference. Catastrophizing is a cognitive response to pain that amplifies feelings of pain, rumination, obsessive worrying and helplessness regarding our ability to cope with and manage our own pain [41]. While the literature regarding catastrophic thinking as a prognostic factor is controversial, it is usually associated with a worse evolution of pain [9, 42, 43]. Moreover, although catastrophizing correlates closely with depression, it has a specific and additive deleterious effect on the evolution of pain [43]. In contrast, a multicentre study to analyse the prognostic value of catastrophizing in a large sample of patients with low back pain in Spain concluded that catastrophizing at baseline did not predict the evolution of pain or associated disability [44]. However, since catastrophizing is potentially modifiable, our results strengthens the hypothesis that interventions to decrease catastrophizing could improve the prognosis of chronic pain [45], at least in the short term. However, this improvement has not always been confirmed in clinical trials [46].
In agreement with published research [47], our previous cross-sectional analysis [14] suggested that patients’ adaptive or maladaptive attitudes and beliefs toward pain could play a prognostic role in pain progression. The interest of this hypothesis lies in the possibility of modifying maladaptive beliefs and enhancing adaptive beliefs through psychological interventions [48]. However, our longitudinal results have not confirmed this hypothesis, beyond having identified the predictive value of the SOPA ‘disability’ subscale in short-term interference.
This study has potential limitations. Firstly, before interpreting the results, we should understand the characteristics of participants. A study by Meisingset et al. [49] concluded that the phenotype of patients with musculoskeletal pain characterized by intense, generalized pain, with significant long-term functional interference and psychological distress (characteristics of the majority of our patients) presented a worse evolution and lower response to interventions. In addition, the sample was recruited from a limited number of primary care centres from a specific area. All these factors can hinder the extrapolation of our results to patients with chronic musculoskeletal pain in other levels of care and from other geographical areas. Secondly, although current objectives are consistent and complementary with the original clinical trial, these conclusions originate from a secondary analysis of data collected for different purposes.
Implications
Despite these limitations, our results provide valuable information on independent factors that predict pain severity and functional interference in a sample of primary care patients with chronic pain and depression. We have identified prognostic factors potentially modifiable with multifactorial interventions, such as catastrophic thinking and occupational status. It is also important to understand the non-modifiable prognostic factors, such as the baseline clinical status or previous evolution, to personalise management and avoid unrealistic expectations. Further studies should confirm the hypothesis that the modification of predictive factors translates into better pain outcomes.
Data Availability
The datasets generated and analysed for this study are not publicity available due to privacy and ethical concerns but are available from the corresponding author on reasonable request.
Abbreviations
- BPI:
-
Brief Pain Inventory
- DSM-5:
-
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
- DALY:
-
Disability adjusted life years
- DROP:
-
Depression and Pain Project
- DUSOI:
-
Duke Severity of Illness Checklist
- HSCL-20:
-
Hopkins Symptom Checklist 20 items
- IDIAP Jordi Gol:
-
Primary Care Research Institute Jordi Gol (in Catalan Institut d’Investigació en Atenció Primària Jordi Gol)
- PCS:
-
Pain Catastrophizing Scale
- PRIME-MD:
-
Primary Care Evaluation of Mental Disorders
- SOPA:
-
Survey of Pain Attitudes
References
Rice ASC, Smith BH, Blyth FM. Pain and the global burden of disease. Pain. 2016;157(4):791–6.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22.
Breivik H, Eisenberg E, O’Brien T, OPENMinds. The individual and societal burden of chronic pain in Europe: the case for strategic prioritisation and action to improve knowledge and availability of appropriate care. BMC Public Health. 2013;13:1229.
Alonso-García M, Sarría-Santamera A. The Economic and Social Burden of Low Back Pain in Spain: A National Assessment of the Economic and Social Impact of Low Back Pain in Spain. Spine (Phila Pa 1976). 2020;45(16):E1026–32.
Finley CR, Chan DS, Garrison S, Korownyk C, Kolber MR, Campbell S, et al. What are the most common conditions in primary care? Systematic review. Can Fam Physician. 2018;64(11):832–40.
Fernández A, Saameño JA, Pinto-Meza A, Luciano JV, Autonell J, Palao D, et al. Burden of chronic physical conditions and mental disorders in primary care. Br J Psychiatry. 2010;196(4):302–9.
Means-Christensen AJ, Roy-Byrne PP, Sherbourne CD, Craske MG, Stein MB. Relationships among pain, anxiety, and depression in primary care. Depress Anxiety. 2008;25(7):593–600.
Kroenke K, Wu J, Bair MJ, Krebs EE, Damush TM, Tu W. Reciprocal relationship between pain and depression: a 12-month longitudinal analysis in primary care. J Pain. 2011;12(9):964–73.
Wertli MM, Eugster R, Held U, Steurer J, Kofmehl R, Weiser S. Catastrophizing-a prognostic factor for outcome in patients with low back pain: a systematic review. Spine J. 2014;14(11):2639–57.
Miró J, Queral R, Nolla MC. Pain-related attitudes and functioning in elderly primary care patients. Span J Psychol. 2015;17:E104.
Alhowimel AS, Alotaibi MA, Alenazi AM, Alqahtani BA, Alshehri MA, Alamam D, et al. Psychosocial Predictors of Pain and disability outcomes in people with chronic low back Pain treated conservatively by Guideline-Based intervention: a systematic review. J Multidiscip Healthc. 2021;14:3549–59.
Buruck G, Tomaschek A, Wendsche J, Ochsmann E, Dörfel D. Psychosocial areas of worklife and chronic low back pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2019;20(1):480.
Artus M, Campbell P, Mallen CD, Dunn KM, van der Windt DA. Generic prognostic factors for musculoskeletal pain in primary care: a systematic review. BMJ Open. 2017;7(1):e012901.
Carnes D, Parsons S, Ashby D, Breen A, Foster NE, Pincus T, et al. Chronic musculoskeletal pain rarely presents in a single body site: results from a UK population study. Rheumatology (Oxford). 2007;46(7):1168–70.
Sánchez-Rodríguez E, Aragonès E, Jensen MP, Tomé-Pires C, Rambla C, López-Cortacans G, et al. The Role of Pain-Related Cognitions in the Relationship between Pain Severity, Depression, and Pain Interference in a sample of primary care patients with both Chronic Pain and Depression. Pain Med. 2020;21(10):2200–11.
Moons KG, Royston P, Vergouwe Y, Grobbee DE, Altman DG. Prognosis and prognostic research: what, why, and how? BMJ. 2009;338:b375.
Hill JC, Whitehurst DG, Lewis M, Bryan S, Dunn KM, Foster NE, et al. Comparison of stratified primary care management for low back pain with current best practice (STarTBack): a randomised controlled trial. Lancet. 2011;378:1560–71.
Aragonès E, López-Cortacans G, Caballero A, Piñol JL, Sánchez-Rodríguez E, Rambla C, et al. Evaluation of a multicomponent programme for the management of musculoskeletal pain and depression in primary care: a cluster-randomised clinical trial (the DROP study). BMC Psychiatry. 2016;16:69.
Aragonès E, Rambla C, López-Cortacans G, Tomé-Pires C, Sánchez-Rodríguez E, Caballero A, et al. Effectiveness of a collaborative care intervention for managing major depression and chronic musculoskeletal pain in primary care: a cluster-randomised controlled trial. J Affect Disord. 2019;252:221–9.
Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. A classification of chronic pain for ICD-11. Pain. 2015;156:1003–7.
First MB. Structured Clinical Interview for the DSM (SCID). The encyclopedia of clinical psychology. Hoboken, NJ, USA:Wiley, 2015.pp. 1–6
Cleeland C. The brief Pain Inventory: user guide. MD Anderson Cancer Center: Houston;; 2009.
Badia X, Muriel C, Gracia A, Núñez-Olarte JM, Perulero N, Gálvez R, et al. Validation of the spanish version of the brief Pain Inventory in patients with oncological pain. Med Clin (Barc). 2003;120:52–9.
Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci. 1974;19:1–15.
Williams JW Jr, Stellato CP, Cornell J, Barrett JE. The 13- and 20-item Hopkins Symptom Checklist Depression Scale: psychometric properties in primary care patients with minor depression or dysthymia. Int J Psychiatry Med. 2004;34:37–50.
Sullivan MJ, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Asses. 1995;7:524–32.
García-Campayo J, Rodero B, Alda M, Sobradiel N, Montero J, Moreno S. Validación de la versión española de la escala de la catastrofización ante el dolor (Pain Catastrophizing Scale) para la evaluación de la catastrofización en la fibromialgia. Med Clin (Barc). 2008;131:487–92.
Jensen MP, Karoly P, Huger R. The development and preliminary validation of an instrument to assess patients’ attitudes toward pain. J Psychosom Res. 1987;31:393–400.
Molinari G, del Río-González E, González-Robles A, Herrero-Camarano R, Botella-Arbona C. Spanish version of the Survey of Pain Attitudes (SOPA-B) in patients with fibromyalgia. Àgora Salut. 1989;1:151–62.
Parkerson GR Jr, Broadhead WE, Tse CK. The Duke Severity of Illness Checklist (DUSOI) for measurement of severity and comorbidity. J Clin Epidemiol. 1993;46:379–93.
Martínez C, Juncosa S, Roset M. ¿Está relacionada la gravedad con la utilización de recursos? Una exploración del Duke Severity of Illness Scale (DUSOI). Aten Primaria. 1998;22:285–92.
Spitzer RL, Williams JB, Kroenke K, Linzer M, deGruy SR 3 et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA. 1994;272:1749–56.
Baca E, Saiz J, Aguera L, Caballero L, Fernandez-Liria A, Ramos J, et al. Validation of the spanish version of PRIME-MD: a procedure for diagnosing mental disorders in primary care. Actas Esp Psiquiatr. 1999;27:375–83.
Teasell RW, Bombardier C. Employment-related factors in chronic pain and chronic pain disability. Clin J Pain. 2001 Dec;17(4 Suppl):39–45.
Kuijer W, Brouwer S, Preuper HR, Groothoff JW, Geertzen JH, Dijkstra PU. Work status and chronic low back pain: exploring the International classification of Functioning, disability and health. Disabil Rehabil. 2006;28(6):379–88.
Moffett JA, Underwood MR, Gardiner ED. Socioeconomic status predicts functional disability in patients participating in a back pain trial. Disabil Rehabil. 2009;31(10):783–90.
Fliesser M, De Witt Huberts J, Wippert P. Education, job position, income or multidimensional indices? Associations between different socioeconomic status indicators and chronic low back pain in a german sample: a longitudinal field study. BMJ Open. 2018;8:e020207.
Nieminen LK, Pyysalo LM, Kankaanpää MJ. Prognostic factors for pain chronicity in low back pain: a systematic review. Pain Rep. 2021;6(1):e919.
Pinheiro MB, Ferreira ML, Refshauge K, Maher CG, Ordoñana JR, Andrade TB, et al. Symptoms of depression as a prognostic factor for low back pain: a systematic review. Spine J. 2016;16(1):105–16.
Kroenke K, Wu J, Bair MJ, Damush TM, Krebs EE, Tu W. Impact of Depression on 12-Month Outcomes in primary-care patients with Chronic Musculoskeletal Pain. J Musculoskelet Pain. 2012;20(1):8–17.
Quartana PJ, Campbell CM, Edwards RR. Pain catastrophizing: a critical review. Expert Rev Neurother. 2009;9(5):745–58.
Martinez-Calderon J, Jensen MP, Morales-Asencio JM, Luque-Suarez A. Pain catastrophizing and function in individuals with Chronic Musculoskeletal Pain: a systematic review and Meta-analysis. Clin J Pain. 2019;35(3):279–93.
Linton SJ, Nicholas MK, MacDonald S, Boersma K, Bergbom S, Maher C, et al. The role of depression and catastrophizing in musculoskeletal pain. Eur J Pain. 2011;15(4):416–22.
Kovacs FM, Seco J, Royuela A, Corcoll-Reixach J, Peña-Arrebola A, Spanish Back Pain Research Network. The prognostic value of catastrophizing for predicting the clinical evolution of low back pain patients: a study in routine clinical practice within the Spanish National Health Service. Spine J. 2012;12(7):545–55.
Schütze R, Rees C, Smith A, Slater H, Campbell JM, O’Sullivan P. How can we best reduce Pain Catastrophizing in adults with chronic Noncancer Pain? A systematic review and Meta-analysis. J Pain. 2018;19(3):233–56.
Riddle DL, Keefe FJ, Ang DC, Slover J, Jensen MP, Bair MJ, et al. Pain coping skills training for patients who Catastrophize about Pain prior to knee arthroplasty: a Multisite Randomized Clinical Trial. J Bone Joint Surg Am. 2019;101(3):218–27.
Tan G, Teo I, Anderson KO, Jensen MP. Adaptive versus maladaptive coping and beliefs and their relation to chronic pain adjustment. Clin J Pain. 2011;27(9):769–74.
Turk DC, Swanson KS, Tunks ER. Psychological approaches in the treatment of chronic pain patients–when pills, scalpels, and needles are not enough. Can J Psychiatry. 2008;53(4):213–23.
Meisingset I, Vasseljen O, Vøllestad NK, Robinson HS, Woodhouse A, Engebretsen KB, et al. Novel approach towards musculoskeletal phenotypes. Eur J Pain. 2020;24(5):921–32.
Acknowledgements
This study has been possible thanks to the generous collaboration of participating family doctors who form the DROP research group, listed in the Additional file 2.
Funding
This project was primarily funded by a research grant from the Carlos III Health Institute of Spain’s Ministry of the Economy and competitiveness, under Health Strategy Action 2013–2016 [PI14/00,573] with co-funding from the European Regional Development Fund. EA received a grant for intensification of research activity from the Carlos III Institute [INT15/00,232]. JM’s work is supported by grants from the Spanish Ministry of Economy, Industry and Competitiveness (RTI2018-09870-B-I00; RED2018-102546-T; PRE2019-089283), Universitat Rovira i Virgili (PFR program), and ICREA-Acadèmia. The Chair in Pediatric Pain is supported by Fundación Grünenthal. EA and GLC have benefitted from grants for intensification of research activity from the IDIAP Jordi Gol, and CR thanks the IDIAP Jordi Gol a predoctoral grant [7Z16/008, 2015]. The funding bodies have had no role in the design of the study, or in the analysis and interpretation of data or its diffusion.
Author information
Authors and Affiliations
Contributions
EA is the principal investigator and developed the original idea for the study. EA is the guarantor of the study. EA, GLC, CR and JM further developed the study design. MP developed the statistical methods. CR and EA wrote the manuscript. All authors have read and corrected draft versions and have approved the final version.
Corresponding author
Ethics declarations
Competing interests
EA has received honoraria as a speaker or consultant from Lündbeck and Esteve. And all other authors declare that they have no other relationships, interests, or activities that could appear to have influenced the submitted work.
Ethics approval and consent to participate
The procedures of this project adhere to the Guidelines for Best Practices in Primary Care Research (Barcelona: Fundació Jordi Gol, 2010). Informed consent was obtained from all participants. The study protocol was approved by the Clinical Research Ethics Committee of the Institut d’Investigació en Atenció Primària (IDIAP) Jordi Gol (P14/142).
Consent for publication
Not applicable
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rambla, C., Aragonès, E., Pallejà-Millán, M. et al. Short and long-term predictors of pain severity and interference in primary care patients with chronic musculoskeletal pain and depression. BMC Musculoskelet Disord 24, 270 (2023). https://doi.org/10.1186/s12891-023-06357-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06357-2