Abstract
Background
In bicruciate-stabilized total knee arthroplasty (BCS-TKA), the relationship between the postoperative kinematics and sports subscales in patient-reported outcome measures (PROMs) remains unknown. The purpose of this study was to determine the relationship between kinematics and sports subscales using the PROMs after BCS-TKA.
Methods
Sixty-one patients with severe knee osteoarthritis were examined at 13.5 ± 7.8 months after BCS-TKA. The patients performed squats under single fluoroscopic surveillance in the sagittal plane. Range of motion of the knee, axial rotation of the femur relative to the tibial component, and anteroposterior (AP) translation of the medial and lateral femorotibial contact points were measured using a 2D-to-3D registration technique. In addition, the relationship between the kinematics and improvement of the sports subscales in the Knee Injury and Osteoarthritis Outcome Score (KOOS) was evaluated.
Results
In rotation angle, the femoral external rotation was observed from 0 to 50° of flexion. The amount of femoral external rotation did not correlate with PROMs-SP. In medial AP translation, posterior translation was observed from 0 to 20° and 80–110° of flexion. Mild anterior translation was observed from 20 to 80° of flexion. Beyond 80° of flexion, posterior translation was positively correlated with squatting. In lateral AP translation, posterior translation was observed from 0 to 20° and 80–110° of flexion. Beyond 80° of flexion, posterior translation was positively correlated with running, jumping, twisting/pivoting, and kneeling.
Conclusion
Femoral rollback at high flexion during squatting may be important to improve sports performance after BCS-TKA.
Similar content being viewed by others
Background
In bicruciate-stabilized total knee arthroplasty (BCS-TKA), the anterior and posterior cruciate ligaments are substituted, wherein the anatomical implant surface provides physiological kinematics [1]. The Journey II BCS (Smith & Nephew, Memphis, TN, USA) has been redesigned to reduce iliotibial band traction syndrome [2]. The second-generation design is associated with a lower risk of reoperation and revision compared to the first [3]. In addition, BCS-TKA provides acceptable outcomes in terms of activities of daily living (ADL) [1, 4, 5].
Recently, with the improvements in ADL after BCS-TKA, patients have been expected to participate in sports activities. In the Knee Society survey, the number of sports activities allowed after TKA has increased [6]. Furthermore, several studies reported that the return to sports or implant survivorship after TKA is favorable [7,8,9]. In contrast, Huch et al. reported that the prevalence of postoperative athletic activity was higher in the hip replacement group than in the knee replacement group due to greater pain relief in the hip replacement group [6, 10]. Additionally, Mont et al. reported that the failure rate was higher in the younger and highly active patients [9].
High-flexion activities, such as exercising and gardening, have recently been classified as ADL. Thus, many patients who undergo TKA are expected to perform high-flexion activities. However, it is difficult for the patients to squat, and the limited range of motion (ROM) is negatively correlated with patient expectations [11]. Moreover, Matsushita et al. demonstrated that the improvement in ADL was related to high satisfaction or expectation to be able to perform sports activities [12]. Therefore, the evaluation of patients’ ability to perform high-flexion activities is important.
Several studies have demonstrated that the postoperative knee kinematics was related to the patient-reported outcome measures (PROMs) [13,14,15]. Van Onsem et al. reported that the high PROM group had more pronounced posterior translation laterally from 60° to 90° of flexion than the low PROM group [16]. However, the relationship between the postoperative kinematics and sports subscales in PROMs remains unknown.
The objective of the current study was to clarify the relationship between kinematics and sports subscales during high-flexion activities based on the PROMs after BCS-TKA. This study hypothesized that posterior translation with flexion was related to the improvement of PROMs concerning sports (PROMs-SP) after BCS-TKA.
Methods
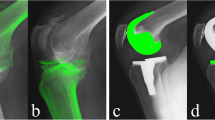
Sixty-one knees with severe medial osteoarthritis that underwent BCS-TKA were examined. Patients who could perform squatting safely at a natural pace after surgery were examined under single fluoroscopy surveillance in the sagittal plane, according to the previously described method [15]. The indication for BCS-TKA was severe osteoarthritis (OA), with the exception of severe valgus OA (hip-knee-ankle angle > 190°).
To estimate the spatial position and orientation of the femoral and tibial components, a 2D-to-3D registration technique was used [17, 18]. The margin of error of the estimated relative motion between the femoral and tibial components is ≤0.5° for rotation and ≤ 0.4° for translation [17]. The following variables were evaluated: knee flexion, axial rotation of the femoral component relative to the tibial component, and anteroposterior (AP) translation of the medial and lateral femorotibial contact points. A local coordinate system at the femoral component was constructed according to previously described methods [17, 19]. Flexion and femoral external rotation were denoted as positive values. Positive or negative values of AP translation were defined as anterior or posterior to the axes of the tibial component, respectively. The femorotibial contact point was defined as the region in which the proximity of the component surfaces was less than 0.5-mm [15]. All data are expressed as means ± standard deviations.
The Knee Injury and Osteoarthritis Outcome Scores (KOOS) [20] were taken preoperatively (within 1 month) and postoperatively (at the fluoroscopic analyses) as part of PROMs. In addition, the relationship between the kinematics and the improvement of PROMs-SP was evaluated.
All patients provided written informed consent for participation. This study was approved by the concerned institutional review board. In addition, all methods were performed in accordance with the relevant guidelines and regulations.
Statistical analyses
To analyze the data, SPSS version 25 (IBM Corp., Armonk, NY, USA), was used. Two-way analysis of variance (ANOVA) and post hoc pairwise comparisons (Bonferroni test) were used to evaluate the axial rotation and AP translation. A paired t-test was used to evaluate the improvement in PROMs-SP. The Spearman rank correlation coefficient was used to evaluate the correlation between kinematics and PROMs-SP. The level of statistical significance was set at p < 0.05. A power analysis was performed with G*Power [21] using an α error of 0.05, and a 1 − β error of 0.80 to compare the means between the two groups; a sample of 44 knees was found to be sufficient for this study.
Results
Fluoroscopic analyses were performed 13.5 ± 7.8 months after surgery. At the time of analysis, the mean age of the patients was 74.8 ± 7.2 years, the mean height was 155.0 ± 7.8 cm, and the mean body weight was 64.6 ± 10.6 kg. Of the 61 knees included in the analysis, 9 belonged to men and 52 belonged to women.
Flexion angle and rotation angle
The knees were gradually flexed from − 2.9 ± 6.4° to 109.5 ± 13.34°. In the rotation angle, the femoral component displayed an external rotation angle of 3.2 ± 3.1° relative to the tibial component from 0° to 50° of flexion. Beyond 50° of flexion, there was no significant movement (Fig. 1).
AP translation
At the medial contact point, the femoral component showed 3.9 ± 2.0 mm of posterior movements from 0°–20° of flexion, followed by 1.8 ± 2.4 mm of anterior movements up to 80° of flexion. Beyond 80° of flexion, the femoral component showed 2.8 ± 1.4 mm posterior movements (Fig. 2).
At the lateral contact point, the femoral component showed 7.7 ± 2.8 mm of posterior movement from 0° –20° of flexion with no significant movement up to 80° of flexion. Beyond 80° of flexion, a posterior movement of 3.5 ± 1.8 mm was observed (Fig. 3).
The improvement of PROMs-SP
As summarized in Table 1, all function, sports, and recreational activities subscales in the KOOS improved postoperatively (p < 0.01).
Correlation between the age or gender, and PROMs-SP
The patients’ age was negatively correlated with running, and male gender was positively correlated with squatting (Table 2).
Correlation between the kinematics and PROMs-SP
In the rotation angle, femoral external rotation was observed from 0°-50° of flexion. The amount of femoral external rotation did not correlate with PROMs-SP (Table 3).
In medial AP translation, posterior translation was observed at 0–20° and 80–110° of flexion. Mild anterior translation was observed from 20 to 80° to flexion. Beyond 80° of flexion, posterior translation was positively correlated with squatting (Table 4).
In lateral AP translation, posterior translation was observed from 0 to 20° and to 80–110° of flexion. Beyond 80° of flexion, posterior translation was positively correlated with running, jumping, twisting/pivoting, and kneeling (Table 5).
Discussion
The most important finding of this study was that the posterior translation at high flexion was correlated with the improvements in PROMs-SP, such as squatting, running, jumping, twisting/pivoting, and kneeling. In normal knees, femoral posterior rollback is observed at high flexion [22, 23]. Kosse et al. demonstrated that sport and quality of life score were better in TKA patients with high maximal flexion (≥125°) [24]. Furthermore, Dennis et al. reported that femoral posterior movement at high flexion increased the flexion angle [25]. In addition, another study reported that the high-PROM group showed posterior femoral movement at high flexion [16]. These facts suggest that it is important to drive the femoral posterior movement at high flexion, similar to normal knees, for satisfactory sports activities after TKA. Kage et al. reported that medial and lateral AP translation did not correlate with improvements in KOOS pain, symptoms, and ADL [13]. Therefore, femoral posterior movement is required, especially during high flexion activities, for sports activities. Several studies have reported that the rate of return to sports (RTS) after TKA was > 70% [8, 26,27,28]. Femoral rollback-guided designs or procedures, such as a post-cam mechanism in posterior stabilized TKA, appropriate cruciate ligament tension in bicruciate-retaining TKA (BCR-TKA), or achievement of an appropriate posterior tibial slope, may improve the RTS rate. In other words, a guided motion TKA such as BCS-TKA or BCR-TKA with appropriate ligament balance might be particularly suitable for patients who are active in sports before the surgery and wish to return to work postoperatively. However, the patient age was negatively correlated with running, and male gender was positively correlated with squatting. The younger patient age may have directly influenced the superior running results, while male patients may find it easier to squat following TKA.
There was no significant correlation between rotation at early flexion and PROMs-SP in the current study. Kage et al. reported that at early flexion, femoral external rotation was positively correlated with improvement of the KOOS pain subscale [13]. These findings suggest that although after TKA, femoral external rotation and pain improves, it may be difficult to improve high flexion activities such as sports.
In this study, a mild femoral external rotation with flexion was observed. This rotational kinematic pattern was similar to that reported in previous studies [1, 13, 15, 29]. One of these previous studies reported that the lower PROM group in BCS-TKA indicated excessive femoral external rotation with flexion [15]. In the current study, the PROMs-SP improved in all subscales. Therefore, after BCS-TKA, excessive femoral external rotation may not be needed to improve sports activities.
The AP translation in this study was similar to that in previous studies [1, 13, 15, 29]. In normal knees, medial pivot motion was observed during early flexion [22]. In other words, no medial posterior translation was observed during early flexion. In contrast, the knees after BCS-TKA showed medial posterior translation during early flexion. Ishibashi et al. reported that medial posterior translation during early flexion was due to anterior post-cam engagement [29]. To achieve normal-like kinematics, further improvement of the post-cam mechanism might be required.
In this study, after BCS-TKA, all sports subscales improved. Vielgut et al. demonstrated that postoperative sports ability was correlated with preoperative activity [30]. Additionally, Ho et al. demonstrated that the RTS rate between TKA and unicompartmental knee arthroplasty did not differ under the same preoperative patient characteristics [31]. Thus, preoperative activity may have influenced the improvement of PROMs-SP.
This study had several limitations. First, in the current study, only squatting was measured. The previous studies reported that knee kinematics differ depending on the type of activities [22, 32]. Therefore, the kinematic effect during other activities might be different from squatting. Second, the squatting motion was measured only one movement repetition per patient because of ethical reasons to reduce patients’ X-ray exposure. Third, the RTS rate was not evaluated after TKA. Therefore, whether the RTS rate correlates with the PROMs-SP is unclear.
Conclusion
Femoral rollback at high flexion during squatting may be important to improve sports performance after BCS-TKA.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request. The data used during the current study could not be deposited because the patients did not approve the permanent availability of data.
Abbreviations
- ADL:
-
Activities of daily living
- ANOVA:
-
Analysis of variance
- AP:
-
Anteroposterior
- BCS-TKA:
-
Bicruciate-stabilized total knee arthroplasty
- DKB:
-
Deep knee bending
- KOOS:
-
Knee Injury and Osteoarthritis Outcome Score
- PROMs:
-
Patient-reported outcome measures
- PROMs-SP:
-
Patient-reported outcome measures concerning sports
- OA:
-
Osteoarthritis
- ROM:
-
Range of motion
- RTS:
-
Return to sports
- TKA:
-
Total knee arthroplasty
- BCR-TKA:
-
Bicruciate-retaining TKA
References
Kono K, Inui H, Tomita T, Yamazaki T, Taketomi S, Sugamoto K, et al. Bicruciate-stabilised total knee arthroplasty provides good functional stability during high-flexion weight-bearing activities. Knee Surg Sports Traumatol Arthrosc. 2019;27:2096–103. https://doi.org/10.1007/s00167-019-05375-9.
Luyckx L, Luyckx T, Bellemans J, Victor J. Iliotibial band traction syndrome in guided motion TKA. A new clinical entity after TKA. Acta Orthop Belg. 2010;76:507–12.
Christen B, Kopjar B. Second-generation bi-cruciate stabilized total knee system has a lower reoperation and revision rate than its predecessor. Arch Orthop Trauma Surg. 2018;138:1591–9. https://doi.org/10.1007/s00402-018-3019-5.
Kaneko T, Kono N, Mochizuki Y, Hada M, Toyoda S, Musha Y. Bi-cruciate substituting total knee arthroplasty improved medio-lateral instability in mid-flexion range. J Orthop. 2017;14:201–6. https://doi.org/10.1016/j.jor.2016.12.005.
Inui H, Taketomi S, Yamagami R, Kono K, Kawaguchi K, Takagi K, et al. Comparison of intraoperative kinematics and their influence on the clinical outcomes between posterior stabilized total knee arthroplasty and bi-cruciate stabilized total knee arthroplasty. Knee. 2020;27:1263–70. https://doi.org/10.1016/j.knee.2020.06.008.
Healy WL, Sharma S, Schwartz B, Iorio R. Athletic activity after total joint arthroplasty. J Bone Joint Surg Am. 2008;90:2245–52. https://doi.org/10.2106/JBJS.H.00274.
Crawford DA, Adams JB, Hobbs GR, Berend KR, Lombardi AV Jr. Higher activity level following total knee arthroplasty is not deleterious to mid-term implant survivorship. J Arthroplast. 2020;35:116–20. https://doi.org/10.1016/j.arth.2019.07.044.
Witjes S, Gouttebarge V, Kuijer PP, van Geenen RC, Poolman RW, Kerkhoffs GM. Return to sports and physical activity after total and unicondylar knee arthroplasty: a systematic review and meta-analysis. Sports Med. 2016;46:269–92. https://doi.org/10.1007/s40279-015-0421-9.
Mont MA, Marker DR, Seyler TM, Jones LC, Kolisek FR, Hungerford DS. High-impact sports after total knee arthroplasty. J Arthroplast. 2008;23(Suppl 1):80–4. https://doi.org/10.1016/j.arth.2008.04.018.
Huch K, Müller KA, Stürmer T, Brenner H, Puhl W, Günther KP. Sports activities 5 years after total knee or hip arthroplasty: the Ulm osteoarthritis study. Ann Rheum Dis. 2005;64:1715–20. https://doi.org/10.1136/ard.2004.033266.
Matsuda S, Kawahara S, Okazaki K, Tashiro Y, Iwamoto Y. Postoperative alignment and ROM affect patient satisfaction after TKA. Clin Orthop Relat Res. 2013;471:127–33. https://doi.org/10.1007/s11999-012-2533-y.
Matsushita Y, Hamai S, Okazaki K, Murakami K, Ma Y, Kiyohara M, et al. Recreational sports, workout and gym activities after total knee arthroplasty: Asian cohort study. J Orthop. 2019;16:41–4. https://doi.org/10.1016/j.jor.2018.12.002.
Kage T, Inui H, Tomita T, Yamazaki T, Taketomi S, Yamagami R, et al. The association between in vivo knee kinematics and patient-reported outcomes during squatting in Bicruciate-stabilized total knee arthroplasty. J Knee Surg. 2021. https://doi.org/10.1055/s-0041-1723763.
Pizza N, Di Paolo S, Zinno R, Marcheggiani Muccioli GM, Agostinone P, Alesi D, et al. Over-constrained kinematic of the medial compartment leads to lower clinical outcomes after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2021. https://doi.org/10.1007/s00167-020-06398-3.
Kono K, Inui H, Tomita T, Yamazaki T, Taketomi S, Yamagami R, et al. The higher patient-reported outcome measure group had smaller external rotation of the femur in bicruciate-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2021. https://doi.org/10.1007/s00167-021-06577-w.
Van Onsem S, Verstraete M, Van Eenoo W, Van Der Straeten C, Victor J. Are TKA kinematics during closed kinetic chain exercises associated with patient-reported outcomes? A preliminary analysis. Clin Orthop Relat Res. 2020;478:255–63. https://doi.org/10.1097/CORR.0000000000000991.
Yamazaki T, Watanabe T, Nakajima Y, Sugamoto K, Tomita T, Yoshikawa H, et al. Improvement of depth position in 2-D/3-D registration of knee implants using single-plane fluoroscopy. IEEE Trans Med Imaging. 2004;23:602–12 http://ieeexplore.ieee.org/ielx5/42/28807/01295080.pdf?tp=&arnumber=1295080&isnumber=28807.
Yamazaki T, Watanabe T, Nakajima Y, Sugamoto K, Tomita T, Maeda D, et al. Visualization of femorotibial contact in total knee arthroplasty using X-ray fluoroscopy. Eur J Radiol. 2005;53:84–9. https://doi.org/10.1016/j.ejrad.2003.09.018.
Shimizu N, Tomita T, Yamazaki T, Yoshikawa H, Sugamoto K. The effect of weight-bearing condition on kinematics of a high-flexion, posterior-stabilized knee prosthesis. J Arthroplast. 2011;26:1031–7. https://doi.org/10.1016/j.arth.2011.01.008.
Nakamura N, Takeuchi R, Sawaguchi T, Ishikawa H, Saito T, Goldhahn S. Cross-cultural adaptation and validation of the Japanese Knee Injury and Osteoarthritis Outcome Score (KOOS). J Orthop Sci. 2011;16:516–23. https://doi.org/10.1007/s00776-011-0112-9.
Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–60. https://doi.org/10.3758/BRM.41.4.1149.
Kono K, Tomita T, Futai K, Yamazaki T, Tanaka S, Yoshikawa H, et al. In vivo three-dimensional kinematics of normal knees during different high-flexion activitie. Bone Joint J. 2018;100–B:50–5. https://doi.org/10.1302/0301-620X.100B1.BJJ-2017-0553.R2.
Hill PF, Vedi V, Williams A, Iwaki H, Pinskerova V, Freeman MA. Tibiofemoral movement 2: the loaded and unloaded living knee studied by MRI. J Bone Joint Surg Br. 2000;82:1196–8 http://bjj.boneandjoint.org.uk/content/jbjsbr/82-B/8/1196.full.pdf.
Kosse NM, Heesterbeek PJC, Defoort KC, Wymenga AB, van Hellemondt GG. Maximal flexion and patient outcomes after TKA, using a bicruciate-stabilizing design. Arch Orthop Trauma Surg. 2020;140:1495–501. https://doi.org/10.1007/s00402-020-03491-7.
Dennis DA, Komistek RD, Mahfouz MR, Haas BD, Stiehl JB. Multicenter determination of in vivo kinematics after total knee arthroplasty. Clin Orthop Relat Res. 2003;416:37–57. https://doi.org/10.1097/01.blo.0000092986.12414.b5.
Hanreich C, Martelanz L, Koller U, Windhager R, Waldstein W. Sport and physical activity following primary total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty. 2020;35:2274–2285.e1. https://doi.org/10.1016/j.arth.2020.04.013.
Bradbury N, Borton D, Spoo G, Cross MJ. Participation in sports after total knee replacement. Am J Sports Med. 1998;26:530–5. https://doi.org/10.1177/03635465980260041001.
Hepperger C, Gföller P, Abermann E, Hoser C, Ulmer H, Herbst E, et al. Sports activity is maintained or increased following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2018;26:1515–23. https://doi.org/10.1007/s00167-017-4529-3.
Ishibashi T, Tomita T, Yamazaki T, Tsuji S, Yoshikawa H, Sugamoto K. Kinematics of bicruciate and posterior stabilized total knee arthroplasty during deep knee flexion and stair climbing. J Orthop Res. 2021;39:1262–70. https://doi.org/10.1002/jor.24773.
Vielgut I, Leitner L, Kastner N, Radl R, Leithner A, Sadoghi P. Sports activity after low-contact-stress total knee arthroplasty - a long term follow-up study. Sci Rep. 2016;6:24630. https://doi.org/10.1038/srep24630.
Ho JC, Stitzlein RN, Green CJ, Stoner T, Froimson MI. Return to sports activity following UKA and TKA. J Knee Surg. 2016;29:254–9. https://doi.org/10.1055/s-0035-1551835.
Kono K, Inui H, Tomita T, Yamazaki T, Taketomi S, Tanaka S. In vivo kinematics of bicruciate-retaining total knee arthroplasty with anatomical articular surface under high-flexion conditions. J Knee Surg. 2021;34:452–9. https://doi.org/10.1055/s-0039-1696959.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Kenichi Kono helped perform the study and formal analysis and wrote the manuscript. Hiroshi Inui and Tomofumi Kage carried out data curation and conceived the study. Takaharu Yamazaki, Ryota Yamagami, and Kohei Kawaguchi provided technical assistance. Tetsuya Tomita, Shuji Taketomi, and Sakae Tanaka provided general support. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in accordance with the principles of the Declaration of Helsinki. Approval was granted by the University of Tokyo Institutional Ethics Review Board [number 10462-(1)]. Informed consent was obtained from all participants included in the study.
Consent for publication
The patients signed informed consent forms for the publication of their data and photographs.
Competing interests
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kono, K., Inui, H., Kage, T. et al. Femoral rollback at high-flexion during squatting is related to the improvement of sports activities after bicruciate-stabilized total knee arthroplasty: an observational study. BMC Musculoskelet Disord 23, 496 (2022). https://doi.org/10.1186/s12891-022-05464-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05464-w