Abstract
Background
Anemia is a significant global public health issue among children aged 6 to 59 months, particularly in low-income countries like Ethiopia. Studies focusing on pastoral communities, especially in the Afar Region, often underestimate the prevalence of anemia in these children. To address this information gap, this study aimed to determine the prevalence of anemia and its associated factors among children aged 6 to 59 months in public hospitals in the Afar Region of northeastern Ethiopia.
Method
A hospital-based cross-sectional study was conducted among children aged 6 to 59 months, using systematic random sampling, at public hospitals in the Afar Region from February 28 to April 30, 2023.The data collection tool was adapted from the Ethiopian National Food Consumption Survey and the World Health Organization Infant and Young Child Feeding guidelines. Data entry was performed using EpiData version 4.2 and Anthroplus software for anthropometric measurements. Data analysis was conducted using SPSS version 26. Binary logistic regression models were applied to identify predictors of anemia, with a p-value of ≤ 0.05 considered statistically significant.
Result
Among the 306 children aged 6 to 59 months, the overall prevalence of anemia was 46.41 (95 CI: 43.8–48.9 ). Of the 142 anemic children aged 6 to 59 months, 62 (43.66 ) had mild anemia, 60 (42.25 ) had moderate anemia, and 20 (14.08 ) had severe anemia. Key factors associated with anemia included mothers with no formal education, the lowest family monthly income, a family size greater than five, and rural residence. Additionally, a previous diagnosis of parasitic infection, children aged 24–35 months, early weaning, a malaria diagnosis within the past three months, and diarrhea in the last two weeks were significant predictors of anemia in children aged 6 to 59 months.
Conclusion
In the current study, anemia in children aged 6 to 59 months was classified as severe and is regarded as a critical public health issue. This suggests that more efforts should be made to significantly decrease anemia by actively involving rural mothers with no formal education and low income who have children aged 6–59 months, focusing on the prevention and management of malaria, diarrhea, and parasitic infections.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Anemia is a condition characterized by a decrease in the number and size of red blood cells or a reduction in hemoglobin (Hgb) concentration, which impairs oxygen transport throughout the body. In children aged 6 to 59 months, anemia is defined by a hemoglobin level of less than 110 g/L [1,2,3].
Anemia can result from excessive blood loss, parasitic infections, or congenital hemolytic diseases. Different types of anemia include iron deficiency anemia, sickle cell anemia, vitamin deficiency anemia, aplastic anemia, hemolytic anemia, and anemia of inflammation. Iron deficiency is the most common cause of anemia, accounting for approximately 42 of cases in children aged 6 to 59 months worldwide [5].
Anemia is a major global public health issue, with a higher prevalence in low-income countries due to their increased vulnerability to various health and socioeconomic challenges directly or indirectly associated with the condition. While anemia can affect any age group for various reasons, children aged 6 to 59 months are among the most vulnerable [6].
In 2019, the global prevalence of anemia in children aged 6 to 59 months was 39.8 , affecting approximately 269 million children. The African region had the highest rate of anemia among children under five, at 60.2 . Additionally, the 2021 WHO report on anemia stated that the prevalence of anemia among children aged 6 to 59 months in Ethiopia ranged from 40 to 60 in 2019 [7, 8].
According to the 2016 Ethiopian Demographic and Health Survey (EDHS), 57 of Ethiopian children aged 6 to 59 months have anemia. Prevalence varies geographically, ranging from 42 in the Amhara Region to 75 in the Afar Region and 83 in the Somali Region [9]. The prevalence of childhood anemia varies across different regions of the country. A study conducted in Kombolicha, northeast Ethiopia, found that 52.2 of children aged 6 to 59 months were anemic [10]. Similarly, studies in various regions of Ethiopia reported the following prevalence rates of anemia in children aged 6 to 59 months: 28.6 in Gondar Town (northwest Ethiopia) [11], 28.5 in North Shewa (central Ethiopia) [12], 21.6 in Tigray (northern Ethiopia) [13], and 41.7 in Hawassa Teaching Hospital (southern Ethiopia) [14].
Numerous studies have identified several factors linked to anemia in children aged 6 to 59 months. These include childhood characteristics such as age, residency, feeding practices, nutritional status, intestinal parasites, malaria infection, iron and vitamin A supplementation, deworming, consumption of raw foods, and dietary diversity [10,11,12,13]. Additionally, family and maternal factors have been associated with anemia in this age group. These factors include the mother’s age, education level, marital status, family income, waste disposal practices, maternal anemia, household food insecurity, water source, family size, antenatal care, and maternal nutritional status [14,15,16,17].
If left untreated, anemia in children aged 6 to 59 months can have significant consequences, including growth retardation, a weakened immune system, and increased susceptibility to illness and mortality. It also has severe socioeconomic impacts on families and communities [18,19,20,21]. Additionally, anemia can have lasting effects on female offspring, resulting in low-birth-weight newborns and postpartum hemorrhage. Children from low-income families are at a higher risk of developing iron deficiency anemia [22].
Despite Ethiopia’s significant efforts to combat anemia among children aged 6 to 59 months, based on World Health Organization (WHO) recommendations—including initiatives such as Infant and Young Child Feeding (IYCF), iron supplementation, increased meal frequency, dietary diversity, and the management of infectious diseases like malaria, helminthic infections, and tuberculosis—anemia in the country remains classified as severe. These efforts are in addition to existing programs like Integrated Management of Newborn and Childhood Illness (IMNCI), safe motherhood, malaria rollback, deworming, and tuberculosis management [7].
Despite numerous studies documenting anemia among children aged 6 to 59 months in Ethiopia, research in pastoral communities, such as the Afar Region, remains limited. These studies often overlook stool examinations, dietary diversity, and environmental factors. Moreover, unlike previous studies, this study was multi-centered. This study aimed to address the information gap and present recommendations that could inspire local multi-sectoral managers to combat anemia and ultimately foster healthier generations.
Methods
Study area and period
The study was conducted in public hospitals in the Afar region from February 28 to April 30, 2023. Ethiopia is divided into 12 regional states, one of which is the Afar National Regional State. This state covers an area of 278,000 square kilometers and is situated between 9 N and 12 N latitude and 40 E and 42 E longitude in the Great East African Rift Valley. The capital city of the Afar National Regional State is Samara, located 570 km north of Addis Ababa in the country’s northeast. The Afar region is served by seven public hospitals, which cater to an estimated population of 5 million people.
Study design and populations
A hospital-based cross-sectional study design was employed. All 6-59-month-old children who visited Afar Region public hospitals were sources of population. However, randomly selected 6-59-month-old children who visited selected Afar Region public hospitals were considered as study units.
Eligibility criteria
This study included all children aged 6 to 59 months who visited the selected public hospitals. Children with a known bleeding disease, severe illness, mentally ill mothers or caregivers, and children who had received blood transfusions in the previous three months were excluded from the study.
Sample size determination and sampling procedures
The required sample size for the study was determined using a single population proportion formula. The calculation employed a formula for a single population with the following parameters: a confidence level of 95 , a margin of error of 0.05, and an anemia prevalence of 75 in the Afar region [9]. .
By including a 10 non-response rate, the total sample size increased to 317.
Out of the seven public hospitals in the study area, four were selected using a simple random sampling method via lottery methods: Asaita District Hospital, Dubti General Hospital, Kelewan General Hospital, and Mohammed Aklie Memorial Hospital. The average number of children aged 6 to 59 months visiting each hospital per month was calculated based on the number of such visits in the quarter preceding the data collection. This resulted in an overall monthly average of 1,400 visits, with 390 at Asaita District Hospital, 410 at Dubti General Hospital, 300 at Kelewan General Hospital, and 300 at Mohammed Aklie Memorial Hospital. Based on these averages, a proportionate allocation to size was determined for each hospital. Consequently, 88 children were allocated to Asaita District Hospital, 93 to Dubti General Hospital, 68 to Kelewan General Hospital, and 68 to Mohammed Aklie Memorial Hospital. The Emergency Triage Assessment and Treatment (ETAT) registration book was used as the sampling frame. Initially, the first child was selected using a lottery method, and then every fourth child aged 6 to 59 months was included in the study using systematic random sampling.
Study variables
Dependent variable
Anemia among children aged 6 to 59 months.
Independent variables
Sociodemographic factors related to the child and their parents.
Maternal and child health-related factors were assessed, including maternal antenatal care (ANC), place of delivery, postpartum care (PNC), child immunization history, and the child’s nutritional status based on WHO anthropometric measures.
Child feeding practices, encompassing dietary diversity scores.
Environmental factors, including the source of water and the status and type of latrines.
The medical history and laboratory examinations included screening for parasitic infections and malaria, assessed through hematologic and stool tests.
Operational definitions
Malnutrition
Children aged 6 to 59 months with a weight-for-length/height between 2 SD and 3 SD from the median were classified as moderately wasted, while those with a weight-for-length/height 3 SD were classified as severely wasted [9]. Similarly, children with a length/height-for-age between 2 SD and 3 SD from the median were considered moderately stunted, and those with a length/height-for-age 3 SD were considered severely stunted [9].
Anemia
Children aged 6 to 59 months with a hemoglobin (Hgb) level of 11.0 g/dl or higher were classified as non-anemic. Those with an Hgb level below 11.0 g/dl were considered anemic. Specifically, Hgb values of 10.0 to 10.9 g/dl indicated mild anemia, values of 7.0 to 9.9 g/dl indicated moderate anemia, and values below 7.0 g/dl indicated severe anemia [9]. This reference value applies to both male and female children, as there is no gender difference in hemoglobin levels until age 12 [24, 25].
Dietary diversity score
This score was calculated by counting the number of food categories consumed in the previous 24 h. For children aged 6 to 23 months, a consumption of 5 to 8 food groups was considered indicative of adequate dietary diversity, while for children aged 24 to 59 months, a consumption of 4 to 7 food groups was deemed adequate [26].
Data collection tools and procedures
In the current study, pretested questionnaires, developed based on previous literature [10, 15, 17, 27, 28], were used to collect relevant data. Data collection involved face-to-face interviews, chart reviews, hematologic and stool examinations, and anthropometric measurements. Section one of the questionnaire covered sociodemographic factors related to the child and their parents or caregivers. Section two focused on maternal and child health, including factors such as maternal antenatal care (ANC), place of delivery, postpartum care (PNC), child immunization history, and the child’s nutritional status through WHO anthropometric measures. Section three assessed child feeding practices, including dietary diversity scores. The questionnaire was developed using the Food and Agriculture Organization (FAO) / Food and Nutrition Technical Assistance (FANTA) recommendations for measuring family and individual dietary diversity [29] and the WHO Infant and Young Child Feeding (IYCF) guidelines [26], both of which are based on the 24-hour recall technique. Additionally, participants were asked whether their child had consumed food from each of eight food groups in the 24 h prior to the survey for children aged 6 to 23 months, and from seven food groups for children aged 24 to 59 months. Section 4 addressed environmental factors such as water source and latrine status and type. Section 5 evaluated anemia status, parasitic infections, and malaria infection through hematologic and stool examinations. To ensure consistency, the questionnaire was originally written in English, translated into Afaragna, and then back-translated into English by experts fluent in both languages. Data collection was carried out by four qualified pediatric nurses and four medical laboratory technicians.
Anthropometrics examinations
Anthropometric measurements were conducted in the hospital examination room. Weight was measured using a digital Seca scale (SECA, Germany) to the nearest 0.1 kg. To ensure privacy, participants wore light clothing and no shoes during the measurement. Each adolescent’s weight was recorded twice, and if the variance between the two measurements exceeded 0.5 kg, both readings were discarded, and the procedure was repeated. Otherwise, the average of the two measurements was used for analysis. Height was measured to the nearest 0.1 cm using a stadiometer (SECA, Germany). Participants stood on the measuring board without shoes, in the normal anatomical position, with their heels, buttocks, shoulders, and the back of their heads touching the board. The headband of the stadiometer was positioned flat against the crown of the head, forming a 90-degree angle with the board.
Blood specimen collection and hematologic examination
Capillary blood samples were obtained from children under rigorous aseptic measures by skilled laboratory professionals after asking their parents or caregivers about their willingness. The Cell-DYN 1800 machinery was used to measure hemoglobin concentration.
Stool specimen collection and examination
Before collecting stool samples, parents and children were informed about the study’s goals and given specific instructions on how to properly collect and store the samples in labelled containers. Each child’s 2 mg feces sample was collected in a clean plastic jar labeled with an identity number. Within 30 min of collecting the sample, a wet-mount smear was made using saline and/or iodine solution for direct microscopic detection of intestinal parasites. The direct smear was inspected by trained medical laboratory personnel using 10x and 40x objectives to detect helminth eggs, larvae, and protozoan parasites.
Data quality control
Data quality was ensured through rigorous design, translation, pre-testing of the questionnaire, and data collector training. Every day after data collection, the lead investigator and supervisors examined the completed questionnaire for completeness, and adjustments were made for the following day. For all laboratory activities, standard operating procedures and the manufacturer’s instructions were rigorously followed. The expiry date of all laboratory reagents was examined. Samples were examined to ensure that they met accepted criteria such as volume, uniformity, and collection time. The cleanliness of microscopic slides and cover glasses was tested.
Data processing and analysis
For analysis, the data was entered into EpiData version 4.2 and exported to Statistical Package for the Social Sciences (SPSS) version 26.0 (IBM-SPSS., Chicago, IL, USA). To determine nutritional status, anthropometric data was entered and analyzed using WHO Anthroplus software Version 3.2. Before conducting the final analysis, an exploratory analysis was performed to check for missing values, outliers, and assumptions. For categorical variables, frequency and percentage were used. To investigate factors associated with anemia, a binary logistic regression model was used. Variables with p values of < 0.25 in the bivariable analysis were included in the multivariate analysis. In the multivariable analysis, the adjusted odds ratio (AOR) with a 95 confidence interval was used to assess the strength of the association, and a p value of < 0.05 was used to declare it statistically significant. Furthermore, multicollinearity was reviewed, and to assess the relative effects of explanatory variables on the outcome, the final logistic model’s goodness of fit was non-significant for the Hosmer and Lemshow tests but significant for the Omnibus test.
Ethical approval and consent to participate
The study protocol was evaluated and approved by Wollo University College of Medicine and Health science research and community service committee with reference No_(WU/CMHS/20/123/2023) and ethical clearance was obtained. Additionally, before commencing the study, permission letters were obtained from each hospital manager and the quality assurance department. Written informed consent was obtained from each children mother. Moreover, this study was conducted in compliance with the Declaration of Helsinki. The purpose and significance of the study were clearly explained to the children’s mothers during the hematologic, stool, and anthropometric assessments. The autonomy and dignity of the participants were respected, and they were allowed to pause the assessments if they experienced any discomfort. Anonymous data were obtained and the confidentiality of participants information was secured. Moreover, subject confidentiality and any special data security requirements were maintained and assured through the use of codes instead of participants’ names.
Result
Socio-demographic characteristics of participants
Out of 317 participants, 306 children aged 6 to 59 months were included, resulting in a response rate of 96.5 . The mean age of the children was 39.6 months (SD ± 26.34 months). Of the total 306 children aged 6 to 59 months, 185 (66.5 ) were older than 24 months, 161 (52.61 ) were female, and 199 (65.03 ) came from urban areas. A total of 120 (39.2 ) of the children’s mothers had no formal education, and 170 (55.56 ) of the study participants lived in households with five family members. Additionally, 111 (36.3 ) had incomes ranging from 3,000 to 7,500 Ethiopian birr (Table 1).
Child and maternal health related characteristics
About 240 children (78.43 ) were fully immunized, while 56 (18.3 ) had experienced diarrhea in the two weeks prior. Before the 48-hour survey, 129 children (42.16 ) had a fever. Additionally, 88 children (28.76 ) were moderately wasted, and 48 (15.7 ) were moderately stunted. Of the total participants, 219 (71.56 ) were born in a hospital, but only 66 (21.56 ) received postnatal care, with 36 (54.55 ) receiving just one visit (Table 2).
Child feeding practices
The vast majority of children, 276 (90.19 ), received colostrum feeding; 164 (53.6 ) were exclusively breastfed for 4–6 months; 152 (49.67 ) started complementary feeding less than 6 months; 125 (40.85 ) received semi-fluid complementary feeding; 211 (69.1 ) had an inadequate dietary diversity score; and 171 (55.89 ) had an inadequate meal frequency of 2–3 times per day (Table 3).
Environmental characteristics
The vast majority of households, 241 (78.76 ), had no water supply, and 172 (56.21 ) used an open field to dispose of solid waste. Furthermore, 195 (63.73 ) of the households had insects, the majority of which were mosquitoes (81, or 41.54 ). Additionally, more than half of the households (55.5 ) had a latrine (Table 4).
Child clinical profile
Approximately 103 children aged 6 to 59 months (33.7 ) had a parasitic infection in the current study. Among these, 51 (49.51 ) were infected with Entamoeba histolytica. Additionally, 72 children (23.53 ) had a history of malaria infection in the previous three months (Table 5).
Prevalence of 6-59-month-old child anemia
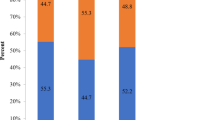
In the current study, the overall prevalence of anemia was 142 cases, representing 46.41 (95 CI: 43.8 − 48.9 ). Among these 142 anemic children, 62 (43.66 ) had mild anemia, 60 (41.38 ) had moderate anemia, and 20 (14.08 ) had severe anemia (Fig. 1). The highest prevalence was observed in the age group of 24 to 35 months (68.8 ), with rates gradually decreasing as the children’s age increased (Fig. 2).
Factors associated with Anemia
In a multivariate analysis, children aged 24 to 35 months were three times more likely to be anemic than children aged 48 to 59 months (AOR = 3.12, 95 CI: 1.47–7.11). Children with mothers who had no formal education were seven times more likely to be anemic (AOR = 7.06, 95 CI: 2.81–19.30) compared to children with mothers who had tertiary education. Furthermore, children from rural areas were six times more likely to be anemic than children from urban areas (AOR = 6.11, 95 CI: 1.49–8.99). Children from families with five or more members were nearly four times more likely to be anemic (AOR = 3.76, 95 CI: 1.82–5.98) compared to those from families with 2 to 4 members. Children who began complementary feeding early were 3.5 times more likely to be anemic (AOR = 3.51, 95 CI: 2.36–6.51) than those who started later. Children who had previously experienced a parasitic infection were nearly four times more likely to be anemic (AOR = 3.76, 95 CI: 2.82–5.98) compared to those who had not. Additionally, children who had malaria in the previous three months were 3.4 times more likely to be anemic (AOR = 3.37, 95 CI: 2.16–11.31) than those who had not had malaria. Similarly, children who had diarrhea were three times more likely to be anemic (AOR = 2.9, 95 CI: 1.57–3.81) than those who did not have diarrhea (Table 6).
Discussion
In the current study, the overall prevalence of anemia among children aged 6 to 59 months attending public hospitals in the Afar region was 46.41 . This indicates that anemia is a severe public health concern for this age group, according to the WHO classification of anemia severity (> 40 ) [30]. This prevalence is comparable to studies conducted in Kombolicha town [10], Debre Brehan (47.5 ) [16], Shanan Gibe Hospital (48.9 ) [31], and Jimma Medical Center in South West Ethiopia (44.8 ) [32]. However, it is lower than the national average [9], the 2016 EDHS report for the Afar region [9], as well as findings from Ghana (78.4 ) [33] and Uganda (58.8 ) [34]. This discrepancy might be due to differences in study settings; the studies mentioned above were conducted in community-based settings, which might result in a higher prevalence of anemia. Other possible explanations include differences in sample size, geographic variations, seasonal factors, and the equipment used for sample analysis. Additionally, the prevalence found in the current study is higher than that reported in northwest Ethiopia (Gondar Town) [11], central Ethiopia (North Shewa) [12], northern Ethiopia (Tigray) [13], and southern Ethiopia (Hawassa Teaching Hospital) [14]. This disparity may be attributed to the fact that the study area is frequently affected by drought and conflict, has an inadequate safe water supply, is a pastoral community, and experiences lower productivity. These factors likely contribute to food insecurity in the region.
In the current study, children aged 6 to 59 months who were from mothers with no education and had the lowest monthly family income were more likely to be anemic. These findings are consistent with studies conducted in Kombolicha Town [10], Gondar Town [11], Gugufitu [15], Hawassa Referral Hospital [14], Tigray [27], and Shanan Gibe Hospital [31]. This may be because children of mothers with no education might lack awareness about meal frequency and dietary diversity, which can contribute to anemia. Additionally, families with the lowest income may experience reduced productivity and worsened food insecurity due to overcrowding, ultimately leading to higher rates of anemia. This suggests that enhancing parental education and promoting diversified agricultural practices could help address food security issues, including anemia.
In this study, children aged 6 to 59 months living in rural areas were more likely to be anemic than those in urban settings. This finding aligns with results from a study conducted at Shanan Gibe Hospital in southwestern Ethiopia [31]. One possible explanation is that lowland rural areas are more prone to anemia due to frequent droughts, inadequate water supplies, poor waste disposal practices, higher rates of malaria, and limited dietary diversity, as these areas are often pastoral communities. Conversely, a study from Gugufitu district in northeastern Ethiopia [15] found that urban children were more likely to be anemic than those in rural areas. This discrepancy might be attributed to differences in agricultural practices, geographic conditions, and water supply. Gugufitu district benefits from more productive and diversified agriculture, higher altitude (over 3000 m), lower malaria prevalence, and better access to safe water compared to the study area.
Children aged 24 to 35 months were found to be more anemic than younger infants up to 24 months old. This finding contrasts with studies conducted in Kilte Awulaelo Woreda [27], Hawassa Referral Hospital [14], Gugufitu [15], Menz Gera [12], and Kombolicha [10], which found that younger children (6–24 months) were more anemic than older children. One possible explanation is that younger infants may benefit from breastfeeding, while older children, who are transitioning to a more diverse diet, might have less nutritional variety in their diet. This lack of diversity during this period can make them more vulnerable to anemia.
Children who were weaned early were more susceptible to anemia than those who began weaning at the appropriate age. This finding aligns with studies conducted in Gugufitu and Kombolicha Towns [10, 15]. The likely explanation is that exclusive breastfeeding for up to six months, as recommended by the WHO, is the optimal feeding strategy. This approach helps prevent respiratory, diarrheal, and chronic diseases and reduces the risk of anemia [35]. These findings imply that starting supplemental feeding too early significantly increases the risk of diarrheal illness and anemia.
In the current study, children who had previously diagnosed parasite infection and malaria and had diarrhea in the last two weeks were more likely to have anemia. This is in line with studies in Shanan Gibe Hospital, southwest Ethiopia, and Kombolicha, northeastern Ethiopia, respectively [10, 31]. One possible explanation is that parasitic and malaria infections lead to the destruction of red blood cells (RBCs), resulting in a significant decrease in RBC count, commonly known as anemia. Additionally, the parasites that cause diarrhea also contribute to anemia. This suggests that further efforts are needed to improve the safe water supply, increase the uptake of deworming treatments, and enhance malaria control measures.
Strength and limitation of the study
The study was conducted in a multi-center setting and used a measurement tool that considered various factors associated with anemia in children aged 6–59 months, including anthropometric data, stool examinations, environmental factors, and relevant child feeding practices. Anemia was determined solely using hemoglobin concentration criteria; however, the addition of other measurements such as serum ferritin may allow for improved case distinction. Because this is an institution-based study, the findings cannot be generalized to the greater community. Objective approaches did not prove the presence of comorbidities such as malaria and diarrhea. We simply asked parents if their child had been exposed to these situations in the previous three months or two weeks. The recall and comprehension of respondents would influence the reliability of this reply. Furthermore, because this study was conducted just during a single season, the prevalence may not be representative throughout the year.
Conclusion
According to the WHO classification, the prevalence of anemia among children aged six to 59 months in the study area was severe, posing serious public health challenges. Factors significantly associated with anemia included the child’s age, maternal education, family size and income, rural residence, early initiation of weaning, and diagnoses of diarrhea, malaria, and parasitic infections. Extensive community- and facility-based efforts to promote exclusive breastfeeding should be strengthened. Empowering mothers through adult education and mixed farming can also help address food security issues. Additionally, improvements in safe water supply, deworming programs, and malaria control activities are essential. Researchers are encouraged to use follow-up studies to explore more biomarkers to better understand the origins of anemia and its fluctuations over time.
Data availability
All data generated or analyzed during this study are included in the manuscript and are also available from the corresponding authors up on request.
Abbreviations
- ANC:
-
Antenatal Care
- AOR:
-
Adjusted Odds Ratio
- CI:
-
Confidence Interval
- COR :
-
Crude Odds Ratio
- EDHS:
-
Ethiopian Demographic and Health Survey
- g/dl :
-
Gram per deciliter
- Hgb :
-
Hemoglobin
- IYCF:
-
Infant and Young Child Feeding
- IMNCI:
-
Integrated Management of Neonatal and Child Illness
- PNC :
-
Post Natal Care
- RBC:
-
Red Blood Cell
- SD:
-
Standard Deviations
- TB:
-
Tuberculosis
- WHO:
-
World Health Organization
References
World Health Organization. Health topics: Anemia. https://www.who.int/health-topics/anaemia#tab = tab_1. Accessed 19 Feb 2023.
World Health Organization. Prevalence of anemia [Internet]. Geneva, Switzerland: World Health Organization. 2017. https://www.who.int/data/gho
World Health Organization. Micronutrients database [Internet]. Geneva. 2021 [cited 2021 Mar 17]. https://www.who.int/vmnis/database/en/
Vieth JT, Lane DR. Anemia. Emerg Med Clin. 2014;32(3):613–28.
World Health Organization. Nutritional anemias: tools for effective prevention and control. Geneva; 2017.
Gardner W. Nicholas Kassebaum. Global, Regional, and National Prevalence of Anemia and its causes in 204 countries and territories, 1990–2019. Curr Dev Nutr. 2020;4.
World Health Organization. WHO methods and data sources for mean hemoglobin and anemia estimates in women of reproductive age and pre-school age children 2000–2019. Department of Nutrition and Food Safety World Health Organization Geneva, Switzerland;2021.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22.
Central Statistical. Agency (CSA) [Ethiopia], ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia; 2017.
Fentaw W, Belachew T, Andargie A. Anemia and associated factors among 6 to 59 months’ age children attending health facilities in Kombolcha town, Northeast Ethiopia: a facility-based cross-sectional study. BMC Pediatr. 2023;23(1):209.
Melku M, Alene KA, Terefe B, Enawgaw B, Biadgo B, Abebe M, et al. Anemia severity among children aged 6–59 months in Gondar town, Ethiopia: a community-based cross-sectional study. Ital J Pediatr. 2018;44:1–12.
Engidaye G, Melku M, Yalew A, Getaneh Z, Asrie F. Under nutrition, maternal anemia and household food insecurity are risk factors of anemia among preschool aged children in Menz Gera Midir district, Eastern Amhara, Ethiopia: a community based cross-sectional study. BMC Public Health. 2019;19:968.
Wasihun AG, Teferi M, Negash L, Marugán J, Yemane D, McGuigan KG, et al. Intestinal parasitosis, anaemia and risk factors among pre-school children in Tigray region, northern Ethiopia. BMC Infect Dis. 2020;20:1–11.
Gebereselassie Y, Birhanselassie M, Menjetta T, Alemu J, Tsegaye A, Magnitude. Severity, and Associated factors of Anemia among under-five children attending Hawassa University Teaching and Referral Hospital, Hawassa, Southern Ethiopia, 2016. Anemia. 2020;2020.
Gebreweld A, Ali N, Ali R, Fisha T. Prevalence of anemia and its associated factors among children under five years of age attending at Guguftu health center, South Wollo, Northeast Ethiopia. PLoS ONE. 2019;14:1–13.
Molla A, Egata G, Mesfin F, Arega M, Getacher L. Prevalence of Anemia and Associated Factors among Infants and Young Children Aged 6–23 Months in Debre Berhan Town, North Shewa, Ethiopia. J Nutr Metab. 2020;2020.
Enawgaw B, Workineh Y, Tadesse S, Mekuria E, Addisu A, Genetu M. Prevalence of anemia and associated factors among hospitalized children attending the University of Gondar Hospital, Northwest Ethiopia. J Int Federation Clin Chem Lab Med. 2019;30:35–47.
Haas JD, Brownlie IVT. Iron deficiency and reduced work capacity: a critical review of the research to determine a causal relationship. J Nutr. 2001;131(2 SUPPL):2:676–90.
Lozoff B. Iron deficiency and child development. Food Nutr Bull. 2007;28(4 SUPPL):560–71.
Oppenheimer SJ. Iron-deficiency anemia: reexamining the nature and magnitude of the public health problem. J Nutr. 2001;131:616–35.
Grantham-Mcgregor S, Baker-Henningham H. Iron deficiency in childhood: causes and consequences for child development. Ann Nestle. 2010;68:105–19.
Kliegman ERB, Jenson RM. HB. Nelson Textbook of Pediatrics. 17th edition. Judith Fletcher; 2004.
WHO, UNICEF. Focusing on anemia: towards an integrated approach for effective anemia control. World Health Organization; 2004.
Fairman JE, Wang M. Iron Deficiency and other types of Anemia in infants and children. Am Fam Physician. 2016;93:270–8.
Janus J, Moerschel SK. Evaluation of Anemia in Children. Am Fam Physician. 2010;81:1462–71.
World Health Organization (WHO). Indicators for assessing infant and young child feeding practices: part 2 measurement. Geneva; 2010.
Gebreegziabiher G, Etana B, Niggusie D. Determinants of Anemia among children aged 6–59 months living in Kilte Awulaelo Woreda, Northern Ethiopia. Anemia. 2014;2014.
Birhanu M, Gedefaw L, Asres Y. Anemia among School-Age children: Magnitude, Severity and Associated factors in Pawe Town, Benishangul-Gumuz Region, Northwest Ethiopia. Ethiop J Health. 2017;28:256.
Food and Agriculture Organization (FAO). Guidelines for measuring household and individual dietary diversity. 2013.
Salami A, Ghssein G, Lamis Salloum HF. Prevalence of anemia among Lebanese hospitalized children. PLOS. 2018;13.
Kebede D, Getaneh F, Endalamaw K, Belay T, Fenta A. Prevalence of anemia and its associated factors among under-five age children in Shanan Gibe hospital, Southwest Ethiopia. BMC Pediatr. 2021;21(1):1–9.
Fufa BD, Gutema H. Prevalence of Anemia and Associated Factors among ChildrenAttended at Jimma Medical Center, South West Ethiopia. Int Arch Nurs Health Care. 2019;5:129. https://doi.org/10.23937/2469-5823/1510129.
Ewusie JE, Ahiadeke C, Beyene J, Hamid JS. Prevalence of anemia among under-5 children in the Ghanaian population: estimates from the Ghana demographic and health survey. BMC Public Health. 2014;14:1–9.
Kuziga F, Adoke Y, Wanyenze RK. Prevalence and factors associated with anaemia among children aged 6 to 59 months in Namutumba district, Uganda: a cross-sectional study. BMC Pediatr. 2017;17(1):1–9.
WHO/UNICEF. Global Nutrition Target 2025: Breastfeeding Policy Brief (WHO/ NMH/NHD/14.7). 2014;8.
Acknowledgements
The authors would like to thank the Afar region public hospitals managers, the care providers, and the participants families for their kind cooperation. The authors are also thankful to the data collectors and the study participants.
Funding
No external funds were obtained; only institutional support from Afar region public hospitals and Wollo university.
Author information
Authors and Affiliations
Contributions
Molla Kasssa made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; Muluken Amare involving in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work; Tarikua Afework , Yemane Eshetu, and Dagne Belete took part in revising it critically for important intellectual content. Furthermore, involved more in acquisition of data, or analysis and interpretation of data.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
This study was approved by the Wollo University College of Medicine and Health science research and community service committee and ethical clearance was obtained. Additionally, before commencing the study, permission letters were obtained from each hospital manager and the quality assurance department. Written informed consent was obtained from each children mother. Moreover, this study was conducted in compliance with the Declaration of Helsinki. The purpose and significance of the study were clearly explained to the children’s mothers during the hematologic, stool, and anthropometric assessments. The autonomy and dignity of the participants were respected, and they were allowed to pause the assessments if they experienced any discomfort. Anonymous data were obtained and the confidentiality of participants information was secured. Moreover, subject confidentiality and any special data security requirements were maintained and assured through the use of codes instead of participants’ names.
Consent for publication
Not applicable.
Competing of interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hailu, M.K., Wudu, M.A., Gebriye, D.B. et al. Prevalence of Anemia and its associated factors among 6–59 months age children visiting public hospitals at Afar Region, Northeast Ethiopia: a hospital-based cross-sectional study. BMC Pediatr 24, 589 (2024). https://doi.org/10.1186/s12887-024-05078-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-024-05078-2