Abstract
Background
Urachal carcinoma is an extremely rare malignant tumor originating from the urachus. Urachal adenocarcinoma has never been reported in patients under 20 years of age. In this case, we describe a 15-year-old patient with urachal adenocarcinoma and propose possible risk factors.
Case presentation
The patient presented with hematuria for two months and dysuria for one month, and had a history of smoking and alcohol consumption for three years. Ultrasonography showed an irregular mass on the anterior wall of the bladder. Contrast-enhanced computed tomography revealed a pedicled soft tissue mass measuring 2.6×2.4 cm within the bladder, showing significant enhancement. Partial cystectomy was conducted, and a histopathological diagnosis of urachal adenocarcinoma (T2N0M0) was made. During eight months of follow-up, the patient remained asymptomatic with no evidence of recurrence.
Conclusions
Urachal remnants may lead to urinary symptoms and the development of urachal carcinoma. A history of smoking and alcohol consumption could be possible risk factors for urachal adenocarcinoma in this case. It is possible that urachal remnants can undergo malignant transformation, even at ages as young as 15 years. Regular follow-up should be recommended for patients whose urachal remnants persist beyond childhood.
Similar content being viewed by others
Background
The urachus is a three-layered tubular structure as a remnant of an embryonic structure. Urachal remnants result from failure of allantois lumen obliteration, and may lead to urinary symptoms and the development of urachal carcinoma at an older age. This anomaly is relatively uncommon, with a prevalence of 1% in children [1]. Urachal carcinoma is an extremely rare malignant tumor originating from the urachus, with an incidence of 0.3% among all bladder cancers [2]. The majority of cases are diagnosed in individuals in their 50s and 60s, with a median age at diagnosis of 52 years, according to a study reviewing 1,010 cases [3]. Urachal adenocarcinoma has never been reported in patients under 20 years of age. Here, we describe a case of 15-year-old with urachal adenocarcinoma.
Case presentation
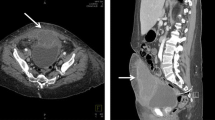
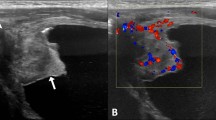
A 15-year-old Chinese boy, previously healthy with an unremarkable past medical and family history, complained of hematuria for two months and dysuria for one month. The boy had a history of smoking and alcohol consumption for three years, smoking approximately 20 cigarettes per day and drinking alcohol approximately once a week. The physical examination was unremarkable. Ultrasonography showed a hypoechoic, obscurely-demarcated, irregular mass on the anterior wall of the bladder (Fig. 1A). Doppler assessment detected vascular flow within the mass. Contrast-enhanced computed tomography revealed a pedicled soft tissue mass measuring 2.6×2.4 cm within the bladder, showing significant enhancement (Fig. 1B). A high-density nodular image was observed in front of the bladder (Fig. 1C).
(A) Ultrasonography showed a hypoechoic, obscurely-demarcated, irregular mass with vascular flow on the anterior wall of the bladder. (B) Contrast-enhanced computed tomography revealed a pedicled soft tissue mass measuring 2.6×2.4 cm within the bladder, showing significant enhancement. (C) computed tomography showed a high-density nodular image in front of the bladder. (D) Histological image of hematoxylin and eosin staining. (E) Positive staining for CK (pan). (F) Positive staining for CK20. (G) Positive staining for CDX2. (H) Positive staining for β-catenin
A bladder tumor was suspected, and open partial cystectomy was conducted. The entire mass, along with part of the bladder wall and the distal segment of the urachus, was resected. The tumor involved the submucosal and muscular layers, but not the peritoneum. The surgical margin was negative. A histopathological diagnosis of urachal adenocarcinoma was made. The high-density nodule in front of the bladder was confirmed to be a stone in the urachus. Mucinous adenocarcinoma cells were identified via hematoxylin and eosin staining, and some cells were signet-ring cells (Fig. 1D). Immunohistochemical analysis showed positive staining for CK (pan), CK20, CDX2 and β-catenin (Fig. 1E, F, G and H). The patient was diagnosed with T2N0M0 urachal adenocarcinoma. An indwelling catheter was placed in the bladder for 5 days after the operation. He recovered uneventfully and was discharged six days after the operation. A CT scan performed six months after discharge showed no evidence of recurrence. During eight months of follow-up after discharge, the patient remained asymptomatic.
Discussion
Urachal adenocarcinoma was previously thought to occur in adults, whereas this case was an adolescent boy with a history of smoking and alcohol consumption. The risk factors for urachal adenocarcinoma remain unclear. In this case, it seems that a history of smoking and alcohol consumption may be a risk factor for urachal adenocarcinoma, which could help explain why urachal adenocarcinoma is more common in men. Additionally, a stone found in the urachus could cause urinary stasis and chronic irritation, which may also contribute to tumor development. The most frequent clinical presentations of urachal adenocarcinoma in adults are hematuria, abdominal pain and dysuria, which are similar to the symptoms observed in this adolescent.
Approximately half of urachal carcinomas exhibit elevated levels of serum markers including CA125, CA19–9, CEA [4, 5]. These makers serve as diagnostic indicators and predictors of therapeutic response and recurrence [4, 6]. We did not examine any of these serum markers before surgery because we were unaware of the possibility of urachal carcinoma. Ultrasonography is widely used to diagnose urinary system diseases and can often identify an irregular mass located at the dome or midline of the anterior wall of the bladder in patients with urachal carcinomas, although it lacks specificity. Mucin-producing urachal adenocarcinoma frequently contains calcification at the dome or midline of the anterior wall of the bladder, which is thought to be characteristic [7]. Calcification are present in about 32% of urachal carcinomas and can be easily detected via computed tomography [3]. Cystoscopy is the most sensitive diagnostic method and should be mandatory when urachal carcinoma is suspected [8].
For localized urachal carcinoma, the recommended treatment is excision of the urachus, umbilicus and partial/radical cystectomy, along with removal of the bilateral pelvic lymph nodes [9]. In this case, we conducted a partial cystectomy without resecting the entire urachus, the umbilicus or the bilateral pelvic lymph node, as we did not initially consider the possibility of urachal adenocarcinoma and the CT scan did not reveal any enlarged pelvic lymph nodes. Partial cystectomy is preferred over radical cystectomy because the survival rate in cases undergoing partial cystectomy is similar to that in cases undergoing radical cystectomy, and patients undergoing partial cystectomy have a better quality of life. More than 20% of patients develop distant metastases at diagnosis [3]. For these patients, chemotherapy is the only treatment choice, and the 5-year survival rate is lower than 20%.3 A cohort study indicates that distant metastasis is more common in patients under 45 years old [10].
In conclusion, urachal remnants may undergo malignant transformation even at ages as young as 15 years. Regular follow-up should be suggested for patients with urachal remnants persisting beyond childhood.
Data availability
The datasets used during the current study are available from the corresponding author on reasonable request.
References
Gleason JM, Bowlin PR, Bagli DJ, Lorenzo AJ, Hassouna T, Koyle MA, et al. A comprehensive review of pediatric urachal anomalies and predictive analysis for adult urachal adenocarcinoma. J Urol. 2015;193:632–6.
Collins DC, Velázquez-Kennedy K, Deady S, Brady AP, Sweeney P, Power DG. National Incidence, Management and Survival of Urachal Carcinoma. Rare Tumors. 2016;8:6257.
Szarvas T, Módos O, Niedworok C, Reis H, Szendröi A, Szász MA, et al. Clinical, prognostic, and therapeutic aspects of urachal carcinoma-A comprehensive review with meta-analysis of 1,010 cases. Urol Oncol. 2016;34:388–98.
Behrendt MA, van Rhijn BW. Genetics and biological markers in urachal cancer. Transl Androl Urol. 2016;5:655–61.
Siefker-Radtke AO, Gee J, Shen Y, Wen S, Daliani D, Millikan RE, et al. Multimodality management of urachal carcinoma: the M. D. Anderson Cancer Center experience. J Urol. 2003;169:1295–8.
Reis H, Szarvas T. Urachal cancer-current concepts of a rare cancer. Pathologe. 2019;40:31–9.
Monteiro V, Cunha TM. Urachal carcinoma: imaging findings. Acta Radiol Short Rep. 2012;1.
Loizzo D, Pandolfo SD, Crocerossa F, Guruli G, Ferro M, Paul AK, et al. Current management of Urachal Carcinoma: an evidence-based Guide for Clinical Practice. Eur Urol Open Sci. 2022;39:1–6.
Aggarwal A, Agarwal S, Pandey S, Sankhwar S. Urachal adenocarcinoma. BMJ Case Rep. 2018;2018.
Bruins HM, Visser O, Ploeg M, Hulsbergen-van de Kaa CA, Kiemeney LA, Witjes JA. The clinical epidemiology of urachal carcinoma: results of a large, population based study. J Urol. 2012;188:1102–7.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
C.W., T.A. and X.M. collected the data. C.W. and T.A. drafted the manuscript. X.M. reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the West China Hospital (2019(1085)) and informed consent was obtained from the patient’s parents.
Abbreviations
Not applicable.
Consent for publication
Written informed consent was obtained from the parents for the publication of this case report and accompanying images.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, C., An, T. & Ma, X. Urachal adenocarcinoma in an adolescent boy: a case report. BMC Pediatr 24, 554 (2024). https://doi.org/10.1186/s12887-024-05021-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-024-05021-5