Abstract
Background
Higher plasma levels of natriuretic peptides (NPs) have been associated with reduced anxiety in experimental research and a number of patient samples. As NP levels are elevated in heart failure patients, we investigate whether this elevation is related to anxiety in patients with heart failure with preserved ejection fraction (HFpEF).
Methods
Post-hoc regression and mediation analyses were conducted, using data of 422 patients with HFpEF from the randomized, placebo-controlled, double-blinded, two-armed, multicentre aldosterone in diastolic heart failure trial, testing associations and their mediators between the N-terminal B-type natriuretic peptide (NT-proBNP) and anxiety at baseline and over 12-month follow-up. Anxiety was measured by the Hospital Anxiety and Depression Scale (HADS), social support by the ENRICHD Social Support Inventory and physical functioning by the Short Form 36 Health Survey.
Results
The mean age of the study population was 66.8 ± 7.6 years, 47.6% were male and 86.0% had NYHA class II. NT-proBNP showed a weak negative correlation with HADS anxiety scores at baseline (r = − 0.087; p = 0.092), which was significant (r = − 0.165; p = 0.028) in men but not in women. NT-proBNP also tended to predict lower anxiety at 12-months in men. On the other hand, higher anxiety at baseline was associated with lower NT-proBNP scores 12 months later (r = − 0.116; p = 0.026). All associations lost significance in multivariate regression for age, perceived social support (ESSI), physical function (SF-36) and study arm. Mediation analyses revealed that social support acts as a full mediator for the link between NT-proBNP levels and anxiety.
Conclusion
The mechanisms linking NT-proBNP to anxiety may be more complex than originally assumed. While effects of NT-proBNP on anxiety may be mediated by perceived social support, there may be an additional negative effect of anxiety on NT-proBNP. Future research should consider this possible bi-directionality of the association and assess the potential influence of gender, social support, oxytocin and vagal tone on the interaction of anxiety and natriuretic peptide levels.
Trial Registration http://www.controlled-trials.com (ISRCTN94726526) on 07/11/2006.
Eudra-CT-number: 2006–002,605-31.
Similar content being viewed by others
Background
Heart failure is a leading cause of morbidity and mortality and its increasing prevalence places an enormous burden on the health care system and society [1, 2]. Epidemiologic studies indicate that up to half of patients with heart failure have a left ventricular ejection fraction (LVEF) of at least 50%, which is referred to as heart failure with preserved left ventricular ejection fraction (HFpEF). However, there are considerably fewer data on its etiology and therapy compared to heart failure with reduced LVEF (HFrEF). Furthermore, a growing body of research points to a mutual deterioration of mental health problems and cardiovascular diseases [3,4,5]. Patients with heart failure show an increased prevalence of reported anxiety. In this population the data vary between 6 and 72% with an average prevalence of 32%. However, prevalence partly depends on the respective measurement instrument and definition of elevated anxiety [6]. Consideration of comorbid anxiety disorders may be of prognostic value as they may increase the risk of developing or aggravating heart failure and are linked to adverse medical and functional outcomes [7, 8].
Natriuretic peptides secreted in response to increased cardiac stress are widely used indicators of cardiac disease severity. Consequently, one might expect higher levels of these peptides to be associated with an increase in psychological distress, including more symptoms of anxiety or depression. Interestingly though, a growing body of research indicates that higher plasma levels of these peptides may be associated with better mental health [9].
Natriuretic peptides and mental health
Through their effect on renal, cardiovascular, neuronal and endocrine functions, natriuretic peptides such as atrial natriuretic peptide (ANP) and B-type natriuretic peptide (BNP) play a crucial role in the regulation of blood pressure and fluid balance [10]. During BNP secretion, the precursor peptide ProBNP is equimolarly cleaved into BNP and the biologically inactive NT-proBNP (amino-terminal-cleavage-fragment of BNP). Since the latter is eliminated exclusively renally and has a higher concentration and longer half-life in plasma/serum than BNP, it has established itself as the preferred measurement value compared to BNP.
Interestingly, they seem to be associated with anxiety as well. For example, Herrmann-Lingen et al. [11] found a negative correlation between pro-ANP levels and self-assessed anxiety in a mixed sample of patients with cardiovascular risk factors or diagnosed heart failure. In the patients from the DIAST-CHF study with risk factors for HFpEF, higher plasma levels of mid-regional proANP were significantly associated with reduced anxiety and for NT-proBNP a trend towards reduced anxiety was observed [12].
Effects on the HPA axis
One explanatory approach for this possible anxiolytic effect deals with the inhibiting effect on the stress-sensitive hypothalamic–pituitary–adrenal axis (HPA axis) and sympathetic tone, which became apparent in various behavioural studies in rats and in clinical studies with patients suffering from panic disorder [13,14,15,16,17]. In line with these results, an anti-ANP serum administered to rats prior to a stress response significantly increased the stress-induced secretion of Adreno-corticotropic hormone (ACTH) and Corticosterone compared to rats with physiological ANP function [18]. Conversely, in humans, administration of ANP prior to pharmacological induction of a panic attack using cholecystokinin tetrapeptide reduced the occurrence of panic attacks [15].
Although ANP and BNP show many similarities in structure and function, there are considerably fewer study results on psychological effects of BNP, compared to ANP. In patients with coronary heart disease and mild to moderate depressive symptoms Fangauf et al. [19] found a significant negative correlation between NT-proBNP levels and the subjective perception of anxiety, depression, fatigue, physical pain and (poor) mental health, which persisted after multivariate adjustment. Furthermore, in a follow-up analysis, they observed that higher baseline levels of NT-proBNP were associated with persistently lower anxiety scores over 24 months [20].
Based on the literature suggesting a negative correlation between natriuretic peptides and anxiety, our primary hypothesis was that higher NT-proBNP plasma levels are correlated with reduced anxiety in HFpEF patients. Although research to date supports an anxiolytic effect of natriuretic peptides, increased anxiety may, conversely, have a suppressive effect on the peptides’ release or production. As most of the previous findings on this relationship come from exclusively cross-sectional studies, longitudinal data from this study may shed new light on a possible bidirectional association between anxiety and NT-proBNP levels, providing the basis for a better understanding of the underlying mechanisms.
Methods
Study design
The Aldosterone Receptor Blockade in Diastolic Heart Failure (Aldo-DHF) trial was a multicenter, prospective, randomized, double-blind, placebo-controlled, two-armed study in patients diagnosed with chronic heart failure stage II or III according to the New York Heart Association (NYHA) and left ventricular ejection fraction > 50%. Additional inclusion criteria were a minimum age of 50 years and echocardiographic evidence of diastolic dysfunction (≥ Grade I) or atrial fibrillation. Main exclusion criteria were various indicators of poor health. The study design has been published previously [21].
Aldo-DHF was conducted in accordance with Good Clinical Practice guidelines and the Declaration of Helsinki. The ethics committees of all participating centers reviewed and accepted the trial protocol and all patients gave their written informed consent before being included in the trial. The trial randomized 422 patients to either 25 mg daily of the aldosterone receptor blocker spironolactone or placebo. Primary endpoints of the study were changes in diastolic left ventricular function and exercise capacity after 12 months.
Clinical assessment
Medical history, clinical examination, electrocardiography, echocardiography, laboratory diagnostics, spiroergometry, six-minute walking test and quality of life assessment were performed at baseline and after 6 and 12 months. Blood was drawn from a cubital vein in resting, non-fasting patients and centrifuged ten minutes in an Eppendorf 5702R centrifuge. The plasma thus obtained was pipetted off and stored at − 80 °C until being analyzed. In the case of blood analyses at external sites, the cold chain was checked during the transport of the blood samples with the help of the company B.R.A.H.M.S. AG Hennigsdorf. Plasma concentrations of NT-proBNP were determined centrally at the University of Göttingen Medical Center using the Elecsys® proBNP test from Roche Diagnostics. The test is a non-competitive electrochemiluminescent immunoassay whose specific polyclonal antibodies bind to certain regions of NT-proBNP.
Psychosocial assessment
The patients' psychosocial status was assessed using the validated German versions of standardized widely used self-rating questionnaires. Anxiety was assessed by the anxiety subscale of the Hospital Anxiety and Depression Scale (HADS) in its German version [22]. The anxiety subscale (HADS-A) consists of seven items asking for symptoms of generalized anxiety and panic, the frequency or extent of which are assessed during the previous week using a 4-level Likert scale (0–3 points) [23]. For evaluation purposes, the 7 item values are summed up to give the sum value for HADS-A with a value range from 0 to 21. Higher values indicate more anxiety [24]. As a cut-off value, a sum value of 8 yields an optimal balance of sensitivity and specificity [25, 26].
Perceived social support was assessed by the German version [27] of the ENRICHD Social Support Inventory (ESSI). The ESSI was developed for patients after myocardial infarction and asks about their perceived emotional support using a 5-point Likert scale. For evaluation, the assigned item values are summed up, with higher values indicating more social support in the patient's environment. A scale value of ≤ 18 and a scale value of ≤ 3 for at least 2 items corresponds to low social support [28].
The Short Form 36 Health Questionnaire (SF-36) is a 36-item, generic instrument designed to measure health-related quality of life related to the last four weeks. It contains eight subscales, one of which assesses physical function [29]. The individual items are answered using Likert scales and eventually coded into a numerical value from 0 to 100, whereby a higher numerical value corresponds to a better self-rated state of health. Finally, a mean score is calculated from the item scores for each subscale [30]. The German version was validated by Bullinger et al. [31].
Data analysis
The statistical analyses were performed with IBM SPSS Statistics Versions 25–28 and the significance level was set at 5% (2-sided). Missing values were excluded pairwise for correlation analyses and listwise for regression and mediation analyses.
Normality was tested using the Kolmogorov–Smirnov and Shapiro–Wilk test. As the distribution of NT-proBNP values was severely skewed, they were log-transformed for tests that require normality. The results of the power analysis for the Aldo-DHF study were reported in the previously published study design.
Demographic and clinical data are presented as means ± standard deviations, median and interquartile range or frequencies and percentages, as appropriate. We used bivariate correlations according to Pearson to evaluate the association between log-transformed values of the biomarker NT-proBNP and scores of the subscale "anxiety" of the HADS at baseline and at 12 months. To identify potentially confounding variables, we tested perceived social support (ESSI), age, BMI and objective severity markers of the physical disease (LVEF, E/A ratio, 6-min walking distance, peak VO2). Of these, social support significantly correlated with HADS anxiety and NT-proBNP at baseline and at 12 months and was therefore included in the respective regression models. All multivariate regression models were adjusted for age and in the full cohort additionally for sex as a standard. The longitudinal regression models were adjusted for study arm to test for potential impact of treatment with spironolactone. Finally, we adjusted for SF-36 Physical function as a measure of perceived disease severity to disentangle the potential relevance of two opposite processes: On the one hand, the literature suggests that BNP may have an anxiety-relieving effect. On the other hand, (NT-pro)BNP reflects increased cardiac stress, indicating more severe disease, which can in turn be expected to increase anxiety.
Based on recent data from Fangauf et al. [20] suggesting a sex difference in the association of NT-proBNP and anxiety we repeated the analyses separately for men and women.
Mediation analyses for social support were performed using the bias-corrected bootstrap confidence interval test [32]. Unstandardized indirect effects were computed for each of 1000 bootstrapped samples and significance was tested by means of 95% confidence intervals (CI). The total effect is the effect of x on y without the mediator. The direct effect is the effect of x on y with the mediator in the model and the indirect effect is the actual mediation effect. A mediation effect is likely involved if the total and direct effect is not significant and the indirect effect is significant.
Results
Descriptive statistics
The ALDO-DHF study enrolled 422 patients with an average age of 66.8 years, a mean E/A ratio of 12.8 and a BMI of 28.9 kg/m2. The average systolic blood pressure was 135 mmHg and the maximum oxygen uptake (peak VO2) was 16.4 ml/kg/min. Patients had a median NT-proBNP value of 158.4 pg/ml and an average HADS anxiety score of 5.3. The majority of patients was classified as NYHA II (86.2%) and diagnosed with hypertension (91.7%). HADS anxiety, social support and median NT-proBNP plasma levels did not significantly differ between female and male patients. Women showed a significantly higher E/A ratio, a lower systolic blood pressure and better physical functioning on the SF-36. Men were more likely to have CAD or diabetes mellitus (Table 1).
Correlations and multiple regression analyses between log NT-proBNP at baseline and HADS anxiety at baseline and after 12 months
Correlation analyses showed weak and non-significant associations of higher NT-proBNP at baseline with lower HADS anxiety scores at baseline and after 12 months (r = − 0.087, p = 0.09 and r = − 0.076, p = 0.15). When tested separately in the male subgroup, the association at baseline was significant (r = − 0.165, p = 0.03) and NT-proBNP at baseline also showed a marginal correlation with HADS-anxiety scores 12 months later (r = − 0.149, p = 0.06). In contrast, none of these associations were significant in female patients.
In multivariate regression models for the full cohort, the weak associations disappeared, and social support and physical function turned out to be independent predictors of low anxiety at baseline and 12 months later (Table 2).
A similar result was observed in the male subgroup, where interestingly spironolactone treatment turned out to be an additional significant predictor for lower anxiety after 12 months (Table 3).
Since both, social support and age correlated positively with NT-proBNP and negatively with the HADS anxiety scale in bivariate analyses (Fig. 1), we concluded that social support might either act as a mediator or as a confounder, which might influence the correlation.
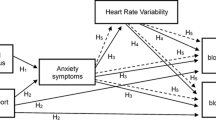
Therefore, we computed a mediation analysis with log-transformed NT-proBNP at baseline as the independent variable, HADS anxiety at baseline as the dependent variable and social support as the potential mediator. While the direct effect of NT-proBNP on HADS anxiety at baseline was not significant (B = -0.288; CI: -1.1095; 0.5334), we found that the relationship between NT-proBNP and HADS anxiety at baseline was mediated by social support with an indirect effect of -0.477 (CI − 0.8770; − 0.1087) (Fig. 2), which got weaker but stayed significant when controlled for age (B = − 0.468; CI − 0.9196; − 0.0488).
Mediation effect of social support for the association between NT-proBNP and HADS anxiety. Path a: Prediction of social support by NT-proBNP. Path b: Prediction of HADS anxiety by social support. \Path c’: Prediction of HADS anxiety by NT-proBNP with social support in the model (Direct effect). Path c: Prediction of HADS anxiety by NT-proBNP without social support in the model (Total effect). Indirect effect: Actual mediation effect by social support. * CI (-0.8770; -0.1087); ** p < 0.01
Similarly, the relationship between NT-proBNP at baseline and HADS anxiety after 12 months was mediated by social support with an indirect effect of − 0.479 (CI − 0.8676; − 0.1182), which stayed significant when controlled for age.
Correlations and multiple regression analyses between HADS anxiety at baseline and log NT-proBNP after 12 months
The longitudinal structure of our study allowed us to examine the potential influence of anxiety at baseline on NT-proBNP levels after 12 months. Interestingly, higher HADS anxiety scores at baseline showed a clearly significant association with lower NT-proBNP values after 12 months (r = − 0.116, p = 0.03), which became even stronger when only male patients were tested (r = − 0.182, p = 0.01). In the full cohort, after multivariate adjustment for social support, age, sex, physical function and study arm, however, these associations disappeared (Table 4). The same applies if only the male patients were tested.
Mediation analyses for this association showed that the indirect effect of social support in the full cohort was not significant. For male patients, the small but initially significant indirect effect of − 0.007 (CI − 0.0169; − 0.0005) disappeared when adjusted for age.
To complement the previous results, we tested whether the data collected at six months corresponded to the associations at baseline and at 12 months. NT-proBNP at baseline significantly predicted anxiety at six months both in the full cohort (r = − 0.100; p = 0.060) and for men only (r = − 0.167; p = 0.032). When looking at anxiety at baseline as predictor and NT-proBNP as dependent variable, correlations remained negative in the full cohort (r = − 0.041; p = 0.431) with a statistical trend in the men (r = − 0.132; p = 0.079).
Discussion
In the present study, we found weak correlations between higher NT-proBNP levels and lower scores on the HADS anxiety scale at baseline and after 12 months, which were, however, not clearly significant. This may be due to the typically observed small effect size and the somewhat smaller patient number compared to studies that found significant effects. When the male subjects were tested separately, the associations became significant or marginally significant and of similar strength as described in previous studies [12, 19] while for the female patients no significant associations were observed. Our findings are consistent with previous results concerning the association of higher plasma levels of natriuretic peptides with reduced anxiety [12, 15, 16, 19]. However, the observed correlations lost significance after adjustment for social support, age, physical function, sex and study arm, which suggests that, at least in patients with HFpEF, the mechanisms possibly linking NT-proBNP to anxiety may be more complex than originally assumed.
Correlation analyses showed that social support, as measured by ESSI, and age were positively associated with NT-proBNP levels and negatively with HADS-anxiety scores. Furthermore, mediation analysis revealed that social support acts as a full mediator, which, together with the confounding variable age, may indirectly link HADS anxiety with NT-proBNP levels. There are different explanatory approaches on how social support might act as a mediator. Possibly, BNP might exert a biological effect on the perception of social interactions leading to more trust and better self-rated social support, which in turn results in less anxiety. This effect could reflect an interaction between BNP and the neuropeptide oxytocin. Beside its main role in reproduction, social bonding and trusting behaviour, a growing body of evidence indicates that oxytocin is involved in cardiovascular regulation and fluid homeostasis [33, 34]. In an experimental model of postinfarction heart failure in rats, Wsol et al. [35] found a direct correlation between intracardiac oxytocin activation and natriuretic peptide expression. The observed heart failure four weeks after induced myocardial infarction was associated with an increase in ANP, BNP, and plasma NT-proBNP. At the same time, they observed an increase in the level of oxytocin in the muscle tissue of the right ventricle. They concluded that oxytocin exerts its cardioprotective effect in part by inducing secretion of natriuretic peptides. These results may indicate that oxytocin acts as a confounding variable that induces secretion of BNP and at the same time decreases anxiety directly or, alternatively, indirectly via a more positive perception of social support. Although a growing number of studies support a negative correlation between anxiety or stress and oxytocin levels [36, 37], study results are inconclusive and the directionality of the association is not clarified, yet. A possible explanation for an anxiolytic effect of oxytocin could be its effect on the amygdala. Higher blood oxytocin levels are associated with smaller volumes and attenuated activity in the central amygdala [38] and reduced amygdala responses to threatening social stimuli [39, 40]. Furthermore, the association seems to be moderated by gender [41]. Consequently, BNP might not have a causal effect on anxiety but could just indicate higher oxytocin levels secreted at the same time, which in turn exert an anxiolytic effect e. g. via reduced amygdala activation.
Alternatively, patients with elevated BNP due to more severe heart failure may benefit from a secondary disease gain if the disease leads to more social attention and support. In turn, greater social support may reduce symptoms of anxiety [42, 43].
Social support, together with age, might as well act as confounders that produce a spurious correlation between (NT-pro)BNP and anxiety. Possibly, persons who experience more social support might be more resilient and thus more capable of dealing with heart failure by increased secretion of BNP.
Another mechanism that could establish a causal link between natriuretic peptides, social support and anxiety is the vagus nerve. Part of the cardioprotective effect of BNP unfolds through its sympatholytic effect and the enhancement of cardiac vagal neurotransmission. BNP has been shown to enhance reflex bradycardia upon stimulation of the peripheral right vagus nerve [44] and electrical vagal nerve stimulation in rats with induced chronic heart failure resulted in an increase in LVEF and concomitant lower serum BNP [45]. In addition, results from a randomized controlled longitudinal field experiment on positive emotions through meditation suggest that an increase in positive emotions leads to higher vagotone and that this effect is mediated by a more favorable perception of social connections. Thus, the authors conclude that positive emotions, valuable social connections, and higher vagotone enhance each other in a self-reinforcing upward spiral dynamic [46]. Similarly, individuals with increased cardiac vagotone were more likely to seek social support in response to a sad experience and were less likely to experience anger. The authors explain the latter with the hypothesis that individuals with higher cardiac vagotone interpret social situations as less hostile [47]. Furthermore, there is evidence that vagus nerve stimulation reduces anxiety in treatment-resistant anxiety patients and improves quality of life in patients with heart failure [48, 49].
There is no sufficient explanation for the observed sex difference at present. In a cohort of patients with cardiovascular risk factors Sadlonova et al. [50] found a negative correlation between serum vasopressin levels and perceived anxiety only for male subjects, but not for female subjects as well. Fangauf et al. [20] found differences in men and women concerning the interaction of NT-proBNP levels and anxiety over time. Furthermore, a study of healthy undergraduates with academic stress revealed a significant interaction between cortisol elevation during exam stress and concomitant decreased NT-proBNP levels. Interestingly, only males showed a significant inverse relationship between the percent change in circulating cortisol and NT-proBNP from control to exam day. In the female group, this inverse relationship was not statistically significant [51]. The underlying mechanism for these sex differences is not known, yet, and should be addressed in future research.
The finding that treatment with the mineralocorticoid receptor antagonist (MRA) spironolactone significantly predicted lower anxiety after 12 months in the male subgroup is partly consistent with findings of previous studies suggesting an anxiolytic effect of MRAs and an anxiogenic effect of aldosterone. Long-term treatment with aldosterone in rats increased anxiety-like behavior [52] and patients with primary hyperaldosteronism tend to present with more symptoms of depression and anxiety than the general population [53,54,55]. In studies with both male rats [56] and patients with primary hyperaldosteronism [57], treatment with an MRA was associated with reduced anxiety. In our study, spironolactone treatment did not significantly predict lower anxiety after 12 months in the full cohort and HADS anxiety scores after 12 months did not significantly differ between the control and treatment groups. The underlying pathophysiology of the association between MRA treatment and anxiety is not entirely understood and whether the observed association in our study reflects an actual effect of spironolactone or e.g. a random significance or inclusion bias remains unclear.
Our primary research question was based on the literature suggesting that natriuretic peptides have a protective effect on perceived anxiety. However, as most previous studies in cardiac patient samples were cross-sectional only, the directionality of the observed associations was not completely clear. Interestingly, while we only observed a non-significant trend for the association between NT-proBNP values at baseline and perceived anxiety 12 months later, there was a significant negative correlation between anxiety at baseline and NT-proBNP levels 12 months later. This finding has not been reported before. Possibly, a moderate level of anxiety may have a positive effect by inducing patients to adopt a healthier lifestyle and to seek medical advice more closely, which could be associated with decreasing (NT-pro)BNP levels in the study cohort of the present study. Whether anxiety has a positive effect on lifestyle and treatment adherence in patients with chronic heart failure and is thus reflected in NT-proBNP progression should be the subject of future studies. On the other hand, increased anxiety or a possibly associated elevated stress level might have a suppressive effect on the production/secretion of (NT-pro)BNP via as yet unknown mechanisms [51]. Brouwers et al. [58] observed a negative, though non-significant, correlation between baseline HADS anxiety and NT-proBNP levels in 95 patients with systolic heart failure. In contrast to our results, their follow-up data collected 9 months later, did not reveal any significant interaction between HADS anxiety scores and NT-proBNP levels over time. Furthermore, Müller-Tasch et al. [59] did not find an association between NT-proBNP and anxiety in either the cross-sectional or the longitudinal analyses. Possible reasons for the lack of significance in these two studies might be low power due to the small sample sizes and the fact that all their patients had been diagnosed with HFrEF rather than HFpEF. Clinical severity and NT-proBNP levels were considerably higher in the Brouwers et al. and Müller-Tasch et al. studies than in ours, while previous studies showing significant associations included substantial percentages of patients with no manifest heart failure. This may indicate that with increasing severity of heart failure the association described in more mildly ill patients is lost, e.g., by downregulation of central natriuretic peptide-receptors in response to permanently elevated peptide levels. In contrast, Herrmann-Lingen et al. [11] found that high plasma levels of N-Terminal Pro-Atrial Natriuretic Peptide were associated with low anxiety in severe heart failure, as well. Further studies are needed to clarify whether our results are transferable to patients with more severe heart failure and higher NT-proBNP-levels. When more severely ill patients are included, we suggest controlling for impairments in physical function, as this could have an anxiogenic effect and thus mask a potential anxiolytic effect of BNP.
Strengths and limitations
There are several limitations to our study findings. They were generated by means of post-hoc analyses, therefore no cause-effect relationships can be concluded from the observed associations. The majority of the patients enrolled in the ALDO-DHF study was diagnosed with NYHA Class II and less frequently NYHA Class III and was at least 50 years old. Additionally, patients whose mental state might have interfered with study adherence were excluded, as well. Consequently, our results cannot easily be generalized to younger or more severely ill patient populations. To investigate the extent to which someone suffers from anxiety, a self-report measure instead of clinical diagnostic interviews was applied. Whether NT-proBNP is related to a clinical diagnosis of anxiety disorder cannot directly be derived from our results. Although our correlation analyses between NT-proBNP and anxiety are consistent with previous findings, we could not definitely confirm them, as our results did not persist after adjustment in multiple regression analyses. Finally, due to the rather weak effects observed in our sample, it remains unclear whether they reflect real correlations or random variations. A strength is that to our knowledge, this is the first investigation of the association of NT-proBNP and symptoms of anxiety in well-characterized patients with HFpEF. Furthermore, the longitudinal nature of our data provides additional insight into the direction of the relationship between these two variables.
Conclusions
The inconsistent associations between NT-proBNP and anxiety observed in our study and others point out that the relationship is still insufficiently understood. Interestingly, our findings provide a first hint that the association between anxiety and NT-proBNP levels may be bidirectional. More research on how cardiac-released natriuretic peptides may exert their anxiolytic effect and if anxiety impairs cardiac prognosis by suppressing counterregulatory BNP secretion is needed. Furthermore, it remains unclear how the associations between anxiety and (NT-pro)BNP levels are mediated. Therefore, potential interactions between natriuretic peptides, oxytocin, social support and anxiety need to be explored in future research, also considering possible age and sex differences.
Availability of data and materials
The datasets analyzed during the current study are not publicly available because they contain reidentifiable patient data and have not been approved for publication by the patients. Data are however available from the corresponding author on reasonable request.
Abbreviations
- LVEF:
-
Left ventricular ejection fraction
- HFpEF:
-
Heart failure with preserved left ventricular ejection fraction
- HFrEF:
-
Heart failure with reduced left ventricular ejection fraction
- ANP:
-
Atrial natriuretic peptide
- BNP:
-
B-type natriuretic peptide
- NT-proBNP:
-
Amino-terminal-cleavage-fragment of B-type natriuretic peptide
- DIAST-SHF:
-
Study on prevalence and clinical course of diastolic dysfunction and diastolic heart failure
- HPA axis:
-
Hypothalamic–pituitary–adrenal axis
- ACTH:
-
Adreno-corticotropic hormone
- NYHA:
-
New York Heart Association
- Aldo-DHF:
-
Aldosterone receptor blockade in diastolic heart failure trial
- HADS:
-
Hospital Anxiety and Depression Scale
- ESSI:
-
ENRICHD Social Support Inventory
- SF-36:
-
Short Form 36 Health Questionnaire
- E/A ratio:
-
Ratio of the early (E) to late (A) ventricular filling velocities
- Peak VO2:
-
Maximum oxygen uptake
- BMI:
-
Body mass index
- MRA:
-
Mineralocorticoid receptor antagonist
References
Savarese G, Lund LH. Global public health burden of heart failure. Card Fail Rev. 2017;3(1):7–11.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2021;42(36):3599–726.
Lichtman JH, Froelicher ES, Blumenthal JA, Carney RM, Doering LV, Frasure-Smith N, et al. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations. Circulation. 2014;129(12):1350–69.
Albus C, Waller C, Fritzsche K, Gunold H, Haass M, Hamann B, et al. Significance of psychosocial factors in cardiology: update 2018. Clin Res Cardiol. 2019;108(11):1175–96.
Levine GN, Cohen BE, Commodore-Mensah Y, Fleury J, Huffman JC, Khalid U, et al. Psychological health, well-being, and the mind-heart-body connection: a scientific statement from the American Heart Association. Circulation. 2021;143(10):e763–83.
Easton K, Coventry P, Lovell K, Carter LA, Deaton C. Prevalence and measurement of anxiety in samples of patients with heart failure. J Cardiovasc Nurs. 2016;31(4):367–79.
Garfield LD, Scherrer JF, Hauptman PJ, Freedland KE, Chrusciel T, Balasubramanian S, et al. Association of anxiety disorders and depression with incident heart failure. Psychosom Med. 2014;76(2):128–36.
Celano CM, Villegas AC, Albanese AM, Gaggin HK, Huffman JC. Depression and anxiety in heart failure: a review. Harv Rev Psychiatry. 2018;26(4):175–84.
Meyer T, Herrmann-Lingen C. Chapter five - natriuretic peptides in anxiety and panic disorder. In: Litwack G, editor. Vitamins and hormones. Cambridge: Academic Press; 2017. p. 131–45.
Pandey KN. Molecular and genetic aspects of guanylyl cyclase natriuretic peptide receptor-A in regulation of blood pressure and renal function. Physiol Genom. 2018;50(11):913–28.
Herrmann-Lingen C, Binder L, Klinge M, Sander J, Schenker W, Beyermann B, et al. High plasma levels of N-terminal pro-atrial natriuretic peptide associated with low anxiety in severe heart failure. Psychosom Med. 2003;65(4):517–22.
Meyer T, Herrrmann-Lingen C, Chavanon ML, Nolte K, Pasedach CA, Binder L, et al. Higher plasma levels of MR-pro-atrial natriuretic peptide are linked to less anxiety: results from the observational DIAST-CHF study. Clin Res Cardiol. 2015;104(7):574–81.
Butler PD, Weiss JM, Stout JC, Nemeroff CB. Corticotropin-releasing factor produces fear-enhancing and behavioral activating effects following infusion into the locus coeruleus. J Neurosci. 1990;10(1):176–83.
Kellner M, Wiedemann K, Holsboer F. Atrial natriuretic factor inhibits the CRH-stimulated secretion of ACTH and cortisol in man. Life Sci. 1992;50(24):1835–42.
Ströhle A, Kellner M, Holsboer F, Wiedemann K. Anxiolytic activity of atrial natriuretic peptide in patients with panic disorder. Am J Psychiatry. 2001;158(9):1514–6.
Wiedemann K, Jahn H, Yassouridis A, Kellner M. Anxiolyticlike effects of atrial natriuretic peptide on cholecystokinin Tetrapeptide-induced panic attacks: preliminary findings. Arch Gen Psychiatry. 2001;58(4):371–7.
Arlt J, Jahn H, Kellner M, Ströhle A, Yassouridis A, Wiedemann K. Modulation of sympathetic activity by corticotropin-releasing hormone and atrial natriuretic peptide. Neuropeptides. 2003;37(6):362–8.
Antoni FA, Hunter EF, Lowry PJ, Noble JM, Seckl JR. Atriopeptin: an endogenous corticotropin-release inhibiting hormone. Endocrinology. 1992;130(3):1753–5.
Fangauf SV, Herbeck B, Meyer T, Albus C, Binder L, Deter HC, et al. Associations of NT-proBNP and parameters of mental health in depressed coronary artery disease patients. Psychoneuroendocrinology. 2018;1(96):188–94.
Fangauf SV, Meyer T, Albus C, Binder L, Deter HC, Ladwig KH, et al. Longitudinal relationship between B-type natriuretic peptide and anxiety in coronary heart disease patients with depression. J Psychosom Res. 2019;1(123): 109728.
Edelmann F, Schmidt AG, Gelbrich G, Binder L, Herrmann-Lingen C, Halle M, et al. Rationale and design of the ‘aldosterone receptor blockade in diastolic heart failure’ trial: a double-blind, randomized, placebo-controlled, parallel group study to determine the effects of spironolactone on exercise capacity and diastolic function in patients with symptomatic diastolic heart failure (Aldo-DHF). Eur J Heart Fail. 2010;12(8):874–82.
Herrmann C, Buss U, Snaith RP. HADS-D - hospital anxiety and depression scale–Deutsche version: Ein Fragebogen zur Erfassung von Angst und Depressivität in der somatischen Medizin. Huber. 1995.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70.
Snaith RP. The hospital anxiety and depression scale. Health Qual Life Outcomes. 2003;1(1):29.
Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the hospital anxiety and depression scale: an updated literature review. J Psychosom Res. 2002;52(2):69–77.
Hinz A, Brähler E. Normative values for the hospital anxiety and depression scale (HADS) in the general German population. J Psychosom Res. 2011;71(2):74–8.
Cordes A, Herrmann-Lingen C, Büchner B, Hessel A. Repräsentative Normierung des ENRICHD- Social-Support-Instrument (ESSI)-Deutsche Version. Klin Diagn Eval. 2009;1(2):16–32.
Kendel F, Spaderna H, Sieverding M, Dunkel A, Lehmkuhl E, Hetzer R, et al. Eine deutsche adaptation des ENRICHD social support inventory (ESSI). Diagnostica. 2011;57(2):99–106.
Tarlov AR, Ware JE, Greenfield S, Nelson EC, Perrin E, Zubkoff M. The medical outcomes study. An application of methods for monitoring the results of medical care. JAMA. 1989;262(7):925–30.
Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. conceptual framework and item selection. Med Care. 1992;30(6):473–83.
Bullinger M, Kirchberger I, Ware J. Der deutsche SF-36 Health Survey Übersetzung und psychometrische Testung eines krankheitsübergreifenden Instruments zur Erfassung der gesundheitsbezogenen Lebensqualität. Z Für Gesundheitswissenschaften J Public Health. 1995;3(1):21.
Hayes AF, Scharkow M. The relative trustworthiness of inferential tests of the indirect effect in statistical mediation analysis: Does method really matter? Psychol Sci. 2013;24(10):1918–27.
Gutkowska J, Jankowski M, Lambert C, Mukaddam-Daher S, Zingg HH, McCann SM. Oxytocin releases atrial natriuretic peptide by combining with oxytocin receptors in the heart. Proc Natl Acad Sci. 1997;94(21):11704–9.
Wang P, Wang SC, Yang H, Lv C, Jia S, Liu X, et al. Therapeutic potential of oxytocin in atherosclerotic cardiovascular disease: mechanisms and signaling pathways. Front Neurosci. 2019. https://doi.org/10.3389/fnins.2019.00454.
Wsol A, Kasarello K, Kuch M, Gala K, Cudnoch-Jedrzejewska A. Increased activity of the intracardiac oxytocinergic system in the development of postinfarction heart failure. BioMed Res Int. 2016. https://doi.org/10.1155/2016/3652068.
Anderberg UM, Uvnäs-Moberg K. Plasma oxytocin levels in female fibromyalgia syndrome patients. Z Für Rheumatol. 2000;59(6):373–9.
Bernhard A, van der Merwe C, Ackermann K, Martinelli A, Neumann ID, Freitag CM. Adolescent oxytocin response to stress and its behavioral and endocrine correlates. Horm Behav. 2018;1(105):157–65.
Lancaster K, Goldbeck L, Pournajafi-Nazarloo H, Connelly JJ, Carter CS, Morris JP. The role of endogenous oxytocin in anxiolysis: structural and functional correlates. Biol Psychiatry Cogn Neurosci Neuroimaging. 2018;3(7):618–25.
Domes G, Heinrichs M, Gläscher J, Büchel C, Braus DF, Herpertz SC. Oxytocin attenuates amygdala responses to emotional faces regardless of valence. Biol Psychiatry. 2007;62(10):1187–90.
Radke S, Volman I, Kokal I, Roelofs K, de Bruijn ERA, Toni I. Oxytocin reduces amygdala responses during threat approach. Psychoneuroendocrinology. 2017;1(79):160–6.
Weisman O, Zagoory-Sharon O, Schneiderman I, Gordon I, Feldman R. Plasma oxytocin distributions in a large cohort of women and men and their gender-specific associations with anxiety. Psychoneuroendocrinology. 2013;38(5):694–701.
Roohafza HR, Afshar H, Keshteli AH, Mohammadi N, Feizi A, Taslimi M, et al. What’s the role of perceived social support and coping styles in depression and anxiety? J Res Med Sci. 2014;19(10):944–9.
Shao R, He P, Ling B, Tan L, Xu L, Hou Y, et al. Prevalence of depression and anxiety and correlations between depression, anxiety, family functioning, social support and coping styles among Chinese medical students. BMC Psychol. 2020;8(1):38.
Herring N, Paterson DJ. Neuromodulators of peripheral cardiac sympatho-vagal balance. Exp Physiol. 2009;94(1):46–53.
Li D, Lu C-J, Hao G, Wright H, Woodward L, Liu K, et al. Efficacy of B-type natriuretic peptide is coupled to phosphodiesterase 2A in cardiac sympathetic neurons. Hypertension. 2015;66(1):190–8.
Kok BE, Coffey KA, Cohn MA, Catalino LI, Vacharkulksemsuk T, Algoe SB, et al. How positive emotions build physical health: perceived positive social connections account for the upward spiral between positive emotions and vagal tone. Psychol Sci. 2013;24(7):1123–32.
Geisler FCM, Kubiak T, Siewert K, Weber H. Cardiac vagal tone is associated with social engagement and self-regulation. Biol Psychol. 2013;93(2):279–86.
George MS, Ward HE, Ninan PT, Pollack M, Nahas Z, Anderson B, et al. A pilot study of vagus nerve stimulation (VNS) for treatment-resistant anxiety disorders. Brain Stimulat. 2008;1(2):112–21.
Schwartz PJ, De Ferrari GM, Sanzo A, Landolina M, Rordorf R, Raineri C, et al. Long term vagal stimulation in patients with advanced heart failure first experience in man. Eur J Heart Fail. 2008;10(9):884–91.
Sadlonova M, Meyer T, Binder L, Wachter R, Edelmann F, Herrmann-Lingen C. Higher plasma levels of CT-proAVP are linked to less anxiety in men but not women with cardiovascular risk factors: results from the observational Diast-CHF study. Psychoneuroendocrinology. 2019;101:272–7.
Amir O, Sagiv M, Eynon N, Yamin C, Rogowski O, Gerzy Y, et al. The response of circulating brain natriuretic peptide to academic stress in college students. Stress. 2010;13(1):83–90.
Hlavacova N, Jezova D. Chronic treatment with the mineralocorticoid hormone aldosterone results in increased anxiety-like behavior. Horm Behav. 2008;54(1):90–7.
Engler L, Adolf C, Heinrich DA, Brem AK, Riester A, Franke A, et al. Effects of chronically high levels of aldosterone on different cognitive dimensions: an investigation in patients with primary aldosteronism. Endocr Connect. 2019;8(4):407–15.
Apostolopoulou K, Künzel HE, Gerum S, Merkle K, Schulz S, Fischer E, et al. Gender differences in anxiety and depressive symptoms in patients with primary hyperaldosteronism: a cross-sectional study. World J Biol Psychiatry. 2014;15(1):26–35.
Sonino N, Tomba E, Genesia ML, Bertello C, Mulatero P, Veglio F, et al. Psychological assessment of primary aldosteronism: a controlled study. J Clin Endocrinol Metab. 2011;96(6):E878–83.
Hlavacova N, Bakos J, Jezova D. Eplerenone, a selective mineralocorticoid receptor blocker, exerts anxiolytic effects accompanied by changes in stress hormone release. J Psychopharmacol Oxf Engl. 2010;24(5):779–86.
Murck H, Adolf C, Schneider A, Schlageter L, Heinrich D, Ritzel K, et al. Differential effects of reduced mineralocorticoid receptor activation by unilateral adrenalectomy vs mineralocorticoid antagonist treatment in patients with primary aldosteronism - Implications for depression and anxiety. J Psychiatr Res. 2021;1(137):376–82.
Brouwers C, Spindler H, Larsen ML, Eiskær H, Videbæk L, Pedersen MS, et al. Association between psychological measures and brain natriuretic peptide in heart failure patients. Scand Cardiovasc J. 2012;46(3):154–62.
Müller-Tasch T, Krug K, Peters-Klimm F. Associations between NT-proBNP and psychosocial factors in patients with chronic systolic heart failure. J Psychosom Res. 2021;1(143): 110385.
Acknowledgements
We acknowledge support by the Open Access Publication Funds of the University of Göttingen.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research did not receive any other specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Aldo-DHF was funded by the Federal Ministry of Education and Research Grant 01GI0205 (clinical trial program Aldo-DHF [FKZ 01KG0506]). The University of Göttingen was the formal sponsor.
Author information
Authors and Affiliations
Contributions
Conception and design of the research was performed by MW, AS and CHL. Acquisition of data was performed by FE and RW. Analyses and interpretation of the data were performed by MW, FE, AS, RW and CHL. Statistical analysis was performed by MW and CHL. Funding was obtained and the work was supervised by FE, RW and CHL. The manuscript was drafted by MW and CHL. For important intellectual content, the manuscript was critically revised by MW, DB, AS, RW, FE and CHL. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Aldo-DHF trial has been conducted in accordance with national laws and ICH guidelines for good clinical practice issued in June 1996 and CPMP/ICH/135/95 from September 1997, taking into account the Directive 2001/20/EC of the European Parliament and of the Council of 4 April 2001. All persons participating in the conduct of the trial committed themselves to consider the Declaration of Helsinki and all its revisions (including the Edinburgh Amendment from October 2000). The study protocol was approved by the Ethics Committee of the University of Göttingen Medical Center (#6/12/06) and all participating sites, i.e. the Ethics Committees at the Universities of Berlin (#566/06), Cologne (#06–229), and Würzburg (#179/06), and the Medical Associations of Hamburg (#M-311–06) and Munich (#411–06).
Consent for publication
Not applicable.
Competing interests
CHL is receiving royalties from Hogrefe Huber Publishers, Berne, for the German version of the Hospital Anxiety and Depression Scale. Over the past 3 years, he has been receiving lecture honoraria from Servier and Novartis. RW reports personal fees from Bayer, grants and personal fees from Boehringer Ingelheim, personal fees from Pfizer/BMS, other from Daiichi Sankyo, personal fees from Novartis, personal fees from Sanofi, personal fees from Servier, grants and personal fees from Medtronic, personal fees from Pharmacosmos, personal fees from CVRx, grants from German Federal Ministry for Education and Research, and grants from DFG, outside the submitted work. AS is receiving grants from the Oskar-Helene-Heim Foundation. MW, DB and FE report no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wilke, M.R., Broschmann, D., Sandek, A. et al. Longitudinal association between N-terminal B-type natriuretic peptide, anxiety and social support in patients with HFpEF: results from the multicentre randomized controlled Aldo-DHF trial. BMC Cardiovasc Disord 23, 184 (2023). https://doi.org/10.1186/s12872-023-03136-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03136-8