Abstract
Background
The microorganisms intended for use as probiotics in aquaculture should exert antimicrobial activity and be regarded as safe not only for the aquatic hosts but also for their surrounding environments and humans. The objective of this work was to investigate the antimicrobial/bacteriocin activity against fish pathogens, the antibiotic susceptibility, and the prevalence of virulence factors and detrimental enzymatic activities in 99 Lactic Acid Bacteria (LAB) (59 enterococci and 40 non-enterococci) isolated from aquatic animals regarded as human food.
Results
These LAB displayed a broad antimicrobial/bacteriocin activity against the main Gram-positive and Gram-negative fish pathogens. However, particular safety concerns based on antibiotic resistance and virulence factors were identified in the genus Enterococcus (86%) (Enterococcus faecalis, 100%; E. faecium, 79%). Antibiotic resistance was also found in the genera Weissella (60%), Pediococcus (44%), Lactobacillus (33%), but not in leuconostocs and lactococci. Antibiotic resistance genes were found in 7.5% of the non-enterococci, including the genera Pediococcus (12.5%) and Weissella (6.7%). One strain of both Pediococcus pentosaceus and Weissella cibaria carried the erythromycin resistance gene mef(A/E), and another two P. pentosaceus strains harboured lnu(A) conferring resistance to lincosamides. Gelatinase activity was found in E. faecalis and E. faecium (71 and 11%, respectively), while a low number of E. faecalis (5%) and none E. faecium exerted hemolytic activity. None enterococci and non-enterococci showed bile deconjugation and mucin degradation abilities, or other detrimental enzymatic activities.
Conclusions
To our knowledge, this is the first description of mef(A/E) in the genera Pediococcus and Weissella, and lnu(A) in the genus Pediococcus. The in vitro subtractive screening presented in this work constitutes a valuable strategy for the large-scale preliminary selection of putatively safe LAB intended for use as probiotics in aquaculture.
Similar content being viewed by others
Background
Aquaculture has the potential to make a significant contribution to the increasing demand for aquatic food in most world regions; however, in order to achieve this goal, the sector will have to face significant challenges, including the production intensification, the disease control and the prevention of the environmental deterioration [1]. In fish farming, the widespread use of antibiotics as prophylactic and therapeutic agents to control bacterial diseases has been associated with the emergence of antibiotic resistance in bacterial pathogens and with the alteration of the microbiota of the aquaculture environment [2, 3]. This resulted in the ban of antibiotic usage as animal growth promoters in Europe and stringent worldwide regulations on therapeutical antibiotic applications. This scenario has led to an evergrowing interest in the search and development of alternative strategies for disease control, within the frame of good husbandry practices, including adequate hygiene conditions, vaccination programmes and the use of probiotics, prebiotics and immunostimulants [4–6]. Recently, novel strategies to control bacterial infections in aquaculture have emerged, such as specific killing of pathogenic bacteria by bacteriophages, growth inhibition of pathogen by short-chain fatty acids and polyhydroxyalkanoates, and interference with the regulation of virulence genes (quorum sensing disruption), which have been reviewed by Defoirdt et al.[7]. With regard to probiotics, they are defined as live microbial adjuncts which have a beneficial effect on the host by: (i) modifying the host-associated or ambient microbial community; (ii) improving feed use or enhancing its nutritional value; (iii) enhancing the host response towards disease; and/or (iv) improving its environment [8]. To date, most probiotics proposed as biocontrollers and bioremediation agents for aquaculture belong to the LAB group (mainly to the genera Lactobacillus, Lactococcus, Leuconostoc, Enterococcus and Carnobacterium), to the genera Vibrio, Bacillus, and Pseudomonas or to the species Saccharomyces cerevisiae[8, 9]. Recently, a probiotic culture (Bactocell®, Pediococcus acidilactici CNCM MA18/5 M) has been authorized for the first time for use in aquaculture in the European Union.
According to the FAO/WHO [10], the development of commercial probiotics requires their unequivocal taxonomic identification, as well as their in vitro and in vivo functional characterization and safety assessment. In Europe, the European Food Safety Agency (EFSA) proposed a system for a pre-market safety assessment of selected groups of microorganisms used in food/feed and the production of food/feed additives leading to a Qualified Presumption of Safety (QPS) status [11–13]. The QPS approach propose that the safety assessment of a defined taxonomic group could be made based on establishing taxonomic identity, body of knowledge, possible pathogenicity and commercial end use. According to the EFSA approach [13], most LAB species are included in the QPS list and, therefore, demonstration of their safety only requires confirmation of the absence of determinants of resistance to antibiotics of human and veterinary clinical significance. However, in the case of enterococci, a more thorough, strain-specific evaluation is required to assess the risk associated to their intentional use in the food chain. In this work, we present the antimicrobial activity against fish pathogens and the in vitro safety assessment beyond the QPS approach of a collection of 99 LAB belonging to the genera Enterococcus, Lactobacillus, Lactococcus, Leuconostoc, Pediococcus and Weissella, previously isolated from aquatic animals regarded as human food [14] and intended for use as probiotics in aquaculture.
Results
Direct antimicrobial activity of the 99 LAB of aquatic origin
The 99 LAB strains isolated from fish, seafood and fish products displayed direct antimicrobial activity against, at least, four of the eight tested indicator microorganisms (Table 1). The most sensitive indicators were Listonella anguillarum CECT4344, Ls. anguillarum CECT7199 and Aeromonas hydrophila CECT5734, followed by Lactococcus garvieae JIP29-99, Streptococcus iniae LMG14521 and Streptococcus agalactiae CF01173. On the contrary, Photobacterium damselae CECT626 and Vibrio alginolyticus CECT521 were the less sensitive indicator microorganisms.
Preliminary safety evaluation of enterococci: presence of virulence factors, production of gelatinase and hemolysin and antibiotic susceptibility
Concerning E. faecalis, most of the strains (20 strains, 95%) harboured, at least, one relevant virulence factor: efaAfs (95%), gelE (71%), or agg (67%) genes (Table 2). A positive gelatinase reaction was found in 15 E. faecalis strains (71%) which harboured gelE, from which 12 also harboured agg gene. Only one E. faecalis strain (E. faecalis SDP10) (5%), harbouring cylL L -cylL S -cylM, exerted hemolytic activity, while none of the strains amplified hyl or esp genes. With regard to E. faecium, 20 strains (53%) harboured, at least, one relevant virulence factor: efaAfs (45%), gelE (24%) or agg (8%), but only 4 strains (11%) exerted gelatinase activity. None of the E. faecium strains exerted hemolytic activity nor amplified hyl or esp genes. The results of the antibiotic susceptibility tests revealed that 39 enterococccal strains (66%) displayed acquired antibiotic resistance to antibiotics other than penicillin G, chloramphenicol and high-level gentamicin. In this respect, 13 E. faecalis strains (62%) showed acquired resistance to (i) second generation quinolones (ciprofloxacin and/or norfloxacin) (12 strains, 57%), (ii) rifampicin (5 strains, 24%), (iii) nitrofurantoin (5 strains, 24%), (iv) glycopeptides (vancomycin and teicoplanin) (4 strains, 19%), and/or (v) erythromycin (1 strain, 5%). However, 26 E. faecium strains (68%), including 17 strains that encode virulence factors and nine strains without these traits, displayed acquired resistance to (i) erythromycin (14 strains, 37%), (ii) nitrofurantoin (11 strains, 29%), (iii) second generation quinolones (ciprofloxacin and/or norfloxacin) (10 strains, 26%), (iv) rifampicin (4 strains, 11%), (v) tetracycline (2 strains, 5%), and/or (vi) glycopeptides (vancomycin and teicoplanin) (1 strain, 3%). Moreover, multiple antibiotic resistance (two to six antibiotics) was found in E. faecalis (10 strains, 48%) and, to a lesser extent, in E. faecium (12 strains, 32%) (Table 2). According to the results above, 21 E. faecalis strains were discarded for further studies based on the presence of virulence factors (8 strains, 38%), acquired antibiotic resistance (1 strain, 5%) or both (12 strains, 57%). Regarding E. faecium strains, 29 (76%) were dropped from further screening based on acquired antibiotic resistance (9 strains, 24%), the presence of virulence factors (3 strains, 8%) or both (17 strains, 45%).
Extracellular antimicrobial activity of the 49 pre-selected LAB
The antimicrobial activity of supernatants from the 49 pre-selected LAB (9 E. faecium selected based on their preliminary safety assessment and 40 non-enterococcal strains) with direct antimicrobial activity against fish pathogens was assayed against three indicator microorganisms by an ADT (Table 3). In this regard, 24 (49%) and 10 (20%) strains displayed extracellular antimicrobial activity in their supernatants and/or 20-fold concentrated supernatants against Pediococcus damnosus CECT4797 and L. garvieae JIP 29–99, respectively, but none of the strains inhibited the Gram-negative strain A. hydrophila CECT5734. Interestingly, the antimicrobial activity of the respective supernatants was sensitive to proteinase K treatment, but was not affected by the heat treatment, revealing the proteinaceous nature and heat stability of the secreted antimicrobial compounds (i.e., heat-stable bacteriocins). The 24 LAB strains secreting bacteriocins into the liquid growth medium belong to the species P. pentosaceus (15 strains), E. faecium (8 strains), and Lb. curvatus (1 strain).
In vitrosafety assessment of the 49 pre-selected LAB
The 49 pre-selected LAB were further submitted to a comprehensive safety assessment by different in vitro tests.
Hemolysin production, bile salts deconjugation and mucin degradation
None of the non-enterococcal strains showed hemolytic activity, similarly as found for the 9 enterococci. Moreover, bile salts deconjugation and mucin degradation abilities were not found in any of the tested strains.
Enzymatic activities
The results of the analysis of enzymatic activity profiles of the tested LAB are shown in Table 4. None of the strains showed lipolytic activity, except E. faecium LPP29, TPM76, SMA7, and SMF8 which produced esterase (C4) and esterase lipase (C8). Moreover, none of the LAB strains showed protease activity (trypsin and α-chymotrypsin). Nevertheless, peptidase activity (leucine, valine or cystine arylamidase) was found in all the species. All strains showed acid phosphatase (except E. faecium TPM76 and Lc. cremoris) and naphthol-AS-BI-phosphohydrolase activities, but none displayed alkaline phosphatase activity. β-Galactosidase was found in most species (but not in all strains) except Lb. curvatus and L. cremoris. However, α-glucosidase was only found in the three Lc. cremoris strains. β-Glucosidase and N-acetyl-β-glucosaminidase activities were observed in most E. faecium, Lactobacillus spp., L. cremoris, and P. pentosaceus strains, but only in two W. cibaria strains, while the three Lc. cremoris strains showed β-glucosidase but lacked N-acetyl-β-glucosaminidase activity. On the other hand, α-galactosidase, β-glucuronidase, α-mannosidase, and α-fucosidase activities were not detected in any of the tested LAB strains.
Antibiotic susceptibility determined by the broth microdilution test
The distribution of MICs of the tested antibiotics is summarized in Tables 5 and 6. Microbiological breakpoints for ampicillin, vancomycin, gentamicin, kanamycin, streptomycin, erythromycin, clindamycin, tetracycline, and chloramphenicol reported by the FEEDAP document on the assessment of bacterial products used as feed additives in relation to antibiotic resistance [15] were used to categorise the 49 LAB as susceptible or resistant strains. In this document, the genus Weissella, which is considered a group of heterofermentative Leuconostoc-like LAB [16], is not included. For this reason, the respective MICs were interpreted by using the breakpoints given for the genus Leuconostoc. Besides, due to the lack of microbiological breakpoints for penicillin and linezolid on the FEEDAP document, we interpreted our results on these antibiotics according to the cut-off levels proposed by Klare et al.[17] for pediococci, namely 1 and 2 mg/L for penicillin and linezolid, respectively. According to our results, the percentages of strains showing antibiotic resistance in the genera Weissella, Pediococcus, Lactobacillus and Enterococcus were 60, 44, 33 and 11%, respectively, while none of the leuconostocs and lactococci showed this phenotype. In summary, 97.5% of the 40 non-enterococal strains resulted susceptible to ampicillin, 100% to gentamicin, 72.5% to kanamycin, 100% to streptomycin, 95% to erythromycin, 87.5% to clindamycin, 95% to tetracycline, and 100% to chloramphenicol. For vancomycin, it is known that facultative and obligate heterofermentative Lactobacillus, Pediococcus spp. and Leuconostoc spp. are intrinsically resistant. In contrast, the three lactococci were clearly susceptible to these antibiotics, showing a MIC of 0.5 mg/L. On the other hand, according to the cut-off values proposed by Klare et al.[17], 93% of P. pentosaceus strains were susceptible to penicillin and linezolid. With regard to E. faecium, all the tested strains were susceptible to ampicillin, vancomycin, gentamicin, kanamycin, streptomycin, tetracycline, chloramphenicol, and erythromycin except E. faecium BNM58 against the latter antibiotic (MIC = 8 mg/L). Moreover, multiple antibiotic resistance (three antibiotics) was only detected in P. pentosaceus LPM78 (6.2%) and W. cibaria SMA25 (6.7%).
Detection of antibiotic resistance genes
The non-enterococcal strains showing antibiotic resistances in the VetMIC assays (17 strains) were further submitted to PCR in order to identify the presence of the respective antibiotic resistance genes. The tested strains were the following: Lb. carnosus B43 (ampicillin resistant), P. pentosaceus TPP3 and SMF120 (tetracycline resistant), P. pentosaceus LPP32, LPM83 and B5 (clindamycin resistant), P. pentosaceus LPV57 and W. cibaria P50, P61, P64, P73, SDM381, SDM389, SMA14 and BCS50 (kanamycin resistant), and P. pentosaceus LPM78 and W. cibaria SMA25 (kanamycin, erythromycin and clindamycin resistant). Acquired antibiotic resistances likely due to added genes were only found in strains within the genera Pediococcus (12.5%) and Weissella (6.7%). The genes involved in the horizontal transfer of resistance to tetracycline [tet(K), tet(L) and tet(M)], kanamycin [aac(6´ )-Ie-aph(2´ ´ )-Ia] and erythromycin [erm(A), erm(B) and erm(C)] were not detected. However, P. pentosaceus LPM78 and W. cibaria SMA25 harboured the erythromycin resistance gene mef(A/E). The obtained amplicons were sequenced and found to have 99% homology with the macrolide-efflux protein (mefE) gene described for Streptococcus pneumoniae and other Streptococcus spp. Moreover, P. pentosaceus LPM78 and LPM83 harboured the lnu(A) gene encoding the lincosamide O-nucleotidyltransferase that inactivates lincomycin and clindamycin. Sequencing of both amplicons showed 97% and 93% homology with lincosamide nucleotidyltransferase [lnu(A)] gene described for Staphylococcus haemolyticus and S. aureus, respectively. Nevertheless, lnu(B) was not detected in any of the tested strains. With regard to E. faecium BNM58, which was phenotypically resistant to erythromycin, none of the respective genes [erm(A), erm(B), erm(C) and mef(A/E)] were detected.
Discussion
In this work, the antimicrobial activity against fish pathogens and the in vitro safety of 99 LAB previously isolated from fish, seafood and fish products [14] have been assayed by using microbiological, biochemical and genetic assays in order to identify and select the most suitable candidates to be further evaluated as probiotics for a sustainable aquaculture. LAB are widely known for their ability to inhibit bacterial pathogens by the production of antimicrobial compounds such as organic acids, oxygen peroxide and ribosomally-synthesized peptides referred to as bacteriocins, which constitutes a desirable property for probiotics and a sustainable alternative to antibiotics [9, 18]. In this respect, most of the LAB of aquatic origin tested in this work displayed a broad antimicrobial spectrum against the main Gram-positive and Gram-negative fish pathogens, being remarkable that a high number of strains (24 out of 49 strains, 49%) were identified as potential bacteriocin producers. Recently, bacteriocin production ability has been proposed as a key property for selection of probiotic LAB to be used in aquaculture as an alternative to antibiotics to fight against fish pathogen infections [19], similarly as proposed for human and farm animal probiotics [20–22]. In aquaculture farming, lactococcosis produced by the zoonotic agent L. garvieae, causing hemorrhagic septicaemia and meningoencephalitis, is one of the most serious diseases affecting several marine and fresh water fish species [23]. With regard to this, our work shows that putative bacteriocinogenic LAB active against this relevant fish pathogen are common amongst the microbiota isolated from aquatic animals (10 strains, 20%).
The application of probiotics in aquaculture may modify the microbial ecology of the aquatic hosts and their surrounding environment, and thus the assessment of their safety to the target aquatic species, the environment and humans constitutes an essential issue [24]. To date, several studies describing the screening and evaluation of LAB as probiotic candidates for aquaculture have been reported [25–28]; however, the safety assessment of the strains is generally limited to in vivo challenge tests and rearing trials in order to confirm their lack of toxicity to the aquatic hosts [24, 25, 28–31]. Strikingly, in vitro safety assessment studies have not been generally addressed, despite they have lower economic and ethic costs and result very effective to evaluate the safety of a high number of candidate probiotic strains not only for the host species, but also for humans and the environment. According to EFSA [13], most of the LAB species tested in this work (P. pentosaceus, Lb. curvatus, L. lactis, Lc. mesenteroides) are included in the QPS list and, therefore, demonstration of their safety only requires confirmation of the absence of determinants of resistance to antibiotics of human and veterinary clinical significance. However, in the case of enterococci, a more thorough, strain-specific evaluation is required to assess the risk associated to their intentional use in the food chain, while no guidelines are given for the safety assessment of the species W. cibaria[13].
Our results show that enterococcal virulence factors were more frequently found in E. faecalis than in E. faecium, which is in concordance with previous reports [32–34]. In this respect, most of the E. faecalis (95%) and a large percentage of the E. faecium (53%) strains evaluated in this work showed, at least, one virulence factor, being efaAfs, gelE and agg the most frequently detected genes. With regard to gelE, which encodes for an extracellular zinc endopeptidase that hydrolyzes gelatin, collagen, hemoglobin, and other bioactive compounds, this gene was detected at high frequency in E. faecalis, with all the gelE+ strains showing gelatinase activity. However, five out of nine E. faecium strains harbouring gelE were unable to degrade gelatin, suggesting the carriage of a non-functional gene, as previously reported [32, 33]. Likewise, in the case of E. faecium P68 and E. faecium GM29 harbouring cylL L cylL S , the lack of hemolytic activity may be explained by the absence of cylM, whose product is involved in the post-translational modification of cytolysin. On the other hand, esp and hyl, which encode a cell wall-associated protein involved in immune evasion and an hyaluronidase enzyme, respectively, were not found in any of the tested LAB. Previous studies have reported that esp and hyl are more common in ampicillin-resistant/vancomycin-resistant E. faecium (VREF) than in ampicillin-susceptible/VREF strains [35]. In this context, the increase in the incidence of VREF at hospital settings has been attributed mainly to the spread of ampicillin-resistant VREF exhibiting esp and/or hyl[36, 37]. Therefore, the fact that the E. faecium strains evaluated in this work lack these genes might be related with their non-clinical origin and absence of ampicillin resistance.
The use and frequent overuse of antibiotics, including those used in human medicine, in fish farming has resulted in the emergence and spread of antibiotic-resistant bacteria in the aquaculture environment. This possesses a threat to human and animal health due to the increase of acquired antibiotic resistance in fish pathogens, the transfer of their genetic determinants to bacteria of terrestrial animals and to human pathogens, and the alterations of the bacterial microbiota of the aquatic environment [11, 29]. In our study, the percentage of enterococcal strains showing acquired antibiotic resistance was 68%. Interestingly, the results found in E. faecium (71%) and E. faecalis (62%) were similar, however, higher percentages of resistance to ciprofloxacin and/or norfloxacin, rifampicin, and glycopeptides were observed in E. faecalis. Nevertheless, the occurrence of erythromycin and tetracycline resistance was frequently detected amongst E. faecium (45%) but only in one E. faecalis strain (5%). In spite of the high prevalence of acquired antibiotic resistance found in enterococci of aquatic origin, they showed low incidence or absence of resistance to the clinically relevant antibiotics vancomycin (8.5%) and ampicillin, penicillin and gentamicin, respectively, which is in agreement with previous studies [33, 38]. Moreover, the percentages of strains showing antibiotic resistance in the genera Weissella, Pediococcus and Lactobacillus were 60, 44 and 33%, respectively, while none of the leuconostocs and lactococci showed this phenotype. In this regard, our results indicate that the LAB susceptibility patterns of MIC values to clinically relevant antibiotics are species-dependent, similarly as previously described by other authors [39, 40]. Moreover, multiple antibiotic resistance was commonly found in strains within the genus Enterococcus (37%), mainly in E. faecalis, while being very infrequent in the non-enterococcal strains (5%).
According to EFSA [29], the determination of MICs above the established breakpoint levels, for one or more antibiotic, requires further investigation to make the distinction between added genes (genes acquired by the bacteria via gain of exogenous DNA) or to the mutation of indigenous genes. According to our results, acquired antibiotic resistance likely due to added genes is not a common feature amongst the non-enterococcal LAB of aquatic origin (7.5%). In this respect, this genotype was only found in the genera Pediococcus (12.5%) and Weissella (6.7%). Although P. pentosaceus LPV57 and LPM78 showed resistance to kanamycin (MIC of 128 mg/L), the respective resistance gene aac(6´ )-Ie-aph(2´ ´ )-Ia was not found in these strains. Similarly, P. pentosaceus TPP3 and SMF120 were phenotypically resistant to tetracycline (MIC of 16 mg/L), but did not contain tet(K), tet(L) or tet(M). In this respect, Ammor et al.[41] reported that pediococci are intrinsically resistant to the latter two antibiotics, as well as to glycopeptides (vancomycin and teicoplanin), streptomycin, ciprofloxacin and trimethoprim-sulphamethoxazole. Other authors proposed a MIC for tetracycline in pediococci ranging between 8 and 16 mg/L [42], or of 32 mg/L for oxytetracycline in P. pentosaceus[17]. The tetracycline breakpoints suggested for pediococci by EFSA are lower than the MICs observed in our work and others [17, 42]. On the other hand, the only antibiotic resistance detected in Leuconostoc strains was for vancomycin, which is an intrinsic property of this genus. It has been previously reported that Leuconostoc strains display poor, if any, resistance to antibiotics of clinical interest [38]. With regard to lactococci, the three L. cremoris strains evaluated were susceptible to all the antibiotics; however, relatively high MICs for rifampicin (16–32 mg/L) and trimethoprim (≥ 64 mg/L) were detected. In fact, most lactococcal species are resistant to trimethoprim [41]. As expected, all strains of heterofermentative Lactobacillus spp. were resistant to vancomycin but susceptible to the rest of the assayed antibiotics, except Lb. carnosus B43, which showed the highest MIC for ampicillin and penicillin (MICs of 8 and 4 mg/L, respectively). In this context, the presence of modifications in the low affinity penicillin-binding protein (PBP) that confers resistance to penicillin and β-lactams in E. faecium and Streptococcus pneumoniae, has been reported [43, 44]. Moreover, nine PBPs have been described in Lb. casei ATCC 393 [45], which leads us to suggest that a similar mechanism may be also responsible for the ampicillin and penicillin resistance found in Lb. carnosus B43. The resistance to vancomycin detected in Pediococcus, Leuconostoc and Lactobacillus species in this study might be due to the presence of D-Ala-D-Lactate in their peptidoglycan rather than D-Ala-D-Ala dipeptide [46]. In this context, all tested W. cibaria strains showed MICs ≥ 128 mg/L for vancomycin, suggesting that vancomycin resistance is an intrinsic property of this species. In relation to Weissella spp., studies on antibiotic resistance profiles are very limited [47] and breakpoints have not been defined by EFSA [15]. In our study, most W. cibaria strains showed low MIC values; however W. cibaria BCS50 showed relatively high MICs for penicillin (8 mg/L) and kanamycin (64 mg/L), and W. cibaria SMA25 showed MICs of 128 mg/L for kanamycin, 8 mg/L for gentamicin, erythromycin and neomycin, and 2 mg/L for clindamycin. Therefore, these two strains were discarded of this study, while W. cibaria P50, P61, P64, P73, SMA14, SDM381 and SDM389 were not included in the final selection due to their MICs for kanamycin (32–64 mg/L). According to these results, as a rule of thumb, we propose for W. cibaria the breakpoints assigned to Leuconostoc spp. by EFSA [15], until further studies establish the wild-type MIC ranges within this species. In spite of that, different MICs for rifampicin and trimethoprim for W. cibaria and Lc. cremoris were found in this study. The reduced susceptibility of W. cibaria towards trimethoprim could indicate an intrinsic resistance to this antibiotic [48]. In our work, the only antibiotic resistance genes found were mef(A/E), which encodes a drug efflux pump conferring a low to moderate level of resistance to 14 (erythromycin and clarithromycin)- and 15 (azithromycin)-membered macrolides but not to lincosamide or streptogramin B antibiotics [49], and lnu(A), encoding the lincosamide O-nucleotidyltransferase that inactivates lincomycin and clindamycin [50]. In this respect, P. pentosaceus LPM78 and W. cibaria SMA25, displaying erythromycin resistance (MIC = 8 and ≥ 8 mg/L, respectively), carried the gene mef(A/E), which can be found in a variety of Gram-positive bacteria, including corynebacteria, enterococci, micrococci, and several streptococcal species [51, 52]. On the other hand, two pediococci (P. pentosaceus LPM78 and LPM83) that showed resistance to clindamycin (MIC = 4 and 2 mg/L, respectively) carried the gene lnu(A), which had been only previously found in staphylococci, streptococci, enterococci and lactobacilli of animal origin and in staphylococci isolated from humans [50, 53]. Strikingly, the clindamycin resistant strains P. pentosaceus LPP32 and B5 and W. cibaria SMA25 (MIC = 4 and 2 mg/L, respectively) did not harbour this gene nor lnu(B). To our knowledge, this is the first description of mef(A/E) in the genera Pediococcus and Weissella, and lnu(A) in the genus Pediococcus. The detection of resistance genes for macrolide and lincosamide in non-enterococcal strains suggests a wider distribution of this group of genes than previously anticipated.
The in vitro subtractive screening proposed in this work also include the assessment of bile salts deconjugation, mucin degradation, biogenic amine production and other potentially detrimental enzymatic activities such as the β-glucuronidase activity, which should be absent in probiotic candidates [54–56]. Excessive deconjugation of bile salts may be unfavourable in animal production since unconjugated bile acids are less efficient than their conjugated counterparts in the emulsification of dietary lipids. In addition, the formation of micelles, lipid digestion and absorption of fatty acids and monoglycerides could be impaired by deconjugated bile salts [57]. Similarly, excessive degradation of mucin may be harmful as it may facilitate the translocation of bacteria to extraintestinal tissues [55]. In this respect, it is worthy to note that none of the 49 tested LAB deconjugated bile salts nor exhibited mucinolytic activity, the latter indicating their low invasive and toxigenic potential at the mucosal barrier. These results are in accordance with previous findings showing that LAB do not degrade mucin in vitro[58, 59]. Moreover, β-glucuronidase activity has been associated with the generation of potential carcinogenic metabolites [56]; however, none of the LAB tested in our study displayed this harmful enzymatic activity. In a previous work [60], we demonstrated that none of the 40 non-enterococcal strains evaluated herein produced histamine, tyramine or putrescine. With regard to enterococci, the nine E. faecium strains only produced tyramine, being E. faecium CV1 a low producer of this biogenic amine. Although the lack of biogenic amine production by probiotic strains is a desirable trait, it should be borne in mind that tyramine production by enterococci is a very frequent trait [60, 61]. Finally, several studies have suggested that probiotic microorganisms might exert a beneficial effect in the digestion process of fish due to the production of extracellular enzymes [62–65]. In our work, the LAB strains of aquatic origin within the genera Pediococcus, Enterococcus and Lactobacillus showed a higher number of enzymatic activities than Lactococcus, Leuconostoc and Weissella, being the enzymatic profiles similar amongst strains within the same genus. In this respect, nearly all the strains produced phosphatases, which might be involved in nutrient absorption [64], and peptidases and glucosidases that breakdown peptides and carbohydrates, respectively. However, the tested LAB showed weak lipolytic activity and no proteolytic activity.
Conclusions
This work shows that antimicrobial/bacteriocin activity against fish pathogens is a widespread probiotic property amongst LAB isolated from aquatic animals regarded as human food. However, particular safety concerns based on antibiotic resistances and virulence factors were dominant within E. faecalis (100%) and E. faecium (79%), and acquired antibiotic resistance genes were not commonly found (7.5%; erythromycin and clindamycin) amongst the non-enterococcal isolates of aquatic origin. To our knowledge, this is the first large-scale study describing the antimicrobial activity against fish pathogens and the safety assessment beyond the QPS approach of LAB isolated from aquatic animals. The in vitro subtractive screening presented herein, which allowed the selection of 33 strains (8 E. faecium, 11 P. pentosaceus, 1 Lb. carnosus, 1 Lb. curvatus, 3 L. cremoris, 3 Lc. cremoris and 6 W. cibaria) out of 99 LAB isolates of aquatic origin, constitutes a valuable strategy for the large-scale preliminary selection of putatively safe LAB intended for use as probiotics in aquaculture and to avoid the spreading of bacterial cultures with harmful traits into the aquatic environment. Nevertheless, a comprehensive in vivo assessment of their lack of toxicity and undesirable effects must be also carried out using cell lines, live food and, ultimately, aquatic animals before their unequivocal consideration as safe probiotics for a sustainable aquaculture.
Methods
Bacterial strains and growth conditions
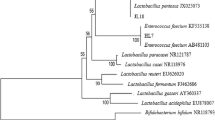
A total of 99 LAB (59 enterococci and 40 non-enterococci) of aquatic origin with antimicrobial activity against spoilage and food-borne pathogenic bacteria of concern for the fish industry, previously isolated and identified by our group from fish, seafood and fish products [14], were used in this study (Table 1). The LAB strains were isolated on non-supplemented MRS (Oxoid, Ltd., Basingstoke, United Kingdom) or KAA (Oxoid) agar (1,5%, w/v) at 25°C, and taxonomically identified [14] by sequencing of the genes encoding 16S rRNA (16S rDNA) [66] and/or superoxide dismutase (sodA) [67]. Unless otherwise stated, LAB were grown aerobically in MRS broth at 32°C.
Direct antimicrobial activity assay
The antimicrobial activity of the 99 LAB against the main Gram-positive and Gram-negative fish pathogens was assayed by a qualitative stab-on-agar test (SOAT) as previously described by Cintas et al. [68]. Briefly, pure cultures were stabbed onto MRS or Tryptone Soya Agar (TSA) (Oxoid) plates supplemented with glucose (2%, w/v) and incubated at 32°C for 5 h, and then 40 ml of the corresponding soft agar (0.8%, w/v) medium containing about 1 × 105 CFU/ml of the indicator strain was poured over the plates. After incubation at 28-37°C for 16–24 h depending on the indicator strain, the plates were checked for inhibition zones (absence of visible microbial growth around the stabbed cultures), and only inhibition halos with diameters >3 mm were considered positive. L. garvieae JIP29-99 was grown aerobically in Tryptone Soya Broth (TSB) (Oxoid) at 37°C. S. agalactiae CF01173 and S. iniae LMG14521 were grown aerobically in Brain Heart Infusion (BHI) broth (Oxoid) at 37°C. A. hydrophila CECT5734, Ls. anguillarum CECT4344, Ls. anguillarum CECT7199, and Ph. damselae CECT626 strains were grown aerobically in TSB at 28°C. V. alginolyticus CECT521 was grown aerobically in TSB supplemented with NaCl (1%, w/v; Panreac Química S.A.U, Barcelona, Spain) at 28°C.
Extracellular antimicrobial activity assay
The antimicrobial activity of supernatants from LAB cultures grown in MRS broth at 32°C for 16 h was determined by an agar well-diffusion test (ADT) as previously described by Cintas et al.[68]. Supernatants were obtained by centrifugation of cultures at 10,000 × g at 4°C for 10 min, adjusted to pH 6.2 with 1 M NaOH, filter-sterilized through 0.22 μm-pore-size filters (Millipore Corp., Bedford, Massachussets, USA) and stored at −20°C until use. Fifty-μl aliquots of cell-free culture supernatants were placed into wells (6-mm diameter) cut in cooled MRS or TSB agar (0.8%, wt/vol) plates previously seeded (1 × 105 CFU/ml) with the indicator microorganisms Pediococcus damnosus CECT4797, L. garvieae JIP29-99 or A. hydrophila CECT5734. After 2 h at 4°C, the plates were incubated under the same conditions mentioned above to allow for the growth of the target microorganisms and then analyzed for the presence of inhibition zones around the wells. To determine the proteinaceous nature of the antimicrobial compounds, supernatants showing antimicrobial activity were subjected to proteinase K treatment (10 mg/ml) (AppliChem GmbH, Germany) at 37°C for 2 h. After proteinase K inactivation by heat treatment (100°C, 10 min), samples were assayed for residual antimicrobial activity by an ADT as described above using P. damnosus CECT4797 as indicator microorganism. Supernatants with no added enzyme were treated as indicated above and used as controls. For further characterization of the antimicrobial compounds, 7 ml of supernatants from an overnight culture of LAB were subjected to peptide concentration by ammonium sulphate precipitation. Ammonium sulphate was gradually added to the supernatants to achieve 50% saturation. Samples were kept at 4°C with stirring for 3 h, and then centrifuged at 10,000 × g at 4°C for 30 min. Pellets and floating solid material were combined and solubilized in 350 μl of 20 mM sodium phosphate (pH 6.0), and antimicrobial activity of the resulting 20-fold concentrated supernatants was determined by an ADT as described above.
PCR detection of potential virulence factors in enterococci
Detection of genes encoding potential virulence factors in the 59 enterococci was performed by PCR. The following primer pairs were used: TE3/TE4 for detection of agg (aggregation substance), TE9/TE10 for gelE (gelatinase), TE34/TE36 for esp (enterococcal surface protein), TE5/TE6 for efaAfs (Enterococus faecalis endocarditis antigen) [32], HYLn1/HYLn2 for hyl (hyaluronidase) [35], CYLLL–R1/CYLLS–R2 for cylL L –cylL S (cytolysin precursor) [69], and RHCT1/RHCT2 for cylL L –cylL S -cylM (cytolysin precursor and posttranslational modifier) [70]. Oligonucleotide primers were obtained from Sigma-Genosys Ltd. (Cambridge, United Kingdom). The positive control strains for detection of potential virulence factors were the following: E. faecalis P4 for cylL L –cylL s , cylL L –cylL S –cylM, agg, gelE and efaAfs, E. faecalis P36 for esp[32], and E. faecium C68 for hyl[35]. PCR-amplifications were performed from total bacterial DNA obtained using the Wizard DNA Purification Kit (Promega, Madrid, Spain) in 25 μl reaction mixtures with 1 μl of purified DNA, 0.7 μM of each primer, 0.2 mM of each dNTP, buffer 1×, 1.5 mM MgCl2 and 0.75 U of Platinum Taq DNA polymerase (Invitrogen, Madrid, Spain). Samples were subjected to an initial cycle of denaturation (97°C for 2 min), followed by 35 cycles of denaturation (94°C for 45 s), annealing (48 to 64°C for 30 s) and elongation (72°C for 30 to 180 s), ending with a final extension step at 72°C for 7 min in an Eppendorf Mastercycler thermal cycler (Eppendorf, Hamburg, Germany). PCR products were analyzed by electrophoresis on 1-2% (w/v) agarose (Pronadisa, Madrid, Spain) gels stained with Gel red (Biotium, California, USA), and visualized with the Gel Doc 1000 documentation system (Bio-Rad, Madrid, Spain). The molecular size markers used were HyperLadder II (Bioline GmbH, Germany) and 1Kb Plus DNA ladder (Invitrogen).
Production of gelatinase by enterococci
Gelatinase production was determined using the method previously described by Eaton and Gasson [32]. Briefly, enterococci were grown in MRS broth overnight at 32°C, and streaked onto Todd-Hewitt (Oxoid) agar plates (1.5%, w/v) containing 30 g of gelatine per litre. After incubation overnight incubation at 37°C, the plates were placed at 4°C for 5 h before examination for zones of turbidity (protein hydrolysis) around the colonies. E. faecalis P4 was used as positive control.
Production of hemolysin
To investigate hemolysin production by the 99 LAB, the strains grown in MRS broth were streaked onto layered fresh horse blood agar plates (BioMérieux, Marcy l'Étoile, France) and grown at 37°C for 1–2 days [32]. β-hemolysis was revealed by the formation of clear zones surrounding the colonies on blood agar plates. E. faecalis P4 was used as positive control.
Determination of antibiotic susceptibility
Antibiotic susceptibility of the 59 enterococci was determined by overlaying antibiotic-containing disks (Oxoid) on Diagnostic Sensitivity Test Agar (Oxoid) previously seeded with approximately 1 × 105 CFU/ml of each enterococcal isolate. The antibiotics tested were ampicillin (10 μg), chloramphenicol (30 μg), ciprofloxacin (5 μg), erythromycin (15 μg), gentamicin (120 μg), nitrofurantoin (300 μg), norfloxacin (10 μg), penicillin G (10 IU), rifampicin (5 μg), teicoplanin (30 μg), tetracycline (30 μg), and vancomycin (30 μg). Inhibition zone diameters were measured after overnight incubation of the plates at 37°C. Resistance phenotypes were recorded as recommended by the Clinical and Laboratory Standards Institute [71]. E. faecalis CECT795 and Staphylococcus aureus CECT435 were used for quality control. The minimum inhibitory concentration for the 49 pre-selected LAB was determined by a broth microdilution test using e-cocci (for enterococci), and Lact-1 and Lact-2 (for non-enterococcal strains) VetMIC microplates (National Veterinary Institute, Uppsala, Sweden). The antibiotics evaluated for enterococci were ampicillin, vancomycin, gentamicin, kanamycin, streptomycin, erythromycin, tetracycline, chloramphenicol, narasin, and linezolid, while for the non-enterococcal strains, the tested antibiotics were ampicillin, vancomycin, gentamicin, kanamycin, streptomycin, erythromycin, clindamycin, tetracycline, chloramphenicol, neomycin, penicillin, linezolid, ciprofloxacin, rifampicin, and trimethoprim. Individual colonies were suspended in a sterile glass tube containing 5 ml saline solution (0.85% NaCl) to a turbidity of 1 in the McFarland scale (approx. 3 × 108 CFU/ml) and further diluted 1000-fold. Iso-sensitest (IST) broth (Oxoid) was used for enterococci, while LSM medium (IST:MRS, 9:1) was used for all the non-enterococcal strains except Lactobacillus curvatus subsp. curvatus BCS35, that required LSM broth supplemented with 0.03% (w/v) L-cysteine (Merck KGaA) [72]. Fifty or 100 μl of the diluted enterococcal and non-enterococcal suspensions, respectively, was added to each microplate well which was then sealed with a transparent covering tape and incubated at 37°C for 18 h (in the case of Lb. curvatus BCS35, the plates were incubated anaerobically at 32°C for 18 h). After incubation, MICs were established as the lowest antibiotic concentration that inhibited bacterial growth, and interpreted according to the breakpoints identified by the FEEDAP Panel and adopted by EFSA to distinguish between susceptible and resistant strains [15]. Accordingly, strains showing MICs higher than the respective breakpoint were considered as resistant. E. faecalis CECT795 and S. aureus CECT794 were used for quality control of e-cocci, and Lact-1 and Lact-2 VetMIC microplates, respectively.
Deconjugation of bile salts
The ability of the 49 pre-selected LAB to deconjugate primary and secondary bile salts was determined according to Noriega et al.[73]. Bile salt plates were prepared by adding 0.5% (w/v) sodium salts of taurocholate (TC) and taurodeoxycholate (TDC) (Sigma-Aldrich Corporation, St. Louis, Missouri, USA) to MRS agar (1.5%, w/v) supplemented with 0.05% (w/v) L-cysteine (Merck KGaA, Darmstadt, Germany). Overnight liquid cultures of strains (10 μl) were spotted onto agar plates and incubated under anaerobic conditions (Anaerogen, Oxoid) at 37°C for 72 h. The presence of precipitated bile acid around the colonies (opaque halo) was considered as a positive result. A fresh fecal slurry of a healthy adult horse was used as positive control for bile salts deconjugating activities.
Degradation of mucin
The capacity of the 49 pre-selected LAB to degrade gastric mucin was determined as described by Zhou et al.[58]. Mucin from porcine stomach type III (Sigma-Aldrich Corp.) and agar were added to medium B without glucose at concentrations of 0.5% (w/v) and 1.5% (w/v), respectively. A volume of 10 μl of 24 h viable bacterial cultures was inoculated onto the surface of medium B. The plates were incubated anaerobically at 37°C for 72 h, subsequently stained with 0.1% (w/v) amido black (Merck KGaA) in 3.5 M acetic acid for 30 min, and then washed with 1.2 M acetic acid (Merck KGaA). A discoloured zone around the colony was considered as a positive result. A fresh fecal slurry of a healthy adult horse was used as positive control for mucin degradation ability.
Determination of enzymatic activities
The APIZYM test (BioMérieux, Montallieu Vercieu, France) was used for determination of enzymatic activities of the 49 pre-selected LAB. Cells from cultures grown at 32°C overnight were harvested by centrifugation at 12,000 g for 2 min, resuspended in 2 ml of API Suspension Medium (BioMérieux) and adjusted to a turbidity of 5–6 in the McFarland scale (approx. 1.5-1.9 × 109 CFU/ml). Aliquots of 65 μl of the suspensions were added to each of the 20 reaction cupules in the APIZYM strip. The strips were incubated at 37°C for 4.5 h and the reactions were developed by addition of one drop each of the APIZYM reagents A and B. Enzymatic activities were graded from 0 to 5, and converted to nanomoles as indicated by the manufacturer´ s instructions.
PCR detection of antibiotic resistance genes
The presence of genetic determinants conferring resistance to aminoglycosides except streptomycin aac(6´)-Ie-aph(2´´)-Ia, to erythromycin erm(A), erm(B), erm(C) and mef(A/E)], to tetracycline tet(K), tet(L) and tet(M)], and to lincosamides lnu(A) and lnu(B)] was determined by PCR in the LAB strains showing antibiotic resistance by the VetMIC assay. PCR-amplifications and PCR-product visualization and analysis were performed as described above using the following primer-pairs: aacF/aacR for detection of aac(6´)-Ie-aph(2´´)-Ia[74], ermAI/ermAII for erm(A) [75, 76], ermBI/ermBII for erm(B) [17], ermCI/ermCII for erm(C) [17, 77], mef(A/E)I/ mef(A/E)II for mef(A/E) [75, 76], tetKI/ tetKII for tet(K) [17], tetLI/tetLII for tet(L) [17, 78], tetMI/tetMII for tet(M) [17, 78], lnuA1/lnuA2 for lnu(A) [79], lnuB1/lnuB2 for lnu(B) [50]. E. faecalis C1570 was used as positive control for amplification of erm(C), lnu(A) and tet(K) and E. faecalis C1231 for erm(A). E. faecium 3Er1 (clonal complex of hospital-associated strain CC9) and E. faecium RC714 were used as positive controls for amplification of aac(6´)-Ie-aph(2´´)-Ia, tet(M) and tet(L), and for erm(B) and mef(A/E), respectively. The amplicons obtained with mef(A/E) and lnu(A) specific primers were purified by using the NucleoSpin Extract II Kit (Macherey-Nagel GmbH & Co. KG, Düren, Germany) and both DNA strands were sequenced at the Unidad de Genómica (Parque Científico de Madrid, Facultad de Ciencias Biológicas, Universidad Complutense de Madrid, Spain). Analysis of DNA sequences was performed with the BLAST program available at the National Center for Biotechnology Information (NCBI).
Abbreviations
- LAB:
-
Lactic Acid Bacteria
- FAO:
-
Food and Agriculture Organization of the United Nations
- WHO:
-
World Health Organization
- EFSA:
-
European Food Safety Agency
- QPS:
-
Qualified Presumption of Safety
- EC:
-
European Commission
- MRS:
-
de Man, Rogosa and Sharpe
- KAA:
-
Kanamycin, Aesculin Azide.
References
FAO: FAO Fisheries Department. State of world aquaculture 2006. FAO Fish Tech Pap. 2006, 500: 1-134.
FAO: Responsible use of antibiotics in aquaculture. FAO Fish Tech Pap. 2005, 469: 1-97.
Cabello FC: Heavy use of prophylactic antibiotics in aquaculture: a growing problem for human and animal health and for the environment. Environ Microbiol. 2006, 8: 1137-1144. 10.1111/j.1462-2920.2006.01054.x.
Austin B: The bacterial microflora of fish, revised. ScientificWorldJournal. 2006, 6: 931-945.
Robertson PAW, O’Dowd C, Burrells C, Williams P, Austin B: Use of Carnobacterium sp. as a probiotic for Atlantic salmon (Salmo salar L.) and rainbow trout (Oncorhynchus mykiss, Walbaum). Aquaculture. 2000, 185: 235-243. 10.1016/S0044-8486(99)00349-X.
Wang Y-B, Li J-R, Lin J: Probiotics in aquaculture: challenges and outlook. Aquaculture. 2008, 281: 1-4. 10.1016/j.aquaculture.2008.06.002.
Defoirdt T, Sorgeloos P, Bossier P: Alternatives to antibiotics for the control of bacterial disease in aquaculture. Curr Opin Microbiol. 2011, 14: 251-258. 10.1016/j.mib.2011.03.004.
Verschuere L, Rombaut G, Sorgeloos P, Verstraete W: Probiotic bacteria as biological control agents in aquaculture. Microbiol Mol Biol Rev. 2000, 64: 655-671. 10.1128/MMBR.64.4.655-671.2000.
Gatesoupe FJ: Updating the importance of lactic acid bacteria in fish farming: natural occurrence and probiotic treatments. J Mol Microbiol Biotechnol. 2008, 14: 107-114. 10.1159/000106089.
FAO/WHO: Probiotics in food. Health and nutritional properties and guidelines for evaluation. FAO Food Nutr Pap. 2006, 85: 1-50.
EC: On a generic approach to the safety assessment of microorganisms used in feed/food and feed/food production - A working paper open for comment. 2003, http://ec.europa.eu/food/fs/sc/scf/out178_en.pdf,
EFSA: Introduction of a Qualified Presumption of Safety (QPS) approach for assessment of selected microorganisms referred to EFSA. The EFSA Journal. 2007, 587: 1-16.
EFSA: Maintenance of the list of QPS biological agents intentionally added to food and feed (2011 update). The EFSA Journal. 2011, 9: 1-82.
Gómez-Sala B, Basanta A, Sánchez J, Martín M, Criado R, Gutiérrez J, Citti R, Herranz C, Hernández PE, Cintas LM: Antimicrobial activity of lactic acid bacteria isolated from aquatic animals and fish products. 13éme Colloque du Club des Bactéries Lactiques, p 45 Abstracts. 2004, Nantes, France: ENITIAA and French National Institute for Agricultural Research (INRA)
EFSA: Guidance on the assessment of bacterial susceptibility to antimicrobials of human and veterinary importance. EFSA Journal. 2012, 10: 2740-2749.
Collins MD, Samelis J, Metaxopoulos J, Wallbanks S: Taxonomic studies on some leuconostoc-like organisms from fermented sausages: description of a new genus Weissella for the Leuconostoc paramesenteroides group of species. J Appl Bacteriol. 1993, 75: 595-603. 10.1111/j.1365-2672.1993.tb01600.x.
Klare I, Konstabel C, Werner G, Huys G, Vankerckhoven V, Kahlmeter G, Hildebrandt B, Müller-Bertling S, Witte W, Goossens H: Antimicrobial susceptibilities of Lactobacillus, Pediococcus and Lactococcus human isolates and cultures intended for probiotic or nutritional use. J Antimicrob Chemother. 2007, 59: 900-912. 10.1093/jac/dkm035.
Ringø E, Gatesoupe FJ: Lactic acid bacteria in fish: a review. Aquaculture. 1998, 160: 177-203. 10.1016/S0044-8486(97)00299-8.
Desriac F, Defer D, Bourgougnon N, Brillet B, Le Chevalier P, Fleury Y: Bacteriocin as weapons in the marine animal-associated bacteria warfare: inventory and potential applications as an aquaculture probiotic. Mar Drugs. 2010, 8: 1153-1177. 10.3390/md8041153.
O'Shea EF, Cotter PD, Stanton C, Ross RP, Hill C: Production of bioactive substances by intestinal bacteria as a basis for explaining probiotic mechanisms: Bacteriocins and conjugated linoleic acid. Int J Food Microbiol. 2012, 152: 189-205. 10.1016/j.ijfoodmicro.2011.05.025.
Gillor O, Etzion A, Riley MA: The dual role of bacteriocins as anti- and probiotics. Appl Microbiol Biotechnol. 2008, 81: 591-606. 10.1007/s00253-008-1726-5.
Corr SC, Li Y, Riedel CU, O'Toole PW, Hill C, Gahan CG: Bacteriocin production as a mechanism for the antiinfective activity of Lactobacillus salivarius UCC118. Proc Natl Acad Sci USA. 2007, 104: 7617-7621. 10.1073/pnas.0700440104.
Vendrell D, Balcazar JL, Ruiz-Zarzuela I, de Blas I, Girones O, Muzquiz JL: Lactococcus garvieae in fish: a review. Comp Immunol Microbiol Infect Dis. 2006, 29: 177-198. 10.1016/j.cimid.2006.06.003.
Decamp O, Moriarty D: Aquaculture species profit from probiotics. Feed Mix. 2007, 15: 20-23.
Dimitroglou A, Merrifield DL, Carnevali O, Picchietti S, Avella M, Daniels C, Güroy D, Davies SJ: Microbial manipulations to improve fish health and production - A Mediterranean perspective. Fish Shellfish Immunol. 2011, 30: 1-16. 10.1016/j.fsi.2010.08.009.
Nikoskelainen S, Salminen S, Bylund G, Ouwehand AC: Characterization of the properties of human- and dairy-derived probiotics for prevention of infectious diseases in fish. Appl Environ Microbiol. 2001, 67: 2430-2435. 10.1128/AEM.67.6.2430-2435.2001.
Balcázar JL, Vendrell D, de Blas I, Ruiz-Zarzuela I, Muzquiz JL, Girones O: Characterization of probiotic properties of lactic acid bacteria isolated from intestinal microbiota of fish. Aquaculture. 2008, 278: 188-191. 10.1016/j.aquaculture.2008.03.014.
Merrifield DL, Dimitroglou A, Foey A, Davies SJ, Baker RTM, Bøgwald J, Castex M, Ringø E: The current status and future focus of probiotic and prebiotic applications for salmonids. Aquaculture. 2010, 302: 1-18. 10.1016/j.aquaculture.2010.02.007.
Das S, Ward LR, Burke C: Screening of marine Streptomyces spp. for potential use as probiotics in aquaculture. Aquaculture. 2010, 305: 32-41. 10.1016/j.aquaculture.2010.04.001.
Wang Y-B, Tian Z-Q, Yao J-T, Li W: Effect of probiotics, Enteroccus faecium, on tilapia (Oreochromis niloticus) growth performance and immune response. Aquaculture. 2008, 277: 203-207. 10.1016/j.aquaculture.2008.03.007.
Olmos J, Ochoa L, Paniagua-Michel J, Contreras R: Functional feed assessment on Litopenaeus vannamei using 100% fish meal replacement by soybean meal, high levels of complex carbohydrates and Bacillus probiotic strains. Mar Drugs. 2011, 9: 1119-1132. 10.3390/md9061119.
Eaton TJ, Gasson MJ: Molecular screening of Enterococcus virulence determinants and potential for genetic exchange between food and medical isolates. Appl Environ Microbiol. 2001, 67: 1628-1635. 10.1128/AEM.67.4.1628-1635.2001.
Gomes BC, Esteves CT, Palazzo IC, Darini AL, Felis GE, Sechi LA, Franco BD, De Martinis EC: Prevalence and characterization of Enterococcus spp. isolated from Brazilian foods. Food Microbiol. 2008, 25: 668-675. 10.1016/j.fm.2008.03.008.
López M, Sáenz Y, Rojo-Bezares B, Martínez S, del Campo R, Ruiz-Larrea F, Zarazaga M, Torres C: Detection of vanA and vanB2-containing enterococci from food samples in Spain, including Enterococcus faecium strains of CC17 and the new singleton ST425. Int J Food Microbiol. 2009, 133: 172-178. 10.1016/j.ijfoodmicro.2009.05.020.
Vankerckhoven V, Van Autgaerden T, Vael C, Lammens C, Chapelle S, Rossi R, Jabes D, Goossens H: Development of a multiplex PCR for the detection of asa1, gelE, cylA, esp, and hyl genes in enterococci and survey for virulence determinants among European hospital isolates of Enterococcus faecium. J Clin Microbiol. 2004, 42: 4473-4479. 10.1128/JCM.42.10.4473-4479.2004.
Klare I, Konstabel C, Mueller-Bertling S, Werner G, Strommenger B, Kettlitz C, Borgmann S, Schulte B, Jonas D, Serr A, et al: Spread of ampicillin/vancomycin-resistant Enterococcus faecium of the epidemic-virulent clonal complex-17 carrying the genes esp and hyl in German hospitals. Eur J Clin Microbiol Infect Dis. 2005, 24: 815-825. 10.1007/s10096-005-0056-0.
Werner G, Coque TM, Hammerum AM, Hope R, Hryniewicz W, Johnson A, Klare I, Kristinsson KG, Leclercq R, Lester CH, et al: Emergence and spread of vancomycin resistance among enterococci in Europe. Euro Surveill. 2008, 13: 1-11.
Ogier JC, Serror P: Safety assessment of dairy microorganisms: the Enterococcus genus. Int J Food Microbiol. 2008, 126: 291-301. 10.1016/j.ijfoodmicro.2007.08.017.
Danielsen M, Wind A: Susceptibility of Lactobacillus spp. to antimicrobial agents. Int J Food Microbiol. 2003, 82: 1-11. 10.1016/S0168-1605(02)00254-4.
Vay C, Cittadini R, Barberis C, Hernán Rodríguez C, Perez Martínez H, Genero F, Famiglietti A: Antimicrobial susceptibility of non-enterococcal intrinsic glycopeptide-resistant Gram-positive organisms. Diagn Microbiol Infect Dis. 2007, 57: 183-188. 10.1016/j.diagmicrobio.2006.08.014.
Ammor MS, Flórez AB, Mayo B: Antibiotic resistance in non-enterococcal lactic acid bacteria and bifidobacteria. Food Microbiol. 2007, 24: 559-570. 10.1016/j.fm.2006.11.001.
Danielsen M, Simpson PJ, O'Connor EB, Ross RP, Stanton C: Susceptibility of Pediococcus spp. to antimicrobial agents. J Appl Microbiol. 2007, 102: 384-389.
Klare I, Konstabel C, Badstübner D, Werner G, Witte W: Occurrence and spread of antibiotic resistances in Enterococcus faecium. Int J Food Microbiol. 2003, 88: 269-290. 10.1016/S0168-1605(03)00190-9.
Albarracín Orio AG, Piñas GE, Cortes PR, Cian MB, Echenique J: Compensatory evolution of pbp mutations restores the fitness cost imposed by beta-lactam resistance in Streptococcus pneumoniae. PLoS Pathog. 2011, 7: e1002000-10.1371/journal.ppat.1002000.
Piuri M, Sanchez-Rivas C, Ruzal SM: Cell wall modifications during osmotic stress in Lactobacillus casei. J Appl Microbiol. 2005, 98: 84-95. 10.1111/j.1365-2672.2004.02428.x.
Klein G, Hallmann C, Casas IA, Abad J, Louwers J, Reuter G: Exclusion of vanA, vanB and vanC type glycopeptide resistance in strains of Lactobacillus reuteri and Lactobacillus rhamnosus used as probiotics by polymerase chain reaction and hybridization methods. J Appl Microbiol. 2000, 89: 815-824. 10.1046/j.1365-2672.2000.01187.x.
Ayeni FA, Sánchez B, Adeniyi BA, de Los Reyes-Gavilán CG, Margolles A, Ruas-Madiedo P: Evaluation of the functional potential of Weissella and Lactobacillus isolates obtained from Nigerian traditional fermented foods and cow's intestine. Int J Food Microbiol. 2011, 147: 97-104. 10.1016/j.ijfoodmicro.2011.03.014.
Ayeni FA, Adeniyi BA, Ogunbanwo ST, Tabasco R, Paarup T, Peláez C, Requena T: Inhibition of uropathogens by lactic acid bacteria isolated from dairy foods and cow's intestine in western Nigeria. Arch Microbiol. 2009, 191: 639-648. 10.1007/s00203-009-0492-9.
Del Grosso M, Iannelli F, Messina C, Santagati M, Petrosillo N, Stefani S, Pozzi G, Pantosti A: Macrolide efflux genes mef(A) and mef(E) are carried by different genetic elements in Streptococcus pneumoniae. J Clin Microbiol. 2002, 40: 774-778. 10.1128/JCM.40.3.774-778.2002.
Bozdogan B, Berrezouga L, Kuo MS, Yurek DA, Farley KA, Stockman BJ, Leclercq R: A new resistance gene, linB, conferring resistance to lincosamides by nucleotidylation in Enterococcus faecium HM1025. Antimicrob Agents Chemother. 1999, 43: 925-929.
Roberts MC, Sutcliffe J, Courvalin P, Jensen LB, Rood J, Seppala H: Nomenclature for macrolide and macrolide-lincosamide-streptogramin B resistance determinants. Antimicrob Agents Chemother. 1999, 43: 2823-2830.
Leclercq R: Mechanisms of resistance to macrolides and lincosamides: nature of the resistance elements and their clinical implications. Clin Infect Dis. 2002, 34: 482-492. 10.1086/324626.
Achard A, Villers C, Pichereau V, Leclercq R: New lnu(C) gene conferring resistance to lincomycin by nucleotidylation in Streptococcus agalactiae UCN36. Antimicrob Agents Chemother. 2005, 49: 2716-2719. 10.1128/AAC.49.7.2716-2719.2005.
Marteau P, Gerhardt MF, Myara A, Bouvier E, Trivin F, Rambaud JC: Metabolism of bile salts by alimentary bacteria during transit in the human small intestine. Microb Ecol Health D. 1995, 8: 151-157. 10.3109/08910609509140093.
Ruseler-van Embden JG, van Lieshout LM, Gosselink MJ, Marteau P: Inability of Lactobacillus casei strain GG, L. acidophilus, and Bifidobacterium bifidum to degrade intestinal mucus glycoproteins. Scand J Gastroenterol. 1995, 30: 675-680. 10.3109/00365529509096312.
Heavey PM, Rowland IR: Microbial-gut interactions in health and disease, Gastrointestinal cancer. Best Pract Res Clin Gastroenterol. 2004, 18: 323-336. 10.1016/j.bpg.2003.10.003.
Begley M, Gahan CG, Hill C: The interaction between bacteria and bile. FEMS Microbiol Rev. 2005, 29: 625-651. 10.1016/j.femsre.2004.09.003.
Zhou JS, Gopal PK, Gill HS: Potential probiotic lactic acid bacteria Lactobacillus rhamnosus (HN001), Lactobacillus acidophilus (HN017) and Bifidobacterium lactis (HN019) do not degrade gastric mucin in vitro. Int J Food Microbiol. 2001, 63: 81-90. 10.1016/S0168-1605(00)00398-6.
Delgado S, O'Sullivan E, Fitzgerald G, Mayo B: Subtractive screening for probiotic properties of Lactobacillus species from the human gastrointestinal tract in the search for new probiotics. J Food Sci. 2007, 72: M310-M315. 10.1111/j.1750-3841.2007.00479.x.
Muñoz-Atienza E, Landeta G, De Las Rivas B, Gómez-Sala B, Muñoz R, Hernández PE, Cintas LM, Herranz C: Phenotypic and genetic evaluations of biogenic amine production by lactic acid bacteria isolated from fish and fish products. Int J Food Microbiol. 2011, 146: 212-216. 10.1016/j.ijfoodmicro.2011.02.024.
Ladero V, Fernández M, Calles-Enríquez M, Sánchez-Llana E, Canedo E, Martín MC, Alvarez MA: Is the production of the biogenic amines tyramine and putrescine a species-level trait in enterococci?. Food Microbiol. 2012, 30: 132-138. 10.1016/j.fm.2011.12.016.
Ringø E, Strom E, Tabachek JA: Intestinal microflora of salmonids: a review. Aquac Res. 1995, 26: 773-789. 10.1111/j.1365-2109.1995.tb00870.x.
Bairagi A, Sarkar Ghosh K, Sen SK, Ray AK: Enzyme producing bacterial flora isolated from fish digestive tracts. Aquacult Int. 2002, 10: 109-121. 10.1023/A:1021355406412.
Ramirez RF, Dixon BA: Enzyme production by obligate intestinal anaerobic bacteria isolated from oscars (Astronotus ocellatus), angelfish (Pterophyllum scalare) and southern flounder (Paralichthys lethostigma). Aquaculture. 2003, 227: 417-426. 10.1016/S0044-8486(03)00520-9.
Fjellheim AJ, Klinkenberg G, Skjermo J, Aasen IM, Vadstein O: Selection of candidate probionts by two different screening strategies from Atlantic cod (Gadus morhua L.) larvae. Vet Microbiol. 2010, 144: 153-159. 10.1016/j.vetmic.2009.12.032.
Kullen MJ, Sanozky-Dawes RB, Crowell DC, Klaenhammer TR: Use of the DNA sequence of variable regions of the 16S rRNA gene for rapid and accurate identification of bacteria in the Lactobacillus acidophilus complex. J Appl Microbiol. 2000, 89: 511-516. 10.1046/j.1365-2672.2000.01146.x.
Poyart C, Quesnes G, Trieu-Cuot P: Sequencing the gene encoding manganese-dependent superoxide dismutase for rapid species identification of enterococci. J Clin Microbiol. 2000, 38: 415-418.
Cintas LM, Rodríguez JM, Fernández MF, Sletten K, Nes IF, Hernández PE, Holo H: Isolation and characterization of pediocin L50, a new bacteriocin from Pediococcus acidilactici with a broad inhibitory spectrum. Appl Environ Microbiol. 1995, 61: 2643-2648.
Gilmore MS, Segarra RA, Booth MC, Bogie CP, Hall LR, Clewell DB: Genetic structure of the Enterococcus faecalis plasmid pAD1-encoded cytolytic toxin system and its relationship to lantibiotic determinants. J Bacteriol. 1994, 176: 7335-7344.
Hickey RM, Twomey DP, Ross RP, Hill C: Production of enterolysin A by a raw milk enterococcal isolate exhibiting multiple virulence factors. Microbiology. 2003, 149: 655-664. 10.1099/mic.0.25949-0.
CLSI: Performance Standards for Antimicrobial Susceptibility Testing: Twenty–first Informational Supplement M100–S21. 2011, Wayne, PA, USA: CLSI
Klare I, Konstabel C, Müller-Bertling S, Reissbrodt R, Huys G, Vancanneyt M, Swings J, Goossens H, Witte W: Evaluation of new broth media for microdilution antibiotic susceptibility testing of Lactobacilli, Pediococci, Lactococci, and Bifidobacteria. Appl Environ Microbiol. 2005, 71: 8982-8986. 10.1128/AEM.71.12.8982-8986.2005.
Noriega L, Cuevas I, Margolles A, Reyes-Gavilán CG Dl: Deconjugation and bile salts hydrolase activity by Bifidobacterium strains with acquired resistance to bile. Int Dairy J. 2006, 16: 850-855. 10.1016/j.idairyj.2005.09.008.
Donabedian SM, Thal LA, Hershberger E, Perri MB, Chow JW, Bartlett P, Jones R, Joyce K, Rossiter S, Gay K, et al: Molecular characterization of gentamicin-resistant Enterococci in the United States: evidence of spread from animals to humans through food. J Clin Microbiol. 2003, 41: 1109-1113. 10.1128/JCM.41.3.1109-1113.2003.
Sutcliffe J, Grebe T, Tait-Kamradt A, Wondrack L: Detection of erythromycin-resistant determinants by PCR. Antimicrob Agents Chemother. 1996, 40: 2562-2566.
Sutcliffe J, Tait-Kamradt A, Wondrack L: Streptococcus pneumoniae and Streptococcus pyogenes resistant to macrolides but sensitive to clindamycin: a common resistance pattern mediated by an efflux system. Antimicrob Agents Chemother. 1996, 40: 1817-1824.
Strommenger B, Kettlitz C, Werner G, Witte W: Multiplex PCR assay for simultaneous detection of nine clinically relevant antibiotic resistance genes in Staphylococcus aureus. J Clin Microbiol. 2003, 41: 4089-4094. 10.1128/JCM.41.9.4089-4094.2003.
Werner G, AWillems RJ, Hildebrandt B, Klare I, Witte W: Influence of transferable genetic determinants on the outcome of typing methods commonly used for Enterococcus faecium. J Clin Microbiol. 2003, 41: 1499-1506. 10.1128/JCM.41.4.1499-1506.2003.
Lina G, Quaglia A, Reverdy ME, Leclercq R, Vandenesch F, Etienne J: Distribution of genes encoding resistance to macrolides, lincosamides, and streptogramins among staphylococci. Antimicrob Agents Chemother. 1999, 43: 1062-1066.
Acknowledgements
This work was partially supported by projects AGL2009 − 08348-ALI from Ministerio de Ciencia y Tecnología (MCYT), Spain; GR35/10-A from Banco Santander-Central Hispano-Universidad Complutense de Madrid (UCM), Spain; S − 2009/AGR − 1489 from Dirección General de Universidades e Investigación, Consejería de Educación, Comunidad de Madrid, Spain, and Spanish-Portuguese Integrated Action HP2008-0070 from Ministerio de Ciencia e Innovación (MICINN), Spain. E. Muñoz-Atienza is recipient of a predoctoral fellowship from UCM, Spain. C. Araújo is financially supported by a predoctoral fellowship from Fundação da Ciência e Tecnologia, Portugal. C. Campanero holds a predoctoral fellowship from UCM, Spain. The authors express their gratitude to Dr. C. Michel, INRA, Jouy-en-Josas, France, for providing a number of fish pathogens strains used as indicators and to Dr. C. Torres, Universidad de la Rioja, Spain; Dr. T.J. Eaton, Institute of Food Research, Norwich, United Kingdom, and Dr. V. Vankerckhoven, University of Antwerp, Belgium, for supplying strains used as PCR controls.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
EMA carried out the phenotypic and genetic analyses, prepared the manuscript draft and participated in the design of the experiments. BGS carried out the isolation of the LAB strains and collaborated in the genetic studies. CA contributed to the phenotypic analyses and to prepare the manuscript draft. CC participated in the phenotypic analyses. RC collaborated in the antibiotic susceptibility tests. LMC conceived the study and, together with CH and PEH, designed the experiments, analyzed the results and revised the manuscript. All authors read and approved the final version of the manuscript.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Muñoz-Atienza, E., Gómez-Sala, B., Araújo, C. et al. Antimicrobial activity, antibiotic susceptibility and virulence factors of Lactic Acid Bacteria of aquatic origin intended for use as probiotics in aquaculture. BMC Microbiol 13, 15 (2013). https://doi.org/10.1186/1471-2180-13-15
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2180-13-15