Abstract
Data obtained by the authors upon creating composite materials based on biopolymers and calcium phosphates adapted to the prototyping technology are presented. Results concerning the creation and investigation of the properties of three-dimensional structures for the replacement of bone defects, as well as novel studies of the functionalization of three-dimensional prototypes based on calcium phosphates and a biopolymer, namely, modification of the surface of mineral–polymer materials by the biomimetic application of active calcium phosphates, are shown.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Despite the fact that a wide range of osteoplastic materials (metallic materials, silicates, calcium phosphate ceramics, biopolymers) are used in existing medical methods, a significant number of studies have been carried out that are aimed both at developing novel materials and at studying the methods for modification and functionalization of implants for the recovery of damaged bone tissues [1, 2].
A large number of works are aimed at creating materials based on calcium phosphates—in particular, ceramics based on tricalcium phosphate (TCP) and octacalcium phosphate (OCP) is commonly considered promising. Such a trend in the studies is determined by several reasons: TCP and OCP ceramics possess a relatively high solubility in the body fluids and promotes the process of biomineralization of the bone tissue being formed [3].
The modern methods for the development of osteoplastic materials are based on the direct fundamental perceptions of the composition and structure of the human bone tissue, which mainly consists of collagen fibrils and biological apatite. It can be stated based on the analysis of the published data that the matrices fabricated from the composite materials of the biopolymer–calcium phosphate type have better physicochemical and biomechanical properties than do ceramic or metallic ones.
Biopolymers possess an enormous potential for various applications in biomedical studies and clinical practice. Biocompatible polymers of various natures and ceramic fillers with various architectonics of the surface, namely, from powders to spherical granules, are used for the creation of composite materials (CMs) [4, 5]. Materials based on the biopolymers of animal and vegetable origin, such as sodium alginate, chitosan, pectin, gelatin, collagen, and fibrinogen, are of special interest due to the wide spectrum of their useful properties such as biocompatibility and bioresorbability. Today, such materials are widely used in various materials for medical use, including for the regeneration of soft and hard tissues, as homeostatic agents, as drug delivery platforms, as growth factors, and as immune system stimulators against viral and bacterial infections [6, 7].
In the creation of three-dimensional composite structures based on polymers and calcium phosphates (CPs), special hopes are placed on the methods of fast prototyping (or additive production) [8]. The three-dimensional model of the required fragment of the patient’s tissue can be obtained on, e.g., a high-resolution X-ray computed tomograph, and then a precise copy thereof—a structure made of biocompatible materials—can be rapidly fabricated. In the process of fabrication of an osteoplastic product, it can be supplemented with certain details, and the creation of the required architectonics can be programmed. Three-dimensional printing (3D printing) should be distinguished in first place among the most thus far developed fast prototyping methods and additive production technologies that make it possible to use various calcium phosphates and polymers as the initial materials [9].
Methods of three-dimensional jet printing of ceramic matrices and methods of fabrication of various tissue-engineered structures based on them have experienced active development in the last decade. However, purely ceramic matrices are characterized by high rigidity and fragility. The possibility of combining ceramic and polymer components and capabilities of three-dimensional printing are directly associated with the creation of novel materials and development of the additive technologies of formation of personalized three-dimensional tissue-engineered structures intended for the elimination of the defects of bone tissues of various origins [10, 11].
Further functionalization of the developed materials is a relevant, scientifically and practically justified task. The functional orientation of nanostructured materials means the possibility of their multipurpose use, namely, not only as a “simple” implantation material, but also as a nanobiostructure with a bioinspired surface containing biologically active molecules (growth factors) or medicines.
The development of such materials and fabrication technology will make it possible to provide the possibility for creating a universal three-dimensional new-generation nanobiostructure at the level of global developments. The possibility of imparting the required properties to the biological systems for the replacement of an osteohondrous defect and use as containers for the local delivery of various medicines to the region of a surgical wound will lead to advancements in the field of biology and medicine [12–14]. In other words, the bioinspiration of the surface of biocompatible materials adapted for the prototyping technology at a nanolevel provides the sorption of various biologically active substances from biological fluids, which will be provide high-quality osteointegration of the implant with the parent bed tissues and the formation of a tissue-specific bone equivalent in a short time.
In the case of modification of the surfaces of an implant with a layer of calcium phosphate, a significant increase in the osteoinduction properties can be achieved. The known methods used for the application of a layer of calcium phosphate onto the surface of implants, such as electrochemical deposition, plasma spraying, sol–gel deposition, electrophoretic deposition, ionic deposition, hot isostatic pressing, and laser-assisted deposition [15, 16], are associated with physical conditions that are far from physiological and, most importantly, are carried out at quite high temperatures. The application of a calcium phosphate coating onto an implant by the high-temperature method excludes the possibility for introducing biological molecules and may lead to thermal decomposition of the material. Therefore, in most cases, biological objects cannot be applied onto the surface of implants [17–20].
The method of biomimetic application of calcium phosphates presupposes the use of physiological temperatures for the modification of the surface. This makes it possible to functionalize materials of various natures and incorporate biological agents (proteins, growth factors) without sacrificing their biological activity. Also, the possibility for applying such a method for complex-geometry implants, in particular, on 3D materials, is a clear advantage, because the physicochemical and morphological properties of biomimetic coatings do not depend on the three-dimensional structure of the material being modified (Fig. 1) [21, 22].
The procedure for application of calcium phosphates onto the material includes the stage of formation of a biomimetic active layer of carbonate-containing amorphous calcium phosphate on the surface. The formation of such a calcium phosphate layer is associated with the oversaturation of isotonic solutions with calcium and phosphorus ions and dissolution–deposition processes occurring as a result of the migrations of these ions. A simulation body fluid (SBF) buffer solution that models the extracellular body fluid with respect to its composition is one of the most widely used for such a method of surface modification [23–25]. Such a fluid is generally close to the blood plasma with respect to the composition and contains phosphate and carbonate ions. Crystallization of calcium phosphates on the surface of the material occurs as a result of the change in the product of the ionic activities in the fluid and in the case of the presence of the corresponding sites [28].
Low-temperature coatings based on calcium phosphates can be obtained by biomimetic deposition on the materials of various natures including polymer scaffolds resistant to dissolution. In such cases, the matrices are immersed into salt buffer solutions to create crystallization sites, with two- and threefold solutions of SBF most often being used for these purposes. Increasing the factor of the solution is associated with the need for the oversaturation of calcium and phosphorus ions for the crystallization of calcium phosphates on the created sites. The thickness of the biomimetic layer increases in time, and the rate of its formation increases with the degree of oversaturation of SBF. The phase composition of the coating depends on the chemical composition of SBF and its factor; one can deposit both amorphous and apatite-like calcium phosphate by varying the concentration of its specific components. Therefore, a coating based on octacalcium phosphate can be obtained, the preparation procedure of which is close to biomimetic deposition, which makes it the most promising surface-incorporable coating [27, 28].
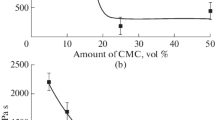
The study of the modification of the surfaces of TCP and OCP ceramics by biomimetic decomposition with the use of fluids mimicking body fluids (SBFs) found the effect of the concentration of the solutions and time of exposure of 1–30 days on the structure and properties of the materials. To study the possibility of surface modification of the ceramics, the experiments were performed in 1, 2, and 3 M solutions of SBF.
The effect of the concentration of the solutions and time of exposure on the microstructure of the surface, phase composition, and properties of the materials was found using modern study methods. Upon immersing the material into a solution, the Ca2+, P\({\text{O}}_{4}^{{3 - }}\), C\({\text{O}}_{3}^{{2 - }}\), and OH– ions can interact between each other in the process of deposition. In a neutral medium (pH 7.4), HP\({\text{O}}_{4}^{{2 - }}\) is formed upon the interaction of phosphate ions with protons. These ions can interact with calcium ions; here, the product of their interaction deposits on the surface in the form of less soluble CaHPO4. In addition, some C\({\text{O}}_{3}^{{2 - }}\) and OH– ions can also interact with calcium ions to form calcite and hydroxide. The deposition–dissolution process apparently proceeds immediately by several reaction mechanisms and depends on the concentration of calcium in the initial buffer solution [29].
However, the value of the pH of the solution shifts from neutral to acidic (with calcium deficiency) with an increase in the time of exposure, while the process of deposition decelerates together with the increase in the rate of dissolution of the coating. Such processes of dissolution–deposition type are most likely observed in the case of implantation of ceramic materials in vivo.
Based on the obtained data, the justified conclusion can be drawn that modern developments and studies in the field of creation of materials for the replacement of the bone tissue are aimed at obtaining a nanostructured material/coating. This is mainly associated with the increased biological activity of such implants and possibility for their multipurpose use as biostructures containing growth factors, medicinal products, and biologically active molecules. The application of such materials will make it possible to achieve high-quality osteogenesis in the case of replacement of complex-geometry critical defects and decrease the frequency of infectious complications of bone wounds.
REFERENCES
A. Oryan, S. Alidadi, A. Moshiri, and N. Maffulli, “Bone regenerative medicine: Classic options, novel strategies, and future directions,” J. Ortho P. Surg. Res. 9 (1), 18–42 (2014).
A. Kolk, J. Handschel, W. Drescher, et al., “Current trends and future perspectives of bone substitute materials – from space holders to innovative biomaterials,” J. Craniomaxillofac. Surg. 40 (8), 706–718 (2012).
O. Suzuki, “Octacalcium phosphate (OCP)-based bone substitute materials,” Jpn. Dental Sci. Rev. 49, 58–71 (2013).
V. K. Popov, V. S. Komlev, and B. N. Chichkov, “Calcium phosphate blossom for bone tissue engineering,” Mater. Today 2, 96–97 (2014).
M. Stoppato, S. Vahabzadeh, and A. Bandyopadhyay, “Bone tissue engineering using 3D printing,” Bioact. Compat. Polym. 28, 16–32 (2013).
S. N. Pawar and K. J. Edgar, “Alginate derivatization: A review of chemistry, properties, and applications,” Biomaterials 33, 3279–3305 (2012).
M. H. Sun, et al., “Applications of hierarchically structured porous materials from energy storage and conversion, catalysis, photocatalysis, adsorption, separation, and sensing to biomedicine,” Chem. Soc. Rev. 45 (12), 3479–3563 (2016).
J. Kundu, F. Pati, J.-H. Shim, and D.-W. Cho, Rapid Prototyping Technology for Bone Regeneration. Principles and Applications (Woodhead Publ., Sawston, Cambridge, 2014), pp. 254–284.
S. M. Barinov and V. S. Komlev, Bioceramics Based on Calcium Phosphates (Nauka, Moscow, 2005) [in Russian].
X. Du, S. Fu, and Y. Zhu, “3D printing of ceramic-based scaffolds for bone tissue engineering: An overview,” J. Mater. Chem. B 6 (27), 4397–4412.
M. Stoppato, S. Vahabzadeh, and A. Bandyopadhyay, “Bone tissue engineering using 3D printing,” Bioact. Compat. Polym. 28, 16–32 (2013).
S. N. Rath, L. A. Strobe, A. Arkudas, J. P. Beier, A. K. Maier, P. Greil, et al., “Osteoinduction and survival of osteoblasts and bone-marrow stromal cells in 3D biphasic calcium phosphate scaffolds under static and dynamic culture conditions,” J. Cell. Mol. Med. 16, 2350–2361 (2012).
V. S. Komlev, V. K. Popov, A. V. Mironov, A. Yu. Fedotov, A. Yu. Teterina, I. V. Smirnov, I. Y. Bozo, V. A. Rybko, and R. V. Deev, “3D printing of octacalcium phosphate bone substitutes,” Front. Bioeng. Biotechnol. 3, 1–7 (2015).
M. Vallet-Regí, D. A. Navarrete, and D. Arcos, Biomimetic Nanoceramics in Clinical Use: From Materials to Applications (R. Soc. Chem., 2008).
S. Samavedi, A. R. Whittington, and A. S. Goldstein, “Calcium phosphate ceramics in bone tissue engineering: A review of properties and their influence on cell behavior,” Acta Biomater. 9 (9), 8037 (2013).
L. G. Daculsi, in CRC Handbook of Bioactive Ceramics, Ed. by T. Yamamuro, L. Hench, and J. Wilson-Hench (CRC Press, Boca Raton, FL, 1990).
X. Du, S. Fu, and Y. Zhu, “3D printing of ceramic-based scaffolds for bone tissue engineering: An overview,” J. Mater. Chem. B 6 (27), 4397–4412.
G. Tozzi, A. De Mori, A. Oliveira, and M. Roldo, “Composite hydrogels for bone regeneration,” Materials 9, 267–291 (2016).
B. Palazzo, S. Scialla, F. Scalera, N. Margiotta, and F. Gervaso, “Nanostructured ceramics and bioceramics for bone cancer treatment,” in Advanced Composite Materials (Wiley Online Library, 2016), pp. 209–273.
H. Liu et al., “A functional chitosan-based hydrogel as a wound dressing and drug delivery system in the treatment of wound healing,” RSC Adv. 8 (14), 7533–7549 (2018).
A. Krząkała, A. Kazek-Kęsik, and W. Simka, “Application of plasma electrolytic oxidation to bioactive surface formation on titanium and its alloys,” RSC Adv. 3 (43), 19725–19743 (2013).
S. Tao et al., “The remineralization effectiveness of PAMAM dendrimer with different terminal groups on demineralized dentin in vitro,” RSC Adv. 7 (87), 54947–54955 (2017).
X. Yu and M. Wei, “Preparation and evaluation of parathyroid hormone incorporated CaP coating via a biomimetic method,” J. Biomed. Mater. Res., Part B: Appl. Biomater. 97, 345–354 (2011).
Y. Li, Octacalcium Phosphate-Metabolite Composites: Model Compounds for Bone Mineral Structure (Univ. Cambridge, 2018).
M. Gelinsky, “Mineralised collagen as biomaterial and matrix for bone tissue engineering,” in Fundamentals of Tissue Engineering and Regenerative Medicine, Ed. by U. Meyer, Th. Meyer, J. Handschel, and H.-P. Wiesmann (Springer, Heidelberg–Berlin, 2009), pp. 485–493.
X. Chen et al., “Biomimetic preparation of trace element-codoped calcium phosphate for promoting osteoporotic bone defect repair,” J. Mater. Chem. B 1 (9), 1316–1325.
O. Suzuki, “Octacalcium phosphate (OCP)-based bone substitute materials,” Jpn. Dental Sci. Rev. 49 (2), 58–71 (2013).
H. Shi et al., “Formation and stability of well-crystallized metastable octacalcium phosphate at high temperature by regulating the reaction environment with carbamide,” CrystEngComm 21 (34), 5174–5184 (2019).
V. S. Komlev, S. M. Barinov, I. I. Bozo, R. V. Deev, I. I. Eremin, A. Yu. Fedotov, A. N. Gurin, N. V. Khromova, P. Kopnin, E. A. Kuvshinova, V. E. Mamonov, V. A. Rybko, N. S. Sergeeva, A. Yu. Teterina, and V. L. Zorin, “Bioceramics composed of octacalcium phosphate demonstrate enhanced biological behavior,” ACS Appl. Mater. Interfaces 6 (19), 16610–16620 (2014).
Funding
A. Teterina is grateful to the Russian Foundation for Basic Research for financial support, project no. 18-33-00955 mol_a. Some works presented in this paper were performed as part of state assignment no. 007-00129-18-00.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare that they have no conflicts of interest.
Additional information
Translated by E. Boltukhina
Rights and permissions
About this article
Cite this article
Teterina, A.Y., Baranov, O.V., Mikheeva, P.V. et al. Developments in the Field of Biocompatible Composite Materials Based on Biopolymers and Calcium Phosphates Adapted to Prototyping Technology. Polym. Sci. Ser. D 14, 265–268 (2021). https://doi.org/10.1134/S1995421221020349
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S1995421221020349