Abstract
We evaluated the relationship between daily stair climbing activity and vascular function as assessed by flow-mediated vasodilation (FMD) and nitroglycerine-induced vasodilation (NID). This study was a cross-sectional study. A total of 374 patients with hypertension were enrolled. The subjects were divided into three groups based on their daily stair climbing habit: no stairs group, climbing stairs to the 2nd-floor group, and climbing stairs to the ≥3rd-floor group. There was a significant difference in FMD between the ≥3rd-floor group and the other two groups (3.3 ± 2.5% vs. 2.3 ± 2.7% and 2.4 ± 2.7%, p = 0.02, respectively). FMD values were similar in the no stairs group and the 2nd-floor group (p = 0.96). There was a significant difference in NID between the no stairs group and the other two groups (7.4 ± 4.2% vs. 10.9 ± 5.3% and 11.3 ± 5.1%, p < 0.001, respectively). NID values were similar in the second-floor group and the ≥3rd-floor group (p = 0.86). These findings suggest that both endothelial function and vascular smooth muscle function are impaired in individuals who do not climb stairs and that endothelial function but not vascular smooth muscle function is impaired in individuals who climb stairs to the second floor compared with individuals who climb stairs to the ≥3rd floor. Stair climbing activity, a simple method for assessing daily physical activity, may reflect vascular function in patients with hypertension.
Similar content being viewed by others
Introduction
Physical inactivity is a well-established risk factor for all-cause mortality, and physical activity is a well-established protective factor [1]. According to the World Health Organization (WHO), physical inactivity is the fourth leading risk factor for mortality (6%) worldwide. The American Heart Association, the American College of Cardiology, and WHO recommend 150 min of moderate-intensity activity per week or 75 min of vigorous-intensity activity per week [2, 3]. However, too few people reach these exercise goals. Previous studies have shown that one-third to one-half of adults do not follow the recommendations for exercise [4, 5]. Recently, it has been reported that stair climbing activity reflects daily physical activity. Stair climbing activity requires more muscle strength and more energy than walking on flat ground or downstairs [6]. Stair climbing activity gives the body the equivalent of 4 METs and moderate-intensity exercise [7]. Therefore, stair climbing activity is used for rehabilitation and assessment of exercise tolerance. A previous study showed that subjects who regularly climbed stairs had a lower risk of coronary heart disease than did subjects who did not regularly climb stairs [8]. Assessment of stair climbing should be a useful and simple marker for daily physical activity.
Hypertension is one of the most important risk factors for several diseases, including myocardial infarction, stroke, heart failure, kidney disease, and vascular dementia, as well as impaired activities of daily living [9,10,11,12,13,14]. A previous meta-analysis showed that aerobic exercise reduces blood pressure [15], and it has been shown those exercise benefits patients with hypertension by improving oxidative stress [16]. Guidelines for the management of hypertension recommend physical activity for controlling blood pressure and preventing cardiovascular events in patients with hypertension [3, 17, 18].
Endothelial dysfunction caused by traditional cardiovascular risk factors, including hypertension, is the initial step in the pathogenesis of atherosclerosis, and it leads to cardiovascular events [19,20,21]. Measurement of flow-mediated vasodilation (FMD) in the brachial artery is an established tool for the assessment of endothelial function. FMD is useful for assessing the present cardiovascular risk and for predicting cardiovascular events [22,23,24,25].
Previous studies, including ours, have shown that aerobic exercise improves and augments endothelial function in patients with cardiovascular disease (CVD) and even in healthy subjects [26, 27]. However, there is no information on the relationship between daily stair climbing activity and vascular function, and the level of stair climbing activity that has beneficial effects on vascular function remains unclear. Therefore, we examined the relationships between daily stair climbing activity and vascular function assessed by FMD as an index of endothelial function and nitroglycerine-induced vasodilation (NID) as an index of vascular smooth muscle function in patients with hypertension.
Methods
Study subjects
A total of 374 patients with hypertension who underwent a health checkup at Hiroshima University between January 2016 and January 2021 were enrolled in this study. We excluded subjects with severe chronic heart failure (New York Heart Association level >III), subjects being treated with nitrate, subjects without information on their daily stair climbing habit, and subjects who could not climb stairs. Hypertension was defined as the use of antihypertensive drugs, systolic blood pressure of more than 140 mm Hg or diastolic blood pressure of more than 90 mm Hg measured in a sitting position on at least 3 occasions. Dyslipidemia was defined according to the third report of the National Cholesterol Education Program [28]. Diabetes mellitus was defined according to the American Diabetes Association recommendation [29]. CVD was defined as coronary heart disease or cerebrovascular disease. Coronary heart disease included angina pectoris, prior myocardial infarction, and unstable angina. Cerebrovascular disease included ischemic stroke, hemorrhagic stroke, and transient ischemic attack. The Ethics Committee of Hiroshima University approved the study protocol. Written informed consent for participation in this study was obtained from all participants.
Study protocol
This study was a cross-sectional study. Subjects were divided into three groups based on information on daily stair climbing activity: no stairs group, climbing stairs to the second-floor group, and climbing stairs to the ≥3rd-floor group. We assessed vascular function in each group. Multivariate regression analysis was performed to identify independent variables associated with vascular function. The subjects were next divided into two groups: climbing stairs to the <3rd floor and climbing stairs to the ≥3rd floor. The subjects were also divided into two other groups: no stairs and climbing stairs to the ≥2nd floor. Finally, we assessed the relationships between daily stair climbing activity and FMD and NID using propensity score matching. The subjects fasted overnight and abstained from drinking alcohol, smoking, and taking caffeine and antioxidant vitamins for at least 12 h before the study. The participants were kept in the supine position in a quiet, dark, air-conditioned room (constant temperature of 22–25 °C) throughout the study. A 23-gauge polyethylene catheter was inserted into the deep antecubital vein to obtain blood samples. After they lay in the supine position for 30 min, FMD and NID were measured. The observers were blinded to the form of examination.
Evaluation of stair climbing activity
Information on physical activity was obtained by using the self-reported modified international physical activity questionnaire (IPAQ). This questionnaire consists of questions on exercise habit, the frequency with which they engaged in each intensity of exercise (light intensity, moderate intensity, and vigorous-intensity) for more than 10 min (times/week), duration of each exercise time (minutes), sitting time (hours/week) and daily stair climbing activity. The intensity of exercise was estimated based on the type of exercise using the compendium of physical activities [30]. Based on the information provided in the questionnaire, we calculated the duration of exercise per week for each subject. Information on daily stair climbing activity was obtained by the following question: up to how many flights of stairs do you usually climb? We defined ground level as the first floor and the floor above the first floor as the second floor.
Measurements of FMD and NID
A high-resolution linear artery transducer was coupled to computer-assisted analysis software (UNEXEF18G, UNEX Co., Nagoya, Japan) that used an automated edge detection system to measure the brachial artery diameter [31]. A blood pressure cuff was placed around the forearm of each subject. The brachial artery was scanned longitudinally 5–10 cm above the elbow. When the clearest B-mode image of the anterior and posterior intimal interfaces between the lumen and vessel wall was obtained, the transducer was held at the same point throughout the scan by using a special probe holder (UNEX Co.) to ensure consistent imaging. Depth and gain settings were set to optimize the images of the arterial lumen wall interface. When the tracking gate was placed on the intima, the artery diameter was automatically tracked, and the waveform of the diameter changes over the cardiac cycle was displayed in real-time using the FMD mode of the tracking system. This allowed the ultrasound images to be optimized at the start of the scan and the transducer position to be adjusted immediately for optimal tracking performance throughout the scan. Pulsed Doppler flow was assessed at baseline and during peak hyperemic flow, which was confirmed to occur within 15 s after cuff deflation. Blood flow velocity was calculated from the color Doppler data and was displayed as a waveform in real-time. Baseline longitudinal images of the artery were acquired for 30 s, and then the blood pressure cuff was inflated to 50 mm Hg above systolic pressure for 5 min. The longitudinal image of the artery was recorded continuously until 5 min after cuff deflation. Pulsed Doppler velocity signals were obtained for 20 s at baseline and for 10 s immediately after cuff deflation. Changes in brachial artery diameter were immediately expressed as percentage changes relative to the vessel diameter before cuff inflation. FMD was automatically calculated as the percentage change in peak vessel diameter from the baseline value. The percentage FMD [(peak diameter−baseline diameter)/baseline diameter] was used for analysis. Blood flow volume was calculated by multiplying the Doppler flow velocity (corrected for the angle) by heart rate and vessel cross-sectional area (−r2). Reactive hyperemia was calculated as the maximum percentage increase in the flow after cuff deflation compared with the baseline flow.
The response to nitroglycerine was used for the assessment of endothelium-independent vasodilation [31]. After acquiring baseline rest images for 30 s, a sublingual tablet (nitroglycerine, 75 µg) was given, and imaging of the artery was done continuously for 5 min. NID was automatically calculated as the percentage change in peak vessel diameter from the baseline. The percentage NID [(peak diameter−baseline diameter)/baseline diameter] was used for analysis. The inter- and intra-assay coefficients of variation for the brachial artery diameter in our laboratory were 1.6% and 1.4%, respectively.
Statistical analysis
Results are presented as means ± SD. All reported probability values were two-sided, and a probability value of <0.05 was considered statistically significant. Categorical values were compared by means of the chi-square test. Continuous variables were compared by using ANOVA for multiple groups. Comparisons between the groups categorized according to stair climbing activity were carried out using repeated-measures ANOVA. Multivariate logistic regression analysis was performed to identify independent variables associated with lower tertiles of FMD (<1.4%) and NID (<7.9%). Age, sex, body mass index, current smoking, presence of dyslipidemia, presence of diabetes mellitus, the prevalence of CVD, total exercise time (h/week), and a total sitting time (h/week) were entered into the multivariate logistic regression analysis. As a sensitivity analysis, propensity score analysis was used to minimize the selection bias for the evaluation of the relationship between daily stair climbing activity and vascular function. The propensity score was calculated for each patient from the result of the logistic regression analysis of the probability of daily stair climbing for subjects who did not climb stairs, subjects who climbed stairs to the ≥2nd floor, subjects who climbed stairs to the <3rd floor, and subjects who climbed stairs to the ≥3rd floor using clinical variables, including age, sex, body mass index, systolic blood pressure, heart rate, total cholesterol, high-density lipoprotein cholesterol (HDL-C), fasting blood glucose, presence of diabetes mellitus (yes or no), current smoking (yes or no), taking lipid-lowering drugs (yes or no) and total exercise time (hours/week). All data were processed using JMP Pro. Ver 14.0 software (SAS Institute, Cary, NC, USA).
Results
Baseline characteristics of the subjects
The baseline characteristics of the 374 patients with hypertension are summarized in Table 1. The mean age of the subjects was 67 years. The 374 subjects included 234 men (62.6%). Some 252 (67.6%) had dyslipidemia, 101 (27.0%) had diabetes mellitus, 90 (24.4%) had previous cardiovascular disease, and 40 (10.1%) were current smokers. The mean exercise time was 1.9 ± 2.6 h/week, and the mean sitting time was 48 ± 22 h/week. The mean FMD value was 2.8 ± 2.6%, and the mean NID value was 10.4 ± 5.2%.
Vascular function in three groups of daily stair climbing activity
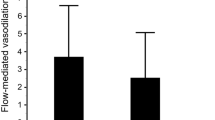
The baseline characteristics of the patients with hypertension who did not climb stairs, who climbed stairs to the second floor, and who climbed stairs to the ≥3rd floor are also summarized in Table 1. There were significant differences between the three groups in age, body mass index, heart rate, systolic blood pressure, diastolic blood pressure, triglycerides (TG), HDL-C, low-density lipoprotein cholesterol (LDL-C), creatinine, exercise time, the prevalence of CVD, use of lipid-lowering drugs, and use of antidiabetic drugs. The baseline brachial diameters were 4.5 ± 0.7 mm in the no stairs group, 4.1 ± 0.7 mm in the second-floor group, and 4.2 ± 0.6 mm in the ≥3rd-floor group. The baseline brachial diameter was larger in the no stairs group than in the second-floor group (p < 0.001) and in the ≥3rd-floor group (p = 0.004). The baseline brachial diameters were similar in the second-floor group and ≥3rd-floor group (p = 0.14). FMD values were 2.3 ± 2.7% in the no stairs group, 2.4 ± 2.7% in the 2nd floor group and 3.3 ± 2.5% in the ≥3rd-floor group (p = 0.005) (Fig. 1A). NID values were 7.4 ± 4.2% in the no stairs group, 10.9 ± 5.3% in the ≥2nd-floor group, and 11.3 ± 5.1% in the ≥3rd-floor group (p < 0.001) (Fig. 1B). Both FMD and NID were significantly smaller in the no stairs group than in the ≥3rd-floor group. FMD, but not NID, was significantly smaller in the no stairs group than in the ≥2nd-floor group.
Multivariate analysis of the relationships among low tertile of FMD, low tertile of NID, stair climbing activity, and clinical variables
The lowest tertile of FMD was 1.4% and the lowest tertile of NID was 7.9%. Therefore, we defined small FMD as FMD < 1.4% and small NID as NID < 7.9%. The group of subjects who did not climb stairs was used as a reference group for deriving the low tertiles of FMD and NID in the other groups. We next examined whether stair climbing activity was independently associated with small FMD and small NID by multiple logistic analysis. After adjustments for age, sex, body mass index, presence of dyslipidemia, presence of diabetes mellitus, the prevalence of CVD, current smoking, sitting time/week, and exercise time/week, the odds of having the lowest tertile of FMD were significantly lower in the ≥3rd-floor group than in the reference group (OR: 0.44, 95% CI: 0.23–0.75, p = 0.01), while the odds of having the lowest tertile of FMD were similar in the second-floor group and the reference group (OR: 1.06, 95% CI: 0.56–2.01, p = 0.86) (Table 2). After adjustments for age, sex, body mass index, presence of dyslipidemia, presence of diabetes mellitus, the prevalence of CVD, current smoking, sitting time/week, and exercise time/week, the odds of having the lowest tertile of NID were significantly lower in the second-floor group and ≥3rd-floor group than in the reference group (OR: 0.28, 95% CI: 0.13–0.57, p < 0.001, OR: 0.42, 95% CI: 0.21–0.81, p = 0.01, respectively) (Table 3).
Vascular function in the no stairs group and the ≥2nd-floor group
The baseline characteristics of the subjects in the no stairs group and the ≥2nd-floor group are summarized in Supplementary Table 1. There were significant differences between the two groups in age, heart rate, systolic blood pressure, total cholesterol, HDL-C, LDL-C, creatinine, exercise time, presence of diabetes mellitus, and use of lipid-lowering drugs. FMD was 2.3 ± 2.7% in the no stairs group and 2.7 ± 2.6% in the ≥2nd-floor group (p = 0.06) (Supplementary Fig. 1A). NID was 7.4 ± 4.2% in the no stairs group and 11.1 ± 5.2% in the ≥2nd-floor group (p < 0.001) (Supplementary Fig. 1B).
Propensity score matching was used to create matched pairs between the no stairs group and the ≥2nd-floor group. The baseline characteristics of the matched pairs are summarized in Supplementary Table 2. There were no significant differences in FMD between the two groups (2.4 ± 3.6% vs. 2.9 ± 2.6%, p = 0.56), while NID was significantly smaller in the no stairs group than in the ≥2nd-floor group (7.2 ± 4.2% vs. 10.3 ± 5.8%, p = 0.02) (Supplementary Fig. 2).
Vascular function in the < 3rd-floor group and ≥3rd-floor group
The baseline characteristics of subjects in the < 3rd-floor group and ≥3rd-floor group are summarized in Supplementary Table 3. There were significant differences between the two groups in age, diastolic blood pressure, total cholesterol, TG, LDL-C, exercise time and prevalence of CVD, use of lipid-lowering drugs, and use of antidiabetic drugs. The FMD value was significantly smaller in the < 3rd-floor group than in the ≥3rd-floor group (2.4 ± 2.7% vs. 3.3 ± 2.5%, p = 0.001) (Supplementary Fig. 3A). The NID value was significantly smaller in the <3rd floor group than in the ≥3rd floor group (9.4 ± 5.2% vs. 11.3 ± 5.1%, p < 0.001) (Supplementary Fig. 3B).
Propensity score matching was used to create matched pairs between the <3rd floor group and the ≥3rd floor group. The baseline characteristics of the matched pairs are summarized in Supplementary Table 4. FMD was significantly smaller in the <3rd floor group than in the ≥3rd floor group (2.0 ± 3.0% vs. 3.6 ± 2.8%, p = 0.005), while there were no significant differences in NID between the two groups (10.0 ± 4.7% vs. 10.5 ± 5.1%, p = 0.53).
Discussion
In patients with hypertension, this study showed for the first time that endothelial function was impaired in patients who regularly climbed stairs to the <3rd floor compared with that in patients who regularly climbed stairs to the ≥3rd floor and that vascular smooth muscle function was impaired in patients who did not climb stairs compared with that in patients who climbed stairs to the ≥2nd floor.
Although NID measurement is considered to be a control test for FMD measurement, recent studies have shown that NID is also smaller in patients with past CVD and in patients with a high risk of CVD, while FMD but not NID is smaller in patients with a low risk of CVD, and both NID and FMD are predictors of cardiovascular events. These findings suggest that FMD is a marker of the early stage of atherosclerosis and that NID is a marker of the advanced stage of atherosclerosis [31]. First, we divided the subjects into three groups in accordance with daily stair climbing activity and assessed vascular function in each group. Both FMD and NID were smaller in patients with hypertension who did not climb stairs than in patients who climbed stairs to the ≥3rd floor. FMD but not NID was smaller in patients who climbed stairs to the second floor than in patients who climbed stairs to the ≥3rd floor. After adjustment for cardiovascular risk factors using propensity score matching, FMD was significantly smaller in the <3rd floor group than in the ≥3rd floor group, and NID was significantly smaller in the no stairs group than in the ≥2nd-floor group. Patients with hypertension who did not climb stairs might have had an advanced stage of atherosclerosis compared with patients with hypertension who usually climbed stairs.
Stair climbing activity could have beneficial effects on vascular function through various mechanisms. Previous studies showed beneficial effects of physical exercise on cardiovascular risk factors such as body weight reduction, decreases in blood pressure, levels of serum blood glucose, LDL-C, and TG, and an increase in the level of HDL-C [32,33,34,35,36]. Indeed, a stair-climbing intervention trial also showed a 7.7% decrease in the level of LDL-C [37]. In this study, after adjustment for cardiovascular risk factors using propensity score matching, FMD was significantly smaller in the <3rd floor group than in the ≥3rd floor group, and NID was significantly smaller in the no stairs group than in the ≥2nd-floor group. These findings suggest that daily stair climbing activity is an independent predictor of vascular function. It is well known that physical exercise has beneficial effects on NO bioavailability. Exercise upregulates the endothelial nitric oxide (NO) synthase (e-NOS) gene through activation of the hypoxia-inducible factor 1 alpha/vascular endothelial growth factor (VEGF) pathway, leading to an increase in NO production [38]. In addition, physical exercise increases the synthesis of L-arginine, a substrate of NO synthase, and reduces the synthesis of asymmetric dimethylarginine (ADMA), an inhibitor of eNOS, resulting in an increase in NO production [39]. It has been reported that exercise inhibits the activity of nicotinamide adenine dinucleotide/nicotinamide adenine dinucleotide phosphate (NADH/NADPH oxidase) [40] and augments the activity of components of the antioxidant system, such as glutathione peroxidase (GPx) [41] and superoxide dismutase (SOD), leading to a decrease in NO inactivation. Interestingly, patients with hypertension have lower levels of L-arginine, SOD, and GPx and higher levels of ADMA, and higher activity of NADPH oxidase than healthy subjects [42,43,44]. Thus, an increase in stair climbing activity may have beneficial effects on vascular function in patients with hypertension through an increase in NO bioavailability.
Interestingly, in the present study, the baseline brachial artery diameter was larger in the no stairs group than in the stair climbing groups. Previous studies, including ours, have shown that brachial artery diameter significantly correlates with cardiovascular risk factors and that an increase in brachial artery diameter increases the prevalence of the cardiovascular disease [45,46,47]. It is thought that blood flow is increased to keep shear stress in an appropriate range, leading to activation of various signaling pathways and resulting in the enlargement of the brachial artery diameter [48, 49]. Although the precise mechanisms by which the diameter of the brachial artery became larger in the no stairs group than in the stair climbing groups are not known, advanced atherosclerosis may have contributed to maladaptive remodeling of the brachial artery in the no stairs group.
This study has some potential limitations. First, it was a single-center, cross-sectional study, so we could not establish a definitive causal relationship between daily stair climbing activity and vascular function. However, the findings indicate the possibility of an association between daily stair climbing activity and vascular function. Second, we cannot deny the possibility that patients with hypertension who have a high level of daily stair climbing activity are focused on being healthy. In the present study, daily stair climbing activity was significantly correlated with exercise time (hours/week). Therefore, to minimize the influence of exercise time on vascular function, we matched exercise time between the two groups by propensity score matching. Third, unfortunately, although there are a number of different ways to assess daily physical activity data, there is no gold standard method for defining daily physical activity based on a self-report survey. The IPAQ is often used to define daily physical activity. In the present study, information on physical activity was obtained by using the self-reported modified IPAQ. It is not clear whether the assessment of stair climbing activity reflects different facets of physical activity than those captured by other questionnaires. However, the levels of daily physical activity based on the questionnaire of stair climbing activity should be simple and useful for the assessment of vascular function. Indeed, in the present study, the assessment of stair climbing activity may reflect vascular function in patients with hypertension. In the IPAQ, we defined habitual exercise as that lasting for more than 10 min and with an intensity of more than three METs. We cannot deny the possibility that the self-reported IPAQ is not sufficient for assessing daily physical activity. Assessment of more detailed daily physical activity would enable us to draw more specific conclusions concerning the role of stair climbing activity in vascular function. Fourth, this study was conducted in patients with hypertension. Further study is needed to confirm the association of daily stair climbing activity with vascular function in a larger population of subjects without hypertension. Finally, we did not have information on the frequency of stair climbing. Previous studies that focused on stair climbing (floors/week) revealed that subjects who climbed ≥35 floors/week had a lower risk of all-cause mortality than subjects who climbed <10 floors/week [50]. Assessment of the frequency of stair climbing would enable us to draw more specific conclusions concerning the role of stair climbing activity in vascular function.
In conclusion, stair climbing activity, a simple method for assessing daily physical activity, may reflect vascular function in patients with hypertension.
References
Jeong SW, Kim SH, Kang SH, Kim HJ, Yoon CH, Youn TJ, et al. Mortality reduction with physical activity in patients with and without cardiovascular disease. Eur Heart J. 2019;40:3547–55.
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451–62.
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation. 2019;140:e596–e646.
Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380:247–57.
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;74:1376–414.
Teh KC, Aziz AR. Heart rate, oxygen uptake, and energy cost of ascending and descending the stairs. Med Sci Sports Exerc. 2002;34:695–9.
Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR Jr, Tudor-Locke C, et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–81.
Morris JN, Heady JA, Raffle PA, Roberts CG, Parks JW. Coronary heart-disease and physical activity of work. Lancet (Lond, Engl). 1953;262:1111–20.
Ninomiya T, Ohara T, Hirakawa Y, Yoshida D, Doi Y, Hata J, et al. Midlife and late-life blood pressure and dementia in Japanese elderly: the Hisayama study. Hypertension. 2011;58:22–28.
Hozawa A, Okamura T, Murakami Y, Kadowaki T, Okuda N, Takashima N, et al. High blood pressure in middle age is associated with a future decline in activities of daily living. NIPPON DATA80. J Hum Hypertens. 2009;23:546–52.
Tozawa M, Iseki K, Iseki C, Kinjo K, Ikemiya Y, Takishita S. Blood pressure predicts risk of developing end-stage renal disease in men and women. Hypertension. 2003;41:1341–5.
Klag MJ, Whelton PK, Randall BL, Neaton JD, Brancati FL, Ford CE, et al. Blood pressure and end-stage renal disease in men. N Engl J Med. 1996;334:13–18.
Collins R, Peto R, MacMahon S, Hebert P, Fiebach NH, Eberlein KA, et al. Blood pressure, stroke, and coronary heart disease. Part 2, short-term reductions in blood pressure: overview of randomised drug trials in their epidemiological context. Lancet. 1990;335:827–38.
Levy D, Larson MG, Vasan RS, Kannel WB, Ho KK. The progression from hypertension to congestive heart failure. Jama 1996;275:1557–62.
Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens. 2006;24:215–33.
Roque FR, Briones AM, García-Redondo AB, Galán M, Martínez-Revelles S, Avendaño MS, et al. Aerobic exercise reduces oxidative stress and improves vascular changes of small mesenteric and coronary arteries in hypertension. Br J Pharm. 2013;168:686–703.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
2018 ESC/ESH. Guidelines for the management of arterial hypertension. Rev Esp Cardiol. 2019;72:160.
Ross R. Atherosclerosis–an inflammatory disease. N Engl J Med. 1999;340:115–26.
Maruhashi T, Soga J, Fujimura N, Idei N, Mikami S, Iwamoto Y, et al. Relationship between flow-mediated vasodilation and cardiovascular risk factors in a large community-based study. Heart. 2013;99:1837–42.
Higashi Y, Noma K, Yoshizumi M, Kihara Y. Endothelial function and oxidative stress in cardiovascular diseases. Circulation J. 2009;73:411–8.
Maruhashi T, Soga J, Fujimura N, Idei N, Mikami S, Iwamoto Y, et al. Endothelial dysfunction, increased arterial stiffness, and cardiovascular risk prediction in patients with coronary artery disease: FMD-J (flow-mediated dilation Japan) study A. J Am Heart Assoc. 2018;7:e008588.
Yeboah J, Folsom AR, Burke GL, Johnson C, Polak JF, Post W, et al. Predictive value of brachial flow-mediated dilation for incident cardiovascular events in a population-based study: the multi-ethnic study of atherosclerosis. Circulation. 2009;120:502–9.
Wolfrum S, Jensen KS, Liao JK. Endothelium-dependent effects of statins. Arterioscler Thromb Vasc Biol. 2003;23:729–36.
Sanada M, Higashi Y, Nakagawa K, Sasaki S, Kodama I, Tsuda M, et al. Relationship between the angiotensin-converting enzyme genotype and the forearm vasodilator response to estrogen replacement therapy in postmenopausal women. J Am Coll Cardiol. 2001;37:1529–35.
Goto C, Higashi Y, Kimura M, Noma K, Hara K, Nakagawa K, et al. Effect of different intensities of exercise on endothelium-dependent vasodilation in humans: role of endothelium-dependent nitric oxide and oxidative stress. Circulation. 2003;108:530–5.
Higashi Y, Sasaki S, Kurisu S, Yoshimizu A, Sasaki N, Matsuura H, et al. Regular aerobic exercise augments endothelium-dependent vascular relaxation in normotensive as well as hypertensive subjects: role of endothelium-derived nitric oxide. Circulation. 1999;100:1194–202.
Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP). Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). Jama 2001;285:2486–97.
American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S13–S28.
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9 Suppl):S498–504.
Maruhashi T, Soga J, Fujimura N, Idei N, Mikami S, Iwamoto Y, et al. Nitroglycerine-induced vasodilation for assessment of vascular function: a comparison with flow-mediated vasodilation. Arterioscler Thromb Vasc Biol. 2013;33:1401–8.
Fahlman MM, Boardley D, Lambert CP, Flynn MG. Effects of endurance training and resistance training on plasma lipoprotein profiles in elderly women. J Gerontol A Biol Sci Med Sci. 2002;57:B54–60.
Snowling NJ, Hopkins WG. Effects of different modes of exercise training on glucose control and risk factors for complications in type 2 diabetic patients: a meta-analysis. Diabetes Care. 2006;29:2518–27.
Kodama S, Tanaka S, Saito K, Shu M, Sone Y, Onitake F, et al. Effect of aerobic exercise training on serum levels of high-density lipoprotein cholesterol: a meta-analysis. Arch Intern Med. 2007;167:999–1008.
Wadden TA, Berkowitz RI, Womble LG, Sarwer DB, Phelan S, Cato RK, et al. Randomized trial of lifestyle modification and pharmacotherapy for obesity. N Engl J Med. 2005;353:2111–20.
Igarashi Y, Akazawa N, Maeda S. Effects of aerobic exercise alone on lipids in healthy east Asians: a systematic review and meta-analysis. J Atheroscler Thromb. 2019;26:488–503.
Boreham CA, Kennedy RA, Murphy MH, Tully M, Wallace WF, Young I. Training effects of short bouts of stair climbing on cardiorespiratory fitness, blood lipids, and homocysteine in sedentary young women. Br J Sports Med. 2005;39:590–3.
Vital TM, Stein AM, de Melo Coelho FG, Arantes FJ, Teodorov E, Santos-Galduróz RF. Physical exercise and vascular endothelial growth factor (VEGF) in elderly: a systematic review. Arch Gerontol Geriatr. 2014;59:234–9.
Riccioni G, Scotti L, Guagnano MT, Bosco G, Bucciarelli V, Di Ilio E, et al. Physical exercise reduces synthesis of ADMA, SDMA, and L-Arg. Front Biosci. 2015;7:417–22.
Zalba G, Beaumont FJ, San José G, Fortuño A, Fortuño MA, Etayo JC, et al. Vascular NADH/NADPH oxidase is involved in enhanced superoxide production in spontaneously hypertensive rats. Hypertension. 2000;35:1055–61.
Urso ML, Clarkson PM. Oxidative stress, exercise, and antioxidant supplementation. Toxicology. 2003;189:41–54.
Rodrigo R, Prat H, Passalacqua W, Araya J, Guichard C, Bächler JP. Relationship between oxidative stress and essential hypertension. Hypertens Res. 2007;30:1159–67.
Brandes RP. Vascular functions of NADPH oxidases. Hypertension. 2010;56:17–21.
Gamil S, Erdmann J, Schwedhelm E, Bakheit KH, Abdalrahman IBB, Mohamed AO. Increased serum levels of asymmetric dimethylarginine and symmetric dimethylarginine and decreased levels of arginine in Sudanese patients with essential hypertension. Kidney Blood Press Res. 2020;45:727–36.
Benjamin EJ, Larson MG, Keyes MJ, Mitchell GF, Vasan RS, Keaney JF Jr, et al. Clinical correlates and heritability of flow-mediated dilation in the community: the Framingham heart study. Circulation 2004;109:613–9.
Maruhashi T, Iwamoto Y, Kajikawa M, Oda N, Kishimoto S, Matsui S, et al. Interrelationships among flow-mediated vasodilation, nitroglycerine-induced vasodilation, baseline brachial artery diameter, hyperemic shear stress, and cardiovascular risk factors. J Am Heart Assoc. 2017;7:e006797.
Maruhashi T, Soga J, Fujimura N, Idei N, Mikami S, Iwamoto Y, et al. Brachial artery diameter as a marker for cardiovascular risk assessment: FMD-J study. Atherosclerosis. 2018;268:92–98.
Chung WB, Hamburg NM, Holbrook M, Shenouda SM, Dohadwala MM, Terry DF, et al. The brachial artery remodels to maintain local shear stress despite the presence of cardiovascular risk factors. Arterioscler Thromb Vasc Biol. 2009;29:606–12.
Korshunov VA, Schwartz SM, Berk BC. Vascular remodeling: hemodynamic and biochemical mechanisms underlying Glagov’s phenomenon. Arterioscler Thromb Vasc Biol. 2007;27:1722–8.
Rey-Lopez JP, Stamatakis E, Mackey M, Sesso HD, Lee IM. Associations of self-reported stair climbing with all-cause and cardiovascular mortality: the Harvard Alumni Health Study. Prev Med Rep. 2019;15:100938.
Acknowledgements
The authors would like to thank all of the patients who participated in this study. In addition, we thank Miki Kumiji, Megumi Wakisaka, Ki-ichiro Kawano, and Satoko Michiyama for their excellent secretarial assistance.
Funding
Grant-in-Aid for Scientific Research from the Ministry of Education, Science and Culture of Japan (18590815 and 21590898 to Y. Higashi).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Yamaji, T., Harada, T., Hashimoto, Y. et al. Stair climbing activity and vascular function in patients with hypertension. Hypertens Res 44, 1274–1282 (2021). https://doi.org/10.1038/s41440-021-00697-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-021-00697-z
- Springer Nature Singapore Pte Ltd.
Keywords
This article is cited by
-
Current topic of vascular function in hypertension
Hypertension Research (2023)
-
Cardiovascular risk in patients receiving antihypertensive drug treatment from the perspective of endothelial function
Hypertension Research (2022)
-
Update on Hypertension Research in 2021
Hypertension Research (2022)
-
Self-reported total sitting time on a non-working day is associated with blunted flow-mediated vasodilation and blunted nitroglycerine-induced vasodilation
Scientific Reports (2022)
-
Routine stair climbing for vascular health
Hypertension Research (2021)