Abstract
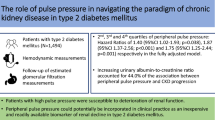
The progression of chronic kidney disease (CKD) inverts the arterial stiffness gradient. However, central hemodynamic pressure profiles in CKD have not been fully examined. A cross-sectional study was performed to assess the relationship between the CKD stage and central hemodynamic processes. The study enrolled 2020 hypertensive patients who had undergone echocardiography and measurement of their serum creatinine levels. Radial tonometry was applied to all patients to measure central blood pressure. Patients were classified according to six CKD stages based on their estimated glomerular filtration rate. Central (PP2) and brachial pulse pressure (PP) were elevated at stages 3a and 3b, respectively. Diastolic blood pressure (DBP) was higher at stage 1 compared to the other stages. The left ventricular mass index was greater at CKD stages 3b–5 than that at stage 1. Either PP or PP2 was sensitive for detecting the presence of left ventricular hypertrophy (LVH). Age, weight, pulse rate, brachial blood pressure, and antihypertensive medication differed among the six stages. Pulse amplification (PA) adjusted for these confounders was the lowest in CKD stages 3a and 3b. The present observations support that cardiovascular risk is higher in CKD stages 3b and later. Our findings indicate that PA is inverted in CKD stages 4 and 5. The present results suggest that aortic stiffening and the subsequent elevation in PA during CKD progression relate to a reduction in the ability of PP2 to predict LVH.
Similar content being viewed by others
Introduction
Central hemodynamic processes play a crucial role in aging and hypertension. The age-related increment of peripheral arterial stiffness compared to aortic stiffness is related to an increase in the reflection wave and pulse pressure (PP) without a reversal of the arterial stiffness gradient [1]. An increased reflection wave mainly accounts for the elevated PP in systolic hypertension. A previous meta-analysis demonstrated that an augmentation index predicts cardiovascular (CV) outcomes [2]. In addition, central PP (PP2) predicted CV events more strongly than brachial PP [3]. The Anglo-Scandinavian Cardiac Outcomes Trial Conduit Artery Function Evaluation study indicated that antihypertensive medications that preferentially reduce central systolic blood pressure (SBP) rather than peripheral SBP resulted in favorable CV outcomes in hypertensive patients [4]. Our previous data indicated that compared to non-vasodilator antihypertensive medications (NVD), vasodilator antihypertensive agents (VD) preferentially reduced central SBP rather than peripheral SBP [5]. Thus, there is an emerging consensus that the definition of central hemodynamic terms should be introduced in the guidelines for hypertension and CV risk [6].
However, the Framingham Heart Study (FHS) provided diverse results. An age-related increase in aortic stiffness compared with peripheral arterial stiffness was associated not only with increases in the forwarding wave amplitude and PP but also with a reversal in the arterial stiffness gradient [7], thereby suggesting that aortic stiffness overcomes peripheral arterial stiffness in aging. An elevated PP was primarily attributable to a reduced effective diameter of the proximal aorta and elevated characteristic impedance during systolic hypertension [8]. Thus, the augmentation index, PP2, and PP amplification were not related to CV events in the FHS [9]. In addition, reduced aortic diameter and aortic wall stiffness were shown to account for sex differences in PP in the elderly population [10]. Furthermore, in the FHS, aortic stiffness, central forwarding wave amplitude, and wave reflection were associated with future SBP, PP, and incident hypertension [11], which supports that aortic stiffness is a precursor to, rather than the result of, hypertension.
These discrepant findings lead to the possibility that some factors that were not appreciated in previous studies simultaneously confound central hemodynamic measurements and contribute to CV outcomes. Chronic kidney disease (CKD) is recognized as a strong CV risk factor [12]. Indeed, an independent graded association was observed between a reduced estimated glomerular filtration rate (eGFR) and the risk of death, CV events, and hospitalization in a large community-based population [13]. CKD patients are exposed to non-traditional as well as to Framingham (traditional) CV risk factors [14]. Of importance, London et al. demonstrated that aortic aging differs between non-CKD and CKD patients [15]. Although the diameter of the ascending aorta remained constant during aging in CKD patients, it increased over time in the population without CKD. It is known that the arterial stiffness gradient is inverted in CKD progression. However, central hemodynamic pressure profiles in CKD have not been fully examined. Here, we present a cross-sectional analysis that assessed whether CKD is associated with abnormal central hemodynamics, including pulse amplification (PA), among patients with hypertension as a common and underappreciated pre-existing medical cause.
Methods
Initially, we enrolled Japanese hypertensive patients who had visited our offices and were stable on antihypertensive medications for at least 3 months. Seven major centers and their related facilities comprised the participating clinics for the Antihypertensives and Blood pressure of Central artery study in Japan (ABC-J study) [5, 16]. Then, the number of enrolled patients was increased with the aid of cooperative doctors (Appendix) to ensure statistical power (ABC-J II). A main objective of the ABC-J II study was to assess CV outcomes [17]. The study was approved by our local ethical committee and complied with the Declaration of Helsinki (registered at UMIN 000002966). Patient enrollment began in 2010 using the following inclusion criteria: age >35 years as well as a diagnosis of hypertension that was treated with stable antihypertensive therapy. Patients with valvular heart disease, severe arrhythmia, or on dialysis were excluded from the study. In addition, if the attending physicians believed that the patients were unsuited for this study, they were not enrolled. In 2011, patient enrollment was closed, and the baseline data were fixed. In 2013, the observations were completed. However, the data from the follow-up study have not yet been published [17]. Therefore, we used the baseline data for this cross-sectional analysis.
For all patients, brachial SBP and diastolic blood pressure (DBP) were measured using oscillometric methods (HEM-9000AI, Omron Healthcare, Kyoto, Japan) in a sitting position after at least a 5-min rest [18]. Radial tonometry was automatically performed to obtain the pulse waveform by applying multiple tonometers on the wrist and assessing the second peak of SBP (SBP2) on the same occasion as the BP measurement. The algorithm of HEM9000AI was used to determine SBP2 by calculating the second maximum of the fourth derivative of the radial waveform [19]. The calibration of the waveform was performed with the SBP and DBP as the peak and bottom of the radial pressure waveform, respectively. Using the data from ABC-J and the other studies, Herbert et al. demonstrated that SBP2 measured using HEM-9000AI was almost identical to central SBP, which was estimated using the SphygmoCor system [20]. Brachial PP and PP2 were determined as SBP—DBP and SBP2—DBP, respectively. The difference in DBP between central and brachial arteries is negligible [18]. Thus, PA was defined as PP/PP2.
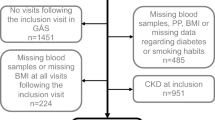
A full medical history was obtained. According to our previous report on central hemodynamics, antihypertensive medication was categorized into VD and NVD [5]. While VD comprises angiotensin receptor blockers, angiotensin converting enzyme inhibitors, calcium channel blockers, and alpha-adrenergic blockers, NVD consisted of beta-adrenergic blockers and diuretics. Diabetes (DM) was diagnosed when patients exhibited a hemoglobin A1c level ≥6.5%, fasting blood glucose level ≥126 mg/dl, postprandial blood glucose level ≥200 mg/dl, and results from an oral 75-g glucose tolerance test that indicated hyperglycemia. Patients taking glucose-lowering drugs and/or insulin were also considered to have DM. Dyslipidemia (HL) was diagnosed when fasting high-density lipoprotein cholesterol was lower than 40 mg/dl, or triglyceride and low-density lipoprotein cholesterol exceeded 150 and 140 mg/dl, respectively [20]. Patients who took lipid-lowering drugs were also considered as having HL. Left ventricular mass index (LVMI) or left ventricular hypertrophy (LVH) was considered an intermediate phenotype of CV risk [21, 22]. Among baseline data of the ABC-J II study, 2020 patients were selected because their serum creatinine level was measured, and they underwent echocardiography. Using the MDRD equation for the Japanese population, the eGFR (ml/min/1.73 m2) was calculated, and patients were divided into six groups according to a revised CKD classification [23].
Laboratory data, including echocardiography findings, such as left ventricular end-diastolic diameter (LVEDd), posterior wall thickness (PWT), and interventricular septal thickness (IVST), were obtained from medical records and used for analysis when they were measured on the same day or within 3 months of radial tonometry. Body surface area was assessed from body weight and height. LVMI was calculated using the following equation: [24]
Data were expressed as the mean ± SD. Statistical analyses were performed using analysis of variance (ANOVA) followed by Dunnett’s test (CKD stage 1 was used as the reference value), the χ2 test with Yates’s correction, and regression analyses and receiver operation curve (ROC) analyses, whenever appropriate; SPSS version 21 (IBM, New York, NY, USA) was used for data analysis. To perform ROC analysis, continuous variables were converted into nominal ones. LVH was determined when LVMI was greater than 115 and 95 g/m2 in male and female patients, respectively [25]. Written informed consent was not obtained from participants due to the observational nature of this study. Statistical significance was assumed when p < 0.05.
Results
Table 1 summarizes the baseline characteristics of enrolled patients. For clarity, only the means were reported. Regarding age, weight, antihypertensive medications, and hemodynamic profiles, there were differences across the six groups (p < 0.001 for all by ANOVA). The patients at CKD stages 2–4 were older than those at stage 1 (p < 0.05). The body weight of patients at CKD stages 4–5 were less than that of patients at stage 1 (p < 0.01). Compared to stage 1, more VD and NVD anti-hypertensive medications were prescribed for CKD stages 3b–5 and stages 3a–5 patients (p < 0.05 for each), respectively. SBP at stage 1 was higher than that at stages 3a–4, and DBP at stage 1 was higher than that at stages 2–5. The second peak of SBP and PA were similar among all CKD stages according to ANOVA results. Accordingly, the blood pressure of patients enrolled in this study was well controlled throughout all CKD stages. Although PP2 at stages 3a–5 was higher than that at stage 1, PP at stage 3b and later was higher than that at stage 1. Thus, PP2 was significantly elevated in the earlier stages of CKD than PP. Pulse rate (PR) was lower at CKD stages 2–4 than at stage 1.
There were differences in patient clinical characteristics, such as age, weight, antihypertensive use, pulse rate, and blood pressure, across the six groups. Because these factors may alter PA, they were adjusted to compare PA. To decrease multicollinearity, SBP was used as a variable for blood pressure. Multiple regression analysis for PA was performed (Table S1), which may have decreased insignificant variables for adjustments, thereby keeping the analyses conservative. Accordingly, PA was adjusted utilizing beta coefficients for weight, SBP, PR, and VD antihypertensive use. Surprisingly, compared to CKD stage 1 (Fig. 1a), the adjusted PA at CKD stages 3a and 3b was lower (p < 0.05 for each). However, the adjusted PA at CKD stage 1 was similar to that at CKD stages 4 and 5. Similar trends were seen when PA was adjusted for all variables shown in Table S1 (Fig. 1b). Thus, CKD progression inverted PA.
From the echocardiography data, the ABC-J II study mined PWT, IVST, and LVEDd to assess the stress experienced by the heart. As shown in Fig. 2, PWT and IVST at CKD stage 1 were smaller than those at stages 3b–5 (p < 0.05 for all). Only at stage 5 was LVEDd greater than that at stage 1 (p < 0.01), thereby supporting that fluid status was maintained until CKD progressed to stage 4. In contrast to CKD stages 2–4, PR at CKD stage 5 was similar to that at CKD stage 1. Compared to stage 1, LVMI increased for CKD stages 3b–5 (p < 0.05 for all). To detect factors contributing to LVMI, simple regression was performed. As described in Table 2, many variables in the patients’ backgrounds exhibited significant correlations. To render statistics more conservative, any independent variables possessing r > 0.1 were selected. They included sex, eGFR, SBP, PP, VD, NVD, SBP2, and PP2. Then, these variables were used as independent variables for multiple regression. The analyses demonstrated that LVMI was strongly related to sex (male) and eGFR, rather than hemodynamic factors (Table 2). To ascertain the above analyses, stepwise regression was performed for all independent variables used for simple regression analyses. Again, eGFR was selected as a single significant contributor for LVMI (R = 0.39, F = 34, df (16,2003), β = −0.49, t = −12, p < 0.0001). Although it is difficult to determine directionality using a cross-sectional study, our data provided evidence that incremental changes in LVMI are associated with the progression to CKD stage 3b.
The left ventricular mass index (LVMI) and CKD stages are shown. Both posterior wall thickness (a: PWT) and interventricular septal thickness (b: IVST) at CKD stages 3b–5 were greater than those at stage 1. The left ventricular end-diastolic diameter (c: LVDd) at CKD stage 5 was larger than that at stage 1. The LVMI (d) at CKD stages 3b–5 was greater than that at stage 1. Asterisk depicts a significant difference from stage 1
ROC analysis was performed to detect significant predictors of LVH in treated hypertension. In the enrolled 2020 patients, 1136 showed LVH (56%). Among the independent variables, PP (AUC: 0.592 ± 0.014, p < 0.01) and PP2 (AUC: 0.597 ± 0.014, p < 0.01) exhibited the strongest prognostic ability (Table 3). The cut-off value for PP to detect LVH was 60 mmHg (sensitivity: 54%; selectivity: 60%), and that for PP2 was 46 mmHg (sensitivity: 59%; selectivity: 55%) (Fig. 3).
Discussion
Physiologically, elastic arteries temporally store approximately 50% of the stroke volume during the systolic period before subsequent flow to the periphery in the diastolic phase [1]. The latter maintains diastolic blood flow and pressure to sufficiently perfuse the coronary arteries. The high compliance of elastic arteries, such as the thoracic aorta, facilitates both the Windkessel effect and transmission, as well as slows the pulse wave velocity (PWV). This results in the late arrival of the reflection wave at the ascending aorta in very late systole or even diastole, thereby reducing the summative effects of reflection and forwarding waves on central SBP. The left ventricle is exposed to central SBP. As a mechanical stress, the central SBP is a driving force for remodeling of the left ventricle and large arteries, such as the ascending aorta and carotid arteries. The FHS indicated that LVH is a strong risk factor for coronary heart disease, heart failure, and CV death [22]. Our results indicated that LVMI at CKD stages 3b–5 was elevated, compared to that at CKD stage 1. This is consistent with the observation that CV mortality is higher in patients at CKD stages 3b and later if, indeed, LVH is a strong risk factor for CV illness [21, 22]. Hypertensive patients at CKD stages 3b–5 were commonly characterized as having a high PP and PP2 as well as using three or more antihypertensive medications, which supports the notion that CKD hides behind resistant hypertension as a common and underappreciated pre-existing medical cause in treated hypertension.
Advanced CKD (stages 4–5) appears to be a typical clinical example of arterial impedance mismatch (Fig. S1). Investigators described the relations between arterial stiffness and CKD [26, 27]. Briet et al. reported that, although carotid stiffness is similar between CKD and hypertensive patients, aortic stiffness in CKD patients is higher than that in hypertensive patients without CKD [28]. Marked reductions in aortic compliance could account for both high PA and diastolic hypotension in advanced CKD. Therefore, ventricular–vascular coupling is disrupted [29], which is consistent with high CV mortality in this population. Our data suggest that advanced CKD is related to both LVH and elevated PA through afterload mismatch [1, 30]. The stiffness gradient disappears or inverts in CKD progression [20]. Thus, proximal aortic stiffening inadequately reduces PP in CKD, which accounts for a high prevalence of microvascular as well as macrovascular diseases of the brain and kidney in this patient population [31]. The forwarding wave pressure increases as aortic compliance is progressively diminished in the patients with advanced CKD. Thus, the relative contribution of reflection pressure to central SBP may shrink, thereby increasing PA in CKD stages 4–5. Accordingly, to our knowledge, the present data constitute the novel demonstration that PA is elevated in advanced CKD patients.
Various clinical studies have reported that the left ventricular mass (LVM) showed a better correlation to PP2 than to PP [21]. Indeed, the present data depicted that although PP at CKD stage 3b was higher than that at CKD stage 1, PP2 at CKD stage 3a was already greater than that at CKD stage 1. Furthermore, our data suggest that PP2 is an early marker for a decrease in arterial compliance rather than for PP in treated hypertension. These observations support the notion that arterial compliance is diminished at CKD stage 3 and later, even in well-treated hypertension. However, our data showed that PP2 and PP similarly predicted LVH in treated hypertension. Although the reasons for this discrepancy are not readily apparent, it may possibly be due to differing patient profiles. Indeed, high-risk patients were enrolled in the present study, as over 50% of patients possessed LVH. In addition, CKD patients are exposed to non-traditional, as well as Framingham (traditional), CV risk factors. Non-classical CV risk factors, such as calcium phosphate abnormalities, are common in advanced CKD and possibly underlie aortic remodeling [15]. Collectively, these results indicate that although BP control is important for LVM regression [32], aortic compliance progressively decreases despite feasible BP control once kidney dysfunction develops (Table 1). Additionally, the results suggest that aortic stiffening and the subsequent elevation in PA during CKD progression relate to a reduction in the ability of PP2 to predict LVH.
The study has limitations. First, we did not take digital records of radial pulse wave forms from all enrolled patients. Thus, waveform analysis using differing algorithms was not available. Second, only echocardiographic data for diastole were taken from patient medical records in the mother ABC-J II study, as LVH was the focus [22]. Although systolic function data such as ejection fraction may affect central hemodynamics, they were not available in this analysis. However, all patients were stable hypertensive patients without congestive symptoms [24]. Third, a cross-sectional study is not suitable for assessing causal relationships. Cohort studies similar to the FHS, which did not appreciate kidney function, may confound the interpretation of data, partly due to the inseparable and complex features of aging and CKD, which progress simultaneously. Fourth, although the study was a multicenter study, all enrolled patients were Japanese who were shorter in height, thereby potentially biasing patient selection [8]. Fifth, Wassertheuer et al. reported that PA was reduced in advanced CKD [33]. However, they compared unadjusted PA among 128 enrolled patients. Finally, PWV data were not available in this study. Although carotid-femoral PWV is supposed to be the gold standard of the aortic stiffness index, it does not consider ascending aortic stiffness or even aortic arch stiffness. The traveling time of the pulse wave from the heart to the carotid arteries may exceed that from the heart to the aortic arch.
In summary, the present observations indicate that LVMI is increased in CKD stages 3b–5. Furthermore, our results are consistent with the reversal of the arterial stiffness gradient in advanced CKD and provide the first evidence for abnormalities in the central hemodynamic pressure profile among these patients. Of importance, aortic stiffening in advanced CKD inadequately reduces PP, further deteriorating microvascular as well as macrovascular beds in the brain and kidney. Taken together, these findings suggest that CKD stage 3b (i.e., eGFR) as well as PP or PP2 come of age as an index for timely CV screening and interventions.
References
Nichols Wilmer W, O’Rourke Michael F, Vlachopoulos Charalambos, editors. McDonald’s blood flow in arteries, sixth edition: theoretical, experimental and clinical principles. Boca Raton, FL: CRC Press; 2011.
Vlachopoulos C, Aznaouridis K, O’Rourke MF, Safar ME, Baou K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J. 2010;31:1865–71.
Roman MJ, Devereux RB, Kizer JR, Lee ET, Galloway JM, Ali T, Umans JG, Howard BV. Central pressure more strongly relates to vascular disease and outcome than does brachial pressure: the Strong Heart study. Hypertension. 2007;50:197–203.
Williams B, Lacy PS, Thom SM, Cruickshank K, Stanton A, Collier D, Hughes AD, Thurston H, O’Rourke M, CAFE Investigators; Anglo-Scandinavian Cardiac Outcomes Trial Investigators; CAFE Steering Committee and Writing Committee. Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation. 2006;113:1213–25.
Miyashita H, Aizawa A, Hashimoto J, Hirooka Y, Imai Y, Kawano Y, Kohara K, Sunagawa K, Suzuki H, Tabara Y, Takazawa K, Takenaka T, Yasuda H, Shimada K. Cross-sectional characterization of all classes of antihypertensives in terms of central blood pressure in Japanese hypertensive patients. Am J Hypertens. 2010;23:260–8.
Agabiti-Rosei E, Mancia G, O’Rourke MF, Roman MJ, Safar ME, Smulyan H, Wang JG, Wilkinson IB, Williams B, Vlachopoulos C. Central blood pressure measurements and antihypertensive therapy: a consensus document. Hypertension. 2007;50:154–60.
Mitchell GF, Parise H, Benjamin EJ, Larson MG, Keyes MJ, Vita JA, Vasan RS, Levy D. Changes in arterial stiffness and wave reflection with advancing age in healthy men and women: the Framingham Heart study. Hypertension. 2004;43:1239–45.
Mitchell GF, Lacourcière Y, Ouellet JP, Izzo JL Jr, Neutel J, Kerwin LJ, Block AJ, Pfeffer MA. Determinants of elevated pulse pressure in middle-aged and older subjects with uncomplicated systolic hypertension: the role of proximal aortic diameter and the aortic pressure-flow relationship. Circulation. 2003;108:1592–8.
Mitchell GF, Hwang SJ, Vasan RS, Larson MG, Pencina MJ, Hamburg NM, Vita JA, Levy D, Benjamin EJ. Arterial stiffness and cardiovascular events: the Framingham Heart study. Circulation. 2010;121:505–11.
Mitchell GF, Gudnason V, Launer LJ, Aspelund T, Harris TB. Hemodynamics of increased pulse pressure in older women in the community-based age, gene/environment susceptibility-Reykjavik study. Hypertension. 2008;51:1123–8.
Kaess BM, Rong J, Larson MG, Hamburg NM, Vita JA, Levy D, Benjamin EJ, Vasan RS, Mitchell GF. Aortic stiffness, blood pressure progression, and incident hypertension. J Am Med Assoc. 2012;308:875–81.
Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, McCullough PA, Kasiske BL, Kelepouris E, Klag MJ, Parfrey P, Pfeffer M, Raij L, Spinosa DJ, Wilson PW, American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on kidney in cardiovascular disease, high blood pressure research, clinical cardiology, and epidemiology and prevention. Circulation. 2003;108:2154–69.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–305.
Chen J, Mohler ER, Xie D, Shlipak M, Townsend RR, Appel LJ, Ojo A, Schreiber M, Nessel L, Zhang X, Raj D, Strauss L, Lora CM, Rahman M, Hamm LL, He J, CRIC Study Investigators. Traditional and non-traditional risk factors for incident peripheral arterial disease among patients with chronic kidney disease. Nephrol Dial Transplant. 2016;31:1145–51.
London GM, Safar ME, Pannier B. Aortic aging in ESRD: structural, hemodynamic, and mortality implications. J Am Soc Nephrol. 2016;27:1837–46.
Kanno Y, Takenaka T, Watanabe Y, Inoue T, Takane H, Ohno Y, Hayashi M, Suzuki H. Paradoxical distribution of augmentation index level in chronic kidney diseases. Nephrol Rev. 2012;4:e19 https://doi.org/10.4081/nr.2012.e19.
Eguchi K, Miyashita H, Takenaka T, Tabara Y, Tomiyama H, Dohi Y, Hoshimoto J, Ohkubo T, Kario K, Takazawa K, Yomashina A, Shimada K. Does central blood pressure predict cardiovascular prognosis in treated hypertensives? The ABC-J follow-up study. J Hypertens. 2016;34:e222–3.
Takenaka T, Kikuta T, Watanabe Y, Inoue T, Takane H, Ohno Y, Suzuki H. Validation of carotid blood pressure assessment by tonometry. J Hypertens. 2012;30:429–32.
Takazawa K, Kobayashi H, Shindo N, Tanaka N, Yamashina A. Relationship between radial and central arterial pulse wave and evaluation of central aortic pressure using the radial arterial pulse wave. Hypertens Res. 2007;30:219–28.
Herbert A, Cruickshank JK, Laurent S, Boutouyrie P, on behalf of The Reference Values for Arterial Measurements Collaboration; on behalf of The Reference Values for Arterial Measurements Collaboration. Establishing reference values for central blood pressure and its amplification in a general healthy population and according to cardiovascular risk factors. Eur Heart J. 2014;35:3122–33.
Roman MJ, Devereux RB. Association of central and peripheral blood pressures with intermediate cardiovascular phenotypes. Hypertension. 2014;63:1148–53.
Kannel WB, Cobb J. Left ventricular hypertrophy and mortality—results from the Framingham study. Cardiology. 1992;81:291–8.
Japanese Society of Nephrology, Evidence-based Clinical Practice Guideline for CKD, 2013. http://www.jsn.or.jp/guideline/pdf/CKD_evidence2013/all.pdf. Accessed 17 May 2017.
Lam CS, Xanthakis V, Sullivan LM, Lieb W, Aragam J, Redfield MM, Mitchell GF, Benjamin EJ, Vasan RS. Aortic root remodelling over the adult life course: longitudinal data from the Framingham Heart study. Circulation. 2010;122:884–90.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Imaging. 2015;16:233–71.
László A, Reusz G, Nemcsik J. Ambulatory arterial stiffness in chronic kidney disease: a methodological review. Hypertens Res. 2016;39:192–8.
van Varik BJ, Vossen LM, Rennenberg RJ, Stoffers HE, Kessels AG, de Leeuw PW, Kroon AA. Arterial stiffness and decline of renal function in a primary care population. Hypertens Res. 2017;40:73–8.
Briet M, Boutouyrie P, Laurent S, London GM. Arterial stiffness and pulse pressure in CKD and ESRD. Kidney Int. 2012;82:388–400.
Jia G, Aroor AR, Sowers JR. Arterial stiffness: a nexus between cardiac and renal disease. Cardiorenal Med. 2014;4:60–71.
Kheder-Elfekih R, Yannoutsos A, Blacher J, London GM, Safar ME. Hypertension and chronic kidney disease: respective contribution of mean and pulse pressure and arterial stiffness. J Hypertens. 2015;33:2010–5.
O’Rourke MF, Safar ME. Relationship between aortic stiffening and microvascular disease in brain and kidney: cause and logic of therapy. Hypertension. 2005;46:200–4.
Miller AB, Reichek N, St John Sutton M, Iyengar M, Henderson LS, Tarka EA, Bakris GL. Importance of blood pressure control in left ventricular mass regression. J Am Soc Hypertens. 2010;4:302–10.
Wassertheurer S, Burkhardt K, Heemann U, Baumann M. Aortic to brachial pulse pressure amplification as functional marker and predictor of renal function loss in chronic kidney disease. J Clin Hypertens. 2014;16:401–5.
Acknowledgements
The authors appreciate numerous fellows, nurses, and laboratory technicians who participated in this study. We also thank Ms. Mieko Iwai for secretarial help during the preparation of the manuscript. Parts of the data in this manuscript were presented at the 37th Annual Scientific Meeting of the Japanese Society of Hypertension, Yokohama Kanagawa, October 2014 and published in abstract form.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The ABC-J study was supported by Omron Healthcare Co., Ltd. Omron Healthcare was not involved in any significant processes of the study, including the design, conducting and monitoring of the study, data analysis, and publication. The authors declare that they have no conflict of interest.
Additional information
Members of the ABC-J II study group are listed above references.
Electronic supplementary material
Appendix
Appendix
Members of the ABC-J II study group
Collaboration and related facilities
Kazuyuki Shimada, Sadayoshi Ito, Yutaka Imai, Kazuo Eguchi, Yuko Ota, Mari Odaira, Kazuomi Kario, Yuhei Kawano, Mineko Kino, Katsuhiko Kohara, Hiromichi Suzuki, Kenji Sunagawa, Kenji Takazawa, Tsuneo Takenaka, Yasuharu Tabara, Yasuaki Dohi, Hirofumi Tomiyama, Junichiro Hashimoto, Yoshitaka Hirooka, Hiroshi Miyashita, Akira Yamashina, Joji Ishikawa, Hideaki Takata, Motoki Fukutomi, Yoshio Matsui, Nobuyuki Shiba, Takahiro Komori.
Cooperation facilities
Toshiro Iketani, Mitsutoshi Kato, Toru Awaya, Yoshikazu Aoka, Tsuguhisa Hatano, Naoto Yagi, Ken Oyama, Masaaki Miyakawa, Hiro Yamakawa, Hareaki Yamamoto, Hisao Mori, Kiyoshi Uchiba, Takeshi Takami.
Independent members for event evaluation and data analysis
Yasuhisa Kitagawa, Junichi Yamazaki, Koichi Hayashi, Uichi Ikeda, Hirohisa Okuma, Kentaro Tokuoka, Shinji Hisatake, Shu Wakino, Hirofumi Tokuyama, Takayoshi Ohkubo.
Rights and permissions
About this article
Cite this article
Takenaka, T., Suzuki, H., Eguchi, K. et al. Elevated pulse amplification in hypertensive patients with advanced kidney disease. Hypertens Res 41, 299–307 (2018). https://doi.org/10.1038/s41440-017-0010-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-017-0010-4
- Springer Nature Singapore Pte Ltd.
This article is cited by
-
Determinants of pulse pressure amplification in hypertensive and diabetic patients
Hypertension Research (2019)
-
Central hemodynamics and left ventricular hypertrophy in chronic kidney disease
Hypertension Research (2018)