Abstract
Background/objectives
Sarcopenia is an age-related muscle disease associated with higher mortality, morbidity risk and health costs. An easy and convenient sarcopenia screening test would be hugely valuable for clinical critical care. The study aimed to assess handgrip strength (HGS) as a screening tool for sarcopenia in acute care-unit inpatients, using the EWGSOP 1 reference-standard definition.
Subjects/methods
Inpatients, aged 75 years old or above, of two acute care wards—a multidisciplinary care unit (MCU) and a geriatric care unit (GCU), were included between September 2017 and June 2018 in a cross-sectional study. HGS, sarcopenia, nutritional status, functional status, number of medications and sociodemographic data were collected. The accuracy of HGS as a screening test for sarcopenia was assessed by gender using receiver operating characteristic (ROC) curves and area under the curve (AUC) in a population of older patients (n = 223; age: 85.8 yrs; BMI: 26.7 kg/m²).
Results
Screening was positive (patients confirmed with sarcopenia by the HGS test) with cut-off values of 18 kg for women and 25.5 kg for men, with ROC analysis giving a sensitivity of 92.9% in women and 78.6% in men. ROC curve analysis found also that HGS should be strictly higher than 15 kg in women and 18 kg in men to maximise AUC. Prevalence of sarcopenia according to the EWGSOP1 definition was 31.8% (95% CI: 22.1–41.6%) in the MCU and 27.8% (95% CI: 19.6–36.0%) in the GCU.
Conclusions
Acute care wards can use HGS as a valid, easy tool for early screening of sarcopenia.
Highlights
-
Handgrip strength is a valid and clinically practicable test, for screening early-onset sarcopenia during hospitalisation.
-
Handgrip strength cut-off values of 18 kg in women and 25.5 kg in men gave 92.9% and 78.6% sensitivity, respectively.
-
One-third of patients admitted to acute care wards have sarcopenia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Sarcopenia is an age-related muscle disease associated with higher mortality, morbidity risk [1,2,3,4,5,6,7,8,9,10,11,12,13], falls in older people, cognitive disorders, surgical complications, and longer hospital stays [4, 5, 7, 8, 10, 11]. An easy and convenient sarcopenia screening test would therefore be hugely valuable, especially when patients are admitted to critical care settings. However, to our knowledge, there is still no easy and practicable screening tool for use by any care workers in any older-adult setting (community-dwelling, hospital and retirement home).
Patients with sarcopenia have a significantly higher mortality rate, not only during their hospital stay but also in the year after discharge [2, 6, 11,12,13,14]. Sarcopenia also carries a significant economic burden. Hospitalisation and social healthcare costs are higher in patients with sarcopenia irrespective of age [15, 16]. The number of patients with sarcopenia is projected to rise dramatically in Europe, from 19,740,527 in 2016 to 32,338,990 in 2045 [17]. The pathogenesis of sarcopenia is multifactorial, encompassing genetics, lifestyle factors (lack of exercise, immobilisation, low-protein/high-fat diet), endocrinology (hormone and cytokine changes), metabolism (anabolic resistance), and neuromuscular factors (motor unit remodelling) [18, 19]. Treatment of sarcopenia may involve interventions including exercise and nutrition, but further evidence is needed [14, 18, 20,21,22,23].
In 2010, the European Working Group on Sarcopenia in Older People (EWGSOP) proposed an algorithm for case-finding based on measures of gait speed and handgrip strength (HGS) or muscle mass [19]. However, early gait speed assessment is infeasible in acute settings as it would delay care [24]. Here, we hypothesise that HGS could be performed to screen sarcopenia earlier during hospital stay, as proposed in the EWGSOP2 revision [25].
Our study called sarcopenia in older adult (SARCSA 1) aimed to assess whether HGS assessment is a relevant sarcopenia’ screening test in acute care unit inpatients, using the EWGSOP 2010 reference-standard definition.
Materials/subjects and methods
Study design
A multidepartment cross-sectional study was conducted in two acute care wards, one multidisciplinary care unit (MCU) and one geriatric care unit (GCU) between September 2017 and June 2018. It was proposed to inpatients during the first three days of their hospital stay. Readmitted patients could not be included a second time. The Confusion Assessment Method was performed to identify confused patients [26, 27], and if patients showed confusion or a medical history of dementia, the study was presented to their family. We, then checked, inclusion and exclusion criteria.
All data was captured once during the first seven days of hospital stay, then analysed at Clermont-Ferrand University Hospital (CFUH) public health unit. The study was sponsored by CFUH, validated by its scientific committee, approved by a local ethic institutional review board [Comité de Protection des Personnes Sud-Est VI] (AU 1289), and registered at Clinical Trials.gov. The study was sponsored also by Nutriset and Nutricia (support from a national congress research price)
Reporting worked to the Standards for Reporting of Diagnostic Accuracy statement [28].
Patients
Inpatients aged ≥75 years were eligible for inclusion. Exclusion criteria were patients in end-of-life care, inappropriate medical situation, patient (or family in background confusion or dementia) refusal to participate, patients safeguarded as vulnerable adults, patients fed exclusively via percutaneous endoscopic gastrostomy. Patients or family gave informed consent.
Measures
Sarcopenia was defined as per EWGSOP 2010 as a combination of low muscle mass with diagnosed low muscle strength or/and low physical performance [19]. Here, we did not make the EWGSOP 2010-defiined distinction between sarcopenia and severe.
Low muscle mass was estimated by calculating skeletal muscle index (SMI) based on bioelectrical-impedance analysis (BIA) using Bodystat® 1500 (Bodystat, United Kingdom). Four surface electrodes were placed, one on the right third metacarpal bone, one between the right styloid of the radius and ulna, one on the right malleoli of the ankle, and one on the third metatarsal bone, with patients supine for at least 10 min. BIA was performed in patients with normal hydration status but not in patients with a pacemaker and implantable cardioverter-defibrillator. Hydration status was evaluated by clinical exam and on blood sample. In case of abnormal hydration status, BIA was done few days after the entrance in a maximum period of 7 days. SMI was calculated as absolute skeletal muscle (SM) mass divided by height squared, with height in metres. SM was calculated using the Janssen et al. equation. The EWGSOP guidelines recommended use of normative references (healthy young adults) with cut-off points set at two standard deviations below the mean reference value [19]. Cut-off points in the French population were low SMI values, at <8.6 kg/m² in men and 6.2 kg/m² in women [29]. Muscle strength was measured by HGS on a Jamar® hydraulic hand dynamometer (Performance Health, France) in sitting position following the Southampton protocol [30]. Three measures were performed from each side, and the highest and the mean were used for analysis. HGS is considered low under 30 kg in men and <20 kg in women [19]. Physical performance was measured using the 4-m gait-speed test, expressed in m/s. It is considered slow under 0.8 m/s [19]. The same BIA device and handgrip dynamometer were used on both sites, so that we are confident on the overall results.
Comorbidity was measured using the Cumulative Illness Rating Scale- for Geriatrics (CIRS-G) [31], which assesses comorbidity through 14 organ system categories on a severity scale from no problem (0) to extremely severe/immediate treatment required/organ failure/severe functional impairment [4]. CIRS-G scoring yields five numbers: total number of categories scored, total score (/56), severity index (ratio of total score/number of categories), number of grade 3 and number of grade 4 categories.
Katz Activities of Daily Living scale (ADL) and Lawton Instrumental Activities of Daily Living scale (IADL) were used to measure functional status [32,33,34]. ADL explored six dimensions rated 0 (unable), 0.5 (partially able) or 1 (able): bathing, dressing, toileting, transferring, continence, and feeding, giving a total score from 0 to 6. IADL measured eight dimensions rated 0 (unable) or 1 (able): telephoning, shopping, cooking, housekeeping, laundry, transportation, managing medications and finances, giving a total score from 0 to 8.
Anthropometric measurements included usual weight (kg), weight at admission (kg), height (m), body mass index (BMI) (weight at admission/height²-kg/m²), BIA values (fat free mass (%), fat mass (%), impedance at 5 khz (ohm), impedance at 50 khz (ohm), resistance (ohm), reactance (ohm) and phase angle (degree). Cellular hydration state was also evaluated clinically and on blood samples, as normal, intracellular dehydration, extracellular dehydration, intracellular hyper-hydration, and extracellular hyper-hydration.
Nutritional status was evaluated using the Mini Nutritional Assessment (MNA) [35] and albumin (g/L), transthyretin (mg/L) and C-reactive-protein (CRP- g/l) measurements. Moderate and severe chronic malnutrition in older people (aged ≥ 75 years) was measured according to French Nutrition Society and French National Health Authority guidelines [36]. Moderate chronic malnutrition was defined as one or more criteria among: weight loss ≥5% in a month or ≥10% in 6 months, BMI < 21 kg/m², albumin < 35 g/L, MNA < 17. Severe chronic malnutrition was defined as one or more criteria among: weight loss ≥ 10% in a month or ≥15% in 6 months, BMI < 18 kg/m², albumin < 30 g/L. Acute malnutrition was defined by prealbumin < 0.2 g/L.
Sociodemographic data were collected on age, gender, housing (at home, a residential home, other), and lifestyle (living alone, in couple, with family, other). Daily medication was recorded.
Statistical analysis
Descriptive analysis was performed to assess sociodemographic characteristics, prevalence of sarcopenia and nutritional status. Qualitative variables were expressed as numbers and percentages. Quantitative variables were expressed as means with standard deviation (SD), median with interquartile range, and min–max.
To assess the accuracy of HGS as a screening test for sarcopenia, receiver operating characteristic curves (ROC) and area under the ROC (AUC) were estimated by gender [37]. Taking the EWGSOP 2010 definition as reference standard [19]. The ROC shows the ability of HGS to discriminate between sarcopenia and no sarcopenia. The AUC ranges from 0.5 to 1 where higher values indicate better test accuracy. HGS thresholds were tested by gender to find optimal sensitivity, specificity, and positive and negative predictive values [38, 39].
Two-sided p values < 0.05 were considered statistically significant. Statistical analysis was performed using SAS software (v9.4. SAS Institute Inc., Cary, NC).
Results
Patient characteristics
Table 1 reports sociodemographics, daily medications, comorbidity and functional status of the 223 patients included, 104 in MCU (56.7% women) and 119 in GCU (76.5% women). Mean age was 85.7 years old (SD 5.3) in MCU and 85.9 years old (SD 4.7) in GCU. Most patients lived at home (89.4% in MCU and 89.9% in GCU). Mean number of daily medications was 7.3 (SD 3.2) in MCU and 7.4 (SD 3.4) in GCU (from 0 to 16). Patients had a mean of 6 (SD 2.1) comorbidities in MCU and 8.7 (SD 3.0) in GCU and all had at least two disorders rated grade 3 or grade 4 severity on the CIRS-G. In terms of functional abilities, 25% of patients needed care-unit support for both ADL and IADL. Only gender and comorbidities were significantly different between patients in MCU and GCU (p = 0.0017 and p < 0.0001 for CIRS-G).
Prevalence of sarcopenia and malnutrition
Table 2 summarises the EWGSOP criteria and cut-off values for sarcopenia. Prevalence of sarcopenia was 31.8% (95% CI: 22.1–41.6%) in MCU and 27.8% (95% CI: 19.6–36.0%) in GCU (Table 3) (p = 0.54). Prevalence of sarcopenia was 31.8% (95% CI: 20.3–43.2%) for men and 28.6% (95% CI: 21.1–36.1%) for women (p = 0.65).
BIA showed a fat mass/lean mass ratio of 43%/57% among women in both MCU and GCU and 33%/67% in MCU and 29%/71% in GCU among men. Mean gait speed was <0.8 m/s in both MCU and GCU (Table 3).
Prevalence of chronic malnutrition was 76% (95% CI: 67.7–84.2%) in MCU and 85.7% (95% CI: 79.4–92%) in GCU. Prevalence of acute malnutrition was 56.9% (95% CI: 47.3–66.5%) in MCU and 50.4% (95% CI: 41.4–59.5%) in GCU (Table 3).
Performance of handgrip strength to screen sarcopenia
The HGS test was well accepted and easy to perform, with measures done for 96.2% and 93.3% of MCU and GCU inpatients, respectively. Mean and maximum of the six HGS measures were 14.2 kg (SD 4.2) and 16.6 kg (SD 4.3) in MCU women, 20.4 kg (SD 7.9) and 22.7 kg (SD 8.1) in MCU men, 10.8 kg (SD 4.9) and 12.9 kg (SD 5.3) in GCU women, and 21.8 kg (SD 7.4) and 25.3 kg (SD 8.0) in GCU men.
As patient sociodemographic characteristics, except gender, functional ability and prevalence of sarcopenia were not significantly different between MCU and GCU, we grouped the two groups of patients together to analyse the screening performance of handgrip strength.
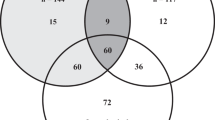
AUC analysis performed using the mean and maximum of the six measures found that maximum values performed better for screening, and so only maximum values are presented in Table 4. ROC curve analysis found that HGS was only useable as a screening test if the measures were strictly higher than 15 kg in women and 18 kg in men, as the AUC was then 0.72 (95% CI: 0.59–0.85) for women and 0.75 (95% CI: 0.58–0.93) for men (Fig. 1). Cut-off points of 18 kg for women and 25.5 kg for men gave satisfactory sensitivity, specificity, and positive and negative predictive values. Using these cut-offs classified 59.0% of women and 49% of men with sarcopenia.
Discussion
Our results validated HGS as an affordable relevant sarcopenia tool in current practice in hospital units, for older subjects over a threshold of usability. This measure reliably discriminated patients with or without sarcopenia with acceptable sensitivity and specificity [39]. The present study confirms that in medical hospital unit, the first step to diagnose sarcopenia should be HGS, as the performance of the two other measures (quantity and quality of muscles and physical performance) could be compromised by the patient health state, i.e. cardiovascular disease with oedema or unable to walk at the start of the hospital stay. In our study, 17.3% and 26.1% of the patients in MCU and GCU, respectively could not perform the gait speed test.
The maximum of HGS measures should be preferred to the mean value for several reasons. Firstly, it is easier in clinical practice to choose a maximum than calculate a mean. Secondly, using the maximum of the measures limited the learning effect. Thirdly, it gave better results in terms of screening performance.
Our study population was comparable to other studies. Several studies were performed in elderly people hospitalised in acute wards or in acute geriatric wards with global prevalence of sarcopenia (EWGSOP 2010 definition) from 10.2 to 34.7%. Most of the studies used the BIA to measure SMI and prevalence of sarcopenia by using 8.87 kg/m² thresholds in men and 6.42 kg/m² in women [12, 13, 24, 40,41,42,43]. Two studies used the BIA with other cut-offs [44, 45] (10.75 kg/m² in men and 6.75 kg/m² in women) with comparable prevalence in women but not in men [46, 47]. One study used two standard deviation below the reference of young adults in the French context and calculated a prevalence of 12.5% in men and 23.6% in women in a younger population (mean age 64.4 (SD 3.7)) [29]. Two studies measured the mid arc muscle circumference [46, 47]. A recent systematic review identified lower prevalence in hospitalised patients age over 60 years, 23% (95% CI: 15–32%) [48].
Our cut-off points for HGS for screening are close to those recommended in the revised version of the EWGSOP group (HGS < 27 kg in men, and <16 kg in women) [25].
Our results could be used to screen sarcopenia sooner in hospitalisation. But the ROC curves analysis needs more subjects to improve our result, in various settings.
HGS (using the maximum of the measures) could not be used as a screening test when muscular force is below or equal to 18 kg in men and 15 kg in women. In these cases, BIA or dual energy X-ray absorptiometry should be performed as soon as possible to diagnose sarcopenia (see EWGSOP2 reference) and patients should be cared as patients with sarcopenia because low HGS is associated with higher risk of morbidity and mortality. The screening with HGS test was positive for measures ≤25.5 kg in men and 18 kg in women. Sarcopenia treatment is based on physical activity as soon as possible and adequate nutritional diet. In this case, caring patients with sarcopenia, even if they are false positive, is not prejudicial in medical hospital units. So, the low specificity of HGS test was not problematic. On the contrary, to wait until the measurement of the quantity and the quality of muscle could be done, would be deleterious for patients due to the delay of the appropriate care. The sensitivity of HGS as a screening test for sarcopenia was satisfactory, especially in women (92.9% in women vs. 78.6% in men).
The EWGSOP group made a revised version of the European algorithm in 2019 [25]. They recommended first to screen people by using the SARC-F, second to diagnose cases by measuring muscular force, third to confirm by measuring muscle quantity or quality, and fourth to evaluate the severity by assessing muscular performance. Considering this revised version, the global prevalence of sarcopenia in the present study were 59.2% (51.0% in MCU and 66.7% in GCU), 54.9% in women (34.5% in MCU and 68.6% in GCU) and 68.7% in men (73.8% in MCU and 60.0% in GCU). The EWGSOP also suggested areas for further research about cut-off points used that need to be validated. The present study identified cut-off points for screening sarcopenia by performing HGS in medical units. But as further research is needed on larger samples and other settings, a study has begun in MCU, rehabilitation units and retired home including more than 350 subjects.
Analysing HGS slope during hospital stays could be relevant to identified patients’ profiles at higher risk. Those profiles could be used to support hospital medical team to take charge patients appropriately during hospitalisation and after in coordination with outpatient care.
HGS is an easy clinically-practicable test for screening early sarcopenia during hospital stay. Further research is needed to confirm cut-off points identified and for dealing with HGS and its evolution during hospital stays. Identifying profiles of patients at risk lead to developing proactive treatment during hospitalisation and after.
References
Visser M, Schaap LA. Consequences of sarcopenia. Clin Geriatr Med. 2011;27:387–99. août
Leeper C, Lin E, Hoffman M, Fombona A, Zhou T, Kutcher M, et al. CT abbreviated assessment of sarcopenia following trauma: the CAAST measurement predicts 6-month mortality in older adult trauma patients. J Trauma Acute Care Surg. 2016;80:805–11.
Janssen I. Influence of sarcopenia on the development of physical disability: the cardiovascular health study. J Am Geriatr Soc. 2006;54:56–62.
Shachar SS, Williams GR, Muss HB, Nishijima TF. Prognostic value of sarcopenia in adults with solid tumours: a meta-analysis and systematic review. Eur J Cancer. 2016;57:58–67.
Nishigori T, Okabe H, Tanaka E, Tsunoda S, Hisamori S, Sakai Y. Sarcopenia as a predictor of pulmonary complications after esophagectomy for thoracic esophageal cancer. J Surg Oncol. 2016;113:678–84.
Chang S-F, Lin P-L. Systematic literature review and meta-analysis of the association of sarcopenia with mortality. Worldviews Evid-Based Nurs. 2016;13:153–62.
Sousa AS, Guerra RS, Fonseca I, Pichel F, Amaral TF. Sarcopenia and length of hospital stay. Eur J Clin Nutr. 2015;34:881–8.
Nishiguchi S, Yamada M, Shirooka H, Nozaki Y, Fukutani N, Tashiro Y, et al. Sarcopenia as a risk factor for cognitive deterioration in community-dwelling older adults: a 1-year prospective study. J Am Med Dir Assoc. 2016;17:372.e5–8.
Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–8.
Clynes MA, Edwards MH, Buehring B, Dennison EM, Binkley N, Cooper C. Definitions of sarcopenia: associations with previous falls and fracture in a population sample. Calcif Tissue Int. 2015;97:445–52.
Hirani V, Blyth F, Naganathan V, Le Couteur DG, Seibel MJ, Waite LM, et al. Sarcopenia is associated with incident disability, institutionalization, and mortality in community-dwelling older men: the concord health and ageing in men project. J Am Med Dir Assoc. 2015;16:607–13.
Cerri AP, Bellelli G, Mazzone A, Pittella F, Landi F, Zambon A, et al. Sarcopenia and malnutrition in acutely ill hospitalized elderly: prevalence and outcomes. Clin Nutr. 2015;34:745–51.
Vetrano DL, Landi F, Volpato S, Corsonello A, Meloni E, Bernabei R, et al. Association of sarcopenia with short- and long-term mortality in older adults admitted to acute care wards: results from the CRIME study. J Gerontol A Biol Sci Med Sci. 2014;69:1154–61.
Beaudart C, Zaaria M, Pasleau F, Reginster J-Y, Bruyère O. Health outcomes of sarcopenia: a systematic review and meta-analysis. PloS One. 2017;12:e0169548.
Sousa AS, Guerra RS, Fonseca I, Pichel F, Ferreira S, Amaral TF. Financial impact of sarcopenia on hospitalization costs. Eur J Clin Nutr. 2016;70:1046–51.
Janssen I, Shepard DS, Katzmarzyk PT, Roubenoff R. The healthcare costs of sarcopenia in the United States. J Am Geriatr Soc. 2004;52:80–5.
Beaudart C, Rizzoli R, Bruyère O, Reginster J-Y, Biver E. Sarcopenia: burden and challenges for public health. Arch Public Health. 2014;72:45.
Dhillon RJS, Hasni S. Pathogenesis and management of sarcopenia. Clin Geriatr Med. 2017;33:17–26.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis. Age Ageing. 2010;39:412–23.
Cruz-Jentoft AJ, Landi F, Schneider SM, Zúñiga C, Arai H, Boirie Y, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing. 2014;43(nov):748–59.
Walrand S, Gryson C, Salles J, Giraudet C, Migné C, Bonhomme C, et al. Fast-digestive protein supplement for ten days overcomes muscle anabolic resistance in healthy elderly men. Clin Nutr. 2016;35:660–8.
Boirie Y, Guillet C. Fast digestive proteins and sarcopenia of aging. Curr Opin Clin Nutr Metab Care. 2018;21:37–41.
Chanet A, Verlaan S, Salles J, Giraudet C, Patrac V, Pidou V, et al. Supplementing breakfast with a vitamin D and leucine-enriched whey protein medical nutrition drink enhances postprandial muscle protein synthesis and muscle mass in healthy older men. J Nutr. 2017;147:2262–71.
Ibrahim K, Howson FFA, Culliford DJ, Sayer AA, Roberts HC. The feasibility of assessing frailty and sarcopenia in hospitalised older people: a comparison of commonly used tools. BMC Geriatr. 2019;19:42.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31.
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–8.
Laplante J, Cole M, McCusker J, Singh S, Ouimet M-A. Confusion Assessment Method. Validation of a French-language version. Perspect Infirm Rev Ordre Infirm Infirm Qué. 2005;3:12–4.
Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig LM, et al. Towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative. BMJ. 2003;326:41–4.
Tichet J, Vol S, Goxe D, Salle A, Berrut G, Ritz P. Prevalence of sarcopenia in the French senior population. J Nutr Health Aging. 2008;12:202–6.
Roberts HC, Denison HJ, Martin HJ, Patel HP, Syddall H, Cooper C, et al. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing. 2011;40:423–9.
Salvi F, Miller MD, Grilli A, Giorgi R, Towers AL, Morichi V, et al. A manual of guidelines to score the modified cumulative illness rating scale and its validation in acute hospitalized elderly patients. J Am Geriatr Soc. 2008;56:1926–31.
Katz S, Akpom CA. A measure of primary sociobiological functions. Int J Health Serv Plan Adm Eval. 1976;6:493–508.
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. the index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–9.
Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–86.
Rubenstein LZ, Harker JO, Salvà A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol A Biol Sci Med Sci. 2001;56:M366–372.
Haute Autorité de Santé S des recommandations professionnelles. Stratégie de prise en charge en cas de dénutrition protéino-énergétique chez la personne âgée. Haute Autorité de Santé; 2007 avr p. 25.
Comparing the accuracy of two diagnostic tests. In: Statistical methods in diagnostic medicine [Internet]. John Wiley & Sons, Ltd; 2011 [cité 19 janv 2020]. p. 165–92. Disponible sur: https://onlinelibrary.wiley.com/doi/abs/10.1002/9780470906514.ch5.
Comparing the accuracy of two diagnostic tests. In: Statistical methods in diagnostic medicine [Internet]. John Wiley & Sons, Ltd; 2008 [cité 19 févr 2020]. p. 165–94. Disponible sur: https://onlinelibrary.wiley.com/doi/abs/10.1002/9780470317082.ch5.
Takwoingi Y, Quinn TJ. Review of Diagnostic Test Accuracy (DTA) studies in older people. Age Ageing. 2018;47:349–55.
Smoliner C, Sieber CC, Wirth R. Prevalence of sarcopenia in geriatric hospitalized patients. J Am Med Dir Assoc. 2014;15:267–72.
Rossi AP, Fantin F, Micciolo R, Bertocchi M, Bertassello P, Zanandrea V, et al. Identifying sarcopenia in acute care setting patients. J Am Med Dir Assoc. 2014;15:303.e7–12.
Zengarini E, Giacconi R, Mancinelli L, Riccardi GR, Castellani D, Vetrano DL, et al. Prognosis and interplay of cognitive impairment and sarcopenia in older adults discharged from Acute Care Hospitals. J Clin Med. 2019;8:1693.
Bianchi L, Abete P, Bellelli G, Bo M, Cherubini A, Corica F, et al. Prevalence and clinical correlates of sarcopenia, identified according to the EWGSOP definition and diagnostic algorithm, in hospitalized older people: the GLISTEN study. J Gerontol A Biol Sci Med Sci. 2017;72:1575–81.
Sipers WMWH, Meijers JMM, van Dijk RB, Halfens RJG, Schols JMGA. Impact of different diagnostic criteria on the prevalence of sarcopenia in an acute care geriatric ward. J Frailty Aging. 2014;3:222–9.
Sousa AS, Guerra RS, Fonseca I, Pichel F, Amaral TF. Sarcopenia among hospitalized patients—a cross-sectional study. Clin Nutr. 2015;34:1239–44.
Gariballa S, Alessa A. Sarcopenia: prevalence and prognostic significance in hospitalized patients. Clin Nutr. 2013;32:772–6.
Jacobsen EL, Brovold T, Bergland A, Bye A. Prevalence of factors associated with malnutrition among acute geriatric patients in Norway: a cross-sectional study. BMJ Open. 2016;6:e011512.
Papadopoulou SK, Tsintavis P, Potsaki P, Papandreou D. Differences in the prevalence of sarcopenia in community-dwelling, nursing home and hospitalized individuals. a systematic review and meta-analysis. J Nutr Health Aging. 2020;24:83–90.
Acknowledgements
The research team thanks paramedical and medical staff of the two acute care wards.
Funding
The study was funded by Clermont-Ferrand University Hospital and two local hospitals. The study was sponsored by Nutriset and Nutricia (support from a national congress research price). These financial supports played no role in the design, execution, analysis and interpretation of the data.
Author information
Authors and Affiliations
Contributions
MB was responsible for designing the protocol, writing the protocol, conducting the clinical research, interpreting results and writing the article. GD was responsible for designing the protocol, conducting the clinical research and reading the article. AS was responsible for reading the article. SD and NF were responsible for designing the protocol and writing the article. VG was responsible for conducting the clinical research and reading the article. CGA and PB were responsible for designing the protocol, writing the protocol, extracting and analysing data, interpreting results and writing the article. JB was responsible for designing the protocol and reading the article. YB and LG were responsible for designing the protocol, interpreting results and writing the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Blanquet, M., Ducher, G., Sauvage, A. et al. Handgrip strength as a valid practical tool to screen early-onset sarcopenia in acute care wards: a first evaluation. Eur J Clin Nutr 76, 56–64 (2022). https://doi.org/10.1038/s41430-021-00906-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-021-00906-5
- Springer Nature Limited
This article is cited by
-
Neural network model for prediction of possible sarcopenic obesity using Korean national fitness award data (2010–2023)
Scientific Reports (2024)
-
Association between reduced physical performance measures and short-term consequences after major emergency abdominal surgery: a prospective cohort study
European Journal of Trauma and Emergency Surgery (2024)
-
Sarcopenia: if it looks/walks like a duck, it must be a duck
European Journal of Clinical Nutrition (2022)